Early Mortality Stratification with Serum Albumin and the Sequential Organ Failure Assessment Score at Emergency Department Admission in Septic Shock Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics and Laboratory Findings
3.2. Comparison of Clinical and Laboratory Characteristics in Each Group According to Albumin Levels
3.3. Risk Factors Associated with 28-Day Mortality and Evaluation of Model Performance of the SOFA Score Combined with Albumin
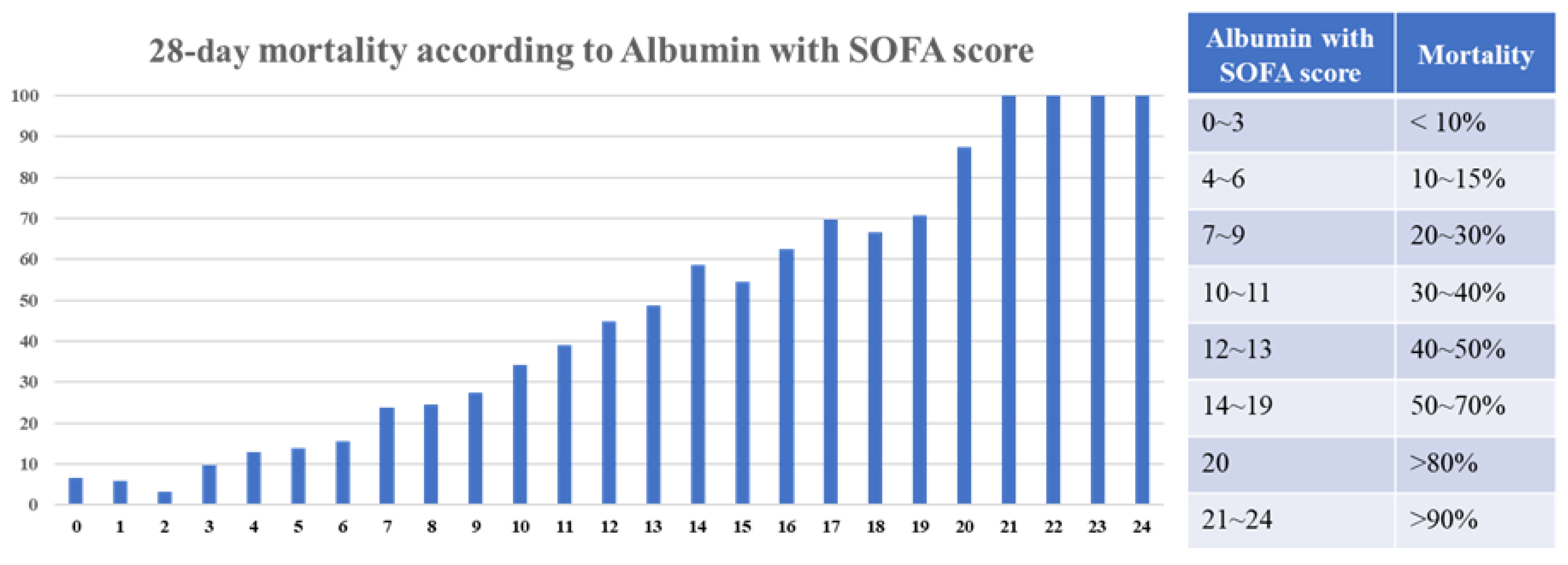
3.4. Mortality Rate According to the SOFA Score Combined with Albumin
3.5. Validation in AMC Cohort and MIMIC-IV Database
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bhavani, S.V.; Carey, K.A.; Gilbert, E.R.; Afshar, M.; Verhoef, P.A.; Churpek, M.M. Identifying Novel Sepsis Subphenotypes Using Temperature Trajectories. Am. J. Respir. Crit. Care Med. 2019, 200, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Kennedy, J.N.; Wang, S.; Chang, C.H.; Elliott, C.F.; Xu, Z.; Berry, S.; Clermont, G.; Cooper, G.; Gomez, H.; et al. Derivation, Validation, and Potential Treatment Implications of Novel Clinical Phenotypes for Sepsis. JAMA 2019, 321, 2003–2017. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Opal, S.; Calandra, T. Sepsis studies need new direction. Lancet Infect. Dis. 2012, 12, 503–505. [Google Scholar] [CrossRef] [PubMed]
- DeMerle, K.M.; Angus, D.C.; Baillie, J.K.; Brant, E.; Calfee, C.S.; Carcillo, J.; Chang, C.H.; Dickson, R.; Evans, I.; Gordon, A.C.; et al. Sepsis Subclasses: A Framework for Development and Interpretation. Crit. Care Med. 2021, 49, 748–759. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V. Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef]
- Peake, S.L.; Delaney, A.; Bailey, M.; Bellomo, R.; Cameron, P.A.; Cooper, D.J.; Higgins, A.M.; Holdgate, A.; Howe, B.D.; Webb, S.A.; et al. Goal-directed resuscitation for patients with early septic shock. N. Engl. J. Med. 2014, 371, 1496–1506. [Google Scholar] [CrossRef]
- Domínguez de Villota, E.; Mosquera, J.M.; Rubio, J.J.; Galdos, P.; Díez Balda, V.; de la Serna, J.L.; Tomás, M.I. Association of a low serum albumin with infection and increased mortality in critically ill patients. Intensive Care Med. 1980, 7, 19–22. [Google Scholar] [CrossRef]
- Eckart, A.; Struja, T.; Kutz, A.; Baumgartner, A.; Baumgartner, T.; Zurfluh, S.; Neeser, O.; Huber, A.; Stanga, Z.; Mueller, B.; et al. Relationship of Nutritional Status, Inflammation, and Serum Albumin Levels during Acute Illness: A Prospective Study. Am. J. Med. 2020, 133, 713–722.e717. [Google Scholar] [CrossRef]
- Caironi, P.; Langer, T.; Gattinoni, L. Albumin in critically ill patients: The ideal colloid? Curr. Opin. Crit. Care 2015, 21, 302–308. [Google Scholar] [CrossRef]
- Finfer, S.; Bellomo, R.; McEvoy, S.; Lo, S.K.; Myburgh, J.; Neal, B.; Norton, R. Effect of baseline serum albumin concentration on outcome of resuscitation with albumin or saline in patients in intensive care units: Analysis of data from the saline versus albumin fluid evaluation (SAFE) study. BMJ 2006, 333, 1044. [Google Scholar] [CrossRef]
- Vincent, J.L.; Dubois, M.J.; Navickis, R.J.; Wilkes, M.M. Hypoalbuminemia in acute illness: Is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann. Surg. 2003, 237, 319–334. [Google Scholar] [CrossRef] [PubMed]
- Yin, M.; Si, L.; Qin, W.; Li, C.; Zhang, J.; Yang, H.; Han, H.; Zhang, F.; Ding, S.; Zhou, M.; et al. Predictive Value of Serum Albumin Level for the Prognosis of Severe Sepsis Without Exogenous Human Albumin Administration: A Prospective Cohort Study. J. Intensive Care Med. 2018, 33, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Shin, T.G.; Kim, W.Y.; Jo, Y.H.; Hwang, Y.J.; Choi, S.H.; Lim, T.H.; Han, K.S.; Shin, J.; Suh, G.J.; et al. A quick Sequential Organ Failure Assessment-negative result at triage is associated with low compliance with sepsis bundles: A retrospective analysis of a multicenter prospective registry. Clin. Exp. Emerg. Med. 2022, 9, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Ko, B.S.; Ryoo, S.M.; Han, E.; Suh, G.J.; Choi, S.H.; Chung, S.P.; Lim, T.H.; Kim, W.Y.; Kwon, W.Y.; et al. Modified cardiovascular SOFA score in sepsis: Development and internal and external validation. BMC Med. 2022, 20, 263. [Google Scholar] [CrossRef]
- You, J.S.; Park, Y.S.; Chung, S.P.; Lee, H.S.; Jeon, S.; Kim, W.Y.; Shin, T.G.; Jo, Y.H.; Kang, G.H.; Choi, S.H.; et al. Relationship between time of emergency department admission and adherence to the Surviving Sepsis Campaign bundle in patients with septic shock. Crit. Care 2022, 26, 43. [Google Scholar] [CrossRef]
- Yealy, D.M.; Kellum, J.A.; Huang, D.T.; Barnato, A.E.; Weissfeld, L.A.; Pike, F.; Terndrup, T.; Wang, H.E.; Hou, P.C.; LoVecchio, F.; et al. A randomized trial of protocol-based care for early septic shock. N. Engl. J. Med. 2014, 370, 1683–1693. [Google Scholar] [CrossRef]
- Mouncey, P.R.; Osborn, T.M.; Power, G.S.; Harrison, D.A.; Sadique, M.Z.; Grieve, R.D.; Jahan, R.; Harvey, S.E.; Bell, D.; Bion, J.F.; et al. Trial of early, goal-directed resuscitation for septic shock. N. Engl. J. Med. 2015, 372, 1301–1311. [Google Scholar] [CrossRef]
- Dellinger, R.P.; Levy, M.M.; Rhodes, A.; Annane, D.; Gerlach, H.; Opal, S.M.; Sevransky, J.E.; Sprung, C.L.; Douglas, I.S.; Jaeschke, R.; et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Crit. Care Med. 2013, 41, 580–637. [Google Scholar] [CrossRef]
- Suh, G.J.; Shin, T.G.; Kwon, W.Y.; Kim, K.; Jo, Y.H.; Choi, S.-H.; Chung, S.P.; Kim, W.Y. Hemodynamic management of septic shock: Beyond the Surviving Sepsis Campaign guidelines. Clin. Exp. Emerg. Med. 2023, 10, 255–264. [Google Scholar] [CrossRef] [PubMed]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Talmor, D.; Greenberg, D.; Howell, M.D.; Lisbon, A.; Novack, V.; Shapiro, N. The costs and cost-effectiveness of an integrated sepsis treatment protocol. Crit. Care Med. 2008, 36, 1168–1174. [Google Scholar] [CrossRef] [PubMed]
- Tong-Minh, K.; Welten, I.; Endeman, H.; Hagenaars, T.; Ramakers, C.; Gommers, D.; van Gorp, E.; van der Does, Y. Predicting mortality in adult patients with sepsis in the emergency department by using combinations of biomarkers and clinical scoring systems: A systematic review. BMC Emerg. Med. 2021, 21, 70. [Google Scholar] [CrossRef] [PubMed]
- Barichello, T.; Generoso, J.S.; Singer, M.; Dal-Pizzol, F. Biomarkers for sepsis: More than just fever and leukocytosis-A narrative review. Crit. Care 2022, 26, 14. [Google Scholar] [CrossRef]
- Churpek, M.M.; Snyder, A.; Han, X.; Sokol, S.; Pettit, N.; Howell, M.D.; Edelson, D.P. Quick Sepsis-related Organ Failure Assessment, Systemic Inflammatory Response Syndrome, and Early Warning Scores for Detecting Clinical Deterioration in Infected Patients outside the Intensive Care Unit. Am. J. Respir. Crit. Care Med. 2017, 195, 906–911. [Google Scholar] [CrossRef]
- Seymour, C.W.; Liu, V.X.; Iwashyna, T.J.; Brunkhorst, F.M.; Rea, T.D.; Scherag, A.; Rubenfeld, G.; Kahn, J.M.; Shankar-Hari, M.; Singer, M.; et al. Assessment of Clinical Criteria for Sepsis: For the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 762–774. [Google Scholar] [CrossRef]
- Bauer, M.; Gerlach, H.; Vogelmann, T.; Preissing, F.; Stiefel, J.; Adam, D. Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019-Results from a systematic review and meta-analysis. Crit. Care 2020, 24, 239. [Google Scholar] [CrossRef]
- Fleischmann, C.; Scherag, A.; Adhikari, N.K.; Hartog, C.S.; Tsaganos, T.; Schlattmann, P.; Angus, D.C.; Reinhart, K. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am. J. Respir. Crit. Care Med. 2016, 193, 259–272. [Google Scholar] [CrossRef]
- Abe, T.; Ogura, H.; Shiraishi, A.; Kushimoto, S.; Saitoh, D.; Fujishima, S.; Mayumi, T.; Shiino, Y.; Nakada, T.A.; Tarui, T.; et al. Characteristics, management, and in-hospital mortality among patients with severe sepsis in intensive care units in Japan: The FORECAST study. Crit. Care 2018, 22, 322. [Google Scholar] [CrossRef]
- Clermont, G.; Angus, D.C.; Linde-Zwirble, W.T.; Griffin, M.F.; Fine, M.J.; Pinsky, M.R. Does acute organ dysfunction predict patient-centered outcomes? Chest 2002, 121, 1963–1971. [Google Scholar] [CrossRef] [PubMed]
- Garland, A.; Olafson, K.; Ramsey, C.D.; Yogendran, M.; Fransoo, R. Distinct determinants of long-term and short-term survival in critical illness. Intensive Care Med. 2014, 40, 1097–1105. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, F.L.; Bota, D.P.; Bross, A.; Mélot, C.; Vincent, J.L. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 2001, 286, 1754–1758. [Google Scholar] [CrossRef] [PubMed]
- Fanali, G.; di Masi, A.; Trezza, V.; Marino, M.; Fasano, M.; Ascenzi, P. Human serum albumin: From bench to bedside. Mol. Aspects Med. 2012, 33, 209–290. [Google Scholar] [CrossRef]
- O’Brien, A.J.; Fullerton, J.N.; Massey, K.A.; Auld, G.; Sewell, G.; James, S.; Newson, J.; Karra, E.; Winstanley, A.; Alazawi, W.; et al. Immunosuppression in acutely decompensated cirrhosis is mediated by prostaglandin E2. Nat. Med. 2014, 20, 518–523. [Google Scholar] [CrossRef]
- Taverna, M.; Marie, A.L.; Mira, J.P.; Guidet, B. Specific antioxidant properties of human serum albumin. Ann. Intensive Care 2013, 3, 4. [Google Scholar] [CrossRef]
- Walley, K.R.; McDonald, T.E.; Wang, Y.; Dai, S.; Russell, J.A. Albumin resuscitation increases cardiomyocyte contractility and decreases nitric oxide synthase II expression in rat endotoxemia. Crit. Care Med. 2003, 31, 187–194. [Google Scholar] [CrossRef]
- Joannidis, M.; Wiedermann, C.J.; Ostermann, M. Ten myths about albumin. Intensive Care Med. 2022, 48, 602–605. [Google Scholar] [CrossRef]
- Goldwasser, P.; Feldman, J. Association of serum albumin and mortality risk. J. Clin. Epidemiol. 1997, 50, 693–703. [Google Scholar] [CrossRef]
- Artero, A.; Zaragoza, R.; Camarena, J.J.; Sancho, S.; González, R.; Nogueira, J.M. Prognostic factors of mortality in patients with community-acquired bloodstream infection with severe sepsis and septic shock. J. Crit. Care 2010, 25, 276–281. [Google Scholar] [CrossRef]
- Magnussen, B.; Oren Gradel, K.; Gorm Jensen, T.; Kolmos, H.J.; Pedersen, C.; Just Vinholt, P.; Touborg Lassen, A. Association between Hypoalbuminaemia and Mortality in Patients with Community-Acquired Bacteraemia Is Primarily Related to Acute Disorders. PLoS ONE 2016, 11, e0160466. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.C.; Corkins, M.R.; Malone, A.; Miller, S.; Mogensen, K.M.; Guenter, P.; Jensen, G.L. The Use of Visceral Proteins as Nutrition Markers: An ASPEN Position Paper. Nutr. Clin. Pract. 2021, 36, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Bretschera, C.; Boesiger, F.; Kaegi-Braun, N.; Hersberger, L.; Lobo, D.N.; Evans, D.C.; Tribolet, P.; Gomes, F.; Hoess, C.; Pavlicek, V.; et al. Admission serum albumin concentrations and response to nutritional therapy in hospitalised patients at malnutrition risk: Secondary analysis of a randomised clinical trial. EClinicalMedicine 2022, 45, 101301. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.K.; Mogensen, K.M.; Casey, J.D.; McKane, C.K.; Moromizato, T.; Rawn, J.D.; Christopher, K.B. The relationship among obesity, nutritional status, and mortality in the critically ill. Crit. Care Med. 2015, 43, 87–100. [Google Scholar] [CrossRef] [PubMed]
- Mogensen, K.M.; Robinson, M.K.; Casey, J.D.; Gunasekera, N.S.; Moromizato, T.; Rawn, J.D.; Christopher, K.B. Nutritional Status and Mortality in the Critically Ill. Crit. Care Med. 2015, 43, 2605–2615. [Google Scholar] [CrossRef]
- Qi, D.; Peng, M. Early Hemoglobin Status as a Predictor of Long-Term Mortality for Sepsis Patients in Intensive Care Units. Shock 2021, 55, 215–223. [Google Scholar] [CrossRef]
- Mansur, A.; Mulwande, E.; Steinau, M.; Bergmann, I.; Popov, A.F.; Ghadimi, M.; Beissbarth, T.; Bauer, M.; Hinz, J. Chronic kidney disease is associated with a higher 90-day mortality than other chronic medical conditions in patients with sepsis. Sci. Rep. 2015, 5, 10539. [Google Scholar] [CrossRef]
- Yamamoto, M.; Adachi, H.; Enomoto, M.; Fukami, A.; Nakamura, S.; Nohara, Y.; Sakaue, A.; Morikawa, N.; Hamamura, H.; Toyomasu, K.; et al. Lower albumin levels are associated with frailty measures, trace elements, and an inflammation marker in a cross-sectional study in Tanushimaru. Environ. Health Prev. Med. 2021, 26, 25. [Google Scholar] [CrossRef]
- Muscedere, J.; Waters, B.; Varambally, A.; Bagshaw, S.M.; Boyd, J.G.; Maslove, D.; Sibley, S.; Rockwood, K. The impact of frailty on intensive care unit outcomes: A systematic review and meta-analysis. Intensive Care Med. 2017, 43, 1105–1122. [Google Scholar] [CrossRef]
- Fernando, S.M.; McIsaac, D.I.; Perry, J.J.; Rochwerg, B.; Bagshaw, S.M.; Thavorn, K.; Seely, A.J.E.; Forster, A.J.; Fiest, K.M.; Dave, C.; et al. Frailty and Associated Outcomes and Resource Utilization among Older ICU Patients With Suspected Infection. Crit. Care Med. 2019, 47, e669–e676. [Google Scholar] [CrossRef]
- Meissner, A.; Genga, K.R.; Studart, F.S.; Settmacher, U.; Hofmann, G.; Reinhart, K.; Sakr, Y. Epidemiology of and factors associated with end-of-life decisions in a surgical intensive care unit. Crit. Care Med. 2010, 38, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.T.; Chuang, Y.C.; Tsai, Y.J.; Ko, W.J.; Yu, C.J. High Mortality in Severe Sepsis and Septic Shock Patients with Do-Not-Resuscitate Orders in East Asia. PLoS ONE 2016, 11, e0159501. [Google Scholar] [CrossRef] [PubMed]


| Variables | All Patients (n = 5805) | Survivors (n = 4276) | Non-Survivors (n = 1529) | p Value |
|---|---|---|---|---|
| Age, years | 68.4 ± 13.1 | 67.6 ± 13.1 | 70.7 ± 12.9 | <0.001 |
| Male | 3328 (57.3) | 2402 (56.2) | 926 (60.6) | 0.003 |
| Medical history | ||||
| Hypertension | 2520 (43.4) | 1859 (43.5) | 661 (43.2) | 0.881 |
| Diabetes mellitus | 1945 (33.5) | 1431 (33.5) | 514 (33.6) | 0.925 |
| Cardiac disease | 867 (14.9) | 627 (14.7) | 240 (15.7) | 0.336 |
| Chronic pulmonary disease | 475 (8.2) | 318 (7.4) | 157 (10.3) | 0.001 |
| Malignancy | 1580 (27.2) | 1066 (24.9) | 514 (33.6) | <0.001 |
| Chronic renal disease | 561 (9.7) | 410 (9.6) | 151 (9.9) | 0.762 |
| Liver cirrhosis | 590 (10.2) | 414 (9.7) | 176 (11.5) | 0.043 |
| Cerebrovascular disease | 799 (13.8) | 573 (13.4) | 226 (14.8) | 0.180 |
| Source of infection | ||||
| Pulmonary | 1914 (33.0) | 1186 (27.7) | 728 (47.6) | <0.001 |
| Genitourinary | 1600 (27.6) | 1280 (29.9) | 320 (20.9) | <0.001 |
| Gastrointestinal | 1055 (18.2) | 733 (17.1) | 322 (21.1) | 0.001 |
| Hepatobiliary | 1149 (19.8) | 924 (21.6) | 225 (14.7) | <0.001 |
| Unknown | 367 (6.3) | 263 (6.2) | 104 (6.8) | 0.391 |
| Initial vital signs | ||||
| Systolic blood pressure, mmHg | 99.7 ± 29.7 | 100.2 ± 29.7 | 98.4 ± 29.9 | 0.040 |
| Diastolic blood pressure, mmHg | 59.9 ± 18.6 | 60.0 ± 18.2 | 59.6 ± 19.6 | 0.483 |
| Heart rate, per min | 109.7 ± 25.5 | 109.0 ± 25.2 | 111.5 ± 26.3 | 0.001 |
| Respiratory rate, per min | 21.9 ± 5.7 | 21.3 ± 5.0 | 23.8 ± 6.9 | <0.001 |
| Clinical characteristics | ||||
| Initial SOFA score | 6.4 ± 3.3 | 5.9 ± 3.0 | 8.0 ± 3.4 | <0.001 |
| Variables | All Patients (n = 5805) | Survivors (n = 4276) | Non-Survivors (n = 1529) | p Value |
|---|---|---|---|---|
| White blood cells, ×103/µL | 13.0 ± 18.6 | 12.5 ± 13.7 | 14.4 ± 28.2 | 0.011 |
| Hemoglobin, g/dL | 10.8 ± 2.6 | 10.9 ± 2.5 | 10.4 ± 2.7 | <0.001 |
| Hematocrit, % | 32.7 ± 7.7 | 33.0 ± 7.5 | 31.9 ± 8.3 | <0.001 |
| Platelets, ×103/µL | 164 ± 128 | 167 ± 126 | 154 ± 131 | <0.001 |
| Sodium, mmol/L | 135 ± 7 | 135 ± 6 | 135 ± 8 | 0.012 |
| Potassium, mmol/L | 4.2 ± 0.9 | 4.2 ± 0.8 | 4.4 ± 1.0 | <0.001 |
| Chloride, mmol/L | 100 ± 8 | 100 ± 7 | 100 ± 9 | 0.878 |
| Blood urea nitrogen, mg/dL | 35 ± 24 | 33 ± 22 | 43 ± 27 | <0.001 |
| Creatinine, mg/dL | 1.9 ± 1.8 | 1.8 ± 1.8 | 2.1 ± 1.5 | <0.001 |
| Albumin, g/dL | 3.0 ± 0.7 | 3.1 ± 0.6 | 2.7 ± 0.6 | <0.001 |
| AST, IU/L | 136 ± 520 | 116 ± 485 | 191 ± 599 | <0.001 |
| ALT, IU/L | 77 ± 269 | 74 ± 283 | 83 ± 225 | 0.308 |
| Prothrombin time (INR) | 1.5 ± 0.9 | 1.4 ± 0.8 | 1.6 ± 1.2 | <0.001 |
| C-reactive protein, mg/dL | 16.1 ± 13.6 | 15.4 ± 13.0 | 17.9 ± 15.1 | <0.001 |
| Initial lactate, mmol/L | 4.4 ± 3.3 | 3.8 ± 2.8 | 6.1 ± 4.1 | <0.001 |
| Arterial pH | 7.404 ± 0.117 | 7.421 ± 0.098 | 7.359 ± 0.148 | <0.001 |
| PaCO2 (mmHg) | 29.4 ± 12.2 | 29.0 ± 11.5 | 30.6 ± 14.1 | <0.001 |
| PaO2 (mmHg) | 91.2 ± 45.9 | 89.8 ± 41.6 | 95.0 ± 55.7 | 0.001 |
| Bicarbonate (arterial, mmol/L) | 18.3 ± 6.4 | 18.6 ± 6.3 | 17.2 ± 6.6 | <0.001 |
| Variables | >3.5 (n = 1503) | 3.0~3.5 (n = 1641) | 2.5~3.0 (n = 1538) | 2.0~2.5 (n = 857) | <2.0 (n = 266) |
|---|---|---|---|---|---|
| Age, years | 66.3 ± 14.5 | 69.5 ± 12.3 | 69.0 ± 12.5 | 69.2 ± 12.7 | 67.3 ± 12.2 |
| Male | 894 (59.5) | 905 (55.1) | 888 (57.7) | 479 (55.9) | 162 (60.9) |
| Medical history | |||||
| Hypertension | 657 (43.7) | 759 (46.3) | 640 (41.6) | 356 (41.5) | 108 (40.6) |
| Diabetes mellitus | 497 (33.1) | 571 (34.8) | 487 (31.7) | 296 (34.5) | 94 (35.3) |
| Cardiac disease | 249 (16.6) | 248 (15.1) | 213 (13.8) | 125 (14.6) | 32 (12.0) |
| Chronic pulmonary disease | 134 (8.9) | 136 (8.3) | 129 (8.4) | 58 (6.8) | 18 (6.8) |
| Malignancy | 306 (20.4) | 407 (24.8) | 474 (30.8) | 303 (35.4) | 90 (33.8) |
| Chronic renal disease | 125 (8.3) | 169 (10.3) | 127 (8.3) | 103 (12.0) | 37 (13.9) |
| Liver cirrhosis | 95 (6.3) | 135 (8.2) | 188 (12.2) | 124 (14.5) | 48 (18.0) |
| Laboratory finding | |||||
| Hemoglobin, g/dL | 12.2 ± 2.6 | 11.0 ± 2.4 | 10.2 ± 2.3 | 9.5 ± 2.3 | 9.1 ± 2.3 |
| Platelet, ×103/µL | 180 ± 136 | 170 ± 123 | 156 ± 120 | 149 ± 130 | 128 ± 130 |
| Blood urea nitrogen, mg/dL | 30 ± 21 | 35 ± 22 | 37 ± 25 | 41 ± 27 | 41 ± 26 |
| Creatinine, mg/dL | 1.7 ± 1.5 | 1.9 ± 1.6 | 1.9 ± 2.2 | 1.9 ± 1.5 | 2.0 ± 1.5 |
| C-reactive protein, mg/dL | 12.7 ± 13.1 | 16.6 ± 15.0 | 18.1 ± 13.1 | 17.5 ± 12.6 | 15.6 ± 9.9 |
| Initial lactate, mmol/L | 4.3 ± 3.2 | 4.1 ± 3.2 | 4.4 ± 3.3 | 5.0 ± 3.7 | 5.2 ± 3.8 |
| Variables | Adjusted OR | 95% CI | p Value |
|---|---|---|---|
| Age | 1.019 | 1.013–1.024 | <0.001 |
| Initial lactate | 1.192 | 1.169–1.217 | <0.001 |
| Albumin with SOFA score | 1.162 | 1.135–1.190 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-M.; Ryoo, S.-M.; Shin, T.-G.; Jo, Y.-H.; Kim, K.; Lim, T.-H.; Chung, S.-P.; Choi, S.-H.; Suh, G.-J.; Kim, W.-Y. Early Mortality Stratification with Serum Albumin and the Sequential Organ Failure Assessment Score at Emergency Department Admission in Septic Shock Patients. Life 2024, 14, 1257. https://doi.org/10.3390/life14101257
Kim S-M, Ryoo S-M, Shin T-G, Jo Y-H, Kim K, Lim T-H, Chung S-P, Choi S-H, Suh G-J, Kim W-Y. Early Mortality Stratification with Serum Albumin and the Sequential Organ Failure Assessment Score at Emergency Department Admission in Septic Shock Patients. Life. 2024; 14(10):1257. https://doi.org/10.3390/life14101257
Chicago/Turabian StyleKim, Sang-Min, Seung-Mok Ryoo, Tae-Gun Shin, You-Hwan Jo, Kyuseok Kim, Tae-Ho Lim, Sung-Phil Chung, Sung-Hyuk Choi, Gil-Joon Suh, and Won-Young Kim. 2024. "Early Mortality Stratification with Serum Albumin and the Sequential Organ Failure Assessment Score at Emergency Department Admission in Septic Shock Patients" Life 14, no. 10: 1257. https://doi.org/10.3390/life14101257
APA StyleKim, S.-M., Ryoo, S.-M., Shin, T.-G., Jo, Y.-H., Kim, K., Lim, T.-H., Chung, S.-P., Choi, S.-H., Suh, G.-J., & Kim, W.-Y. (2024). Early Mortality Stratification with Serum Albumin and the Sequential Organ Failure Assessment Score at Emergency Department Admission in Septic Shock Patients. Life, 14(10), 1257. https://doi.org/10.3390/life14101257






