A Systematic Review on the Application of Virtual Reality for Muscular Dystrophy Rehabilitation: Motor Learning Benefits
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Protocol Registration
2.2. Literature Search, Study Selection, and Data Extraction
2.3. Quality Assessment
3. Results
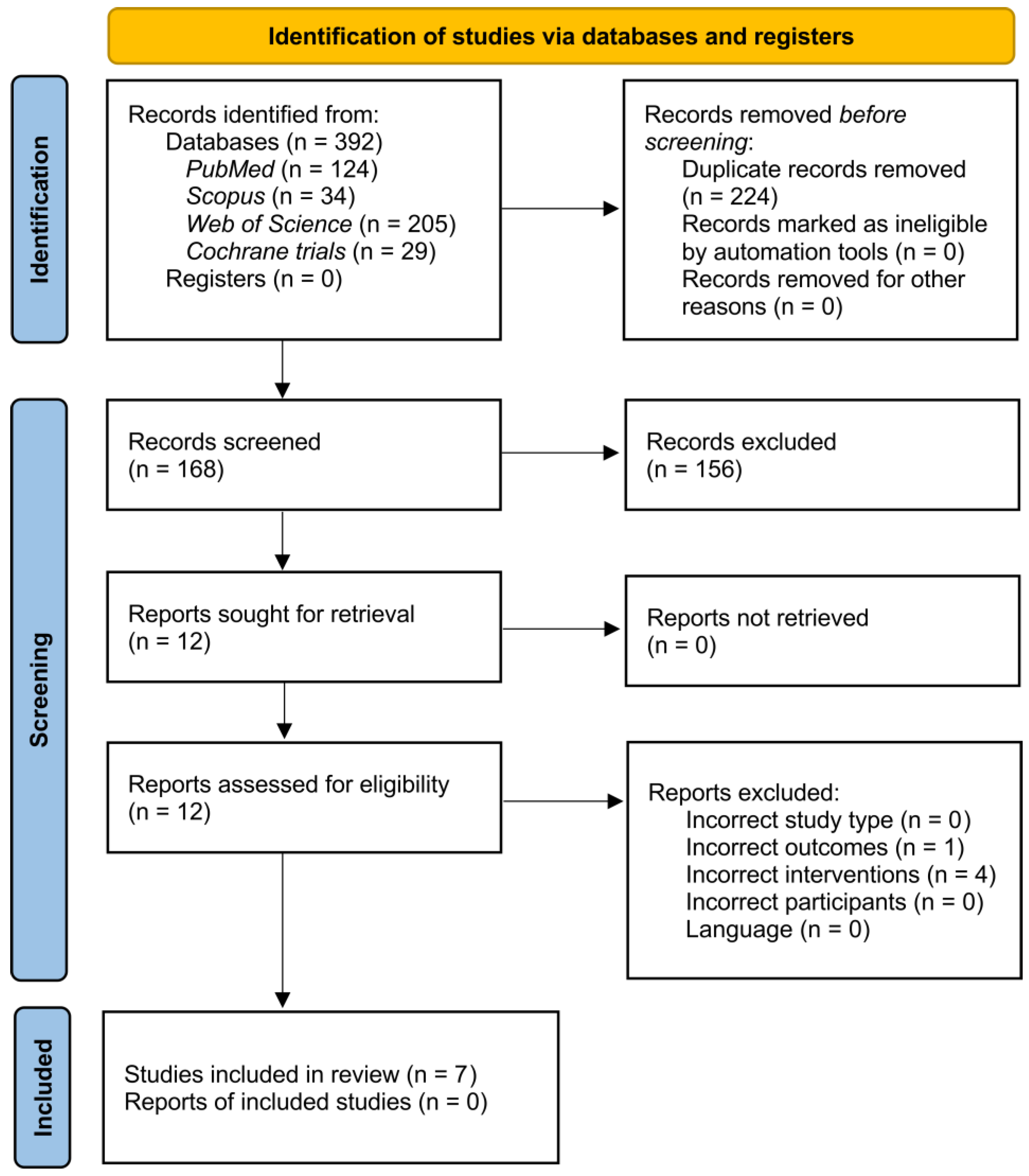
3.1. Result of the Search
3.2. Characteristics of the Included Studies
3.3. Motor Learning
3.4. Effectiveness of VR Intervention
3.5. Risk of Bias
3.6. Meta-Analysis
4. Discussion
4.1. Clinical Implication and Future Study Directions
4.2. Study Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carter, J.C.; Sheehan, D.W.; Prochoroff, A.; Birnkrant, D.J. Muscular Dystrophies. Clin. Chest Med. 2018, 39, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Mah, J.K.; Korngut, L.; Fiest, K.M.; Dykeman, J.; Day, L.J.; Pringsheim, T.; Jette, N. A Systematic Review and Meta-Analysis on the Epidemiology of the Muscular Dystrophies. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2016, 43, 163–177. [Google Scholar] [CrossRef] [PubMed]
- Apkon, S.D.; Alman, B.; Birnkrant, D.J.; Fitch, R.; Lark, R.; Mackenzie, W.; Weidner, N.; Sussman, M. Orthopedic and Surgical Management of the Patient With Duchenne Muscular Dystrophy. Pediatrics 2018, 142, S82–S89. [Google Scholar] [CrossRef] [PubMed]
- Pandey, S.N.; Kesari, A.; Yokota, T.; Pandey, G.S. Muscular Dystrophy: Disease Mechanisms and Therapies. BioMed Res. Int. 2015, 2015, 456348. [Google Scholar] [CrossRef] [PubMed]
- Flanigan, K.M. Duchenne and Becker Muscular Dystrophies. Neurol. Clin. 2014, 32, 671–688. [Google Scholar] [CrossRef] [PubMed]
- Leung, D.G.; Wagner, K.R. Therapeutic Advances in Muscular Dystrophy. Ann. Neurol. 2013, 74, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, S.; Kiper, P.; Cacciante, L.; Cieślik, B.; Mazurek, J.; Turolla, A.; Szczepańska-Gieracha, J. Use of Virtual Reality-Based Training in Different Fields of Rehabilitation: A Systematic Review and Meta-Analysis. J. Rehabil. Med. 2020, 52, jrm00121. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Bonanno, M.; Torregrossa, W.; Cacciante, L.; Celesti, A.; Rifici, C.; Tonin, P.; Luca, R.D.; Quartarone, A. Benefits of Telerehabilitation for Patients With Severe Acquired Brain Injury: Promising Results From a Multicenter Randomized Controlled Trial Using Nonimmersive Virtual Reality. J. Med. Internet Res. 2023, 25, e45458. [Google Scholar] [CrossRef] [PubMed]
- Goffredo, M.; Baglio, F.; De Icco, R.; Proietti, S.; Maggioni, G.; Turolla, A.; Pournajaf, S.; Jonsdottir, J.; Zeni, F.; Federico, S.; et al. Efficacy of Non-Immersive Virtual Reality-Based Telerehabilitation on Postural Stability in Parkinson’s Disease: A Multicenter Randomized Controlled Trial. Eur. J. Phys. Rehabil. Med. 2023, 59, 689–696. [Google Scholar] [CrossRef]
- Rose, T.; Nam, C.S.; Chen, K.B. Immersion of Virtual Reality for Rehabilitation—Review. Appl. Ergon. 2018, 69, 153–161. [Google Scholar] [CrossRef]
- Cieślik, B.; Mazurek, J.; Wrzeciono, A.; Maistrello, L.; Szczepańska-Gieracha, J.; Conte, P.; Kiper, P. Examining Technology-Assisted Rehabilitation for Older Adults’ Functional Mobility: A Network Meta-Analysis on Efficacy and Acceptability. Npj Digit. Med. 2023, 6, 159. [Google Scholar] [CrossRef]
- Verhey, J.T.; Haglin, J.M.; Verhey, E.M.; Hartigan, D.E. Virtual, Augmented, and Mixed Reality Applications in Orthopedic Surgery. Int. J. Med. Robot. Comput. Assist. Surg. MRCAS 2020, 16, e2067. [Google Scholar] [CrossRef] [PubMed]
- Graf, D.L.; Pratt, L.V.; Hester, C.N.; Short, K.R. Playing Active Video Games Increases Energy Expenditure in Children. Pediatrics 2009, 124, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Haddock, B.L.; Brandt, A.M.; Siegel, S.R.; Wilkin, L.D.; Han, J.-K. Active Video Games and Energy Expenditure in Overweight Children. Int. J. Fit. 2008, 4, 17. [Google Scholar]
- Favetta, M.; Romano, A.; Valè, N.; Cieslik, B.; Federico, S.; Girolami, A.; Mazzarotto, D.; Pregnolato, G.; Righetti, A.; Salvalaggio, S.; et al. A Scoping Review of Scientific Concepts Concerning Motor Recovery after Stroke as Employed in Clinical Trials. Front. Neurol. 2023, 14, 1221656. [Google Scholar] [CrossRef]
- Maier, M.; Ballester, B.R.; Verschure, P.F.M.J. Principles of Neurorehabilitation After Stroke Based on Motor Learning and Brain Plasticity Mechanisms. Front. Syst. Neurosci. 2019, 13, 74. [Google Scholar] [CrossRef]
- Jacques, M.F.; Stockley, R.C.; Onambele-Pearson, G.L.; Reeves, N.D.; Stebbings, G.K.; Dawson, E.A.; Groves, L.; Morse, C.I. Quality of Life in Adults with Muscular Dystrophy. Health Qual. Life Outcomes 2019, 17, 121. [Google Scholar] [CrossRef]
- Angelini, C.; Marozzo, R.; Pegoraro, V. Current and Emerging Therapies in Becker Muscular Dystrophy (BMD). Acta Myol. Myopathies Cardiomyopathies Off. J. Mediterr. Soc. Myol. 2019, 38, 172–179. [Google Scholar]
- Case, L.E.; Apkon, S.D.; Eagle, M.; Gulyas, A.; Juel, L.; Matthews, D.; Newton, R.A.; Posselt, H.F. Rehabilitation Management of the Patient With Duchenne Muscular Dystrophy. Pediatrics 2018, 142, S17–S33. [Google Scholar] [CrossRef]
- Meyns, P.; Roman de Mettelinge, T.; van der Spank, J.; Coussens, M.; Van Waelvelde, H. Motivation in Pediatric Motor Rehabilitation: A Systematic Search of the Literature Using the Self-Determination Theory as a Conceptual Framework. Dev. Neurorehabil. 2018, 21, 371–390. [Google Scholar] [CrossRef]
- Howard, M.C. A Meta-Analysis and Systematic Literature Review of Virtual Reality Rehabilitation Programs. Comput. Hum. Behav. 2017, 70, 317–327. [Google Scholar] [CrossRef]
- Baeza-Barragán, M.R.; Manzanares, M.T.L.; Vergara, C.R.; Casuso-Holgado, M.J.; Martín-Valero, R. The Use of Virtual Reality Technologies in the Treatment of Duchenne Muscular Dystrophy: Systematic Review. JMIR MHealth UHealth 2020, 8, e21576. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Rathbone, J.; Carter, M.; Hoffmann, T.; Glasziou, P. Better Duplicate Detection for Systematic Reviewers: Evaluation of Systematic Review Assistant-Deduplication Module. Syst. Rev. 2015, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Guimarães, N.S.; Ferreira, A.J.F.; Ribeiro Silva, R.D.C.; de Paula, A.A.; Lisboa, C.S.; Magno, L.; Ichiara, M.Y.; Barreto, M.L. Deduplicating Records in Systematic Reviews: There Are Free, Accurate Automated Ways to Do So. J. Clin. Epidemiol. 2022, 152, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, A.P.; de Vet, H.C.; de Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi List: A Criteria List for Quality Assessment of Randomized Clinical Trials for Conducting Systematic Reviews Developed by Delphi Consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef] [PubMed]
- van Tulder, M.; Furlan, A.; Bombardier, C.; Bouter, L. Editorial Board of the Cochrane Collaboration Back Review Group Updated Method Guidelines for Systematic Reviews in the Cochrane Collaboration Back Review Group. Spine 2003, 28, 1290–1299. [Google Scholar] [CrossRef] [PubMed]
- Herrador Colmenero, L.; Perez Marmol, J.M.; Martí-García, C.; Querol Zaldivar, M.D.L.Á.; Tapia Haro, R.M.; Castro Sánchez, A.M.; Aguilar-Ferrándiz, M.E. Effectiveness of Mirror Therapy, Motor Imagery, and Virtual Feedback on Phantom Limb Pain Following Amputation: A Systematic Review. Prosthet. Orthot. Int. 2018, 42, 288–298. [Google Scholar] [CrossRef]
- Capelini, C.M.; da Silva, T.D.; Tonks, J.; Watson, S.; Alvarez, M.P.B.; de Menezes, L.D.C.; Favero, F.M.; Caromano, F.A.; Massetti, T.; de Mello Monteiro, C.B. Improvements in Motor Tasks through the Use of Smartphone Technology for Individuals with Duchenne Muscular Dystrophy. Neuropsychiatr. Dis. Treat. 2017, 13, 2209–2217. [Google Scholar] [CrossRef]
- da Silva, T.D.; Ribeiro-Papa, D.C.; Coe, S.; Malheiros, S.R.P.; Massetti, T.; Meira Junior, C.D.M.; Nicolai Ré, A.H.; Collett, J.; Monteiro, C.B.D.M.; Dawes, H. Evaluation of Speed-Accuracy Trade-off in a Computer Task to Identify Motor Difficulties in Individuals with Duchenne Muscular Dystrophy—A Cross-Sectional Study. Res. Dev. Disabil. 2020, 96, 103541. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, B.; Da Silva, T.; Crocetta, T.; Massetti, T.; De Araujo, L.; Coe, S.; Dawes, H.; Caromano, F.; De Mello Monteiro, C. Analysis of Different Device Interactions in a Virtual Reality Task in Individuals with Duchenne Muscular Dystrophy-a Randomized Controlled Trial. Front. Neurol. 2019, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Quadrado, V.H.; da Silva, T.D.; Favero, F.M.; Tonks, J.; Massetti, T.; Monteiro, C.B.D.M. Motor Learning from Virtual Reality to Natural Environments in Individuals with Duchenne Muscular Dystrophy. Disabil. Rehabil. Assist. Technol. 2019, 14, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Malheiros, S.R.P.; da Silva, T.D.; Favero, F.M.; de Abreu, L.C.; Fregni, F.; Ribeiro, D.C.; de Mello Monteiro, C.B. Computer Task Performance by Subjects with Duchenne Muscular Dystrophy. Neuropsychiatr. Dis. Treat. 2016, 12, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Massetti, T.; Fávero, F.; Menezes, L.; Alvarez, M.; Crocetta, T.; Guarnieri, R.; Nunes, F.; Monteiro, C.; Silva, T. Achievement of Virtual and Real Objects Using a Short-Term Motor Learning Protocol in People with Duchenne Muscular Dystrophy: A Crossover Randomized Controlled Trial. Games Health J. 2018, 7, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Heutinck, L.; Jansen, M.; van den Elzen, Y.; van der Pijl, D.; de Groot, I. Virtual Reality Computer Gaming with Dynamic Arm Support in Boys with Duchenne Muscular Dystrophy. J. Neuromuscul. Dis. 2018, 5, 359–372. [Google Scholar] [CrossRef]
- Nakafuji, A.; Tsuji, K. Learning and Transfer in Two Perceptual-Motor Skills in Duchenne Muscular Dystrophy. Percept. Mot. Skills 2001, 93, 339–352. [Google Scholar] [CrossRef] [PubMed]
- Levac, D.E.; Huber, M.E.; Sternad, D. Learning and Transfer of Complex Motor Skills in Virtual Reality: A Perspective Review. J. Neuroeng. Rehabil. 2019, 16, 121. [Google Scholar] [CrossRef]
- Benzing, V.; Schmidt, M. Exergaming for Children and Adolescents: Strengths, Weaknesses, Opportunities and Threats. J. Clin. Med. 2018, 7, 422. [Google Scholar] [CrossRef]
- Wenk, N.; Penalver-Andres, J.; Buetler, K.A.; Nef, T.; Müri, R.M.; Marchal-Crespo, L. Effect of Immersive Visualization Technologies on Cognitive Load, Motivation, Usability, and Embodiment. Virtual Real. 2023, 27, 307–331. [Google Scholar] [CrossRef]
| Author (Year) | Study Design | N | Group Characteristics (Mean Age; tMFM) | Interventions | Outcomes | Conclusions |
|---|---|---|---|---|---|---|
| Motor learning | ||||||
| da Silva et al. (2020) [31] | Cross-sectional study | G1: 17 G2: 17 | G1: DMD (15.4 years; tMFM: 46.6) G2: TD (15.4 years) | Computerized Discrete Aiming Task (v.1.0) (total 12 trials) | Movement time, Vignos scale | Tasks that require accuracy should predominately be used in DMD daily activities in order to keep them engaged in social participation. |
| De Freitas et al. (2019) [32] | RCT | G1: 60 G2: 60 | G1: DMD (16.0 years; tMFM: 54.4) G2: TD (16.0 years) | Upper extremity dexterity computer game using 3 different conditions: Leap Motion, Kinect and Touch Screen | Vignos scale, Acquisition, Retention, Transfer | A device with no contact (Leap Motion) facilitated the successful implementation of the proposed task. Therefore, an improvement in performance when using a virtual interface requiring no physical contact for individuals with DMD. |
| Massetti et al. (2018) [35] | RCT with crossover | G1: 11 G2: 11 | G1: DMD (14.8 years; tMFM: 49.8) G2: DMD (16.8 years; tMFM: 55.7) | G1: Virtual task with MoVER software and Kinect sensor G2: Real task with Kinect sensor (total 40 trials) | MFM, Movement time, Acquisition, Retention, Transfer | Both virtual and real tasks promoted improvement of performance, although performance of participants in the real task was better than that in the virtual one. |
| Capelini et al. (2017) [30] | Two arm study | G1: 50 G2: 50 | G1: DMD (17.2 years; tMFM: 48.5) G2: TD (17.3 years) | Moving a virtual ball in virtual maze in smartphone game (total 45 trials) | EK, Vignos scale, Acquisition, Retention Transfer | Practice of a visual motor task in mobile game promoted improvement in performance during the acquisition of the game in groups with DMD and TD. |
| Quadrado et al. (2019) [33] | Two arm study | G1: 32 G2: 32 | G1: DMD (18.0 years tMFM: NS) G2: TD (18.0 years) | Upper extremity dexterity computer game with motion capture device and computer keyboard (total 35 trials) | Movement time, Acquisition, Retention, Transfer | Individuals with DMD, conducting a coincidence timing task in a virtual environment facilitated transfer to the real environment. |
| Malheiros et al. (2016) [34] | Two arm study | G1: 42 G2: 42 | G1: DMD (18.1 years; tMFM: 43.2) G2: TD (18.1 years) | Virtual maze in computer game (total 30 trials) | Movement time, Acquisition, Retention, Transfer | Intervention improved in computational task performance among participants with DMD following practice. Difference in movement time was observed in all attempts among individuals from both groups. |
| VR intervention efficacy | ||||||
| Heutinck et al. (2018) [36] | explorative RCT | G1: 7 G2: 9 | G1: DMD (12.9 years; tMFM: NS) G2: DMD (12.6 years tMFM: NS) | G1: Games with motion capture and gravity compensation for the arms (five 15 min sessions a week for 20 weeks) G2: Usual care | PUL, QMUS, A6MCT, MFM, Global Health Question, Kidscreen-52 | Study did not show a significant effect of training on the primary outcome measure, and there were indications that training may decline the loss of range of motion and strength. |
| Author (Year) | (1) * | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | Tot. | IVS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| da Silva et al. (2020) [31] | X | X | X | X | X | X | 5/10 | 2/7 | |||||
| De Freitas et al. (2019) [32] | X | X | X | X | X | X | X | 6/10 | 3/7 | ||||
| Heutinck et al. (2018) [36] | X | X | X | X | X | 5/10 | 2/7 | ||||||
| Massetti et al. (2018) [35] | X | X | X | X | X | X | X | X | 7/10 | 4/7 | |||
| Capelini et al. (2017) [30] | X | X | X | X | X | X | X | 6/10 | 3/7 | ||||
| Quadrado et al. (2019) [33] | X | X | X | X | X | X | X | X | 7/10 | 4/7 | |||
| Malheiros et al. (2016) [34] | X | X | X | X | X | X | 5/10 | 2/7 | |||||
| %, X | 86 | 71 | 29 | 100 | 0 | 0 | 14 | 86 | 86 | 100 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiper, P.; Federico, S.; Szczepańska-Gieracha, J.; Szary, P.; Wrzeciono, A.; Mazurek, J.; Luque-Moreno, C.; Kiper, A.; Spagna, M.; Barresi, R.; et al. A Systematic Review on the Application of Virtual Reality for Muscular Dystrophy Rehabilitation: Motor Learning Benefits. Life 2024, 14, 790. https://doi.org/10.3390/life14070790
Kiper P, Federico S, Szczepańska-Gieracha J, Szary P, Wrzeciono A, Mazurek J, Luque-Moreno C, Kiper A, Spagna M, Barresi R, et al. A Systematic Review on the Application of Virtual Reality for Muscular Dystrophy Rehabilitation: Motor Learning Benefits. Life. 2024; 14(7):790. https://doi.org/10.3390/life14070790
Chicago/Turabian StyleKiper, Pawel, Sara Federico, Joanna Szczepańska-Gieracha, Patryk Szary, Adam Wrzeciono, Justyna Mazurek, Carlos Luque-Moreno, Aleksandra Kiper, Mattia Spagna, Rita Barresi, and et al. 2024. "A Systematic Review on the Application of Virtual Reality for Muscular Dystrophy Rehabilitation: Motor Learning Benefits" Life 14, no. 7: 790. https://doi.org/10.3390/life14070790
APA StyleKiper, P., Federico, S., Szczepańska-Gieracha, J., Szary, P., Wrzeciono, A., Mazurek, J., Luque-Moreno, C., Kiper, A., Spagna, M., Barresi, R., & Cieślik, B. (2024). A Systematic Review on the Application of Virtual Reality for Muscular Dystrophy Rehabilitation: Motor Learning Benefits. Life, 14(7), 790. https://doi.org/10.3390/life14070790









