Pilot Study of Home-Based Virtual Reality Fitness Training in Post-Discharge Rehabilitation for Patients with Spinal Cord Injury: A Randomized Double-Blind Multicenter Trial
Abstract
:1. Introduction
2. Methods
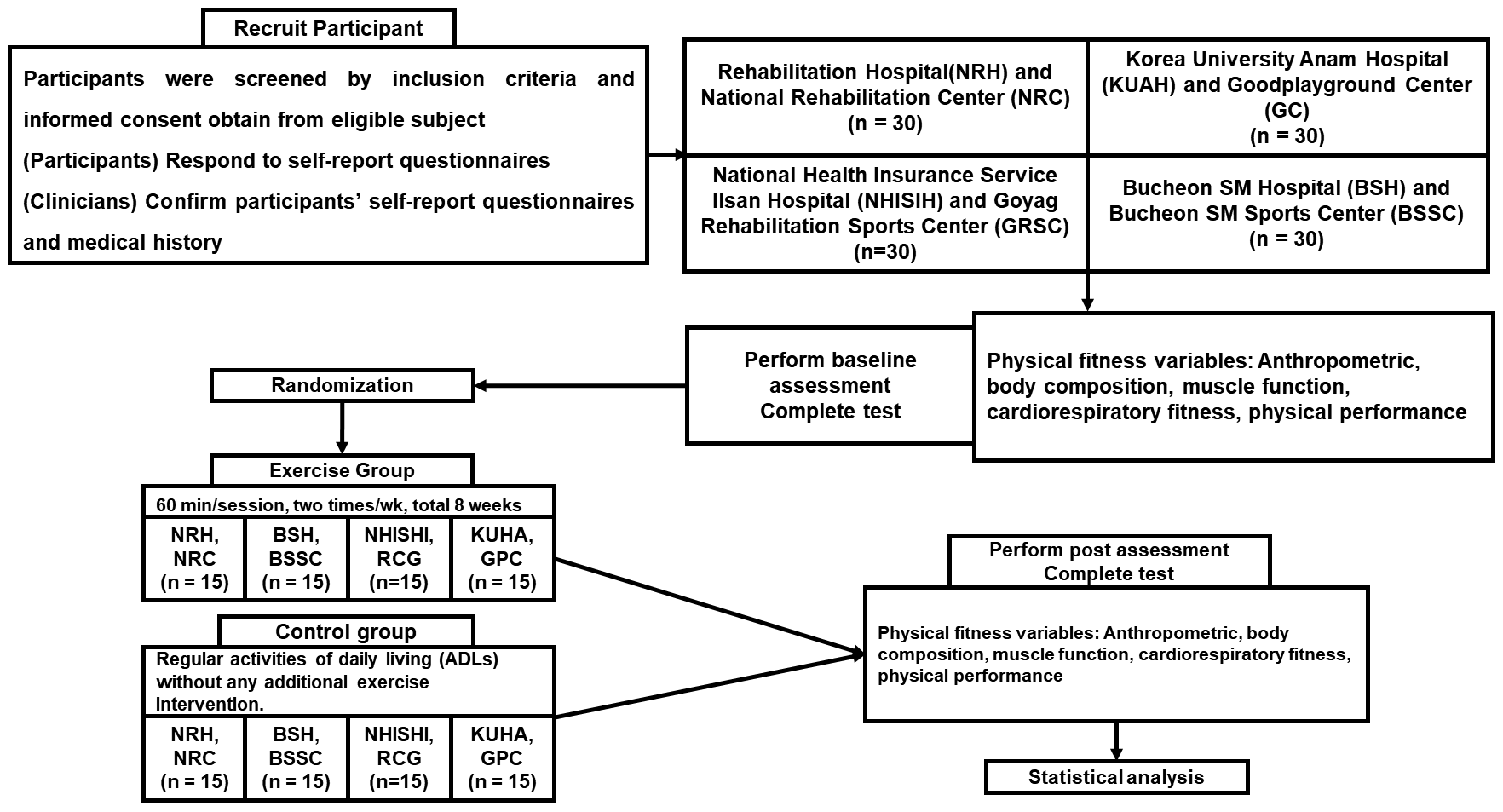
2.1. Experimental Design
2.2. Participants
2.3. Randomization
2.4. Random Assignment
2.5. Protocol
2.6. Program
2.7. Measures
2.7.1. Muscle Function
2.7.2. Cardiopulmonary Fitness
2.7.3. Physical Performance
2.7.4. Body Composition
2.7.5. Quality of Life
2.8. Participant Timeline
2.9. Data Collection Methods and Analysis
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singh, A.; Tetreault, L.; Kalsi-Ryan, S.; Nouri, A.; Fehlings, M.G. Global prevalence and incidence of traumatic spinal cord injury. Clin. Epidemiol. 2014, 6, 309–331. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.B.; Cripps, R.A.; Fitzharris, M.; Wing, P.C. The global map for traumatic spinal cord injury epidemiology: Update 2011, global incidence rate. Spinal Cord 2014, 52, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Furlan, J.C.; Sakakibara, B.M.; Miller, W.C.; Krassioukov, A.V. Global incidence and prevalence of traumatic spinal cord injury. Can. J. Neurol. Sci. 2013, 40, 456–464. [Google Scholar] [CrossRef] [PubMed]
- New, P.W.; Sundararajan, V. Incidence of non-traumatic spinal cord injury in Victoria, Australia: A population-based study and literature review. Spinal Cord 2008, 46, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Shin, H. Etiology and epidemiology of spinal cord injury in Korea. J. Korean Med. Assoc. 2020, 63, 589–595. [Google Scholar] [CrossRef]
- Curt, A.; Van Hedel, H.J.; Klaus, D.; Dietz, V. Recovery from a spinal cord injury: Significance of compensation, neural plasticity, and repair. J. Neurotrauma 2008, 25, 677–685. [Google Scholar] [CrossRef] [PubMed]
- Dietz, V.; Fouad, K. Restoration of sensorimotor functions after spinal cord injury. Brain 2014, 137, 654–667. [Google Scholar] [CrossRef] [PubMed]
- Elbasiouny, S.M.; Moroz, D.; Bakr, M.M.; Mushahwar, V.K. Management of spasticity after spinal cord injury: Current techniques and future directions. Neurorehabil. Neural Repair. 2010, 24, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Tetreault, L.A.; Wilson, J.R.; Kwon, B.K.; Burns, A.S.; Martin, A.R.; Hawryluk, G.; Harrop, J.S. A clinical practice guideline for the management of acute spinal cord injury: Introduction, rationale, and scope. Glob. Spine J. 2017, 7, 84S–94S. [Google Scholar] [CrossRef]
- Kirshblum, S.C.; Burns, S.P.; Biering-Sørensen, F.; Donovan, W.; Graves, D.E.; Jha, A.; Waring, W. International standards for neurological classification of spinal cord injury (revised 2011). J. Spinal Cord Med. 2011, 34, 535–546. [Google Scholar] [CrossRef]
- Hicks, A.L.; Martin, K.A.; Ditor, D.S.; Latimer, A.E.; Maher, J.L.; McCartney, N.; Phillips, S.M. Long-term exercise training in persons with spinal cord injury: Effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003, 41, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Van Hedel, H.J.A.; Dietz, V. Rehabilitation of locomotion after spinal cord injury. Restor. Neurol. Neurosci. 2010, 28, 123–134. [Google Scholar] [CrossRef] [PubMed]
- Dallmeijer, A.J.; van der Woude, L.H. Health related functional status in men with spinal cord injury: Relationship with lesion level and endurance capacity. Spinal Cord 2001, 39, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Nooijen, C.F.; Stam, H.J.; Sluis, T.; Valent, L.; Twisk, J.; Van Den Berg-Emons, R.J. A behavioral intervention promoting physical activity in people with subacute spinal cord injury: Secondary effects on health, social participation and quality of life. Clin. Rehabil. 2017, 31, 772–780. [Google Scholar] [CrossRef] [PubMed]
- Latimer, A.E.; Martin Ginis, K.A.; Arbour, K.P. The efficacy of an implementation intention intervention for promoting physical activity among individuals with spinal cord injury: A randomized controlled trial. Rehabil. Psychol. 2006, 51, 273. [Google Scholar] [CrossRef]
- De Araújo, A.V.L.; Neiva, J.F.D.O.; Monteiro, C.B.D.M.; Magalhães, F.H. Efficacy of virtual reality rehabilitation after spinal cord injury: A systematic review. BioMed Res. Int. 2019, 2019, 7106951. [Google Scholar] [CrossRef]
- Asadzadeh, A.; Samad-Soltani, T.; Salahzadeh, Z.; Rezaei-Hachesu, P. Effectiveness of virtual reality-based exercise therapy in rehabilitation: A scoping review. Inform. Med. Unlocked 2021, 24, 100562. [Google Scholar] [CrossRef]
- Vibhuti; Kumar, N.; Kataria, C. Efficacy assessment of virtual reality therapy for neuromotor rehabilitation in home environment: A systematic review. Disabil. Rehabil. Assist. Technol. 2023, 18, 1200–1220. [Google Scholar] [CrossRef]
- De Miguel-Rubio, A.; Rubio, M.D.; Alba-Rueda, A.; Salazar, A.; Moral-Munoz, J.A.; Lucena-Anton, D. Virtual reality systems for upper limb motor function recovery in patients with spinal cord injury: Systematic review and meta-analysis. JMIR mHealth uHealth 2020, 8, e22537. [Google Scholar] [CrossRef]
- Costa, M.T.S.; Vieira, L.P.; de Oliveira Barbosa, E.; Oliveira, L.M.; Maillot, P.; Vaghetti, C.A.O.; Monteiro-Junior, R.S. Virtual reality-based exercise with exergames as medicine in different contexts: A short review. Clin. Pract. Epidemiol. Ment. Health 2019, 15, 15. [Google Scholar] [CrossRef]
- Rutkowski, S.; Kiper, P.; Cacciante, L.; Cieslik, B.; Mazurek, J.; Turolla, A.; Szczepanska-Gieracha, J. Use of virtual reality-based training in different fields of rehabilitation: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Park, J.; Eun, S.D. Home-based virtual reality exergame program after stroke rehabilitation for patients with stroke: A study protocol for a multicenter, randomized controlled trial. Life 2023, 13, 2256. [Google Scholar] [CrossRef] [PubMed]
- De Miguel-Rubio, A.; Rubio, M.D.; Salazar, A.; Camacho, R.; Lucena-Anton, D. Effectiveness of virtual reality on functional performance after spinal cord injury: A systematic review and meta-analysis of randomized controlled trials. J. Clin. Med. 2020, 9, 2065. [Google Scholar] [CrossRef] [PubMed]
- Sweet, S.N.; Rocchi, M.; Arbour-Nicitopoulos, K.; Kairy, D.; Fillion, B. A telerehabilitation approach to enhance quality of life through exercise among adults with paraplegia: Study protocol. JMIR Res. Protoc. 2017, 6, e8047. [Google Scholar] [CrossRef] [PubMed]
- Touchett, H.; Apodaca, C.; Siddiqui, S.; Huang, D.; Helmer, D.A.; Lindsay, J.A.; Skelton, F. Current approaches in telehealth and telerehabilitation for spinal cord injury (TeleSCI). Curr. Phys. Med. Rehabil. Rep. 2022, 10, 77–88. [Google Scholar] [CrossRef]
- Chemtob, K.; Rocchi, M.; Arbour-Nicitopoulos, K.; Kairy, D.; Fillion, B.; Sweet, S.N. Using tele-health to enhance motivation, leisure time physical activity, and quality of life in adults with spinal cord injury: A self-determination theory-based pilot randomized control trial. Psychol. Sport Exerc. 2019, 43, 243–252. [Google Scholar] [CrossRef]
- Solomon, R.M.; Dhakal, R.; Halpin, S.J.; Hariharan, R.; O’Connor, R.J.; Allsop, M.; Sivan, M. Telerehabilitation for individuals with spinal cord injury in low-and middle-income countries: A systematic review of the literature. Spinal Cord 2022, 60, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Rupp, R.; Biering-Sørensen, F.; Burns, S.P.; Graves, D.E.; Guest, J.; Jones, L.; Kirshblum, S. International standards for neurological classification of spinal cord injury: Revised 2019. Top. Spinal Cord Inj. Rehabil. 2021, 27, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.W.; Tetzlaff, J.M.; Altman, D.G.; Laupacis, A.; Gøtzsche, P.C.; Krleža-Jerić, K.; Hróbjartsson, A.; Mann, H.; Dickersin, K.; Berlin, J.A.; et al. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Ann. Intern. Med. 2013, 158, 200–207. [Google Scholar] [CrossRef]
- Koivisto, J.; Hamari, J. The rise of motivational information systems: A review of gamification research. Int. J. Inf. Manag. 2019, 45, 191–210. [Google Scholar] [CrossRef]
- Tuan, S.H.; Chang, L.H.; Sun, S.F.; Lin, K.L.; Tsai, Y.J. Using exergame-based exercise to prevent and postpone the loss of muscle mass, muscle strength, cognition, and functional performance among elders in rural long-term care facilities: A protocol for a randomized controlled trial. Front. Med. 2022, 9, 1071409. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Hassan, L.; Buruk, O.; Nummenmaa, T.; Peltonen, J. ‘Switch’ up your exercise: An empirical analysis of online user discussion of the ring fit adventure exergame. In Proceedings of the 5th International GamiFIN Conference, Levi, Finland, 7–9 April 2021. [Google Scholar]
- Williams, N. The Borg Rating of Perceived Exertion (RPE) scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Adams, J.; Lai, B.; Rimmer, J.; Powell, D.; Yarar-Fisher, C.; Oster, R.A.; Fisher, G. Telehealth high-intensity interval exercise and cardiometabolic health in spinal cord injury. Trials 2022, 23, 633. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, M.S.; Younesian, A. Lipid profiles are influenced by arm cranking exercise and training in individuals with spinal cord injury. Spinal Cord 2005, 43, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Kang, D.; Eun, S.D. Development and pilot testing of novel game-based respiratory rehabilitation exercise devices for patients with tetraplegia. Technol. Health Care 2021, 29, 1119–1127. [Google Scholar] [CrossRef]
- Kang, D.; Park, J.; Eun, S.D. A preliminary study on the feasibility of community game-based respiratory muscle training for individuals with high cervical spinal cord injury levels: A novel approach. BMC Sports Sci. Med. Rehabil. 2022, 14, 137. [Google Scholar] [CrossRef] [PubMed]
- Arsh, A.; Darain, H.; Rahman, M.U.; Ullah, I.; Shakil-Ur-Rehman, S. Reliability of modified functional reach test in the assessment of balance function in people with spinal cord injury: A systematic review. JPMA J. Pak. Med. Assoc. 2021, 71, 2040–2044. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A.G. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Harkema, S.; MacKay-Lyons, M. Best practices for the management of individuals with spinal cord injury. J. Rehabil. Res. Dev. 2013, 50, 1–20. [Google Scholar] [CrossRef]
- Van Schaik, P.; Blake, J.; Pernet, F.; Spears, I.; Fencott, C. Virtual augmented exercise gaming for older adults. Cyberpsychol. Behav. 2008, 11, 103–106. [Google Scholar] [CrossRef]
- Sarupuri, B.; Kulpa, R.; Aristidou, A.; Multon, F. Dancing in virtual reality as an inclusive platform for social and physical fitness activities: A survey. Vis. Comput. 2024, 40, 4055–4070. [Google Scholar] [CrossRef]
- Tharu, N.S.; Wong, A.Y.L.; Zheng, Y.P. Neuromodulation for recovery of trunk and sitting functions following spinal cord injury: A comprehensive review of the literature. Bioelectron. Med. 2023, 9, 11. [Google Scholar] [CrossRef]
- Holden, M.K. Virtual environments for motor rehabilitation. Cyberpsychol. Behav. 2005, 8, 187–211. [Google Scholar] [CrossRef] [PubMed]

| Warm-Up/Cool-Down | Upper Extremities | Trunk | |
|---|---|---|---|
| Aerobic | Flexibility | ||
| Freewheeling |
|
|
|
| Medical Part | Age | Years |
| Gender | Male or female | |
| American Spinal Injury Association (ASIA) level | A, B, C, D, E | |
| Hypertension, anemia, dyspnea or asthma, orthostatic hypotension, diabetes, medications for heart disease, coronary stent, epilepsy, medications for anticoagulants, medications for depression, rigidity, autonomic dysreflexia, bladder management, bowel care, pressure ulcer, acute low back pain within 4 weeks, joint pain, medications for osteoporosis, hip or femur fractures | Yes or no | |
| Anthropometric Part | Blood pressure | mmHg |
| Height | cm | |
| Weight | kg | |
| Body mass index | Underweight/normal weight/overweight | |
| Days of discharge from the hospital | Number of days |
| Study Period | ||||
|---|---|---|---|---|
| Enrollment | Allocation | Post-Allocation | Closeout | |
| Timepoint, baseline | t | 0 | T16 | tx |
| Enrollment | ||||
| Eligibility screening | X | |||
| Informed consent | X | |||
| (Participant) Self-report questionnaires | X | |||
| (Clinicians) Confirm participants’ self-report questionnaires and medical history and write doctor’s notes | X | |||
| Allocation | X | |||
| Assessments | ||||
| Baseline variables | X | |||
| Post-intervention variables | X | X | ||
| Intervention | ||||
| Experimental group | X | X | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, D.; Eun, S.-D.; Park, J. Pilot Study of Home-Based Virtual Reality Fitness Training in Post-Discharge Rehabilitation for Patients with Spinal Cord Injury: A Randomized Double-Blind Multicenter Trial. Life 2024, 14, 859. https://doi.org/10.3390/life14070859
Kang D, Eun S-D, Park J. Pilot Study of Home-Based Virtual Reality Fitness Training in Post-Discharge Rehabilitation for Patients with Spinal Cord Injury: A Randomized Double-Blind Multicenter Trial. Life. 2024; 14(7):859. https://doi.org/10.3390/life14070859
Chicago/Turabian StyleKang, Dongheon, Seon-Deok Eun, and Jiyoung Park. 2024. "Pilot Study of Home-Based Virtual Reality Fitness Training in Post-Discharge Rehabilitation for Patients with Spinal Cord Injury: A Randomized Double-Blind Multicenter Trial" Life 14, no. 7: 859. https://doi.org/10.3390/life14070859







