Is It the Best Option? Robotic Surgery for Endometriosis
Abstract
1. Introduction
2. Brief History of the Development of Robotic Surgery
3. Current Application and Outcomes on Endometriosis
3.1. Comparison of Surgical Outcomes
3.2. Fertility Preservation or Residual Ovarian Function
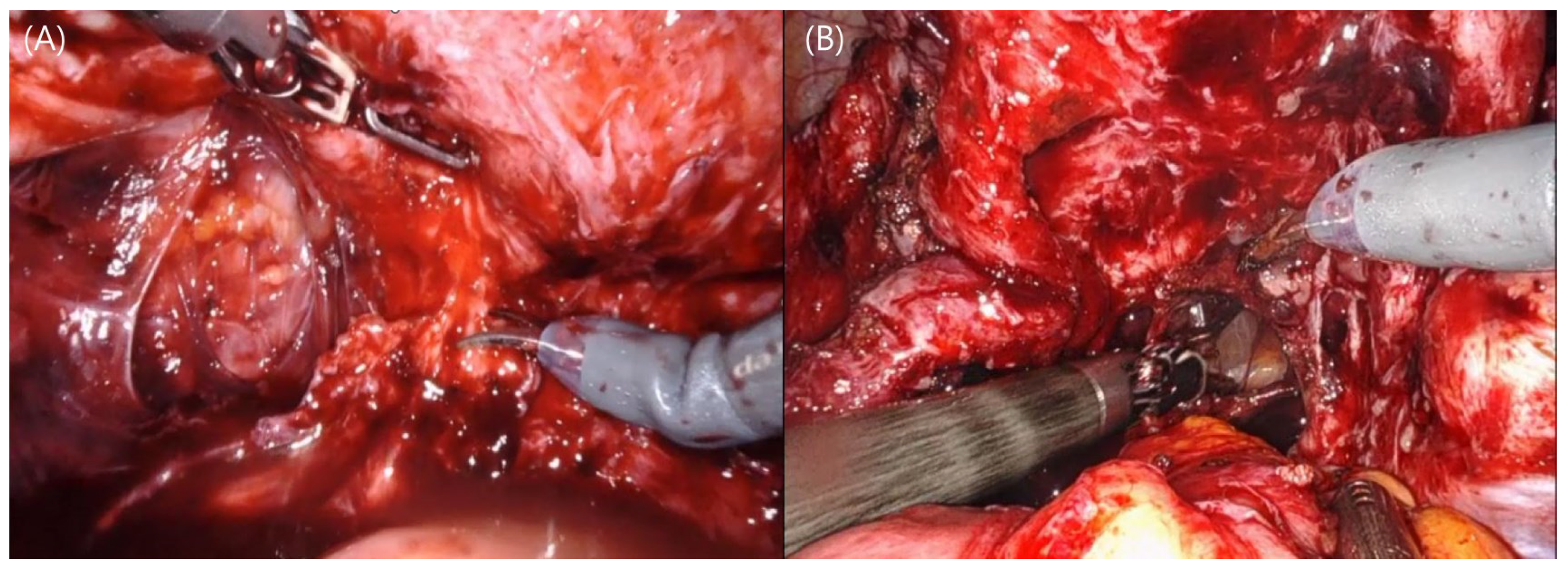
3.3. Robotic Systems and Deep Infiltrating Endometriosis
4. Clinical Benefits of Robotic Surgery
4.1. Precision, Accuracy, and Ergonomics
4.2. Reduced Surgeon Fatigue
4.3. Fast Learning Curve
4.4. Utilization of Single-Site Surgery
5. Limitations and Challenges
5.1. Absence of Tactile Sense, Forced Feedback
5.2. Accessibility and Availability
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Allaire, C.; Bedaiwy, M.A.; Yong, P.J. Diagnosis and management of endometriosis. CMAJ 2023, 195, E363–E371. [Google Scholar] [CrossRef]
- Westwood, S.; Fannin, M.; Ali, F.; Thigpen, J.; Tatro, R.; Hernandez, A.; Peltzer, C.; Hildebrand, M.; Fernandez-Pacheco, A.; Raymond-Lezman, J.R.; et al. Disparities in Women with Endometriosis Regarding Access to Care, Diagnosis, Treatment, and Management in the United States: A Scoping Review. Cureus 2023, 15, e38765. [Google Scholar] [CrossRef]
- Warzecha, D.; Szymusik, I.; Wielgos, M.; Pietrzak, B. The Impact of Endometriosis on the Quality of Life and the Incidence of Depression-A Cohort Study. Int. J. Env. Res. Public Health 2020, 17, 3641. [Google Scholar] [CrossRef] [PubMed]
- Kalaitzopoulos, D.R.; Samartzis, N.; Kolovos, G.N.; Mareti, E.; Samartzis, E.P.; Eberhard, M.; Dinas, K.; Daniilidis, A. Treatment of endometriosis: A review with comparison of 8 guidelines. BMC Womens Health 2021, 21, 397. [Google Scholar] [CrossRef]
- Rimbach, S.; Ulrich, U.; Schweppe, K.W. Surgical Therapy of Endometriosis: Challenges and Controversies. Geburtshilfe Frauenheilkd. 2013, 73, 918–923. [Google Scholar] [CrossRef]
- Cho, A.; Park, C.M. Minimally invasive surgery for deep endometriosis. Obs. Gynecol. Sci. 2024, 67, 49–57. [Google Scholar] [CrossRef]
- Cela, V.; Obino, M.E.; Sergiampietri, C.; Simi, G.; Papini, F.; Pinelli, S.; Freschi, L.; Artini, P. The role of robotics in the management of endometriosis. Minerva Ginecol. 2017, 69, 504–516. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Sanjay, M.; Rupa, B.; Kumari, S. Robotic surgery in gynecology. J. Minim. Access Surg. 2015, 11, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Bramhe, S.; Pathak, S.S. Robotic Surgery: A Narrative Review. Cureus 2022, 14, e29179. [Google Scholar] [CrossRef]
- Reddy, K.; Gharde, P.; Tayade, H.; Patil, M.; Reddy, L.S.; Surya, D. Advancements in Robotic Surgery: A Comprehensive Overview of Current Utilizations and Upcoming Frontiers. Cureus 2023, 15, e50415. [Google Scholar] [CrossRef]
- Ngu, J.C.; Tsang, C.B.; Koh, D.C. The da Vinci Xi: A review of its capabilities, versatility, and potential role in robotic colorectal surgery. Robot. Surg. 2017, 4, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Kwak, Y.H.; Lee, H.; Seon, K.; Lee, Y.J.; Lee, Y.J.; Kim, S.W. Da Vinci SP Single-Port Robotic Surgery in Gynecologic Tumors: Single Surgeon’s Initial Experience with 100 Cases. Yonsei Med. J. 2022, 63, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.C.; Slack, M.; Hussain, M.; Barber, N.; Pradhan, A.; Dinneen, E.; Stewart, G.D. Preclinical Evaluation of the Versius Surgical System, a New Robot-assisted Surgical Device for Use in Minimal Access Renal and Prostate Surgery. Eur. Urol. Focus 2021, 7, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Ngu, J.; Lin, C.; Sia, C.; Teo, N.-Z. A narrative review of the Medtronic Hugo RAS and technical comparison with the Intuitive da Vinci robotic surgical system. J. Robot. Surg. 2024, 18, 99. [Google Scholar] [CrossRef] [PubMed]
- Cepolina, F.; Razzoli, R.P. An introductory review of robotically assisted surgical systems. Int. J. Med. Robot. 2022, 18, e2409. [Google Scholar] [CrossRef] [PubMed]
- Cepolina, F.; Razzoli, R. Review of robotic surgery platforms and end effectors. J. Robot. Surg. 2024, 18, 74. [Google Scholar] [CrossRef] [PubMed]
- Giannini, A.; Pisaneschi, S.; Malacarne, E.; Cela, V.; Melfi, F.; Perutelli, A.; Simoncini, T. Robotic Approach to Ureteral Endometriosis: Surgical Features and Perioperative Outcomes. Front. Surg. 2018, 5, 51. [Google Scholar] [CrossRef] [PubMed]
- Soto, E.; Luu, T.H.; Liu, X.; Magrina, J.F.; Wasson, M.N.; Einarsson, J.I.; Cohen, S.L.; Falcone, T. Laparoscopy vs. Robotic Surgery for Endometriosis (LAROSE): A multicenter, randomized, controlled trial. Fertil. Steril. 2017, 107, 996–1002.e1003. [Google Scholar] [CrossRef]
- Le Gac, M.; Ferrier, C.; Touboul, C.; Owen, C.; Arfi, A.; Boudy, A.S.; Jayot, A.; Bendifallah, S.; Darai, E. Comparison of robotic versus conventional laparoscopy for the treatment of colorectal endometriosis: Pilot study of an expert center. J. Gynecol. Obs. Hum. Reprod. 2020, 49, 101885. [Google Scholar] [CrossRef]
- Nezhat, C.; Lewis, M.; Kotikela, S.; Veeraswamy, A.; Saadat, L.; Hajhosseini, B.; Nezhat, C. Robotic versus standard laparoscopy for the treatment of endometriosis. Fertil. Steril. 2010, 94, 2758–2760. [Google Scholar] [CrossRef]
- Chu, C.M.; Chang-Jackson, S.C.; Nezhat, F.R. Retrospective Study Assessing Laparoscopic Versus Robotic Assisted Laparoscopic Treatment of Severe Endometriosis. J. Minim. Invasive Gynecol. 2011, 18, S101. [Google Scholar] [CrossRef]
- Dulemba, J.F.; Pelzel, C.; Hubert, H.B. Retrospective analysis of robot-assisted versus standard laparoscopy in the treatment of pelvic pain indicative of endometriosis. J. Robot. Surg. 2013, 7, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Nezhat, F.R.; Sirota, I. Perioperative outcomes of robotic assisted laparoscopic surgery versus conventional laparoscopy surgery for advanced-stage endometriosis. JSLS 2014, 18, e2014.00094. [Google Scholar] [CrossRef] [PubMed]
- Nezhat, C.R.; Stevens, A.; Balassiano, E.; Soliemannjad, R. Robotic-assisted laparoscopy vs conventional laparoscopy for the treatment of advanced stage endometriosis. J. Minim. Invasive Gynecol. 2015, 22, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Magrina, J.F.; Espada, M.; Kho, R.M.; Cetta, R.; Chang, Y.H.; Magtibay, P.M. Surgical Excision of Advanced Endometriosis: Perioperative Outcomes and Impacting Factors. J. Minim. Invasive Gynecol. 2015, 22, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Raimondo, D.; Alboni, C.; Orsini, B.; Aru, A.C.; Farulla, A.; Maletta, M.; Arena, A.; Del Forno, S.; Sampogna, V.; Mastronardi, M.; et al. Comparison of perioperative outcomes between standard laparoscopic and robot-assisted approach in patients with rectosigmoid endometriosis. Acta Obs. Gynecol. Scand. 2021, 100, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Hiltunen, J.; Eloranta, M.L.; Lindgren, A.; Keski-Nisula, L.; Anttila, M.; Sallinen, H. Robotic-assisted laparoscopy is a feasible method for resection of deep infiltrating endometriosis, especially in the rectosigmoid area. J. Int. Med. Res 2021, 49, 3000605211032788. [Google Scholar] [CrossRef] [PubMed]
- Legendri, S.; Carbonnel, M.; Feki, A.; Moawad, G.; Aubry, G.; Vallee, A.; Ayoubi, J.M. Improvement of Post-Operative Quality of Life in Patients 2 Years after Minimally Invasive Surgery for Pain and Deep Infiltrating Endometriosis. J. Clin. Med. 2022, 11, 6132. [Google Scholar] [CrossRef] [PubMed]
- Ferrier, C.; Le Gac, M.; Kolanska, K.; Boudy, A.S.; Dabi, Y.; Touboul, C.; Bendifallah, S.; Darai, E. Comparison of robot-assisted and conventional laparoscopy for colorectal surgery for endometriosis: A prospective cohort study. Int. J. Med. Robot. 2022, 18, e2382. [Google Scholar] [CrossRef]
- Crestani, A.; Bibaoune, A.; Le Gac, M.; Dabi, Y.; Kolanska, K.; Ferrier, C.; Bendifallah, S.; Touboul, C.; Darai, E. Changes in hospital consumption of opioid and non-opioid analgesics after colorectal endometriosis surgery. J. Robot. Surg. 2023, 17, 2703–2710. [Google Scholar] [CrossRef]
- Verrelli, L.; Merlot, B.; Chanavaz-Lacheray, I.; Braund, S.; D’Ancona, G.; Kade, S.; Dennis, T.; Roman, H. Robotic Surgery for Severe Endometriosis: A Preliminary Comparative Study of Cost Estimation. J. Minim. Invasive Gynecol. 2024, 31, 95–101.e101. [Google Scholar] [CrossRef] [PubMed]
- Volodarsky-Perel, A.; Merlot, B.; Denost, Q.; Dennis, T.; Chanavaz-Lacheray, I.; Roman, H. Robotic-assisted versus conventional laparoscopic approach in patients with large rectal endometriotic nodule: The evaluation of safety and complications. Colorectal Dis. 2023, 25, 2233–2242. [Google Scholar] [CrossRef] [PubMed]
- Bandala, C.; Cifuentes-Chacon, J.P.; Cortes-Vazquez, A.; Ruz-Barros, R.; Garrocho-Hernandez, L.; Cortes-Algara, A. Efficacy between Conventional Laparoscopy and Robotic Surgery in Mexican Patients with Endometriosis: A Comparative Study. J. Clin. Med. 2024, 13, 3576. [Google Scholar] [CrossRef] [PubMed]
- Jayakumaran, J.; Patel, S.D.; Gangrade, B.K.; Narasimhulu, D.M.; Pandian, S.R.; Silva, C. Robotic-assisted laparoscopy in reproductive surgery: A contemporary review. J. Robot. Surg. 2017, 11, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Working group of ESGE, ESHRE and WES; Saridogan, E.; Becker, C.M.; Feki, A.; Grimbizis, G.F.; Hummelshoj, L.; Keckstein, J.; Nisolle, M.; Tanos, V.; Ulrich, U.A.; et al. Recommendations for the surgical treatment of endometriosis-part 1: Ovarian endometrioma. Gynecol. Surg. 2017, 14, 27. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Park, S.Y.; Jeong, K.; Yun, H.Y.; Chung, H.W. What is the role of robotic surgery in ovarian cystectomy with fertility preservation? J. Robot. Surg. 2023, 17, 2743–2747. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Rallabandi, H.; Bana, R.; Bag, M.; Raina, R.; Sridhar, D.; Deepika, H.K.; Reddy, P. Ovarian Loss in Laparoscopic and Robotic Cystectomy Compared Using Artificial Intelligence Pathology. JSLS 2024, 28, e2024.00001. [Google Scholar] [CrossRef] [PubMed]
- Pavone, M.; Baroni, A.; Campolo, F.; Goglia, M.; Raimondo, D.; Carcagni, A.; Akladios, C.; Marescaux, J.; Fanfani, F.; Scambia, G.; et al. Robotic assisted versus laparoscopic surgery for deep endometriosis: A meta-analysis of current evidence. J. Robot. Surg. 2024, 18, 212. [Google Scholar] [CrossRef] [PubMed]
- Csirzo, A.; Kovacs, D.P.; Szabo, A.; Fehervari, P.; Janko, A.; Hegyi, P.; Nyirady, P.; Sipos, Z.; Sara, L.; Acs, N.; et al. Robot-assisted laparoscopy does not have demonstrable advantages over conventional laparoscopy in endometriosis surgery: A systematic review and meta-analysis. Surg. Endosc. 2024, 38, 529–539. [Google Scholar] [CrossRef]
- Terho, A.M.; Makela-Kaikkonen, J.; Ohtonen, P.; Uimari, O.; Puhto, T.; Rautio, T.; Koivurova, S. Robotic versus laparoscopic surgery for severe deep endometriosis: Protocol for a randomised controlled trial (ROBEndo trial). BMJ Open 2022, 12, e063572. [Google Scholar] [CrossRef]
- Chatterjee, S.; Das, S.; Ganguly, K.; Mandal, D. Advancements in robotic surgery: Innovations, challenges and future prospects. J. Robot. Surg. 2024, 18, 28. [Google Scholar] [CrossRef] [PubMed]
- Goh, E.Z.; Ali, T. Robotic surgery: An evolution in practice. J. Surg. Protoc. Res. Methodol. 2022, 2022, snac003. [Google Scholar] [CrossRef]
- Cunningham, B.W.; Brooks, D.M.; McAfee, P.C. Accuracy of Robotic-Assisted Spinal Surgery-Comparison to TJR Robotics, da Vinci Robotics, and Optoelectronic Laboratory Robotics. Int. J. Spine Surg. 2021, 15, S38–S55. [Google Scholar] [CrossRef] [PubMed]
- Hurley, A.M.; Kennedy, P.J.; O’Connor, L.; Dinan, T.G.; Cryan, J.F.; Boylan, G.; O’Reilly, B.A. SOS save our surgeons: Stress levels reduced by robotic surgery. Gynecol. Surg. 2015, 12, 197–206. [Google Scholar] [CrossRef]
- Kim, S.; Min, K.J.; Lee, S.; Hong, J.H.; Song, J.Y.; Lee, J.K.; Lee, N.W. Robotic single-site surgery versus laparo-endoscopic single-site surgery in ovarian cystectomy: A retrospective analysis in single institution. Gynecol. Robot. Surg. 2020, 1, 21–26. [Google Scholar] [CrossRef]
- Yohannes, P.; Rotariu, P.; Pinto, P.; Smith, A.D.; Lee, B.R. Comparison of robotic versus laparoscopic skills: Is there a difference in the learning curve? Urology 2002, 60, 39–45, discussion 45. [Google Scholar] [CrossRef] [PubMed]
- Kanitra, J.J.; Khogali-Jakary, N.; Gambhir, S.B.; Davis, A.T.; Hollis, M.; Moon, C.; Gupta, R.; Haan, P.S.; Anderson, C.; Collier, D.; et al. Transference of skills in robotic vs. laparoscopic simulation: A randomized controlled trial. BMC Surg. 2021, 21, 379. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.S.; Shim, J.E.; Lee, S.R.; Jeong, K. The Comparison of Robotic Single-Site Surgery to Single-Port Laparoendoscopic Surgery for the Treatment of Advanced-Stage Endometriosis. J. Laparoendosc. Adv. Surg. Tech. A 2018, 28, 1483–1488. [Google Scholar] [CrossRef]
- Jayakumaran, J.; Pavlovic, Z.; Fuhrich, D.; Wiercinski, K.; Buffington, C.; Caceres, A. Robotic single-site endometriosis resection using near-infrared fluorescence imaging with indocyanine green: A prospective case series and review of literature. J. Robot. Surg. 2020, 14, 145–154. [Google Scholar] [CrossRef]
- Intuitive Announces FDA Clearance of Fifth-Generation Robotic System, da Vinci 5. Available online: https://isrg.intuitive.com/node/20696/pdf (accessed on 5 May 2024).
- Sadri, H.; Fung-Kee-Fung, M.; Shayegan, B.; Garneau, P.Y.; Pezeshki, P. A systematic review of full economic evaluations of robotic-assisted surgery in thoracic and abdominopelvic procedures. J. Robot. Surg. 2023, 17, 2671–2685. [Google Scholar] [CrossRef]
- Mehta, A.; Cheng Ng, J.; Andrew Awuah, W.; Huang, H.; Kalmanovich, J.; Agrawal, A.; Abdul-Rahman, T.; Hasan, M.M.; Sikora, V.; Isik, A. Embracing robotic surgery in low- and middle-income countries: Potential benefits, challenges, and scope in the future. Ann. Med. Surg. (Lond) 2022, 84, 104803. [Google Scholar] [CrossRef] [PubMed]
- Brar, G.; Xu, S.; Anwar, M.; Talajia, K.; Ramesh, N.; Arshad, S.R. Robotic surgery: Public perceptions and current misconceptions. J. Robot. Surg. 2024, 18, 84. [Google Scholar] [CrossRef] [PubMed]
- Rivero-Moreno, Y.; Echevarria, S.; Vidal-Valderrama, C.; Pianetti, L.; Cordova-Guilarte, J.; Navarro-Gonzalez, J.; Acevedo-Rodriguez, J.; Dorado-Avila, G.; Osorio-Romero, L.; Chavez-Campos, C.; et al. Robotic Surgery: A Comprehensive Review of the Literature and Current Trends. Cureus 2023, 15, e42370. [Google Scholar] [CrossRef] [PubMed]
- Marcus, H.J.; Ramirez, P.T.; Khan, D.Z.; Layard Horsfall, H.; Hanrahan, J.G.; Williams, S.C.; Beard, D.J.; Bhat, R.; Catchpole, K.; Cook, A.; et al. The IDEAL framework for surgical robotics: Development, comparative evaluation and long-term monitoring. Nat. Med. 2024, 30, 61–75. [Google Scholar] [CrossRef] [PubMed]

| Study | Design | Group | Age | rASRM Stage | Operation Time (min) | Blood Loss (mL) | Hospital Stay (Days) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RALS | LPS | RALS | LPS | RALS | LPS | RALS | LPS | RALS | LPS | |||
| Nezhat et al. [20] (2010) | Retrospective | 40 | 38 | 35 | 33 | I–IV | 191 (135–295) | 159 (85–320) | 60 | 65 | N/A | N/A |
| Chu et al. [21] (2011) | Retrospective | 25 | 96 | N/A | N/A | III–IV | 238 (120–630) | 190 (71–674) | No difference | No difference | No difference | No difference |
| Dulemba et al. [22] (2013) | Retrospective | 180 | 100 | 32.6 | 29.2 | I–IV | 77.4 ± 41.6 | 72.0 ± 28.5 | 2.92 ± 43.2 | 24.9 ± 24.3 | N/A | N/A |
| Nezhat et al. [23] (2014) | Retrospective | 32 | 86 | 42.5 | 40 | III–IV | 250 (176–328) | 173 (123–237) | 100 | 50 | 1 | 1 |
| Nezhat et al. [24] (2015) | Retrospective | 147 | 273 | 30 | 31 | III–IV | 196 | 135 | 40 | 25 | >1 | 1 |
| Magrina et al. [25] (2015) | Retrospective | 331 | 162 | 40 | 38.3 | III–IV | 139 (40–531) | 113 (28–347) | 92 | 82 | 1.1 | 0.7 |
| Soto et al. [18] (2017) | Prospective | 35 | 38 | 34.3 | 34.5 | I–IV | 106 ± 48 | 101 ± 63 | 100 ± 229 | 43 ± 39 | N/A | N/A |
| Le Gac et al. [19] (2020) | Prospective | 23 | 25 | 36 | 37 | III–IV | 221 ± 94 | 163 ± 83 | 130 ± 86 | 108 ± 99 | 8.0 ± 4.4 | 6.5 ± 2.6 |
| Raimondo et al. [26] (2021) | Retrospective | 22 | 22 | 38 | 36 | III–IV | 207 ± 79 | 177 ± 63 | 181 ± 214 | 144 ± 101 | 8 ± 7 | 6 ± 2 |
| Hiltunen et al. [27] (2021) | Retrospective | 18 | 76 | N/A | N/A | I–IV | N/A | N/A | N/A | N/A | N/A | N/A |
| Legendri et al. [28] (2022) | Retrospective | 26 | 28 | 36.5 | 34 | IV | N/A | N/A | N/A | N/A | N/A | N/A |
| Ferrier et al. [29] (2022) | Prospective | 61 | 61 | 36 | 35 | I–IV | 208 ± 90 | 169 ± 81 | No difference | No difference | N/A | N/A |
| Crestani et al. [30] (2023) | Retrospective | 89 | 73 | N/A | N/A | III–IV | N/A | N/A | N/A | N/A | N/A | N/A |
| Verrelli et al. [31] (2023) | Retrospective | 71 | 104 | 37.3 | 38.4 | III–IV | 150 | 105 | N/A | N/A | No difference | No difference |
| Volodarsky Perel et al. [32] (2023) | Retrospective | 97 | 451 | 37.3 | 37.9 | III–IV | N/A | N/A | N/A | N/A | N/A | N/A |
| Bandala et al. [33] (2024) | Retrospective | 37 | 56 | 47.3 | 35.8 | I–IV | 170 ± 52 | 125 ± 43.6 | 50 ± 47.3 | 50 ± 46.8 | 1 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Kim, S. Is It the Best Option? Robotic Surgery for Endometriosis. Life 2024, 14, 982. https://doi.org/10.3390/life14080982
Lee J, Kim S. Is It the Best Option? Robotic Surgery for Endometriosis. Life. 2024; 14(8):982. https://doi.org/10.3390/life14080982
Chicago/Turabian StyleLee, Jihyun, and Seongmin Kim. 2024. "Is It the Best Option? Robotic Surgery for Endometriosis" Life 14, no. 8: 982. https://doi.org/10.3390/life14080982
APA StyleLee, J., & Kim, S. (2024). Is It the Best Option? Robotic Surgery for Endometriosis. Life, 14(8), 982. https://doi.org/10.3390/life14080982






