Introducing a Simple Tool of Patient Self-Assessment of Wrist Range of Motion
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
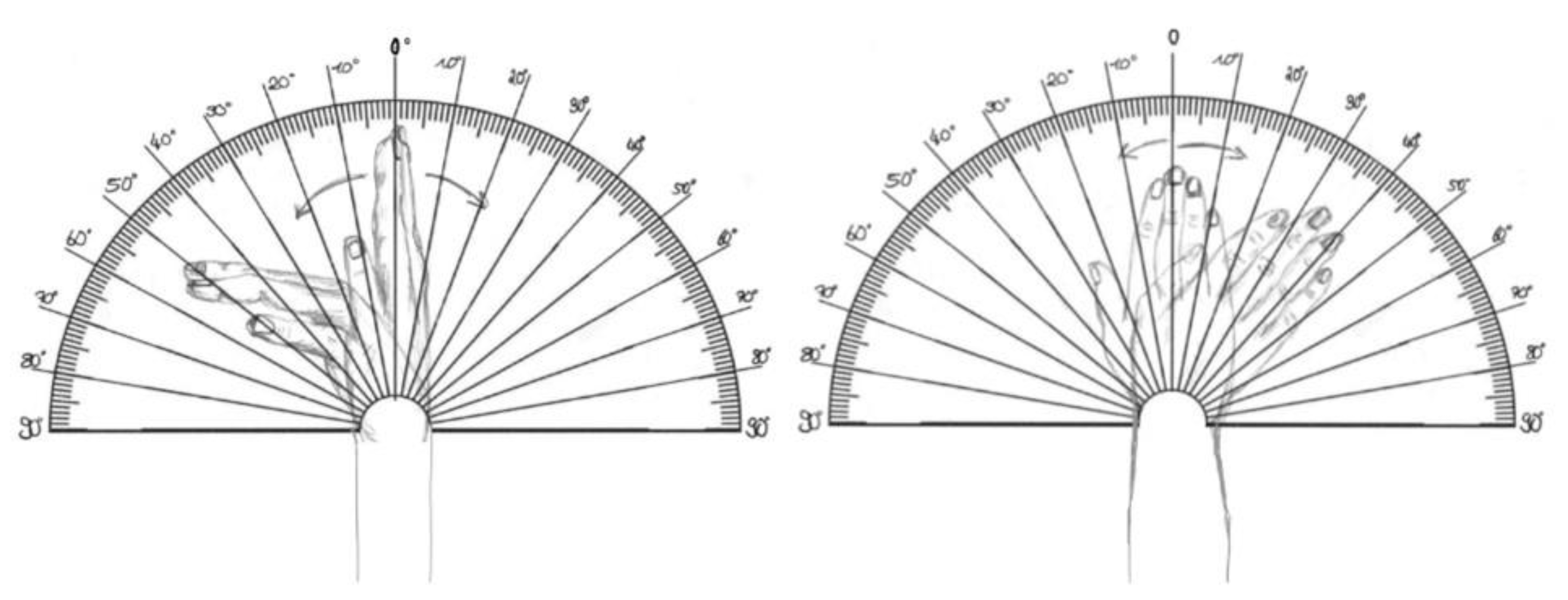
2.2. Design of Template
2.3. Assessment
2.4. Statistical Analysis
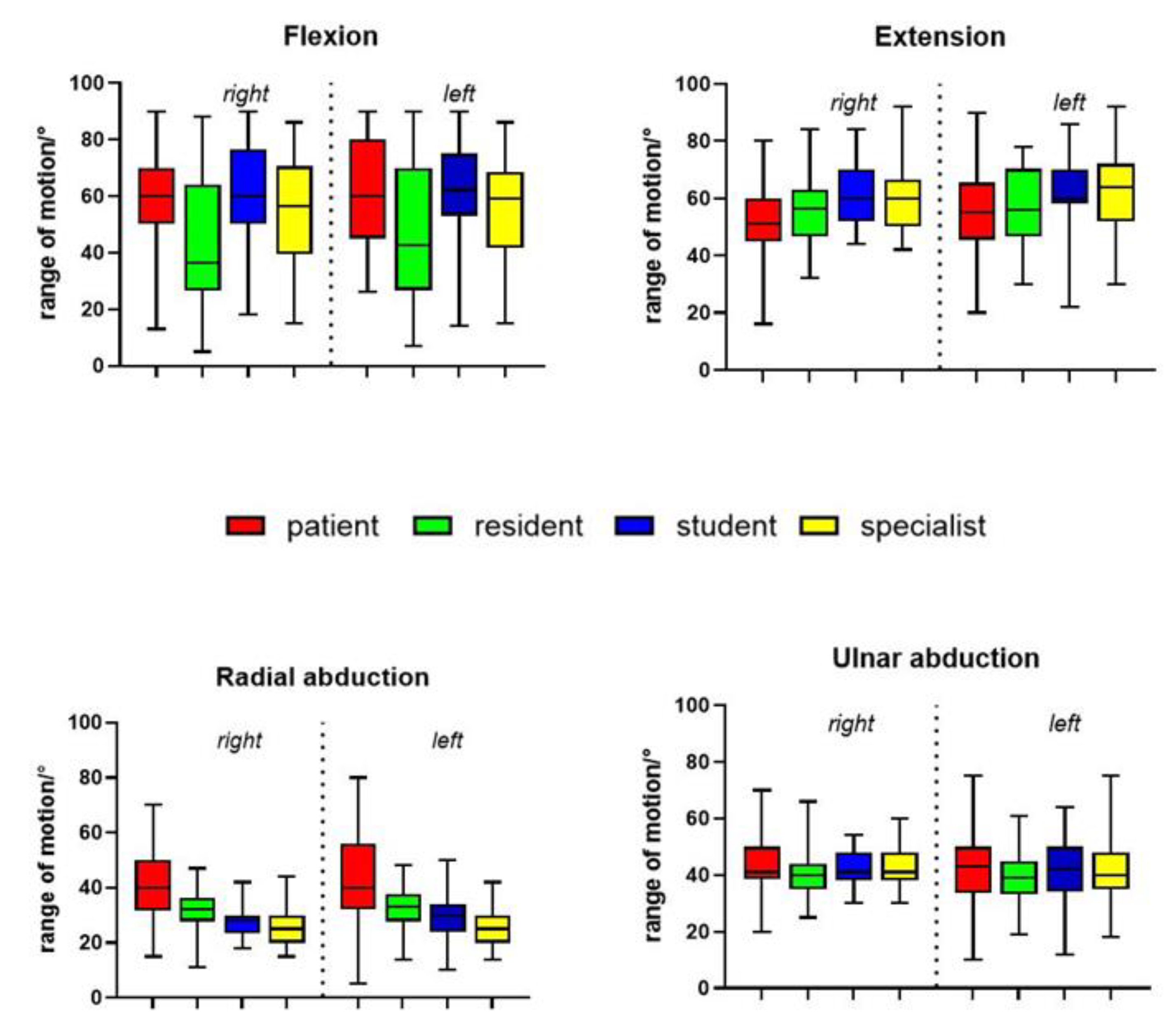
3. Results
3.1. Pre-Study
3.2. Study
3.3. Subgroup Analysis: Academics vs. Non-Academics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kassay, A.D.; Daher, B.; Lalone, E.A. An analysis of wrist and forearm range of motion using the Dartfish motion analysis system. J. Hand Ther. 2021, 34, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Lefevre-Colau, M.M.; Poiraudeau, S.; Oberlin, C.; Demaille, S.; Fermanian, J.; Rannou, F.; Revel, M. Reliability, validity, and responsiveness of the modified Kapandji index for assessment of functional mobility of the rheumatoid hand. Arch. Phys. Med. Rehabil. 2003, 84, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Ellis, B.; Bruton, A.; Goddard, J.R. Joint angle measurement: A comparative study of the reliability of goniometry and wire tracing for the hand. Clin. Rehabil. 1997, 11, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Kuchtaruk, A.; Yu, S.S.Y.; Iansavichene, A.; Davidson, J.; Wilson, C.A.; Symonette, C. Telerehabilitation Technology Used for Remote Wrist/Finger Range of Motion Evaluation: A Scoping Review. Plast. Reconstr. Surg. Glob. Open 2023, 11, e5147. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Wessel, J.; Humphrey, R.; Ross, D.; Roth, J.H. Validity of self-report measures of pain and disability for persons who have undergone arthroplasty for osteoarthritis of the carpometacarpal joint of the hand. Osteoarthr. Cartil. 2007, 15, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Shafiee, E.; MacDermid, J.; Farzad, M.; Karbalaei, M. A systematic review and meta-analysis of Patient-Rated Wrist (and Hand) Evaluation (PRWE/PRWHE) measurement properties, translation, and/ or cross-cultural adaptation. Disabil. Rehabil. 2022, 44, 6551–6565. [Google Scholar] [CrossRef] [PubMed]
- Stumpfe, F.M.; Schneider, M.O.; Hein, A.; Faschingbauer, F.; Kehl, S.; Hermanek, P.; Bohm, J.; Scharl, A.; Beckmann, M.W.; Staerk, C.; et al. Limited Effects of SARS-CoV-2 Pandemic-related Lockdowns and Reduced Population Mobility on Preterm Birth Rates: A Secondary Analysis of Bavarian Obstetric Quality Parameters from 2010 to 2020. Geburtshilfe Frauenheilkd 2022, 82, 842–851. [Google Scholar] [CrossRef]
- Prgomet, M.; Hardie, R.A.; Sezgin, G.; Thomas, J.; Pearce, C.; McGuire, P.; Weeding, S.; McLeod, A.; Georgiou, A. Telehealth Uptake and Impact on Care Activities in Australian General Practice During the COVID-19 Pandemic. Stud. Health Technol. Inform. 2023, 309, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Millman, A.; Huang, J.; Graetz, I.; Lee, C.; Shan, J.; Hsueh, L.; Muelly, E.; Gopalan, A.; Reed, M. Patient-reported Primary Care Video and Telephone Telemedicine Preference Shifts During the COVID-19 Pandemic. Med. Care 2023, 61, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Haimi, M.; Goren, U.; Grossman, Z. Barriers and challenges to telemedicine usage among the elderly population in Israel in light of the COVID-19 era: A qualitative study. Digit. Health 2024, 10, 20552076241240235. [Google Scholar] [CrossRef] [PubMed]
- Menendez, M.E.; Ring, D. Factors associated with non-attendance at a hand surgery appointment. Hand 2015, 10, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Bhavsar, N.A.; Doerfler, S.M.; Giczewska, A.; Alhanti, B.; Lutz, A.; Thigpen, C.A.; George, S.Z. Prevalence and predictors of no-shows to physical therapy for musculoskeletal conditions. PLoS ONE 2021, 16, e0251336. [Google Scholar] [CrossRef] [PubMed]
- Groth, G.N.; Wilder, D.M.; Young, V.L. The impact of compliance on the rehabilitation of patients with mallet finger injuries. J. Hand Ther. 1994, 7, 21–24. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Pathirana, P.N.; Trinh, H.; Fay, P. A Non-Contact Measurement System for the Range of Motion of the Hand. Sensors 2015, 15, 18315–18333. [Google Scholar] [CrossRef] [PubMed]
- Butler, S.M. After COVID-19-Thinking Differently About Running the Health Care System. JAMA Health Forum 2020, 1, e200478. [Google Scholar] [CrossRef] [PubMed]
- Gajarawala, S.N.; Pelkowski, J.N. Telehealth Benefits and Barriers. J. Nurse Pract. 2021, 17, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Hailey, D.; Roine, R.; Ohinmaa, A.; Dennett, L. Evidence of benefit from telerehabilitation in routine care: A systematic review. J. Telemed. Telecare 2011, 17, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Ge, M.; Chen, J.; Zhu, Z.J.; Shi, P.; Yin, L.R.; Xia, L. Wrist ROM measurements using smartphone photography: Reliability and validity. Hand Surg. Rehabil. 2020, 39, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Grandizio, L.C.; Foster, B.K.; Klena, J.C. Telemedicine in Hand and Upper-Extremity Surgery. J. Hand Surg. Am. 2020, 45, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Scott, K.L.; Skotak, C.M.; Renfree, K.J. Remote Assessment of Wrist Range of Motion: Inter- and Intra-Observer Agreement of Provider Estimation and Direct Measurement with Photographs and Tracings. J. Hand Surg. Am. 2019, 44, 954–965. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.W.L.; Tan, K.G.; Neoh, E.C.; Wong, J.; Roslan, A.S.; Huang, S.; Tan, T.L. The effect of patient positioning on the accuracy and reliability of assessment of knee range of motion over a telemedicine platform. J. Telemed. Telecare 2024, 30, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Reissner, L.; Fischer, G.; List, R.; Taylor, W.R.; Giovanoli, P.; Calcagni, M. Minimal detectable difference of the finger and wrist range of motion: Comparison of goniometry and 3D motion analysis. J. Orthop. Surg. Res. 2019, 14, 173. [Google Scholar] [CrossRef] [PubMed]
- Costa, V.; Ramirez, O.; Otero, A.; Munoz-Garcia, D.; Uribarri, S.; Raya, R. Validity and reliability of inertial sensors for elbow and wrist range of motion assessment. PeerJ 2020, 8, e9687. [Google Scholar] [CrossRef] [PubMed]
- Crasto, J.A.; Sayari, A.J.; Gray, R.R.; Askari, M. Comparative analysis of photograph-based clinical goniometry to standard techniques. Hand 2015, 10, 248–253. [Google Scholar] [CrossRef] [PubMed]
- Worboys, T.; Brassington, M.; Ward, E.C.; Cornwell, P.L. Delivering occupational therapy hand assessment and treatment sessions via telehealth. J. Telemed. Telecare 2018, 24, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Ellis, B.; Bruton, A. A study to compare the reliability of composite finger flexion with goniometry for measurement of range of motion in the hand. Clin. Rehabil. 2002, 16, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Marx, R.G.; Bombardier, C.; Wright, J.G. What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? J. Hand Surg. Am. 1999, 24, 185–193. [Google Scholar] [CrossRef]
- Marti-Puente, M.; Sullivan, P.; O’Connor, E.F.; Iwuagwu, F.C. Measurements of range of motion of finger joints with simple digital photography: A validation study. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 2392–2442. [Google Scholar] [CrossRef] [PubMed]
- Meijer, H.A.W.; Graafland, M.; Obdeijn, M.C.; Schijven, M.P.; Goslings, J.C. Validity and reliability of a wearable-controlled serious game and goniometer for telemonitoring of wrist fracture rehabilitation. Eur. J. Trauma. Emerg. Surg. 2022, 48, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Smeragliuolo, A.H.; Hill, N.J.; Disla, L.; Putrino, D. Validation of the Leap Motion Controller using markered motion capture technology. J. Biomech. 2016, 49, 1742–1750. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.R.; Conti Mica, M.; Shin, A.Y. Smartphone photography utilized to measure wrist range of motion. J. Hand Surg. Eur. Vol. 2018, 43, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Wirth, M.A.; Fischer, G.; Verdu, J.; Reissner, L.; Balocco, S.; Calcagni, M. Comparison of a New Inertial Sensor Based System with an Optoelectronic Motion Capture System for Motion Analysis of Healthy Human Wrist Joints. Sensors 2019, 19, 5297. [Google Scholar] [CrossRef] [PubMed]
- Suffa, N.; Merkel, P.; Horch, R.E.; Arkudas, A.; Ludolph, I.; Stumpfe, M.C. Temporarily Transfixation of the distal interphalangeal Joint in Mallet fingers. Handchir. Mikrochir. Plast. Chir. 2021, 53, 441–446. [Google Scholar] [CrossRef]
- Stumpfe, M.C.; Suffa, N.; Merkel, P.; Ludolph, I.; Arkudas, A.; Horch, R.E. Quick and safe: Why a k-wire-extension-block-fixation of a bony mallet finger is the favoured treatment. Arch. Orthop. Trauma. Surg. 2024, 144, 1437–1442. [Google Scholar] [CrossRef] [PubMed]

| Flexion | Extension | Radial Abduction | Ulnar Abduction | |
|---|---|---|---|---|
| Goniometer | 79.5 ± 6.5 | 67.9 ± 67.9 | 26.5 ± 6.4 | 45.2 ± 6.4 |
| Template | 73.6 ± 7.2 | 68.2 ± 7.8 | 26.6 ± 2.9 | 40.8 ± 4.8 |
| Mean difference | 5.9 | 0.3 | 0.1 | 4.4 |
| p = 0.04 | n.s. | n.s. | p = 0.02 |
| Flexion | Extension | Radial Abduction | Ulnar Abduction | |||||
|---|---|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | Right | Left | |
| Patient | 60.0 +/− 19.4 | 60.0 +/− 18.9 | 51.0 +/− 12.7 | 55.0 +/− 15.5 | 40.0 +/− 13.1 | 40.0 +/− 15.7 | 41.0 +/− 9.5 | 43.0 +/− 12.6 |
| Resident | 36.6 +/− 21.5 | 42.5 +/− 24.4 | 56.5 +/− 11.3 | 56.0 +/− 13.5 | 32.0 +/− 6.8 | 33.0 +/− 7.6 | 40.0 +/− 8.7 | 39.0 +/− 9.0 |
| Student | 60.0 +/− 19.4 | 62.0 +/− 17.0 | 60.0 +/− 10.1 | 60.0 +/− 11.2 | 28.0 +/− 5.2 | 30.0 +/− 7.7 | 41.0 +/− 6.6 | 42.0 +/− 10.2 |
| Specialist | 56.5 +/− 20.2 | 59.0 +/− 17.8 | 60.0 +/− 11.5 | 64.0 +/− 13.6 | 25.0 +/− 6.1 | 25.0 +/− 7.0 | 41.0 +/− 6.6 | 40.0 +/− 10.4 |
| p-Value | Mean Deviation | ||
|---|---|---|---|
| Radial abduction | |||
| right—patient vs. student | *** | <0.0001 | 13.2 |
| right—patient vs. resident | *** | <0.0001 | 9.2 |
| right—patient vs. specialist | *** | <0.0001 | 15.1 |
| right—student vs. resident | ** | 0.0084 | −4.1 |
| right—resident vs. specialist | *** | <0.0001 | 6.0 |
| left—patient vs. student | *** | <0.0001 | 13.5 |
| left—patient vs. resident | *** | <0.0001 | 11.1 |
| left—patient vs. specialist | *** | <0.0001 | 16.5 |
| left—resident vs. specialist | ** | 0.0018 | 5.4 |
| Extension | |||
| right—patient vs. student | *** | <0.0001 | −8.5 |
| right—patient vs. specialist | * | 0.012 | −7.4 |
| right—student vs. resident | *** | 0.0002 | 6.5 |
| Flexion | |||
| right—patient vs. resident | *** | <0.0001 | 15.3 |
| right—student vs. resident | *** | <0.0001 | 16.9 |
| right—resident vs. specialist | ** | 0.0016 | −10.9 |
| left—patient vs. resident | *** | 0.0009 | 12.8 |
| left—student vs. resident | *** | <0.0001 | 14.7 |
| left—student vs. specialist | ** | 0.005 | 7.2 |
| p-Value | Mean Deviation | |||||
|---|---|---|---|---|---|---|
| Radial abduction | ||||||
| A | NA | A | NA | A | NA | |
| right—patient vs. student | ** | *** | 0.0099 | 0.0005 | 10.4 | 11.9 |
| right—patient vs. resident | n.s. | ** | 0.0594 | 0.0037 | 8.3 | 7.4 |
| right—patient vs. specialist | ** | *** | 0.0077 | 0.0002 | 13.5 | 12.2 |
| left—patient vs. student | * | n.s. | 0.0190 | 0.8231 | 11.0 | 1.7 |
| left—patient vs. resident | n.s. | n.s. | 0.1494 | 0.4695 | 5.9 | 3.4 |
| left—patient vs. specialist | ** | n.s. | 0.0088 | 0.9994 | 11.5 | 0.3 |
| Ulnar abduction | ||||||
| right—patient vs. student | n.s. | n.s. | 0.8500 | 0.1714 | 1.7 | 4.2 |
| right—patient vs. resident | n.s. | n.s. | 0.8015 | 0.0625 | 1.9 | 5.0 |
| right—patient vs. specialist | n.s. | n.s. | 0.9459 | 0.7625 | 1.3 | 1.9 |
| left—patient vs. student | n.s. | n.s. | 0.9949 | 0.8231 | 0.6 | 1.7 |
| left—patient vs. resident | n.s. | n.s. | 0.3837 | 0.4695 | 4.2 | 3.4 |
| left—patient vs. specialist | n.s. | n.s. | 0.9974 | 0.9994 | 0.6 | 0.3 |
| Extension | ||||||
| right—patient vs. student | ** | *** | 0.0011 | 0.0005 | 9.3 | 8.8 |
| right—patient vs. resident | n.s. | n.s. | 0.9990 | 0.9939 | 0.3 | 0.6 |
| right—patient vs. specialist | n.s. | * | 0.7297 | 0.0362 | 3.7 | 8.5 |
| left—patient vs. student | ** | n.s. | 0.0046 | 0.3907 | 10.5 | 3.9 |
| left—patient vs. resident | n.s. | n.s. | 0.2339 | 0.9992 | 5.8 | 0.4 |
| left—patient vs. specialist | n.s. | n.s. | 0.1095 | 0.0982 | 8.3 | 6.4 |
| Flexion | ||||||
| right—patient vs. student | n.s. | n.s. | 0.8962 | 0.9955 | 3.3 | 0.7 |
| right—patient vs. resident | * | *** | 0.0176 | <0.0001 | 15.3 | 17.4 |
| right—patient vs. specialist | n.s. | n.s. | 0.9501 | 0.0831 | 2.3 | 7.8 |
| left—patient vs. student | n.s. | n.s. | 0.2236 | 0.9996 | 6.2 | 0.3 |
| left—patient vs. resident | n.s. | *** | 0.0750 | 0.0004 | 9.5 | 14.6 |
| left—patient vs. specialist | n.s. | ** | 0.7566 | 0.0076 | 2.9 | 8.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stumpfe, M.C.; Beneke, K.; Horch, R.E.; Arkudas, A.; Müller-Seubert, W.; Cai, A. Introducing a Simple Tool of Patient Self-Assessment of Wrist Range of Motion. Life 2024, 14, 997. https://doi.org/10.3390/life14080997
Stumpfe MC, Beneke K, Horch RE, Arkudas A, Müller-Seubert W, Cai A. Introducing a Simple Tool of Patient Self-Assessment of Wrist Range of Motion. Life. 2024; 14(8):997. https://doi.org/10.3390/life14080997
Chicago/Turabian StyleStumpfe, Maximilian C., Kaya Beneke, Raymund E. Horch, Andreas Arkudas, Wibke Müller-Seubert, and Aijia Cai. 2024. "Introducing a Simple Tool of Patient Self-Assessment of Wrist Range of Motion" Life 14, no. 8: 997. https://doi.org/10.3390/life14080997
APA StyleStumpfe, M. C., Beneke, K., Horch, R. E., Arkudas, A., Müller-Seubert, W., & Cai, A. (2024). Introducing a Simple Tool of Patient Self-Assessment of Wrist Range of Motion. Life, 14(8), 997. https://doi.org/10.3390/life14080997








