Advancing Post-Stroke Depression Research: Insights from Murine Models and Behavioral Analyses
Abstract
1. Background
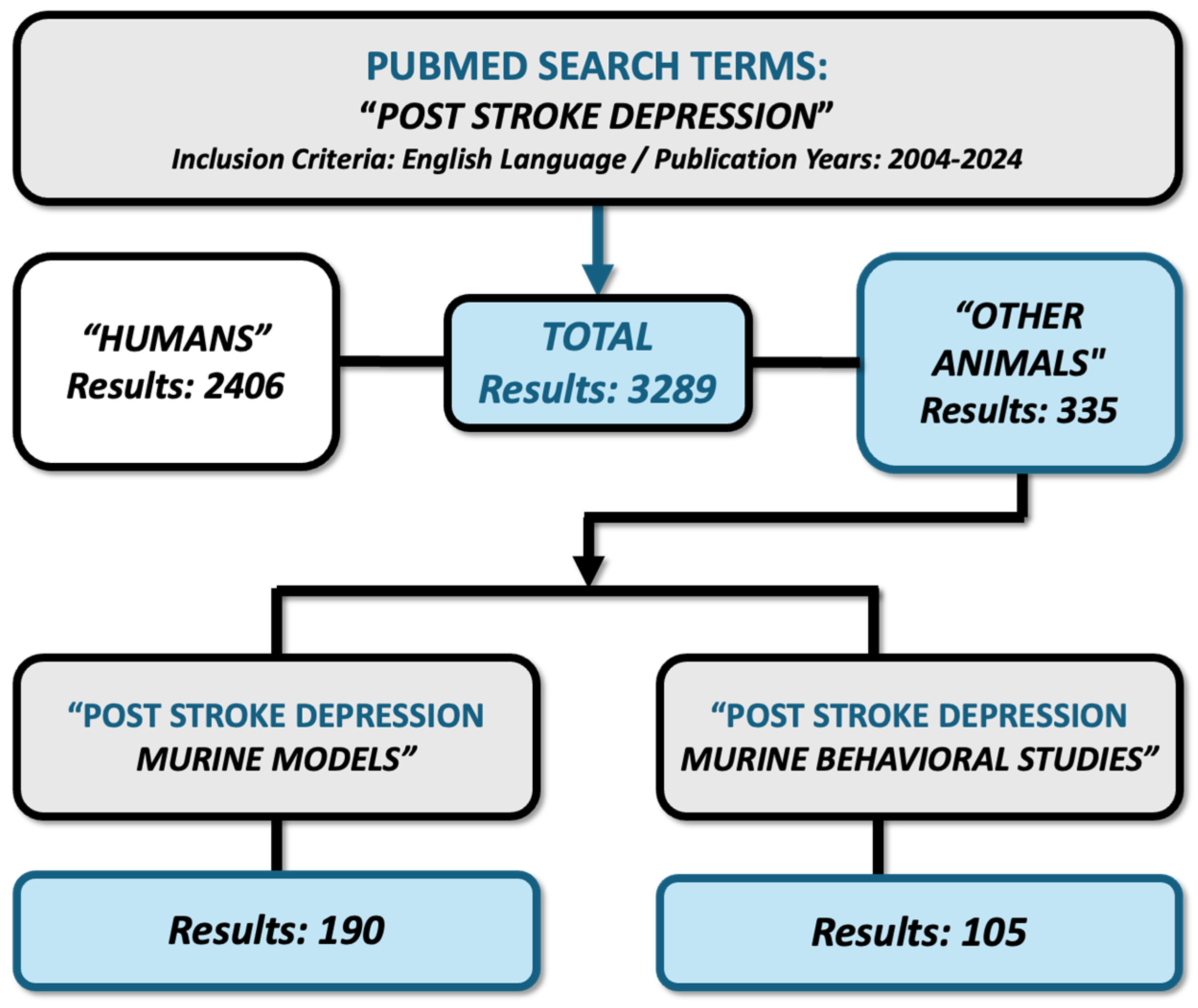
2. Materials and Methods
3. Incidence and Prevalence of PSD
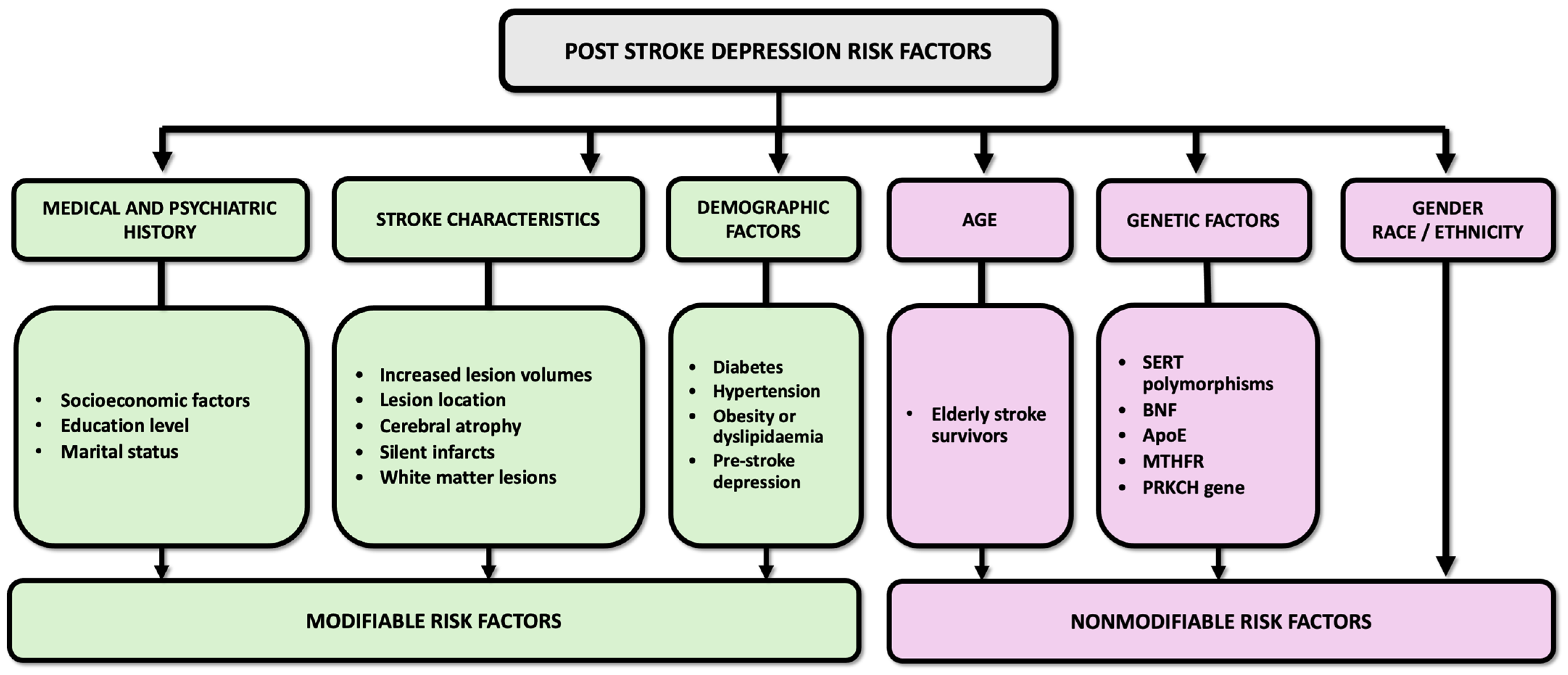
4. Risk Factors Involved in PSD
4.1. Stroke Characteristics and Lesion Localization
4.2. Demographic Factors
4.3. Age
4.4. Genetic Factors
4.5. Medical and Psychiatric History
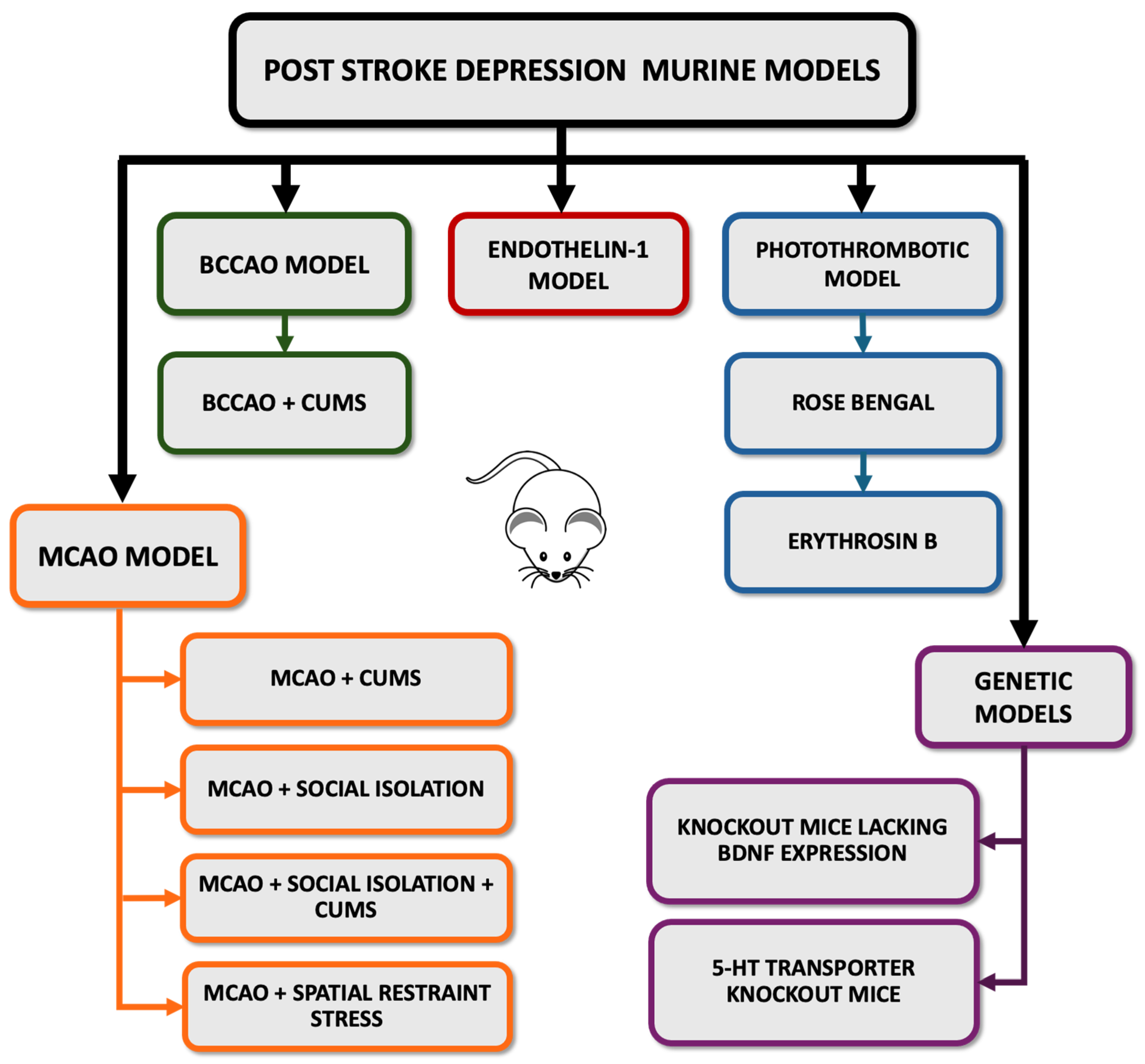
5. Valid Animal Models for PSD
5.1. Middle Cerebral Artery Occlusion (MCAO) Model
5.2. MCAO Model Combined with CUMS
5.3. MCAO Model Combined with Social Isolation
5.4. MCAO + Social Isolation + CUMS Model
5.5. MCAO Model Combined with Spatial Restraint Stress
5.6. Bilateral Common Carotid Artery Occlusion (BCCAO) Model
5.7. BCCAO Model Combined with CUMS
5.8. Intracerebral Injection of Endothelin-1 (ET-1)
5.9. Photothrombotic Model
5.10. Genetic Models of PSD
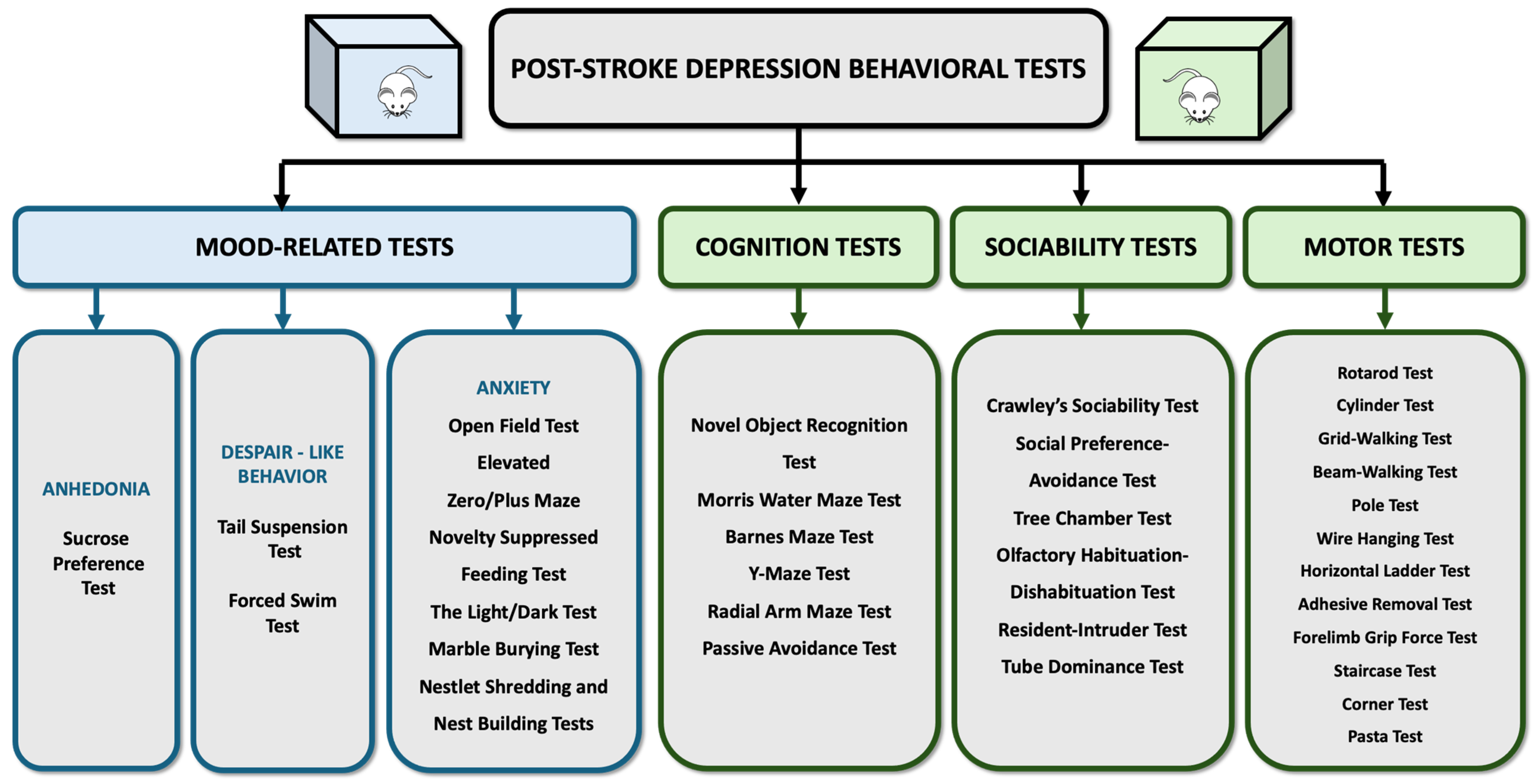
6. Assessing Symptoms and Behaviors: Key Tests for Studying PSD
6.1. Anhedonia Test: Sucrose Preference Test (SPT)
6.2. Depression-like Behavior Tests: Forced Swim Test and Tail Suspension Test
6.3. Anxiety Tests: Open Field/Elevated Zero Maze/Novelty Suppressed Feeding/The Light/Dark/Marble Burying
6.4. Social Withdrawal Tests: Crawley’s Sociability/Social Preference-Avoidance/Tree Chamber/Olfactory Habituation-Dishabituation/Resident-Intruder/Tube Dominance
6.5. Cognitive Impairments Tests: Morris Water Maze/Barnes Maze/Y-Maze/Novel Object Recognition/Radial Arm Maze/Passive Avoidance
6.6. Motor Function Tests: Rotarod/Cylinder/Grid-Walking/Beam-Walking/Pole/Wire Hanging/Horizontal Ladder/Adhesive Removal/Forelimb Grip/Staircase/Corner/Pasta
7. Pathophysiological Mechanisms Involved in PSD
8. Strain Differences in Rodents
9. Translatability of PSD Research
10. Future Directions
11. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Donkor, E.S. Stroke in the 21(st) Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res. Treat. 2018, 2018, 3238165. [Google Scholar] [CrossRef] [PubMed]
- Fekadu, G.; Adola, B.; Mosisa, G.; Shibiru, T.; Chelkeba, L. Clinical characteristics and treatment outcomes among stroke patients hospitalized to Nekemte referral hospital, western Ethiopia. J. Clin. Neurosci. 2020, 71, 170–176. [Google Scholar] [CrossRef]
- Boehme, A.K.; Esenwa, C.; Elkind, M.S. Stroke Risk Factors, Genetics, and Prevention. Circ. Res. 2017, 120, 472–495. [Google Scholar] [CrossRef] [PubMed]
- Arboix, A. Cardiovascular risk factors for acute stroke: Risk profiles in the different subtypes of ischemic stroke. World J. Clin. Cases 2015, 3, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Kernan, W.N.; Dearborn, J.L. Obesity increases stroke risk in young adults: Opportunity for prevention. Stroke 2015, 46, 1435–1436. [Google Scholar] [CrossRef][Green Version]
- Kotlęga, D.; Gołąb-Janowska, M.; Masztalewicz, M.; Ciećwież, S.; Nowacki, P. The emotional stress and risk of ischemic stroke. Neurol. Neurochir. Pol. 2016, 50, 265–270. [Google Scholar] [CrossRef]
- Kelly-Hayes, M. Influence of age and health behaviors on stroke risk: Lessons from longitudinal studies. J. Am. Geriatr. Soc. 2010, 58 (Suppl. 2), S325–S328. [Google Scholar] [CrossRef]
- Platz, T. Evidence-Based Guidelines and Clinical Pathways in Stroke Rehabilitation-An International Perspective. Front. Neurol. 2019, 10, 200. [Google Scholar] [CrossRef]
- Inatomi, Y.; Nakajima, M.; Yonehara, T.; Ando, Y. Ipsilateral hemiparesis in ischemic stroke patients. Acta Neurol. Scand. 2017, 136, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Yanohara, R.; Teranishi, T.; Tomita, Y.; Tanino, G.; Ueno, Y.; Sonoda, S. Recovery process of standing postural control in hemiplegia after stroke. J. Phys. Ther. Sci. 2014, 26, 1761–1765. [Google Scholar] [CrossRef]
- Kim, Y.W. Update on Stroke Rehabilitation in Motor Impairment. Brain Neurorehabil. 2022, 15, e12. [Google Scholar] [CrossRef] [PubMed]
- Chohan, S.A.; Venkatesh, P.K.; How, C.H. Long-term complications of stroke and secondary prevention: An overview for primary care physicians. Singap. Med. J. 2019, 60, 616–620. [Google Scholar] [CrossRef] [PubMed]
- Rost, N.S.; Brodtmann, A.; Pase, M.P.; van Veluw, S.J.; Biffi, A.; Duering, M.; Hinman, J.D.; Dichgans, M. Post-Stroke Cognitive Impairment and Dementia. Circ. Res. 2022, 130, 1252–1271. [Google Scholar] [CrossRef]
- Gaete, J.M.; Bogousslavsky, J. Post-stroke depression. Expert. Rev. Neurother. 2008, 8, 75–92. [Google Scholar] [CrossRef]
- Li, W.; Xiao, W.M.; Chen, Y.K.; Qu, J.F.; Liu, Y.L.; Fang, X.W.; Weng, H.Y.; Luo, G.P. Anxiety in Patients With Acute Ischemic Stroke: Risk Factors and Effects on Functional Status. Front. Psychiatry 2019, 10, 257. [Google Scholar] [CrossRef]
- Acciarresi, M.; Bogousslavsky, J.; Paciaroni, M. Post-stroke fatigue: Epidemiology, clinical characteristics and treatment. Eur. Neurol. 2014, 72, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Wang, X.P.; Yang, G.Y. Sleep Disorders in Stroke: An Update on Management. Aging Dis. 2021, 12, 570–585. [Google Scholar] [CrossRef]
- Guo, J.; Wang, J.; Sun, W.; Liu, X. The advances of post-stroke depression: 2021 update. J. Neurol. 2022, 269, 1236–1249. [Google Scholar] [CrossRef]
- Al-Qazzaz, N.K.; Ali, S.H.; Ahmad, S.A.; Islam, S.; Mohamad, K. Cognitive impairment and memory dysfunction after a stroke diagnosis: A post-stroke memory assessment. Neuropsychiatr. Dis. Treat. 2014, 10, 1677–1691. [Google Scholar] [CrossRef]
- Lee, C.H.; Jeon, S.H.; Kim, M.J.; Ra, G.D.; Lee, Y.H.; Hong, S.H.; Shin, B.S.; Kang, H.G. Factors Affecting Post-Stroke Depression in Acute Ischemic Stroke Patients after 3 Months. J. Pers. Med. 2021, 11, 1178. [Google Scholar] [CrossRef]
- Liu, L.; Xu, M.; Marshall, I.J.; Wolfe, C.D.; Wang, Y.; O’Connell, M.D. Prevalence and natural history of depression after stroke: A systematic review and meta-analysis of observational studies. PLoS Med. 2023, 20, e1004200. [Google Scholar] [CrossRef]
- Cai, W.; Mueller, C.; Li, Y.-J.; Shen, W.-D.; Stewart, R. Post stroke depression and risk of stroke recurrence and mortality: A systematic review and meta-analysis. Ageing Res. Rev. 2019, 50, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Xiang, Y.; Yang, Y.; Zhang, N.; Wang, S.; Ungvari, G.S.; Chiu, H.F.K.; Tang, W.K.; Wang, Y.; Zhao, X.; et al. Depression after minor stroke: Prevalence and predictors. J. Psychosom. Res. 2015, 79, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Bour, A.; Rasquin, S.; Aben, I.; Boreas, A.; Limburg, M.; Verhey, F. A one-year follow-up study into the course of depression after stroke. J. Nutr. Health Aging 2010, 14, 488–493. [Google Scholar] [CrossRef]
- Hong, J.P.; Park, S.; Ahn, S.-H.; Kim, J.S. Factors associated with post-stroke suicidal death. J. Psychiatr. Res. 2018, 96, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Bartoli, F.; Pompili, M.; Lillia, N.; Crocamo, C.; Salemi, G.; Clerici, M.; Carrà, G. Rates and correlates of suicidal ideation among stroke survivors: A meta-analysis. J. Neurol. Neurosurg. Psychiatry 2017, 88, 498–504. [Google Scholar] [CrossRef]
- Kauhanen, M.; Korpelainen, J.T.; Hiltunen, P.; Brusin, E.; Mononen, H.; Määttä, R.; Nieminen, P.; Sotaniemi, K.A.; Myllylä, V.V. Poststroke depression correlates with cognitive impairment and neurological deficits. Stroke 1999, 30, 1875–1880. [Google Scholar] [CrossRef]
- Srivastava, A.; Taly, A.B.; Gupta, A.; Murali, T. Post-stroke depression: Prevalence and relationship with disability in chronic stroke survivors. Ann. Indian. Acad. Neurol. 2010, 13, 123–127. [Google Scholar] [CrossRef]
- Kim, E.S.; Kim, J.W.; Kang, H.J.; Bae, K.Y.; Kim, S.W.; Kim, J.T.; Park, M.S.; Cho, K.H.; Kim, J.M. Longitudinal Impact of Depression on Quality of Life in Stroke Patients. Psychiatry Investig. 2018, 15, 141–146. [Google Scholar] [CrossRef]
- Paparella, I.; Vandewalle, G.; Stagg, C.J.; Maquet, P. An integrated measure of GABA to characterize post-stroke plasticity. NeuroImage Clin. 2023, 39, 103463. [Google Scholar] [CrossRef]
- Nagy, E.E.; Frigy, A.; Szász, J.A.; Horváth, E. Neuroinflammation and microglia/macrophage phenotype modulate the molecular background of post-stroke depression: A literature review. Exp. Ther. Med. 2020, 20, 2510–2523. [Google Scholar] [CrossRef]
- Loubinoux, I.; Kronenberg, G.; Endres, M.; Schumann-Bard, P.; Freret, T.; Filipkowski, R.K.; Kaczmarek, L.; Popa-Wagner, A. Post-stroke depression: Mechanisms, translation and therapy. J. Cell Mol. Med. 2012, 16, 1961–1969. [Google Scholar] [CrossRef] [PubMed]
- Zirk, M.; Storm, V. Subjective Stroke Impact and Depressive Symptoms: Indications for a Moderating Role of Health-Related Locus of Control. Front. Psychiatry 2019, 10, 918. [Google Scholar] [CrossRef] [PubMed]
- Kronenberg, G.; Gertz, K.; Heinz, A.; Endres, M. Of mice and men: Modelling post-stroke depression experimentally. Br. J. Pharmacol. 2014, 171, 4673–4689. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.R.; Kim, H.N.; Pak, M.E.; Ahn, S.M.; Hong, K.H.; Shin, H.K.; Choi, B.T. Studies on the animal model of post-stroke depression and application of antipsychotic aripiprazole. Behav. Brain Res. 2015, 287, 294–303. [Google Scholar] [CrossRef]
- Wu, C.; Zhang, J.; Chen, Y. Study on the behavioral changes of a post-stroke depression rat model. Exp. Ther. Med. 2015, 10, 159–163. [Google Scholar] [CrossRef][Green Version]
- Braeuninger, S.; Kleinschnitz, C. Rodent models of focal cerebral ischemia: Procedural pitfalls and translational problems. Exp. Transl. Stroke Med. 2009, 1, 8. [Google Scholar] [CrossRef]
- Tao, X.; Yang, W.; Zhu, S.; Que, R.; Liu, C.; Fan, T.; Wang, J.; Mo, D.; Zhang, Z.; Tan, J.; et al. Models of poststroke depression and assessments of core depressive symptoms in rodents: How to choose? Exp. Neurol. 2019, 322, 113060. [Google Scholar] [CrossRef]
- Chen, D.; Wang, J.; Xing, Y.; Jia, P.; Zhang, Y.; Wang, J.; Ren, H.; Le, A.; Chen, X.; Wang, J. Behavioral assessment of post-stroke depression and anxiety in rodents. Brain Hemorrhages 2020, 1, 105–111. [Google Scholar] [CrossRef]
- Can, A.; Dao, D.T.; Arad, M.; Terrillion, C.E.; Piantadosi, S.C.; Gould, T.D. The mouse forced swim test. J. Vis. Exp. 2012, 59, e3638. [Google Scholar] [CrossRef]
- Liu, M.Y.; Yin, C.Y.; Zhu, L.J.; Zhu, X.H.; Xu, C.; Luo, C.X.; Chen, H.; Zhu, D.Y.; Zhou, Q.G. Sucrose preference test for measurement of stress-induced anhedonia in mice. Nat. Protoc. 2018, 13, 1686–1698. [Google Scholar] [CrossRef]
- Kraeuter, A.K.; Guest, P.C.; Sarnyai, Z. The Open Field Test for Measuring Locomotor Activity and Anxiety-Like Behavior. Methods Mol. Biol. 2019, 1916, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Balkaya, M.; Kröber, J.M.; Rex, A.; Endres, M. Assessing post-stroke behavior in mouse models of focal ischemia. J. Cereb. Blood Flow Metab. 2013, 33, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J.E.; Weber, S.; Jakob, R.; Chute, C.G. ICD-11: An international classification of diseases for the twenty-first century. BMC Med. Inform. Decis. Mak. 2021, 21, 206. [Google Scholar] [CrossRef] [PubMed]
- Tolentino, J.C.; Schmidt, S.L. DSM-5 Criteria and Depression Severity: Implications for Clinical Practice. Front. Psychiatry 2018, 9, 450. [Google Scholar] [CrossRef] [PubMed]
- Bos, E.H.; de Jonge, P.; Cox, R.F.A. Affective variability in depression: Revisiting the inertia-instability paradox. Br. J. Psychol. 2019, 110, 814–827. [Google Scholar] [CrossRef]
- Liang, J.; Yue, Y.; Jiang, H.; Geng, D.; Wang, J.; Lu, J.; Li, S.; Zhang, K.; Wu, A.; Yuan, Y. Genetic variations in the p11/tPA/BDNF pathway are associated with post stroke depression. J. Affect. Disord. 2018, 226, 313–325. [Google Scholar] [CrossRef]
- Zhou, Z.; Ding, X.; Yang, Q.; Hu, J.; Shang, X.; Huang, X.; Ge, L.; Zhou, T. Association between Single-Nucleotide Polymorphisms of the Tyrosine Kinase Receptor B (TrkB) and Post-Stroke Depression in China. PLoS ONE 2015, 10, e0144301. [Google Scholar] [CrossRef]
- Zhao, F.; Yue, Y.; Jiang, H.; Yuan, Y. Shared genetic risk factors for depression and stroke. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2019, 93, 55–70. [Google Scholar] [CrossRef]
- Okbay, A.; Baselmans, B.M.; De Neve, J.E.; Turley, P.; Nivard, M.G.; Fontana, M.A.; Meddens, S.F.; Linnér, R.K.; Rietveld, C.A.; Derringer, J.; et al. Genetic variants associated with subjective well-being, depressive symptoms, and neuroticism identified through genome-wide analyses. Nat. Genet. 2016, 48, 624–633. [Google Scholar] [CrossRef]
- Wang, Z.; Shi, Y.; Liu, F.; Jia, N.; Gao, J.; Pang, X.; Deng, F. Diversiform Etiologies for Post-stroke Depression. Front. Psychiatry 2018, 9, 761. [Google Scholar] [CrossRef] [PubMed]
- Caplan, S.; Alvidrez, J.; Paris, M.; Escobar, J.I.; Dixon, J.K.; Desai, M.M.; Whittemore, R.; Scahill, L.D. Subjective versus objective: An exploratory analysis of latino primary care patients with self-perceived depression who do not fulfill primary care evaluation of mental disorders patient health questionnaire criteria for depression. Prim. Care Companion J. Clin. Psychiatry 2010, 12, 26886. [Google Scholar] [CrossRef] [PubMed]
- Perna, L.; Zhang, Y.; Matias-Garcia, P.R.; Ladwig, K.-H.; Wiechmann, T.; Wild, B.; Waldenberger, M.; Schöttker, B.; Mons, U.; Ihle, A.; et al. Subjective mental health, incidence of depressive symptoms in later life, and the role of epigenetics: Results from two longitudinal cohort studies. Transl. Psychiatry 2020, 10, 323. [Google Scholar] [CrossRef] [PubMed]
- Dąbrowska-Bender, M.; Milewska, M.; Gołąbek, A.; Duda-Zalewska, A.; Staniszewska, A. The Impact of Ischemic Cerebral Stroke on the Quality of Life of Patients Based on Clinical, Social, and Psychoemotional Factors. J. Stroke Cerebrovasc. Dis. 2017, 26, 101–107. [Google Scholar] [CrossRef]
- Paprocka-Borowicz, M.; Wiatr, M.; Ciałowicz, M.; Borowicz, W.; Kaczmarek, A.; Marques, A.; Murawska-Ciałowicz, E. Influence of Physical Activity and Socio-Economic Status on Depression and Anxiety Symptoms in Patients after Stroke. Int. J. Environ. Res. Public Health 2021, 18, 8058. [Google Scholar] [CrossRef]
- Zhan, Q.; Kong, F. Mechanisms associated with post-stroke depression and pharmacologic therapy. Front. Neurol. 2023, 14, 1274709. [Google Scholar] [CrossRef]
- Naghavi, F.S.; Koffman, E.E.; Lin, B.; Du, J. Post-stroke neuronal circuits and mental illnesses. Int. J. Physiol. Pathophysiol. Pharmacol. 2019, 11, 1–11. [Google Scholar]
- Balami, J.S.; Chen, R.L.; Grunwald, I.Q.; Buchan, A.M. Neurological complications of acute ischaemic stroke. Lancet Neurol. 2011, 10, 357–371. [Google Scholar] [CrossRef]
- Strawbridge, R.; Young, A.H.; Cleare, A.J. Biomarkers for depression: Recent insights, current challenges and future prospects. Neuropsychiatr. Dis. Treat. 2017, 13, 1245–1262. [Google Scholar] [CrossRef]
- Ayerbe, L.; Ayis, S.; Wolfe, C.D.; Rudd, A.G. Natural history, predictors and outcomes of depression after stroke: Systematic review and meta-analysis. Br. J. Psychiatry 2013, 202, 14–21. [Google Scholar] [CrossRef]
- Hackett, M.L.; Pickles, K. Part I: Frequency of depression after stroke: An updated systematic review and meta-analysis of observational studies. Int. J. Stroke 2014, 9, 1017–1025. [Google Scholar] [CrossRef]
- Dong, L.; Sánchez, B.N.; Skolarus, L.E.; Stulberg, E.; Morgenstern, L.B.; Lisabeth, L.D. Sex difference in prevalence of depression after stroke. Neurology 2020, 94, e1973–e1983. [Google Scholar] [CrossRef] [PubMed]
- Mayman, N.A.; Tuhrim, S.; Jette, N.; Dhamoon, M.S.; Stein, L.K. Sex Differences in Post-Stroke Depression in the Elderly. J. Stroke Cerebrovasc. Dis. 2021, 30, 105948. [Google Scholar] [CrossRef]
- Driga, M.P.; Catalin, B.; Olaru, D.G.; Slowik, A.; Plesnila, N.; Hermann, D.M.; Popa-Wagner, A. The Need for New Biomarkers to Assist with Stroke Prevention and Prediction of Post-Stroke Therapy Based on Plasma-Derived Extracellular Vesicles. Biomedicines 2021, 9, 1226. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S. Post-stroke Mood and Emotional Disturbances: Pharmacological Therapy Based on Mechanisms. J. Stroke 2016, 18, 244–255. [Google Scholar] [CrossRef] [PubMed]
- Rupprechter, S.; Romaniuk, L.; Series, P.; Hirose, Y.; Hawkins, E.; Sandu, A.L.; Waiter, G.D.; McNeil, C.J.; Shen, X.; Harris, M.A.; et al. Blunted medial prefrontal cortico-limbic reward-related effective connectivity and depression. Brain 2020, 143, 1946–1956. [Google Scholar] [CrossRef]
- Li, G.; Liu, Y.; Zheng, Y.; Wu, Y.; Li, D.; Liang, X.; Chen, Y.; Cui, Y.; Yap, P.T.; Qiu, S.; et al. Multiscale neural modeling of resting-state fMRI reveals executive-limbic malfunction as a core mechanism in major depressive disorder. Neuroimage Clin. 2021, 31, 102758. [Google Scholar] [CrossRef]
- Soares, J.C.; Mann, J.J. The anatomy of mood disorders--review of structural neuroimaging studies. Biol. Psychiatry 1997, 41, 86–106. [Google Scholar] [CrossRef]
- Barker-Collo, S.L. Depression and anxiety 3 months post stroke: Prevalence and correlates. Arch. Clin. Neuropsychol. 2007, 22, 519–531. [Google Scholar] [CrossRef]
- Wei, N.; Yong, W.; Li, X.; Zhou, Y.; Deng, M.; Zhu, H.; Jin, H. Post-stroke depression and lesion location: A systematic review. J. Neurol. 2015, 262, 81–90. [Google Scholar] [CrossRef]
- Klingbeil, J.; Brandt, M.L.; Wawrzyniak, M.; Stockert, A.; Schneider, H.R.; Baum, P.; Hoffmann, K.T.; Saur, D. Association of Lesion Location and Depressive Symptoms Poststroke. Stroke 2022, 53, e467–e471. [Google Scholar] [CrossRef]
- Volz, M.; Ladwig, S.; Werheid, K. Gender differences in post-stroke depression: A longitudinal analysis of prevalence, persistence and predictive value of known risk factors. Neuropsychol. Rehabil. 2021, 31, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Poynter, B.; Shuman Hon, M.; Diaz-Granados, N.; Kapral, M.; Grace, S.L.; Stewart, D.E. Sex Differences in the Prevalence of Post-Stroke Depression: A Systematic Review. Psychosomatics 2009, 50, 563–569. [Google Scholar] [CrossRef]
- Mirolovics, Á.; Bokor, M.; Dobi, B.; Zsuga, J.; Bereczki, D. Socioeconomic Factors Predicting Depression Differ in the Acute Stage and at 1 year After Ischemic Stroke or TIA. J. Stroke Cerebrovasc. Dis. 2020, 29, 105241. [Google Scholar] [CrossRef]
- Gloria, M.U.; Jonah, O.E.; Olusanjo, A.C.; Chiebuka, O.E.; Nene, J.J.; Nwakego, A.U.; Chinyere, A.C. Post-Stroke Depression and Suicidal Ideations: Relationship with Gender and Marital Status: A Cross Sectional Study. J. Prim. Care Community Health 2024, 15, 21501319241233172. [Google Scholar] [CrossRef] [PubMed]
- Tento, T.; Kume, A.; Kumaso, S. Risk factors for stroke-related functional disability and mortality at Felege Hiwot Referral Hospital, Ethiopia. BMC Neurol. 2023, 23, 393. [Google Scholar] [CrossRef]
- Yoo, J.W.; Hong, B.Y.; Jo, L.; Kim, J.S.; Park, J.G.; Shin, B.K.; Lim, S.H. Effects of Age on Long-Term Functional Recovery in Patients with Stroke. Medicina 2020, 56, 451. [Google Scholar] [CrossRef] [PubMed]
- Lökk, J.; Delbari, A. Management of depression in elderly stroke patients. Neuropsychiatr. Dis. Treat. 2010, 6, 539–549. [Google Scholar] [CrossRef]
- Lindén, T.; Blomstrand, C.; Skoog, I. Depressive disorders after 20 months in elderly stroke patients: A case-control study. Stroke 2007, 38, 1860–1863. [Google Scholar] [CrossRef]
- Wolf, V.L.; Ergul, A. Progress and challenges in preclinical stroke recovery research. Brain Circ. 2021, 7, 230–240. [Google Scholar] [CrossRef]
- Chen, R.; Ovbiagele, B.; Feng, W. Diabetes and Stroke: Epidemiology, Pathophysiology, Pharmaceuticals and Outcomes. Am. J. Med. Sci. 2016, 351, 380–386. [Google Scholar] [CrossRef]
- Johansson, B.B. Hypertension mechanisms causing stroke. Clin. Exp. Pharmacol. Physiol. 1999, 26, 563–565. [Google Scholar] [CrossRef] [PubMed]
- Gajurel, B.P.; Gurung, A.; Ojha, R.; Rajbhandari, R.; Karn, R. Dyslipidemia and Obesity in Ischemic Stroke. Cureus 2023, 15, e45409. [Google Scholar] [CrossRef] [PubMed]
- Popa-Wagner, A.; Petcu, E.B.; Capitanescu, B.; Hermann, D.M.; Radu, E.; Gresita, A. Ageing as a risk factor for cerebral ischemia: Underlying mechanisms and therapy in animal models and in the clinic. Mech. Ageing Dev. 2020, 190, 111312. [Google Scholar] [CrossRef] [PubMed]
- Popa-Wagner, A.; Udristoiu, I.; Gresita, A.; Lledós, M.; Cadenas, I. Post-Stroke Depression: Genetics, Mechanisms, and Treatment; Springer International Publishing: Cham, Switzerland, 2022; pp. 4467–4478. [Google Scholar]
- Kohen, R.; Cain, K.C.; Mitchell, P.H.; Becker, K.; Buzaitis, A.; Millard, S.P.; Navaja, G.P.; Teri, L.; Tirschwell, D.; Veith, R. Association of serotonin transporter gene polymorphisms with poststroke depression. Arch. Gen. Psychiatry 2008, 65, 1296–1302. [Google Scholar] [CrossRef]
- Zhang, E.; Liao, P. Brain-derived neurotrophic factor and post-stroke depression. J. Neurosci. Res. 2020, 98, 537–548. [Google Scholar] [CrossRef]
- Qayyum, A.; Zai, C.C.; Hirata, Y.; Tiwari, A.K.; Cheema, S.; Nowrouzi, B.; Beitchman, J.H.; Kennedy, J.L. The Role of the Catechol-o-Methyltransferase (COMT) GeneVal158Met in Aggressive Behavior, a Review of Genetic Studies. Curr. Neuropharmacol. 2015, 13, 802–814. [Google Scholar] [CrossRef]
- Kwon, S.; Hartzema, A.G.; Duncan, P.W.; Min-Lai, S. Disability measures in stroke: Relationship among the Barthel Index, the Functional Independence Measure, and the Modified Rankin Scale. Stroke 2004, 35, 918–923. [Google Scholar] [CrossRef]
- Notsu, Y.; Nabika, T.; Park, H.Y.; Masuda, J.; Kobayashi, S. Evaluation of genetic risk factors for silent brain infarction. Stroke 1999, 30, 1881–1886. [Google Scholar] [CrossRef]
- Devereux, N.; Berns, A.M. Evaluation & Treatment of Psychological Effects of Stroke. Dela J. Public. Health 2023, 9, 62–69. [Google Scholar] [CrossRef]
- Ladwig, S.; Werheid, K.; Südmeyer, M.; Volz, M. Predictors of post-stroke depression: Validation of established risk factors and introduction of a dynamic perspective in two longitudinal studies. Front. Psychiatry 2023, 14, 1093918. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Rowan, M.; Momoh, O.; Ayerbe, L.; Evans, J.J.; Stott, D.J.; Quinn, T.J. Prevalence of pre-stroke depression and its association with post-stroke depression: A systematic review and meta-analysis. Psychol. Med. 2019, 49, 685–696. [Google Scholar] [CrossRef] [PubMed]
- Wist, S.; Clivaz, J.; Sattelmayer, M. Muscle strengthening for hemiparesis after stroke: A meta-analysis. Ann. Phys. Rehabil. Med. 2016, 59, 114–124. [Google Scholar] [CrossRef]
- Cuccurullo, S.J.; Fleming, T.K.; Zinonos, S.; Cosgrove, N.M.; Cabrera, J.; Kostis, J.B.; Greiss, C.; Ray, A.R.; Eckert, A.; Scarpati, R.; et al. Stroke Recovery Program with Modified Cardiac Rehabilitation Improves Mortality, Functional & Cardiovascular Performance. J. Stroke Cerebrovasc. Dis. 2022, 31, 106322. [Google Scholar] [CrossRef] [PubMed]
- Moore, N.; Reeder, S.; O’Keefe, S.; Alves-Stein, S.; Schneider, E.; Moloney, K.; Radford, K.; Lannin, N.A. “I’ve still got a job to go back to”: The importance of early vocational rehabilitation after stroke. Disabil. Rehabil. 2023, 46, 2769–2776. [Google Scholar] [CrossRef]
- Deepradit, S.; Powwattana, A.; Lagampan, S.; Thiangtham, W. Effectiveness of a family-based program for post-stroke patients and families: A cluster randomized controlled trial. Int. J. Nurs. Sci. 2023, 10, 446–455. [Google Scholar] [CrossRef]
- Pérez-de la Cruz, S. Influence of an Aquatic Therapy Program on Perceived Pain, Stress, and Quality of Life in Chronic Stroke Patients: A Randomized Trial. Int. J. Environ. Res. Public Health 2020, 17, 4796. [Google Scholar] [CrossRef]
- Dayuan, Z.; Lan, L.; Hui, C.; Huanjie, L.; Deliang, L.; Yihui, D. The effect of music as an intervention for post-stroke depression: A systematic review and meta-analysis. Complement. Ther. Med. 2022, 71, 102901. [Google Scholar] [CrossRef]
- Wang, S.B.; Wang, Y.Y.; Zhang, Q.E.; Wu, S.L.; Ng, C.H.; Ungvari, G.S.; Chen, L.; Wang, C.X.; Jia, F.J.; Xiang, Y.T. Cognitive behavioral therapy for post-stroke depression: A meta-analysis. J. Affect. Disord. 2018, 235, 589–596. [Google Scholar] [CrossRef]
- Gao, W.; Xue, F.; Yu, B.; Yu, S.; Zhang, W.; Huang, H. Repetitive transcranial magnetic stimulation for post-stroke depression: An overview of systematic reviews. Front. Neurol. 2023, 14, 930558. [Google Scholar] [CrossRef]
- Machová, K.; Procházková, R.; Říha, M.; Svobodová, I. The Effect of Animal-Assisted Therapy on the State of Patients’ Health After a Stroke: A Pilot Study. Int. J. Environ. Res. Public Health 2019, 16, 3272. [Google Scholar] [CrossRef] [PubMed]
- Zulkifli, W.; Shamsuddin, S.; Lim, T.H. Animal Robot Assisted-therapy for Rehabilitation of Patient with Post-Stroke Depression. IOP Conf. Ser. Mater. Sci. Eng. 2017, 210, 012005. [Google Scholar] [CrossRef]
- Remes, O.; Mendes, J.F.; Templeton, P. Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature. Brain Sci. 2021, 11, 1633. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; McCullough, L.D. Middle cerebral artery occlusion model in rodents: Methods and potential pitfalls. J. Biomed. Biotechnol. 2011, 2011, 464701. [Google Scholar] [CrossRef] [PubMed]
- Fluri, F.; Schuhmann, M.K.; Kleinschnitz, C. Animal models of ischemic stroke and their application in clinical research. Drug Des. Devel Ther. 2015, 9, 3445–3454. [Google Scholar] [CrossRef]
- Kuts, R.; Melamed, I.; Shiyntum, H.N.; Frank, D.; Grinshpun, J.; Zlotnik, A.; Brotfain, E.; Dubilet, M.; Natanel, D.; Boyko, M. A Middle Cerebral Artery Occlusion Technique for Inducing Post-stroke Depression in Rats. J. Vis. Exp. 2019, 147, e58875. [Google Scholar] [CrossRef]
- Liu, S.; Zhen, G.; Meloni, B.P.; Campbell, K.; Winn, H.R. RODENT STROKE MODEL GUIDELINES FOR PRECLINICAL STROKE TRIALS (1ST EDITION). J. Exp. Stroke Transl. Med. 2009, 2, 2–27. [Google Scholar] [CrossRef]
- Gresita, A.; Mihai, R.; Hermann, D.M.; Amandei, F.S.; Capitanescu, B.; Popa-Wagner, A. Effect of environmental enrichment and isolation on behavioral and histological indices following focal ischemia in old rats. GeroScience 2022, 44, 211–228. [Google Scholar] [CrossRef]
- Boboc, I.K.S.; Chirea, A.C.; Gheorman, V.; Gresita, A.; Balseanu, T.A.; Catalin, B.; Calina, D. Investigating the Neuroprotective and Neuroregenerative Effect of Trazodone Regarding Behavioral Recovery in a BL6C57 Mice Stroke Model. Curr. Health Sci. J. 2023, 49, 210–219. [Google Scholar] [CrossRef]
- Pinosanu, L.R.; Boboc, I.K.S.; Balseanu, T.A.; Gresita, A.; Hermann, D.M.; Popa-Wagner, A.; Catalin, B. Beam narrowing test: A motor index of post-stroke motor evaluation in an aged rat model of cerebral ischemia. J. Neural Transm. 2024, 131, 763–771. [Google Scholar] [CrossRef]
- Boboc, I.K.S.; Rotaru-Zavaleanu, A.D.; Calina, D.; Albu, C.V.; Catalin, B.; Turcu-Stiolica, A. A Preclinical Systematic Review and Meta-Analysis of Behavior Testing in Mice Models of Ischemic Stroke. Life 2023, 13, 567. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Chen, L.; Yang, L.; Hua, X.; Zhou, B.; Miao, Z.; Li, J.; Hu, H.; Namaka, M.; Kong, J.; et al. Combined use of spatial restraint stress and middle cerebral artery occlusion is a novel model of post-stroke depression in mice. Sci. Rep. 2015, 5, 16751. [Google Scholar] [CrossRef]
- Cunningham, C.J.; Wong, R.; Barrington, J.; Tamburrano, S.; Pinteaux, E.; Allan, S.M. Systemic conditioned medium treatment from interleukin-1 primed mesenchymal stem cells promotes recovery after stroke. Stem Cell Res. Ther. 2020, 11, 32. [Google Scholar] [CrossRef]
- Kawai, H.; Yamashita, T.; Ohta, Y.; Deguchi, K.; Nagotani, S.; Zhang, X.; Ikeda, Y.; Matsuura, T.; Abe, K. Tridermal tumorigenesis of induced pluripotent stem cells transplanted in ischemic brain. J. Cereb. Blood Flow. Metab. 2010, 30, 1487–1493. [Google Scholar] [CrossRef]
- Patkar, S.; Tate, R.; Modo, M.; Plevin, R.; Carswell, H.V. Conditionally immortalised neural stem cells promote functional recovery and brain plasticity after transient focal cerebral ischaemia in mice. Stem Cell Res. 2012, 8, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Sun, R.; Peng, M.; Xu, P.; Huang, F.; Xie, Y.; Li, J.; Hong, Y.; Guo, H.; Liu, Q.; Zhu, W. Low-density lipoprotein receptor (LDLR) regulates NLRP3-mediated neuronal pyroptosis following cerebral ischemia/reperfusion injury. J. Neuroinflamm. 2020, 17, 330. [Google Scholar] [CrossRef]
- Cao, Z.; Balasubramanian, A.; Pedersen, S.E.; Romero, J.; Pautler, R.G.; Marrelli, S.P. TRPV1-mediated Pharmacological Hypothermia Promotes Improved Functional Recovery Following Ischemic Stroke. Sci. Rep. 2017, 7, 17685. [Google Scholar] [CrossRef] [PubMed]
- Suenaga, J.; Hu, X.; Pu, H.; Shi, Y.; Hassan, S.H.; Xu, M.; Leak, R.K.; Stetler, R.A.; Gao, Y.; Chen, J. White matter injury and microglia/macrophage polarization are strongly linked with age-related long-term deficits in neurological function after stroke. Exp. Neurol. 2015, 272, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Ding, Z.; Gao, J.; Feng, Y.; Wang, M.; Zhao, H.; Wu, R.; Zheng, X.; Feng, X.; Lai, M. Electroacupuncture Ameliorates Depression-Like Behaviors in Post-Stroke Rats via Activating AMPK-Mediated Mitochondrial Function. Neuropsychiatr. Dis. Treat. 2023, 19, 2657–2671. [Google Scholar] [CrossRef]
- Wang, S.; Sun, H.; Liu, S.; Wang, T.; Guan, J.; Jia, J. Role of hypothalamic cannabinoid receptors in post-stroke depression in rats. Brain Res. Bull. 2016, 121, 91–97. [Google Scholar] [CrossRef]
- Qian, L.; Huang, S.; Liu, X.; Jiang, Y.; Jiang, Y.; Hu, Y.; Yang, Z. Morroniside improves the symptoms of post-stroke depression in mice through the BDNF signaling pathway mediated by MiR-409-3p. Phytomedicine 2024, 123, 155224. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Liang, L. Vitamin D3/vitamin D receptor signaling mitigates symptoms of post-stroke depression in mice by upregulating hippocampal BDNF expression. Neurosci. Res. 2021, 170, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Gaignier, F.; Legrand-Frossi, C.; Stragier, E.; Mathiot, J.; Merlin, J.L.; Cohen-Salmon, C.; Lanfumey, L.; Frippiat, J.P. A Model of Chronic Exposure to Unpredictable Mild Socio-Environmental Stressors Replicates Some Spaceflight-Induced Immunological Changes. Front. Physiol. 2018, 9, 514. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Li, A.; Yang, Q.; Li, J.; Zheng, L.; Wang, G.; Sun, Y.; Huang, Y.; Zhang, M.; Song, Z.; et al. Matrine alleviates depressive-like behaviors via modulating microbiota–gut–brain axis in CUMS-induced mice. J. Transl. Med. 2023, 21, 145. [Google Scholar] [CrossRef]
- Yan, W.; Dong, Z.; Zhao, D.; Li, J.; Zeng, T.; Mo, C.; Gao, L.; Lv, Z. Xiaoyaosan Exerts Antidepressant Effect by Downregulating RAGE Expression in Cingulate Gyrus of Depressive-Like Mice. Front. Pharmacol. 2021, 12, 703965. [Google Scholar] [CrossRef] [PubMed]
- Mușat, M.I.; Mitran, S.I.; Udriștoiu, I.; Albu, C.V.; Cătălin, B. The impact of stress on the behavior of C57BL/6 mice with liver injury: A comparative study. Front. Behav. Neurosci. 2024, 18, 1358964. [Google Scholar] [CrossRef]
- Wu, J.; Li, J.; Gaurav, C.; Muhammad, U.; Chen, Y.; Li, X.; Chen, J.; Wang, Z. CUMS and dexamethasone induce depression-like phenotypes in mice by differentially altering gut microbiota and triggering macroglia activation. Gen. Psychiatr. 2021, 34, e100529. [Google Scholar] [CrossRef]
- Wang, Y.-l.; Wu, H.-r.; Zhang, S.-s.; Xiao, H.-l.; Yu, J.; Ma, Y.-y.; Zhang, Y.-d.; Liu, Q. Catalpol ameliorates depressive-like behaviors in CUMS mice via oxidative stress-mediated NLRP3 inflammasome and neuroinflammation. Transl. Psychiatry 2021, 11, 353. [Google Scholar] [CrossRef]
- Wang, G.; Lei, C.; Tian, Y.; Wang, Y.; Zhang, L.; Zhang, R. Rb1, the Primary Active Ingredient in Panax ginseng C.A. Meyer, Exerts Antidepressant-Like Effects via the BDNF-Trkb-CREB Pathway. Front. Pharmacol. 2019, 10, 1034. [Google Scholar] [CrossRef]
- Wen, G.; Yao, H.; Li, Y.; Ding, R.; Ren, X.; Tan, Y.; Ren, W.; Yu, H.; Zhan, X.; Wang, X.; et al. Regulation of Tau Protein on the Antidepressant Effects of Ketamine in the Chronic Unpredictable Mild Stress Model. Front. Psychiatry 2019, 10, 287. [Google Scholar] [CrossRef]
- Li, M.; Fu, Q.; Li, Y.; Li, S.; Xue, J.; Ma, S. Emodin opposes chronic unpredictable mild stress induced depressive-like behavior in mice by upregulating the levels of hippocampal glucocorticoid receptor and brain-derived neurotrophic factor. Fitoterapia 2014, 98, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Wang, H.; Peng, J.; Qing, D.; Zhang, X.; Guo, D.; Meng, P.; Luo, Z.; Wang, X.; Peng, Q. Acacetin protects against depression-associated dry eye disease by regulating ubiquitination of NLRP3 through gp78 signal. Front. Pharmacol. 2022, 13, 984475. [Google Scholar] [CrossRef]
- Wassouf, Z.; Hentrich, T.; Casadei, N.; Jaumann, M.; Knipper, M.; Riess, O.; Schulze-Hentrich, J.M. Distinct Stress Response and Altered Striatal Transcriptome in Alpha-Synuclein Overexpressing Mice. Front. Neurosci. 2018, 12, 1033. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Gu, J.H.; Liu, L.; Liu, Y.; Tang, W.Q.; Ji, C.H.; Guan, W.; Zhao, X.Y.; Sun, Y.F.; Xu, D.W.; et al. Hippocampal PPARα Plays a Role in the Pharmacological Mechanism of Vortioxetine, a Multimodal-Acting Antidepressant. Front. Pharmacol. 2021, 12, 673221. [Google Scholar] [CrossRef]
- Kalliokoski, O.; Teilmann, A.C.; Jacobsen, K.R.; Abelson, K.S.; Hau, J. The lonely mouse—Single housing affects serotonergic signaling integrity measured by 8-OH-DPAT-induced hypothermia in male mice. PLoS ONE 2014, 9, e111065. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, P.; Liu, H.; Yao, H.; Yao, S.; Yuan, S.Y.; Zhang, J.C. Hyperforin improves post-stroke social isolation-induced exaggeration of PSD and PSA via TGF-β. Int. J. Mol. Med. 2019, 43, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.H.; Zhang, N.; Li, W.Y.; Fang, M.R.; Zhang, H.; Fang, Y.S.; Ding, M.X.; Fu, X.Y. Overexpression of brain-derived neurotrophic factor in the hippocampus protects against post-stroke depression. Neural Regen. Res. 2015, 10, 1427–1432. [Google Scholar] [CrossRef]
- Niu, L.; Jin, X.; Zhang, Y.; Liu, B.; Li, C. Feasibility of focal cerebral ischemia and reperfusion surgery combined with chronic unpredictable mild stress to simulate the post-stroke depressive state in rats. Behav. Brain Funct. 2015, 11, 39. [Google Scholar] [CrossRef]
- Wang, A.R.; Mi, L.F.; Zhang, Z.L.; Hu, M.Z.; Zhao, Z.Y.; Liu, B.; Li, Y.B.; Zheng, S. Saikosaponin A improved depression-like behavior and inhibited hippocampal neuronal apoptosis after cerebral ischemia through p-CREB/BDNF pathway. Behav. Brain Res. 2021, 403, 113138. [Google Scholar] [CrossRef]
- Aarsland, T.I.; Landaas, E.T.; Hegvik, T.A.; Ulvik, A.; Halmøy, A.; Ueland, P.M.; Haavik, J. Serum concentrations of kynurenines in adult patients with attention-deficit hyperactivity disorder (ADHD): A case-control study. Behav. Brain Funct. 2015, 11, 36. [Google Scholar] [CrossRef]
- Pałucha-Poniewiera, A.; Podkowa, K.; Rafało-Ulińska, A. The group II mGlu receptor antagonist LY341495 induces a rapid antidepressant-like effect and enhances the effect of ketamine in the chronic unpredictable mild stress model of depression in C57BL/6J mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 109, 110239. [Google Scholar] [CrossRef]
- Zain, M.A.; Pandy, V.; Majeed, A.B.A.; Wong, W.F.; Mohamed, Z. Chronic restraint stress impairs sociability but not social recognition and spatial memoryin C57BL/6J mice. Exp. Anim. 2019, 68, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Zhi, L.; Zhang, F.; Liu, H.; Jiang, X.; Zhang, Y.; Yang, Q.; Zhang, X.; Liu, M.; Zhang, Z.; Song, J. CRS induces depression-like behavior after MCAO in rats possibly by activating p38 MAPK. Behav. Brain Res. 2023, 437, 114104. [Google Scholar] [CrossRef] [PubMed]
- Tekam, C.S.; Shinde, S.; Ranjana, P.; Mahto, S. Bilateral Common Carotid Artery Occlusion: Stroke Model; Springer International Publishing: Cham, Switzerland, 2021; pp. 41–56. [Google Scholar]
- Di Lorenzo, A.; Nabavi, S.F.; Sureda, A.; Moghaddam, A.H.; Khanjani, S.; Arcidiaco, P.; Nabavi, S.M.; Daglia, M. Antidepressive-like effects and antioxidant activity of green tea and GABA green tea in a mouse model of post-stroke depression. Mol. Nutr. Food Res. 2016, 60, 566–579. [Google Scholar] [CrossRef] [PubMed]
- Daglia, M.; Di Lorenzo, A.; Nabavi, S.F.; Sureda, A.; Khanjani, S.; Moghaddam, A.H.; Braidy, N.; Nabavi, S.M. Improvement of Antioxidant Defences and Mood Status by Oral GABA Tea Administration in a Mouse Model of Post-Stroke Depression. Nutrients 2017, 9, 446. [Google Scholar] [CrossRef]
- Nabavi, S.M.; Nabavi, S.F.; Sureda, A.; Caprioli, G.; Iannarelli, R.; Sokeng, A.J.T.; Braidy, N.; Khanjani, S.; Moghaddam, A.H.; Atanasov, A.G.; et al. The water extract of tutsan (Hypericum androsaemum L.) red berries exerts antidepressive-like effects and in vivo antioxidant activity in a mouse model of post-stroke depression. Biomed. Pharmacother. 2018, 99, 290–298. [Google Scholar] [CrossRef]
- Aggarwal, A.; Gaur, V.; Kumar, A. Nitric oxide mechanism in the protective effect of naringin against post-stroke depression (PSD) in mice. Life Sci. 2010, 86, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.R.; Choi, B.; Paul, S.; Seo, J.H.; Back, D.B.; Han, J.S.; Choi, D.H.; Kwon, K.J.; Shin, C.Y.; Lee, J.; et al. Depressive-like behaviors in a rat model of chronic cerebral hypoperfusion. Transl. Stroke Res. 2015, 6, 207–214. [Google Scholar] [CrossRef]
- Hu, G.; Zhou, C.; Wang, J.; Ma, X.; Ma, H.; Yu, H.; Peng, Z.; Huang, J.; Cai, M. Electroacupuncture treatment ameliorates depressive-like behavior and cognitive dysfunction via CB1R dependent mitochondria biogenesis after experimental global cerebral ischemic stroke. Front. Cell Neurosci. 2023, 17, 1135227. [Google Scholar] [CrossRef]
- Molcho, L.; Ben-Zur, T.; Barhum, Y.; Offen, D. DJ-1 based peptide, ND-13, promote functional recovery in mouse model of focal ischemic injury. PLoS ONE 2018, 13, e0192954. [Google Scholar] [CrossRef]
- Vahid-Ansari, F.; Lagace, D.C.; Albert, P.R. Persistent post-stroke depression in mice following unilateral medial prefrontal cortical stroke. Transl. Psychiatry 2016, 6, e863. [Google Scholar] [CrossRef] [PubMed]
- Happ, D.; Tasker, R.A.; Wegener, G.P. 2.038—Endothelin-1 injection into the left medial prefrontal cortex induces anxiety-like symptoms—A possible model for post-stroke anxiety? Eur. Neuropsychopharmacol. 2018, 28, S48–S49. [Google Scholar] [CrossRef]
- Sommer, C.J. Ischemic stroke: Experimental models and reality. Acta Neuropathol. 2017, 133, 245–261. [Google Scholar] [CrossRef]
- Kim, G.W.; Sugawara, T.; Chan, P.H. Involvement of oxidative stress and caspase-3 in cortical infarction after photothrombotic ischemia in mice. J. Cereb. Blood Flow. Metab. 2000, 20, 1690–1701. [Google Scholar] [CrossRef] [PubMed]
- Talley Watts, L.; Zheng, W.; Garling, R.J.; Frohlich, V.C.; Lechleiter, J.D. Rose Bengal Photothrombosis by Confocal Optical Imaging In Vivo: A Model of Single Vessel Stroke. J. Vis. Exp. 2015, 100, e52794. [Google Scholar] [CrossRef]
- Wester, P.; Watson, B.D.; Prado, R.; Dietrich, W.D. A photothrombotic ‘ring’ model of rat stroke-in-evolution displaying putative penumbral inversion. Stroke 1995, 26, 444–450. [Google Scholar] [CrossRef]
- Lunardi Baccetto, S.; Lehmann, C. Microcirculatory Changes in Experimental Models of Stroke and CNS-Injury Induced Immunodepression. Int. J. Mol. Sci. 2019, 20, 5184. [Google Scholar] [CrossRef]
- Lindholm, J.S.; Castrén, E. Mice with altered BDNF signaling as models for mood disorders and antidepressant effects. Front. Behav. Neurosci. 2014, 8, 143. [Google Scholar] [CrossRef]
- Holmes, A.; Murphy, D.L.; Crawley, J.N. Abnormal behavioral phenotypes of serotonin transporter knockout mice: Parallels with human anxiety and depression. Biol. Psychiatry 2003, 54, 953–959. [Google Scholar] [CrossRef]
- Craske, M.G.; Meuret, A.E.; Ritz, T.; Treanor, M.; Dour, H.J. Treatment for Anhedonia: A Neuroscience Driven Approach. Depress. Anxiety 2016, 33, 927–938. [Google Scholar] [CrossRef]
- Sah, A.; Schmuckermair, C.; Sartori, S.B.; Gaburro, S.; Kandasamy, M.; Irschick, R.; Klimaschewski, L.; Landgraf, R.; Aigner, L.; Singewald, N. Anxiety- rather than depression-like behavior is associated with adult neurogenesis in a female mouse model of higher trait anxiety- and comorbid depression-like behavior. Transl. Psychiatry 2012, 2, e171. [Google Scholar] [CrossRef] [PubMed]
- Labenz, C.; Huber, Y.; Michel, M.; Nagel, M.; Galle, P.R.; Kostev, K.; Schattenberg, J.M. Nonalcoholic Fatty Liver Disease Increases the Risk of Anxiety and Depression. Hepatol. Commun. 2020, 4, 1293–1301. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.H.; Wang, S. Strain differences in the chronic mild stress animal model of depression. Behav. Brain Res. 2010, 213, 94–102. [Google Scholar] [CrossRef]
- Primo, M.J.; Fonseca-Rodrigues, D.; Almeida, A.; Teixeira, P.M.; Pinto-Ribeiro, F. Sucrose preference test: A systematic review of protocols for the assessment of anhedonia in rodents. Eur. Neuropsychopharmacol. 2023, 77, 80–92. [Google Scholar] [CrossRef]
- Wang, L.; Cui, Q.; Liu, J.; Zou, H. Emotion Reactivity and Suicide Risk in Patients With Depression: The Mediating Role of Non-Suicidal Self-Injury and Moderating Role of Childhood Neglect. Front. Psychiatry 2021, 12, 707181. [Google Scholar] [CrossRef] [PubMed]
- Busquet, P.; Nguyen, N.K.; Schmid, E.; Tanimoto, N.; Seeliger, M.W.; Ben-Yosef, T.; Mizuno, F.; Akopian, A.; Striessnig, J.; Singewald, N. CaV1.3 L-type Ca2+ channels modulate depression-like behaviour in mice independent of deaf phenotype. Int. J. Neuropsychopharmacol. 2010, 13, 499–513. [Google Scholar] [CrossRef]
- Seo, J.S.; Wei, J.; Qin, L.; Kim, Y.; Yan, Z.; Greengard, P. Cellular and molecular basis for stress-induced depression. Mol. Psychiatry 2017, 22, 1440–1447. [Google Scholar] [CrossRef]
- Sasaki, K.; Halder, S.K.; Matsunaga, H.; Ueda, H. Beneficial actions of prothymosin alpha-mimetic hexapeptide on central post-stroke pain, reduced social activity, learning-deficit and depression following cerebral ischemia in mice. Peptides 2020, 126, 170265. [Google Scholar] [CrossRef]
- Partoazar, A.; Seyyedian, Z.; Zamanian, G.; Saffari, P.M.; Muhammadnejad, A.; Dehpour, A.R.; Goudarzi, R. Neuroprotective phosphatidylserine liposomes alleviate depressive-like behavior related to stroke through neuroinflammation attenuation in the mouse hippocampus. Psychopharmacology 2021, 238, 1531–1539. [Google Scholar] [CrossRef]
- Wu, D.; Zhang, G.; Zhao, C.; Yang, Y.; Miao, Z.; Xu, X. Interleukin-18 from neurons and microglia mediates depressive behaviors in mice with post-stroke depression. Brain Behav. Immun. 2020, 88, 411–420. [Google Scholar] [CrossRef]
- Weiss, S.M.; Wadsworth, G.; Fletcher, A.; Dourish, C.T. Utility of ethological analysis to overcome locomotor confounds in elevated maze models of anxiety. Neurosci. Biobehav. Rev. 1998, 23, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, J.; Niu, R.; Manthari, R.K.; Yang, K.; Wang, J. Effect of fluoride exposure on anxiety- and depression-like behavior in mouse. Chemosphere 2019, 215, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, P.; O’Hara, K.; Xu, Z.; Yang, Y. HFD-induced energy states-dependent bidirectional control of anxiety levels in mice. Int. J. Obes. 2017, 41, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Pitzer, C.; La Porta, C.; Treede, R.D.; Tappe-Theodor, A. Inflammatory and neuropathic pain conditions do not primarily evoke anxiety-like behaviours in C57BL/6 mice. Eur. J. Pain. 2019, 23, 285–306. [Google Scholar] [CrossRef] [PubMed]
- Blasco-Serra, A.; González-Soler, E.M.; Cervera-Ferri, A.; Teruel-Martí, V.; Valverde-Navarro, A.A. A standardization of the Novelty-Suppressed Feeding Test protocol in rats. Neurosci. Lett. 2017, 658, 73–78. [Google Scholar] [CrossRef]
- Pietri, M.; Djillani, A.; Mazella, J.; Borsotto, M.; Heurteaux, C. First evidence of protective effects on stroke recovery and post-stroke depression induced by sortilin-derived peptides. Neuropharmacology 2019, 158, 107715. [Google Scholar] [CrossRef]
- Bourin, M.; Hascoët, M. The mouse light/dark box test. Eur. J. Pharmacol. 2003, 463, 55–65. [Google Scholar] [CrossRef]
- Takao, K.; Miyakawa, T. Light/dark transition test for mice. J. Vis. Exp. 2006, 1, e104. [Google Scholar] [CrossRef]
- Njung’e, K.u.; Handley, S.L. Evaluation of marble-burying behavior as a model of anxiety. Pharmacol. Biochem. Behav. 1991, 38, 63–67. [Google Scholar] [CrossRef]
- Bahi, A.; Dreyer, J.L. Hippocampus-specific deletion of tissue plasminogen activator “tPA” in adult mice impairs depression- and anxiety-like behaviors. Eur. Neuropsychopharmacol. 2012, 22, 672–682. [Google Scholar] [CrossRef]
- Dorninger, F.; Zeitler, G.; Berger, J. Nestlet Shredding and Nest Building Tests to Assess Features of Psychiatric Disorders in Mice. Bio Protoc. 2020, 10, e3863. [Google Scholar] [CrossRef] [PubMed]
- Teo, A.R.; Nelson, S.; Strange, W.; Kubo, H.; Katsuki, R.; Kurahara, K.; Kanba, S.; Kato, T.A. Social withdrawal in major depressive disorder: A case-control study of hikikomori in japan. J. Affect. Disord. 2020, 274, 1142–1146. [Google Scholar] [CrossRef] [PubMed]
- Katayama, Y.; Nishiyama, M.; Shoji, H.; Ohkawa, Y.; Kawamura, A.; Sato, T.; Suyama, M.; Takumi, T.; Miyakawa, T.; Nakayama, K.I. CHD8 haploinsufficiency results in autistic-like phenotypes in mice. Nature 2016, 537, 675–679. [Google Scholar] [CrossRef]
- Peça, J.; Feliciano, C.; Ting, J.T.; Wang, W.; Wells, M.F.; Venkatraman, T.N.; Lascola, C.D.; Fu, Z.; Feng, G. Shank3 mutant mice display autistic-like behaviours and striatal dysfunction. Nature 2011, 472, 437–442. [Google Scholar] [CrossRef]
- Wilson, C.A.; Koenig, J.I. Social interaction and social withdrawal in rodents as readouts for investigating the negative symptoms of schizophrenia. Eur. Neuropsychopharmacol. 2014, 24, 759–773. [Google Scholar] [CrossRef] [PubMed]
- Kaidanovich-Beilin, O.; Lipina, T.; Vukobradovic, I.; Roder, J.; Woodgett, J.R. Assessment of social interaction behaviors. J. Vis. Exp. 2011, 48, e2473. [Google Scholar] [CrossRef]
- Ni, R.J.; Tian, Y.; Dai, X.Y.; Zhao, L.S.; Wei, J.X.; Zhou, J.N.; Ma, X.H.; Li, T. Social avoidance behavior in male tree shrews and prosocial behavior in male mice toward unfamiliar conspecifics in the laboratory. Zool. Res. 2020, 41, 258–272. [Google Scholar] [CrossRef]
- Liu, Y.; Deng, S.L.; Li, L.X.; Zhou, Z.X.; Lv, Q.; Wang, Z.Y.; Wang, F.; Chen, J.G. A circuit from dorsal hippocampal CA3 to parvafox nucleus mediates chronic social defeat stress-induced deficits in preference for social novelty. Sci. Adv. 2022, 8, eabe8828. [Google Scholar] [CrossRef]
- Piccin, A.; Contarino, A. Long-lasting pseudo-social aggressive behavior in opiate-withdrawn mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 2020, 97, 109780. [Google Scholar] [CrossRef]
- Alsaeed, I.; Al-Somali, F.; Sakhnini, L.; Aljarallah, O.S.; Hamdan, R.M.; Bubishate, S.A.; Sarfaraz, Z.K.; Kamal, A. Autism-relevant social abnormalities in mice exposed perinatally to extremely low frequency electromagnetic fields. Int. J. Dev. Neurosci. 2014, 37, 58–64. [Google Scholar] [CrossRef]
- Bevins, R.A.; Besheer, J. Object recognition in rats and mice: A one-trial non-matching-to-sample learning task to study ‘recognition memory’. Nat. Protoc. 2006, 1, 1306–1311. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, H.; Tsuboi, A. Olfactory Habituation-dishabituation Test (Mouse). Bio Protoc. 2017, 7, e2154. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Wang, W.; Pan, Y.W.; Lu, S.; Xia, Z. Methods to measure olfactory behavior in mice. Curr. Protoc. Toxicol. 2015, 63, 11.18.11–11.18.21. [Google Scholar] [CrossRef]
- Choi, K.W.; Kim, Y.K.; Jeon, H.J. Comorbid Anxiety and Depression: Clinical and Conceptual Consideration and Transdiagnostic Treatment. Adv. Exp. Med. Biol. 2020, 1191, 219–235. [Google Scholar] [CrossRef]
- Koolhaas, J.M.; Coppens, C.M.; de Boer, S.F.; Buwalda, B.; Meerlo, P.; Timmermans, P.J. The resident-intruder paradigm: A standardized test for aggression, violence and social stress. J. Vis. Exp. 2013, 77, e4367. [Google Scholar] [CrossRef]
- Fan, Z.; Zhu, H.; Zhou, T.; Wang, S.; Wu, Y.; Hu, H. Using the tube test to measure social hierarchy in mice. Nat. Protoc. 2019, 14, 819–831. [Google Scholar] [CrossRef]
- Yang, C.R.; Bai, Y.Y.; Ruan, C.S.; Zhou, H.F.; Liu, D.; Wang, X.F.; Shen, L.J.; Zheng, H.Y.; Zhou, X.F. Enhanced aggressive behaviour in a mouse model of depression. Neurotox. Res. 2015, 27, 129–142. [Google Scholar] [CrossRef]
- Douglas, K.M.; Gallagher, P.; Robinson, L.J.; Carter, J.D.; McIntosh, V.V.; Frampton, C.M.; Watson, S.; Young, A.H.; Ferrier, I.N.; Porter, R.J. Prevalence of cognitive impairment in major depression and bipolar disorder. Bipolar Disord. 2018, 20, 260–274. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, M.; Liu, H.; Zhu, R.; He, H.; Zhou, Y.; Zhang, Y.; Li, C.; Liang, D.; Zeng, Q.; et al. Bone marrow mesenchymal stem cell-derived exosomes attenuate cerebral ischemia-reperfusion injury-induced neuroinflammation and pyroptosis by modulating microglia M1/M2 phenotypes. Exp. Neurol. 2021, 341, 113700. [Google Scholar] [CrossRef]
- Balseanu, A.T.; Buga, A.M.; Catalin, B.; Wagner, D.C.; Boltze, J.; Zagrean, A.M.; Reymann, K.; Schaebitz, W.; Popa-Wagner, A. Multimodal Approaches for Regenerative Stroke Therapies: Combination of Granulocyte Colony-Stimulating Factor with Bone Marrow Mesenchymal Stem Cells is Not Superior to G-CSF Alone. Front. Aging Neurosci. 2014, 6, 130. [Google Scholar] [CrossRef]
- Yang, K.; Tan, Y.; Wang, F.; Zhang, Q.; Sun, P.; Zhang, Y.; Yao, N.; Zhao, Y.; Wang, X.; Fan, A.; et al. The improvement of spatial memory deficits in APP/V717I transgenic mice by chronic anti-stroke herb treatment. Exp. Biol. Med. 2014, 239, 1007–1017. [Google Scholar] [CrossRef]
- Pitts, M.W. Barnes Maze Procedure for Spatial Learning and Memory in Mice. Bio Protoc. 2018, 8, e2744. [Google Scholar] [CrossRef]
- Kraeuter, A.K.; Guest, P.C.; Sarnyai, Z. The Y-Maze for Assessment of Spatial Working and Reference Memory in Mice. Methods Mol. Biol. 2019, 1916, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Huo, K.; Wei, M.; Zhang, M.; Wang, Z.; Pan, P.; Shaligram, S.S.; Huang, J.; Prado, L.B.D.; Wong, J.; Su, H. Reduction of neuroinflammation alleviated mouse post bone fracture and stroke memory dysfunction. J. Cereb. Blood Flow. Metab. 2021, 41, 2162–2173. [Google Scholar] [CrossRef]
- Ahnstedt, H.; Patrizz, A.; Chauhan, A.; Roy-O’Reilly, M.; Furr, J.W.; Spychala, M.S.; D’Aigle, J.; Blixt, F.W.; Zhu, L.; Bravo Alegria, J.; et al. Sex differences in T cell immune responses, gut permeability and outcome after ischemic stroke in aged mice. Brain Behav. Immun. 2020, 87, 556–567. [Google Scholar] [CrossRef] [PubMed]
- Toshkezi, G.; Kyle, M.; Longo, S.L.; Chin, L.S.; Zhao, L.R. Brain repair by hematopoietic growth factors in the subacute phase of traumatic brain injury. J. Neurosurg. 2018, 129, 1286–1294. [Google Scholar] [CrossRef] [PubMed]
- Olton, D.S.; Collison, C.; Werz, M.A. Spatial memory and radial arm maze performance of rats. Learn. Motiv. 1977, 8, 289–314. [Google Scholar] [CrossRef]
- Kohler, J.; Mei, J.; Banneke, S.; Winter, Y.; Endres, M.; Emmrich, J.V. Assessing spatial learning and memory in mice: Classic radial maze versus a new animal-friendly automated radial maze allowing free access and not requiring food deprivation. Front. Behav. Neurosci. 2022, 16, 1013624. [Google Scholar] [CrossRef]
- Borlongan, C.V.; Cahill, D.W.; Sanberg, P.R. Locomotor and passive avoidance deficits following occlusion of the middle cerebral artery. Physiol. Behav. 1995, 58, 909–917. [Google Scholar] [CrossRef]
- Senechal, Y.; Kelly, P.H.; Dev, K.K. Amyloid precursor protein knockout mice show age-dependent deficits in passive avoidance learning. Behav. Brain Res. 2008, 186, 126–132. [Google Scholar] [CrossRef]
- Singh, N.; Ma, B.; Leonardo, C.C.; Ahmad, A.S.; Narumiya, S.; Doré, S. Role of PGE2 EP1 receptor in intracerebral hemorrhage-induced brain injury. Neurotox. Res. 2013, 24, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Deacon, R.M. Measuring motor coordination in mice. J. Vis. Exp. 2013, 75, e2609. [Google Scholar] [CrossRef]
- Jacobs, J.R.; Carey, M.R. Move Over Rotarod, Here Comes RotaWheel. Neuroscience 2021, 466, 258–259. [Google Scholar] [CrossRef]
- Nguyen, K.P.; Sharma, A.; Gil-Silva, M.; Gittis, A.H.; Chase, S.M. Distinct Kinematic Adjustments over Multiple Timescales Accompany Locomotor Skill Development in Mice. Neuroscience 2021, 466, 260–272. [Google Scholar] [CrossRef]
- Syeara, N.; Bagchi, S.; Al Shoyaib, A.; Karamyan, S.T.; Alamri, F.F.; Karamyan, V.T. The Finer Aspects of Grid-Walking and Cylinder Tests for Experimental Stroke Recovery Studies in Mice. Methods Mol. Biol. 2023, 2616, 345–353. [Google Scholar] [CrossRef]
- Zalewska, K.; Pietrogrande, G.; Ong, L.K.; Abdolhoseini, M.; Kluge, M.; Johnson, S.J.; Walker, F.R.; Nilsson, M. Sustained administration of corticosterone at stress-like levels after stroke suppressed glial reactivity at sites of thalamic secondary neurodegeneration. Brain Behav. Immun. 2018, 69, 210–222. [Google Scholar] [CrossRef]
- Modo, M.; Stroemer, R.P.; Tang, E.; Veizovic, T.; Sowniski, P.; Hodges, H. Neurological sequelae and long-term behavioural assessment of rats with transient middle cerebral artery occlusion. J. Neurosci. Methods 2000, 104, 99–109. [Google Scholar] [CrossRef]
- Hayashi, K.; Hasegawa, Y.; Takemoto, Y.; Cao, C.; Mukasa, A.; Kim-Mitsuyama, S. Enhanced oxidative stress contributes to worse prognosis and delayed neurofunctional recovery after striatal intracerebral hemorrhage in 5XFAD mice. Eur. J. Neurosci. 2020, 51, 1806–1814. [Google Scholar] [CrossRef] [PubMed]
- Carter, R.J.; Morton, J.; Dunnett, S.B. Motor coordination and balance in rodents. Curr. Protoc. Neurosci. 2001, 15, 8–12. [Google Scholar] [CrossRef]
- Hu, M.Z.; Wang, A.R.; Zhao, Z.Y.; Chen, X.Y.; Li, Y.B.; Liu, B. Antidepressant-like effects of paeoniflorin on post-stroke depression in a rat model. Neurol. Res. 2019, 41, 446–455. [Google Scholar] [CrossRef]
- Du, Y.; Liang, H.; Zhang, L.; Fu, F. Administration of Huperzine A exerts antidepressant-like activity in a rat model of post-stroke depression. Pharmacol. Biochem. Behav. 2017, 158, 32–38. [Google Scholar] [CrossRef]
- Ji, S.; Kronenberg, G.; Balkaya, M.; Färber, K.; Gertz, K.; Kettenmann, H.; Endres, M. Acute neuroprotection by pioglitazone after mild brain ischemia without effect on long-term outcome. Exp. Neurol. 2009, 216, 321–328. [Google Scholar] [CrossRef]
- Feng, L.; Han, C.-X.; Cao, S.-Y.; Zhang, H.-M.; Wu, G.-Y. Deficits in motor and cognitive functions in an adult mouse model of hypoxia-ischemia induced stroke. Sci. Rep. 2020, 10, 20646. [Google Scholar] [CrossRef] [PubMed]
- Shi, X.; Bai, H.; Wang, J.; Wang, J.; Huang, L.; He, M.; Zheng, X.; Duan, Z.; Chen, D.; Zhang, J.; et al. Behavioral Assessment of Sensory, Motor, Emotion, and Cognition in Rodent Models of Intracerebral Hemorrhage. Front. Neurol. 2021, 12, 667511. [Google Scholar] [CrossRef] [PubMed]
- Metz, G.A.; Whishaw, I.Q. The ladder rung walking task: A scoring system and its practical application. J. Vis. Exp. 2009, 28, e1204. [Google Scholar] [CrossRef]
- Tamakoshi, K.; Ishida, A.; Takamatsu, Y.; Hamakawa, M.; Nakashima, H.; Shimada, H.; Ishida, K. Motor skills training promotes motor functional recovery and induces synaptogenesis in the motor cortex and striatum after intracerebral hemorrhage in rats. Behav. Brain Res. 2014, 260, 34–43. [Google Scholar] [CrossRef]
- Sun, J.; Wei, Z.Z.; Gu, X.; Zhang, J.Y.; Zhang, Y.; Li, J.; Wei, L. Intranasal delivery of hypoxia-preconditioned bone marrow-derived mesenchymal stem cells enhanced regenerative effects after intracerebral hemorrhagic stroke in mice. Exp. Neurol. 2015, 272, 78–87. [Google Scholar] [CrossRef]
- Beray-Berthat, V.; Delifer, C.; Besson, V.C.; Girgis, H.; Coqueran, B.; Plotkine, M.; Marchand-Leroux, C.; Margaill, I. Long-term histological and behavioural characterisation of a collagenase-induced model of intracerebral haemorrhage in rats. J. Neurosci. Methods 2010, 191, 180–190. [Google Scholar] [CrossRef] [PubMed]
- Schaar, K.L.; Brenneman, M.M.; Savitz, S.I. Functional assessments in the rodent stroke model. Exp. Transl. Stroke Med. 2010, 2, 13. [Google Scholar] [CrossRef]
- de Oliveira, J.L.; Ávila, M.; Martins, T.C.; Alvarez-Silva, M.; Winkelmann-Duarte, E.C.; Salgado, A.S.I.; Cidral-Filho, F.J.; Reed, W.R.; Martins, D.F. Medium- and long-term functional behavior evaluations in an experimental focal ischemic stroke mouse model. Cogn. Neurodyn 2020, 14, 473–481. [Google Scholar] [CrossRef]
- Zarruk, J.; Garcia-Yebenes, I.; Romera, V.G.; Ballesteros, I.; Moraga, A.; Cuartero, M.; Hurtado, O.; Sobrado, M.; Pradillo, J.; Fernandez-Lopez, D.; et al. Neurological tests for functional outcome assessment in rodent models of ischaemic stroke. Rev. Neurol. 2011, 53, 607–618. [Google Scholar] [PubMed]
- Hao, J.; Mdzinarishvili, A.; Abbruscato, T.J.; Klein, J.; Geldenhuys, W.J.; Van der Schyf, C.J.; Bickel, U. Neuroprotection in mice by NGP1-01 after transient focal brain ischemia. Brain Res. 2008, 1196, 113–120. [Google Scholar] [CrossRef]
- Narayan, S.K.; Grace Cherian, S.; Babu Phaniti, P.; Babu Chidambaram, S.; Rachel Vasanthi, A.H.; Arumugam, M. Preclinical animal studies in ischemic stroke: Challenges and some solutions. Anim. Model. Exp. Med. 2021, 4, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Allred, R.P.; Adkins, D.L.; Woodlee, M.T.; Husbands, L.C.; Maldonado, M.A.; Kane, J.R.; Schallert, T.; Jones, T.A. The vermicelli handling test: A simple quantitative measure of dexterous forepaw function in rats. J. Neurosci. Methods 2008, 170, 229–244. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.M.; Lima, F.O.; Barreira, J.; Appenzeller, S.; Fernandes, P.T. Is there a correlation between depressive symptoms and motor skills in post-stroke patients? Arq. Neuropsiquiatr. 2019, 77, 155–160. [Google Scholar] [CrossRef]
- Ritzel, R.M.; Lai, Y.J.; Crapser, J.D.; Patel, A.R.; Schrecengost, A.; Grenier, J.M.; Mancini, N.S.; Patrizz, A.; Jellison, E.R.; Morales-Scheihing, D.; et al. Aging alters the immunological response to ischemic stroke. Acta Neuropathol. 2018, 136, 89–110. [Google Scholar] [CrossRef]
- Gu, S.; He, Z.; Xu, Q.; Dong, J.; Xiao, T.; Liang, F.; Ma, X.; Wang, F.; Huang, J.H. The Relationship Between 5-Hydroxytryptamine and Its Metabolite Changes With Post-stroke Depression. Front. Psychiatry 2022, 13, 871754. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Ogden, R.T.; Huang, Y.Y.; Oquendo, M.A.; Mann, J.J.; Parsey, R.V. Higher in vivo serotonin-1a binding in posttraumatic stress disorder: A PET study with [11C]WAY-100635. Depress. Anxiety 2013, 30, 197–206. [Google Scholar] [CrossRef]
- Spasojevic, N.; Jovanovic, P.; Dronjak, S. Chronic fluoxetine treatment affects gene expression of catecholamine enzymes in the heart of depression model rats. Indian. J. Exp. Biol. 2012, 50, 771–775. [Google Scholar]
- Starr, L.R.; Hammen, C.; Brennan, P.A.; Najman, J.M. Serotonin transporter gene as a predictor of stress generation in depression. J. Abnorm. Psychol. 2012, 121, 810–818. [Google Scholar] [CrossRef]
- Kim, J.M.; Stewart, R.; Kim, S.W.; Shin, I.S.; Kim, J.T.; Park, M.S.; Park, S.W.; Kim, Y.H.; Cho, K.H.; Yoon, J.S. Associations of cytokine gene polymorphisms with post-stroke depression. World J. Biol. Psychiatry 2012, 13, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Ogłodek, E. Changes in the Serum Levels of Cytokines: IL-1β, IL-4, IL-8 and IL-10 in Depression with and without Posttraumatic Stress Disorder. Brain Sci. 2022, 12, 387. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Wang, R.; Liu, L.; Qiao, D.; Baldwin, D.S.; Hou, R. Effects of SSRIs on peripheral inflammatory markers in patients with major depressive disorder: A systematic review and meta-analysis. Brain Behav. Immun. 2019, 79, 24–38. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Zong, Y.; Ren, Z.; Hu, J.; Wu, X.; Xiao, H.; Qin, S.; Zhou, G.; Ma, Y.; Zhang, Y.; et al. Regulation of indoleamine 2, 3-dioxygenase in hippocampal microglia by NLRP3 inflammasome in lipopolysaccharide-induced depressive-like behaviors. Eur. J. Neurosci. 2020, 52, 4586–4601. [Google Scholar] [CrossRef]
- Holsboer, F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology 2000, 23, 477–501. [Google Scholar] [CrossRef]
- Pace, T.W.; Hu, F.; Miller, A.H. Activation of cAMP-protein kinase A abrogates STAT5-mediated inhibition of glucocorticoid receptor signaling by interferon-alpha. Brain Behav. Immun. 2011, 25, 1716–1724. [Google Scholar] [CrossRef]
- El Husseini, N.; Laskowitz, D.T. The role of neuroendocrine pathways in prognosis after stroke. Expert. Rev. Neurother. 2014, 14, 217–232. [Google Scholar] [CrossRef]
- Kim, J.M.; Stewart, R.; Kang, H.J.; Kim, S.Y.; Kim, S.W.; Shin, I.S.; Park, M.S.; Kim, H.R.; Shin, M.G.; Cho, K.H.; et al. A longitudinal study of BDNF promoter methylation and genotype with poststroke depression. J. Affect. Disord. 2013, 149, 93–99. [Google Scholar] [CrossRef]
- Zhang, Y.; Jiang, H.; Yue, Y.; Yin, Y.; Zhang, Y.; Liang, J.; Li, S.; Wang, J.; Lu, J.; Geng, D.; et al. The protein and mRNA expression levels of glial cell line-derived neurotrophic factor in post stroke depression and major depressive disorder. Sci. Rep. 2017, 7, 8674. [Google Scholar] [CrossRef]
- Kunze, A.; Zierath, D.; Drogomiretskiy, O.; Becker, K. Strain differences in fatigue and depression after experimental stroke. Transl. Stroke Res. 2014, 5, 604–611. [Google Scholar] [CrossRef]
- Lavu, V.K.; Mohamed, R.A.; Huang, R.; Potla, S.; Bhalla, S.; Al Qabandi, Y.; Nandula, S.A.; Boddepalli, C.S.; Gutlapalli, S.D.; Mohammed, L. Evaluation and Treatment of Depression in Stroke Patients: A Systematic Review. Cureus 2022, 14, e28137. [Google Scholar] [CrossRef]
- Starkstein, S.E.; Hayhow, B.D. Treatment of Post-Stroke Depression. Curr. Treat. Options Neurol. 2019, 21, 31. [Google Scholar] [CrossRef]
- Medeiros, G.C.; Roy, D.; Kontos, N.; Beach, S.R. Post-stroke depression: A 2020 updated review. Gen. Hosp. Psychiatry 2020, 66, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Zhang, W.; Zhang, Y.; Zhao, Y.; Zheng, C.; Tian, H.; Lei, J.; Liu, Y.; Zhao, R.; Tang, Q. Multimodal Magnetic Resonance Imaging and Therapeutic Intervention With Yi-nao-jie-yu Decoction in a Rat Model of Post-stroke Depression. Front. Psychiatry 2020, 11, 557423. [Google Scholar] [CrossRef]
- Chen, C.; Dong, Y.; Liu, F.; Gao, C.; Ji, C.; Dang, Y.; Ma, X.; Liu, Y. A Study of Antidepressant Effect and Mechanism on Intranasal Delivery of BDNF-HA2TAT/AAV to Rats with Post-Stroke Depression. Neuropsychiatr. Dis. Treat. 2020, 16, 637–649. [Google Scholar] [CrossRef]
- Ngwa, C.; Al Mamun, A.; Qi, S.; Sharmeen, R.; Xu, Y.; Liu, F. Regulation of microglial activation in stroke in aged mice: A translational study. Aging 2022, 14, 6047–6065. [Google Scholar] [CrossRef] [PubMed]
- Morioka, T.; Kalehua, A.N.; Streit, W.J. Characterization of microglial reaction after middle cerebral artery occlusion in rat brain. J. Comp. Neurol. 1993, 327, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Lambertsen, K.L.; Biber, K.; Finsen, B. Inflammatory cytokines in experimental and human stroke. J. Cereb. Blood Flow. Metab. 2012, 32, 1677–1698. [Google Scholar] [CrossRef]
- Kang, J.B.; Son, H.K.; Shah, M.A.; Koh, P.O. Retinoic acid attenuates ischemic injury-induced activation of glial cells and inflammatory factors in a rat stroke model. PLoS ONE 2024, 19, e0300072. [Google Scholar] [CrossRef] [PubMed]
- Cojocaru, A.; Burada, E.; Bălșeanu, A.T.; Deftu, A.F.; Cătălin, B.; Popa-Wagner, A.; Osiac, E. Roles of Microglial Ion Channel in Neurodegenerative Diseases. J. Clin. Med. 2021, 10, 1239. [Google Scholar] [CrossRef]
- Miao, Z.; Wang, Y.; Sun, Z. The Relationships Between Stress, Mental Disorders, and Epigenetic Regulation of BDNF. Int. J. Mol. Sci. 2020, 21, 1375. [Google Scholar] [CrossRef]
- Wu, X.; Gu, J.; Zou, Z.; Yu, M.; Zhang, C.; Xiao, Q.; Chen, X.; Li, C. Suppressive Effects of Isofraxidin on Depressive-like Behaviors Induced by Chronic Unpredictable Mild Stress in Mice. Brain Sci. 2022, 12, 1376. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Choi-Kwon, S. Poststroke depression and emotional incontinence: Correlation with lesion location. Neurology 2000, 54, 1805–1810. [Google Scholar] [CrossRef]
- Harciarek, M.; Mańkowska, A. Hemispheric stroke: Mood disorders. Handb. Clin. Neurol. 2021, 183, 155–167. [Google Scholar] [CrossRef]
- Carson, A.J.; MacHale, S.; Allen, K.; Lawrie, S.M.; Dennis, M.; House, A.; Sharpe, M. Depression after stroke and lesion location: A systematic review. Lancet 2000, 356, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Herrmann, N.; Black, S.E. The importance of lesion location in poststroke depression: A critical review. Can. J. Psychiatry 1998, 43, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Dockman, R.L.; Carpenter, J.M.; Diaz, A.N.; Benbow, R.A.; Filipov, N.M. Sex differences in behavior, response to LPS, and glucose homeostasis in middle-aged mice. Behav. Brain Res. 2022, 418, 113628. [Google Scholar] [CrossRef]
- Furman, O.; Tsoory, M.; Chen, A. Differential chronic social stress models in male and female mice. Eur. J. Neurosci. 2022, 55, 2777–2793. [Google Scholar] [CrossRef]
- Sohrabji, F.; Okoreeh, A.; Panta, A. Sex hormones and stroke: Beyond estrogens. Horm. Behav. 2019, 111, 87–95. [Google Scholar] [CrossRef]
- Jiang, H.; Xiao, L.; Jin, K.; Shao, B. Estrogen administration attenuates post-stroke depression by enhancing CREB/BDNF/TrkB signaling in the rat hippocampus. Exp. Ther. Med. 2021, 21, 433. [Google Scholar] [CrossRef]
- Zeng, P.Y.; Tsai, Y.H.; Lee, C.L.; Ma, Y.K.; Kuo, T.H. Minimal influence of estrous cycle on studies of female mouse behaviors. Front. Mol. Neurosci. 2023, 16, 1146109. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.-H.; Wu, K.-Y.; Su, N.C.; Edwards, A.; Huang, G.-J. The influence of sex difference on behavior and adult hippocampal neurogenesis in C57BL/6 mice. Sci. Rep. 2023, 13, 17297. [Google Scholar] [CrossRef] [PubMed]
- Tariq, M.B.; Lee, J.; McCullough, L.D. Sex differences in the inflammatory response to stroke. Semin. Immunopathol. 2023, 45, 295–313. [Google Scholar] [CrossRef] [PubMed]
| Stressors and Duration | Days of CUMS/Mice Housing | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gaignier F., 2018 [124] | Alterations of the light-dark cycle | Cage tilt 1 h, 2 h, 15 h | Food deprivation overnight 15 h | Illumination at night 15 h | Small cage 1 h, 2 h | Soiled cage overnight 15 h | Paired housing 2 h | 21 days Individually housing | |||||
| Zhang M., 2023 [125] | Exposure to a stroboscope 12 h | Cage tilt 12 h | Traffic noise (70–90 dB) 6 h | Food deprivation 12 h | Illumination at night 12 h | Food and water deprivation 24 h | Crowding: ten mice per cage 12 h | Water deprivation 12 h | Level shaking 15 min | 28 days Individually housing | |||
| Yan W., 2021 [126] | Ice water swimming 5 min | Cage tilt 5 min | Exposure to an empty bottle 1 h | Food deprivation 24 h | Illumination at night 12 h | Restraint stress 2 h | Soiled cage 24 h | Exposure to a foreign object 24 h | Water deprivation 24 h | 28 days Group housing | |||
| Wu J., 2021 [128] | Ice water swimming 5 min | Cage tilt 24 h | Foot electric shock twice | Food deprivation 24 h | Continuous illumination 24 h | Restraint stress 2 h | Wet bedding 24 h | Tail-clamp 90 s | Water deprivation 24 h | Cage shaking 15 min | 35 days Individually housing | ||
| Wang Y.I., 2021 [129] | Ice water swimming 5 min | Cage tilt 24 h | Food deprivation 24 h | Continuous illumination 24 h | Restraint stress 6 h | Wet bedding 24 h | Water deprivation 24 h | Cage shaking 30 min | 35 days Individually housing | ||||
| Wang G., 2019 [130] | Ice water swimming 5 min | Cage tilt 12 h | Plantar electrical stimulation 10 min | Food deprivation 12 h | Continuous illumination 36 h | White noise 12 h | Soiled cage 24 h | Tail nipping 2 min | Water deprivation 12 h | Exposure to a stroboscope 2 h | 35 days Group housing | ||
| Wen G., 2019 [131] | Exposure to a stroboscope overnight | Cage tilt 4 h | 120-dB noise overnight | Food deprivation 24 h | Alterations of the light-dark cycle | Restraint stress 4 h | Wet bedding 4 h | Water deprivation 24 h | 42 days Individually housing | ||||
| Li M., 2014 [132] | Alterations of the light-dark cycle | Cage tilt 12 h | Exposure to an empty bottle 10 min | Food deprivation 24 h | Overnight illumination | White noise 1 h | Overhang 10 min | Soiled cage 24 h | Exposure to a foreign object 12 h | Water deprivation 24 h | Tail pinch 1 min | Oscillation 5 min | 42 days Group housing |
| Xie M., 2022 [133] | No bedding 24 h | Cage tilt 24 h | Food deprivation 24 h | Overnight illumination (twice per week) | Restraint stress 6 h | Wet bedding 24 h | Tail pinching 5 min | Water deprivation 24 h | Cage shaking 15 min | 49 days Individually housing | |||
| Wassouf Z., 2019 [134] | Switched day/night-cycle 48 h | Cage tilt 2 h | Food deprivation 16 h | Illumination at night 12 h | Restraint stress 1 h | Rat confrontation 30 min | Water deprivation 16 h | 56 days Individually housing | |||||
| Wang Y., 2021 [135] | 4 °C exposure 1 h | Cage tilt 12 h | Food deprivation 23 h | Day/night inversion | Restraint stress 1 h | Damp bedding 24 h | Water deprivation 23 h | Cage shaking 30 min | 56 days Group housing | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mușat, M.I.; Cătălin, B.; Hadjiargyrou, M.; Popa-Wagner, A.; Greșiță, A. Advancing Post-Stroke Depression Research: Insights from Murine Models and Behavioral Analyses. Life 2024, 14, 1110. https://doi.org/10.3390/life14091110
Mușat MI, Cătălin B, Hadjiargyrou M, Popa-Wagner A, Greșiță A. Advancing Post-Stroke Depression Research: Insights from Murine Models and Behavioral Analyses. Life. 2024; 14(9):1110. https://doi.org/10.3390/life14091110
Chicago/Turabian StyleMușat, Mădălina Iuliana, Bogdan Cătălin, Michael Hadjiargyrou, Aurel Popa-Wagner, and Andrei Greșiță. 2024. "Advancing Post-Stroke Depression Research: Insights from Murine Models and Behavioral Analyses" Life 14, no. 9: 1110. https://doi.org/10.3390/life14091110
APA StyleMușat, M. I., Cătălin, B., Hadjiargyrou, M., Popa-Wagner, A., & Greșiță, A. (2024). Advancing Post-Stroke Depression Research: Insights from Murine Models and Behavioral Analyses. Life, 14(9), 1110. https://doi.org/10.3390/life14091110









