Abstract
Chronic kidney disease (CKD) involves inflammation, oxidative stress, and fibrosis, leading to renal dysfunction. Dapagliflozin, an SGLT2 inhibitor, shows renoprotective effects beyond glucose control, but its precise molecular mechanisms remain unclear. This study utilizes network pharmacology and molecular docking to elucidate its multi-target effects in CKD. Dapagliflozin’s SMILES structure was analyzed for ADMET properties. Potential targets were identified via SwissTargetPrediction, GeneCards, and SEA, and common CKD-related targets were determined. A protein–protein interaction (PPI) network was constructed, and key pathways were identified using GO and KEGG enrichment analyses. Molecular docking was conducted to validate dapagliflozin’s binding affinities with hub proteins. A total of 208 common targets were identified, including EGFR, GSK3β, and IL-6. GO and KEGG analyses highlighted key pathways, such as PI3K-Akt, MAPK, and AGE-RAGE, involved in inflammation, oxidative stress, and metabolic regulation. Molecular docking confirmed strong binding affinities with EGFR (−8.42 kcal/mol), GSK3β (−7.70 kcal/mol), and IL-6 (−6.83 kcal/mol). Dapagliflozin exhibits multi-target therapeutic potential in CKD by modulating inflammation, oxidative stress, and metabolic pathways. This integrative approach enhances the understanding of its mechanisms, supporting future experimental validation and clinical application in CKD management.
1. Introduction
Chronic kidney disease (CKD) is a significant global health issue that affects millions of individuals and imposes substantial economic and social costs [1]. With a prevalence of approximately 9.5% across 162 countries, CKD strains healthcare systems and contributes to elevated morbidity, mortality, and diminished quality of life [2]. The pathophysiology of CKD is multifaceted, involving mechanisms such as glomerular hypertension, tubulointerstitial fibrosis, and inflammation [3,4]. These processes cumulatively lead to a progressive decline in renal function and eventual end-stage renal disease (ESRD), necessitating interventions such as dialysis or transplantation [5]. Inflammation plays a particularly critical role in CKD progression, marked by elevated levels of pro-inflammatory cytokines, such as interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) [6,7]. Additionally, oxidative stress and mitochondrial dysfunction exacerbate renal damage, highlighting the importance of addressing these mechanisms in therapeutic development [8,9].
Dapagliflozin, an SGLT2 inhibitor, has shown promise as a therapeutic agent for CKD [10]. By inhibiting glucose reabsorption in the proximal tubules, dapagliflozin induces glucosuria, reducing blood glucose levels [11]. Beyond its glucose-lowering effects, dapagliflozin demonstrates renoprotective mechanisms, such as reducing intraglomerular pressure, lowering albuminuria, and attenuating tubulointerstitial fibrosis [12,13]. Preclinical studies in animal models have supported its ability to reduce markers of renal injury and improve renal outcomes [14,15]. Clinical trials have further established its efficacy in reducing ESRD progression and cardiovascular events in CKD patients, regardless of diabetes status [16,17]. However, the molecular mechanisms underlying these effects remain partially understood and warrant further investigation.
Network pharmacology, a systems biology approach, provides a powerful framework for elucidating the complex interactions between drugs, targets, and disease pathways. By integrating data from multiple databases and computational tools, this approach enables the identification of potential molecular targets and pathways involved in drug action [18]. This approach enables a comprehensive analysis of the interactions between drugs, targets, and disease pathways, offering insights into potential therapeutic mechanisms and novel targets. The application of network pharmacology to dapagliflozin provides an opportunity to uncover its multi-target effects and explore its broader therapeutic potential in CKD.
This study aims to utilize network pharmacology and molecular docking to investigate the mechanisms of dapagliflozin in CKD. By integrating data from diverse databases, we systematically identify and analyze the common molecular targets of dapagliflozin and CKD, construct protein–protein interaction (PPI) networks, and perform gene ontology (GO) and KEGG pathway enrichment analyses. Additionally, molecular docking simulations are conducted to validate the binding interactions of dapagliflozin with key hub proteins. These comprehensive analyses aim to provide novel insights into dapagliflozin’s therapeutic mechanisms, laying the groundwork for future experimental and clinical validation.
2. Materials and Methods
2.1. Drug Activity Evaluation of Dapagliflozin
The drug activity of dapagliflozin was evaluated using in silico ADMET (Absorption, Distribution, Metabolism, Excretion, and Toxicity) analysis and drug-likeness prediction through the SwissADME (http://www.swissadme.ch/ accessed on 2 November 2024) and pkCSM platforms (https://biosig.lab.uq.edu.au/pkcsm/ accessed on 2 November 2024). Dapagliflozin’s adherence to Lipinski’s rule of five was assessed to evaluate its potential as an orally bioavailable drug. The analyses included physicochemical property evaluation, lipophilicity and solubility prediction, pharmacokinetic profiling, and toxicity assessment, which were generated using both SwissADME and pkCSM [19].
2.2. Screening the Targets of Dapagliflozin and Chronic Kidney Disease
The potential targets of dapagliflozin were gathered from the SwissTargetPrediction (http://www.swisstargetprediction.ch/ accessed on 4 November 2024), Super-PRED (https://prediction.charite.de/subpages/target_prediction.php/ accessed on 4 November 2024), and similarity ensemble approach or SEA (https://sea.bkslab.org/ accessed on 4 November 2024) [20]. The names of target proteins were translated into gene names in the UniProt (http://www.uniprot.org/ accessed on 5 November 2024) database [21]. The CKD-related genes were derived from the GeneCards (https://www.GeneCards.org/ accessed on 7 November 2024) databases by searching the keywords of chronic kidney disease [22].
2.3. Construction of Drug-Target Network
The common targets of dapagliflozin and CKD were determined using a Venn diagram (https://bioinfogp.cnb.csic.es/tools/venny/index.html accessed on 10 November 2024) [23]. Intersecting genes were the potential targets of dapagliflozin, and they overlapped with CKD.
2.4. Construction of Protein-Protein Interaction (PPI) Network
Intersecting genes from a Venn diagram were uploaded to the STRING database (https://string-db.org/ accessed on 12 November 2024), and Homo sapiens was chosen for species [24]. The result from the STRING database was downloaded and imported to Cytoscape 3.8.0 software (https://cytoscape.org/ accessed on 13 November 2024) [25]. Then the protein interaction information was obtained, a network analysis of the PPI network was performed, and the top 10 targets of the degree centrality (DC) values were screened.
2.5. Gene Functions and Pathway Enrichment Analysis with Potential Targets
Gene ontology (GO) enrichment analysis and the Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses were carried out using ShinyGO 0.80 (http://bioinformatics.sdstate.edu/go/ accessed on 15 November 2024) [26]. The GO enrichment and KEGG pathway analyses were screened for p < 0.05. The top 20 results from the GO enrichment and KEGG pathway analyses were presented. The GO enrichment analysis mainly shows three aspects of biology, such as biological process, molecular component, and cellular component. It is widely used for gene function classification and target function distribution prediction.
2.6. Protein and Compound Preparation
To enhance our understanding of the relationship, modes of interaction, and mechanisms of action between the candidate proteins (or hub targets) and dapagliflozin, we employed a computational technique known as molecular docking. This simulation methodology enables the prediction of the affinity and orientation of a compound within a protein’s structure, thereby providing insights into potential binding modes. To initiate this process, we obtained the 3D structures of the pivotal proteins from the Protein Data Bank (PDB) and performed essential cleaning procedures to eliminate water molecules or other small molecules that might interfere with the docking process [27]. This preparatory phase was conducted using BIOVIA Discovery Studio software (Version 2021 Client). The 3D protein structures of the top 10 target proteins, including GAPDH (PDB 6M61), IL-6 (PDB 1ALU), SRC (PDB 1Y57), EGFR (PDB 1M17), HSP90AA1 (PDB 4AWQ), NFKB (PDB 3GUT), CASP3 (PDB 3KJF), HSP90AB1 (PDB 5UCJ), MAPK3 (PDB 4QTB), and GSK3β (PDB 6TCU), were downloaded from the RCSB Protein Data Bank (https://www.rcsb.org/ accessed on 20 November 2024) in PDB format [28]. Details of the proteins were collected from the PDB database (Table 1). The Protein Data Bank (PDB) is a global repository of 3D structural data for major proteins. The co-crystallized ligand and water molecules were removed from the protein structures. Polar hydrogens, charges, solvation parameters, and fragmental volumes were assigned to the protein using the Kollman united atom force field via AutoDock Tools (ADT) (Version 1.1.2) [29]. The cleaned protein structures were then saved in the PDBQT file format.

Table 1.
Details of the protein targets in the PDB database and the grid docking parameters in molecular docking.
The three-dimensional (3D) structure of dapagliflozin (CID 9887712) was retrieved from the PubChem database (http://pubchem.ncbi.nlm.nih.gov/ accessed on 25 November 2024) and prepared for docking. Known tyrosinase inhibitors or positive controls were also retrieved from co-crystallized protein structures. This preparation involved structural optimization, the addition of missing hydrogen atoms, and charge correction. The ligand was further optimized and converted to a PDB file using UCSF Chimera software (version 1.17.1) [30]. Energy minimization using conjugate and steepest descent methods, along with the addition of charges for correcting ionization, was employed to prepare the ligands. Missing hydrogen atoms and polar hydrogens were added to all ligands at a pH of 7.4. Bond orders, angles, and topology were assigned to optimize the structure. AutoDock Tools (ADT) automatically assigned Gasteiger charges and default atomic parameters. Finally, the optimized structures were saved in PDBQT file format using ADT.
2.7. Molecular Docking Simulation
Molecular docking was performed using AutoDock version 4.2. The Lamarckian genetic algorithm method was employed for the molecular docking experiment, and it was conducted with AutoDock4 software. During the procedure, the protein structure was treated as a rigid molecule, while the ligand was considered flexible. Default parameter values in AutoDockTools (ADT) were used for all other settings. For conformational sampling, fifty genetic algorithm (GA) runs were executed with a population size of 200. A docking box was constructed to completely encompass the binding site of the receptor protein. The parameters of the docking box were recorded (Table 1). Molecular docking was carried out using AutoDockTools 1.5.7, where the binding energy magnitude was used to assess the likelihood of binding between the receptor and the ligand. The optimal pose was determined as the conformation with the lowest binding energy (kcal/mol). The interactions of natural ligands or drugs were compared to the best-docked pose of dapagliflozin. Binding energy data from the molecular docking process were gathered using AutoDockTools 1.5.7. Finally, potential protein–ligand interactions and binding modes were analyzed and visualized using the BIOVIA Discovery Studio Visualizer software (Accelrys, San Diego, CA, USA) [19].
3. Results
3.1. Drug Activity of Dapagliflozin
The drug activity of dapagliflozin was evaluated using ADMET analysis and drug-likeness prediction through SwissADME and pkCSM platforms. As shown in Table S1, the analysis revealed key physicochemical properties, pharmacokinetics, and toxicity profiles. The molecular weight (MW) of dapagliflozin is 408.87 g/mol, with a formula of C21H25ClO6. It exhibits six hydrogen bond acceptors, four hydrogen bond donors, and a topological polar surface area (TPSA) of 99.38 Å2. Its predicted lipophilicity (LogP) values from different models (iLOGP, XLOGP3, WLOGP, Silicos-IT Log P) range from 1.07 to 3.17, with a consensus LogP of 2.18, indicating moderate lipophilicity. Dapagliflozin is classified as soluble based on ESOL predictions and moderately soluble by aliphatic and silicos-IT classifications.
In terms of pharmacokinetics, dapagliflozin shows high gastrointestinal (GI) absorption but does not cross the blood–brain barrier (BBB). It is a substrate for P-glycoprotein but not for CYP2D6 or CYP3A4 enzymes. It inhibits CYP2D6 but does not inhibit other key cytochrome P450 enzymes (CYP1A2, CYP2C19, CYP2C9, or CYP3A4). The predicted skin permeability (log Kp) is −7.13 cm/s, and the total clearance is 0.194 log mL/min/kg.
From a toxicity perspective, dapagliflozin demonstrates no AMES toxicity, hepatotoxicity, or skin sensitization. It is not a substrate or inhibitor of hERG channels, indicating low cardiac risk. Predicted oral rat acute toxicity (LD50) is 2.475 mol/kg, and chronic toxicity (LOAEL) is 3.63 log mg/kg/day. It also shows moderate environmental toxicity with a Tetrahymena pyriformis toxicity (log µg/L) of 0.289 and minnow toxicity (log mM) of 1.079.
Dapagliflozin adheres to Lipinski’s rule of five with zero violations, suggesting good oral bioavailability (bioavailability score of 0.55). No alerts for pan-assay interference compounds alerts (PAINS), Brenk, or lead-likeness were identified. The synthetic accessibility score is 4.52, indicating a moderately complex synthesis. These results highlight dapagliflozin’s favorable drug-likeness profile and suitability for oral administration, with minimal toxicity risks.
3.2. Targets of Dapagliflozin and Chronic Kidney Disease
The screening process identified a total of 231 potential targets for dapagliflozin through the SwissTargetPrediction, Super-PRED, and Similarity Ensemble Approach (SEA) platforms. These targets were converted into gene names using the UniProt database for standardization. Concurrently, 16,154 chronic kidney disease (CKD)-related genes were extracted from the GeneCards database using the keyword “chronic kidney disease”.
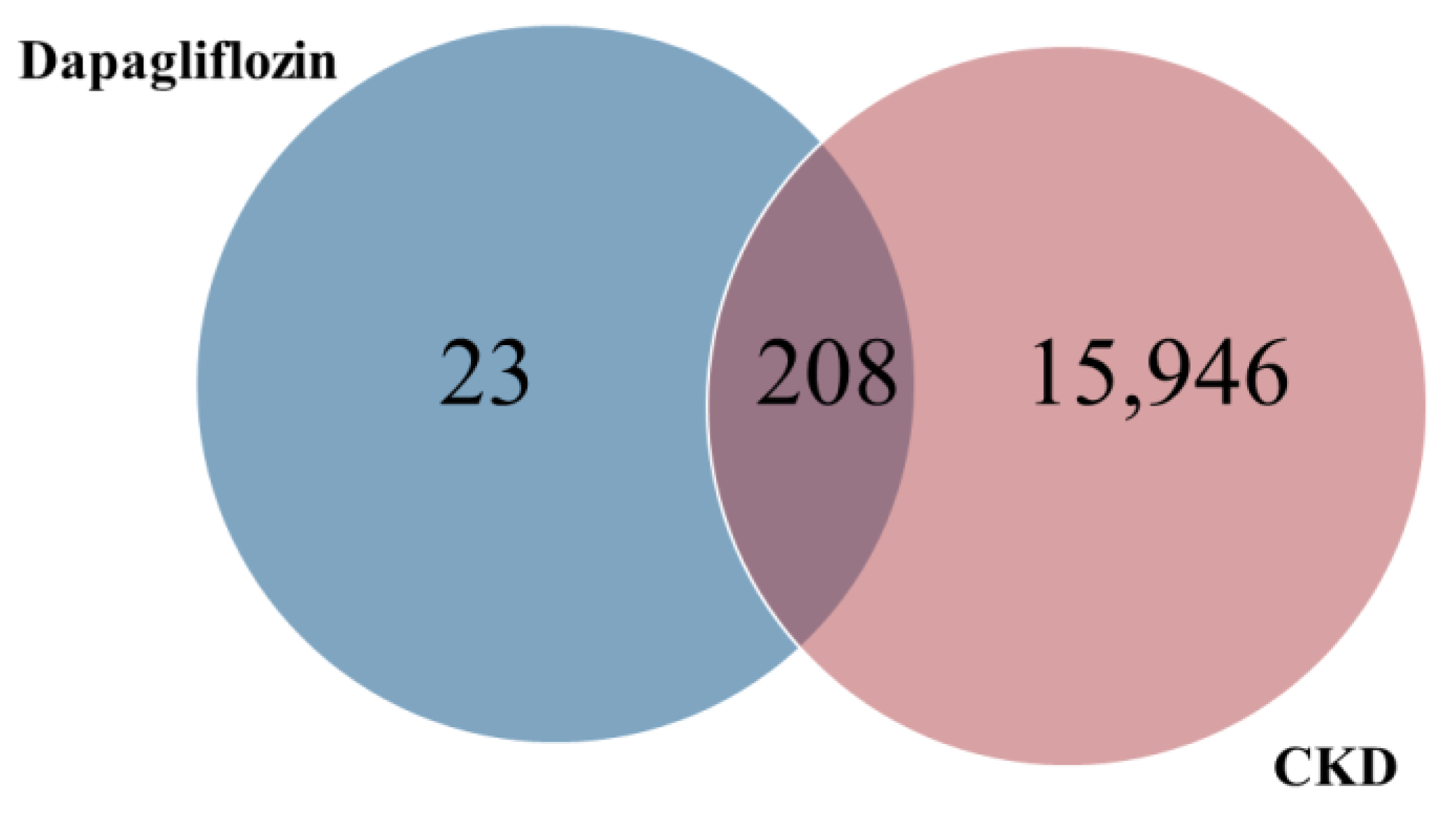
3.3. Prediction of Common Targets Between Dapagliflozin and Chronic Kidney Disease
The common targets of dapagliflozin and CKD were identified using a Venn diagram analysis. Out of the 231 potential targets of dapagliflozin and 16,154 CKD-related genes, a total of 208 overlapping targets were identified, as shown in Figure 1 and Table 2. These overlapping genes represent the potential targets through which dapagliflozin may exert therapeutic effects on CKD. This result highlights a significant overlap and provides a foundation for further investigation into the molecular mechanisms underlying the drug’s action in CKD.
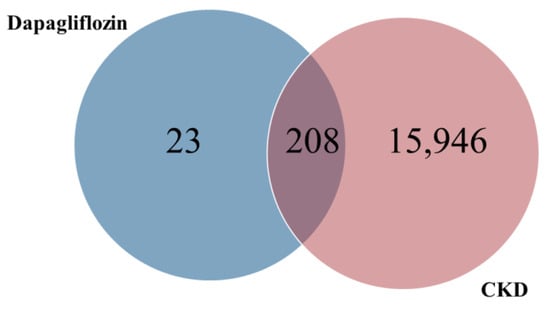
Figure 1.
Overlapping targets of dapagliflozin and chronic kidney disease.

Table 2.
The 208 overlapping targets of dapagliflozin and CKD.
3.4. Construction of PPI Networks
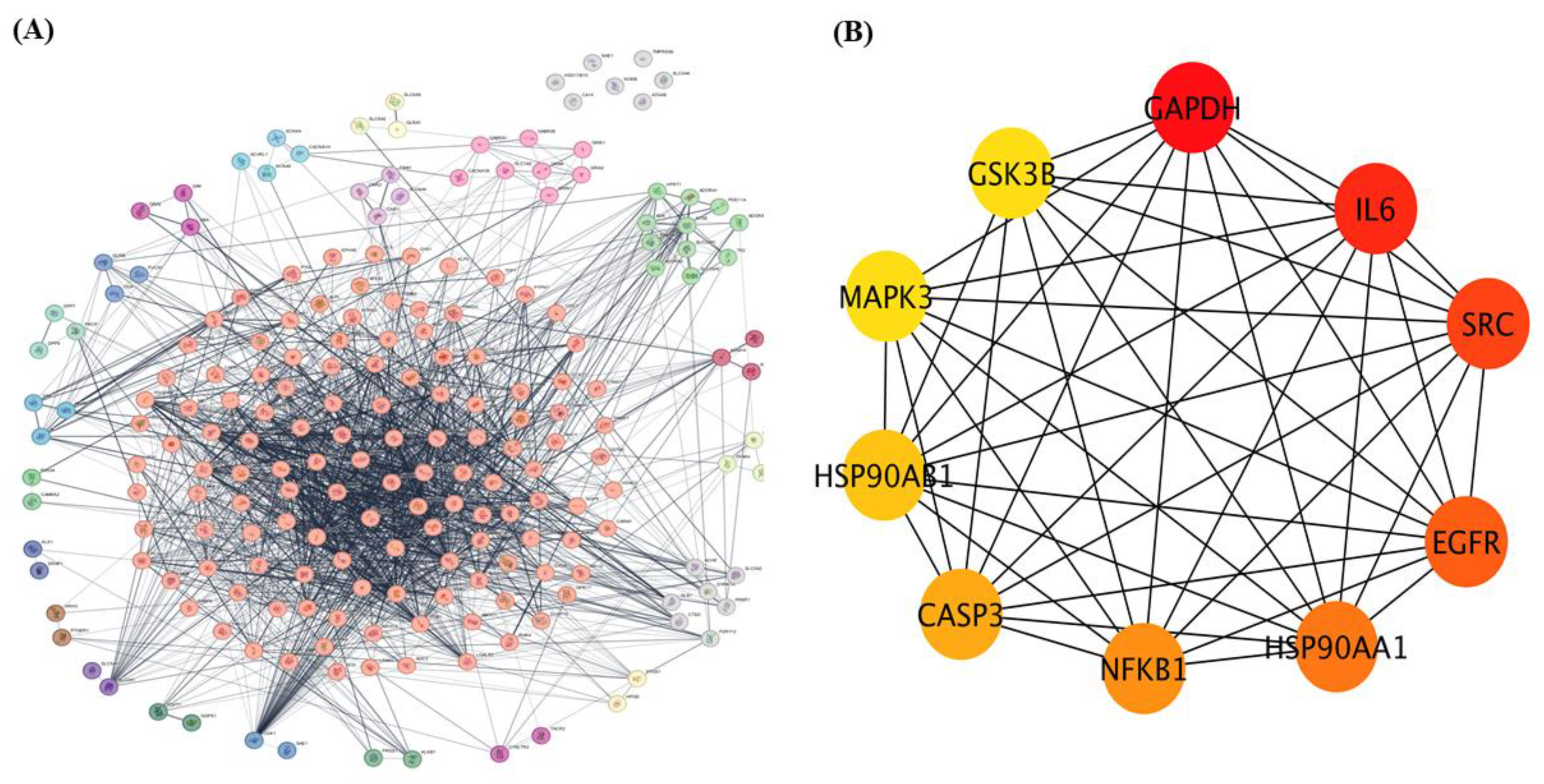
The 208 overlapping genes identified as common targets of dapagliflozin and CKD were uploaded to the STRING database to construct a protein–protein interaction (PPI) network, with Homo sapiens selected as the species, as shown in Figure 2A. The interaction data were exported and imported into Cytoscape 3.10.3 for network visualization and analysis.
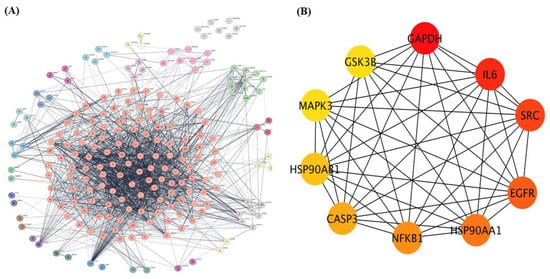
Figure 2.
The protein–protein interaction (PPI) network of overlapping targets of dapagliflozin and chronic kidney disease. (A) protein-protein interaction (PPI) network of 208 overlapping genes identified as common targets of dapagliflozin and chronic kidney disease (CKD). The network was constructed using the STRING database with Homo sapiens as the selected species and visualized in Cytoscape 3.10.3. The complex network displays interactions among these genes, with edges representing experimentally and computationally determined connections. This method organizes key proteins into clusters based on the MCL cluster network in Cytoscape. (B) The top 10 hub genes from the PPI network, identified using the cytoHubba plugin in Cytoscape based on degree centrality (DC) values. The hub genes include GAPDH, IL-6, SRC, EGFR, HSP90AA1, NFKB1, CASP3, HSP90AB1, MAPK3, and GSK3B. Node coloration, ranging from yellow to dark red, indicates DC scores, with darker red nodes representing higher centrality and greater importance within the network. These hub genes are potential key players in the mechanism of action of dapagliflozin in CKD.
Using the Cytoscape plugin cytoHubba, a network analysis was performed to identify the top 10 hub genes based on degree centrality (DC) values as shown in Figure 2B. These hub targets, which represent the most interconnected and potentially critical nodes in the PPI network, are glyceraldehyde-3-phosphate dehydrogenase (GAPDH), interleukin-6 (IL-6), proto-oncogene tyrosine-protein kinase Src (SRC), epidermal growth factor receptor (EGFR), heat shock protein HSP 90-alpha (HSP90AA1), nuclear factor NF-kappa-B p105 subunit (NFKB1), caspase-3 (CASP3), heat shock protein HSP 90-beta (HSP90AB1), mitogen-activated protein kinase 3 (MAPK3), and glycogen synthase kinase-3 beta (GSK3β). Their significance within the network is highlighted by node coloration, where darker and redder hues correspond to higher scores, indicating greater importance in the network. These hub targets may play pivotal roles in the mechanism of action of dapagliflozin in CKD.
3.5. KEGG Pathway Enrichment Analysis and GO Enrichment Analysis
GO Enrichment analysis and KEGG pathway enrichment analysis were conducted to explore the biological roles of the intersecting genes identified as targets of dapagliflozin in chronic kidney disease (CKD).
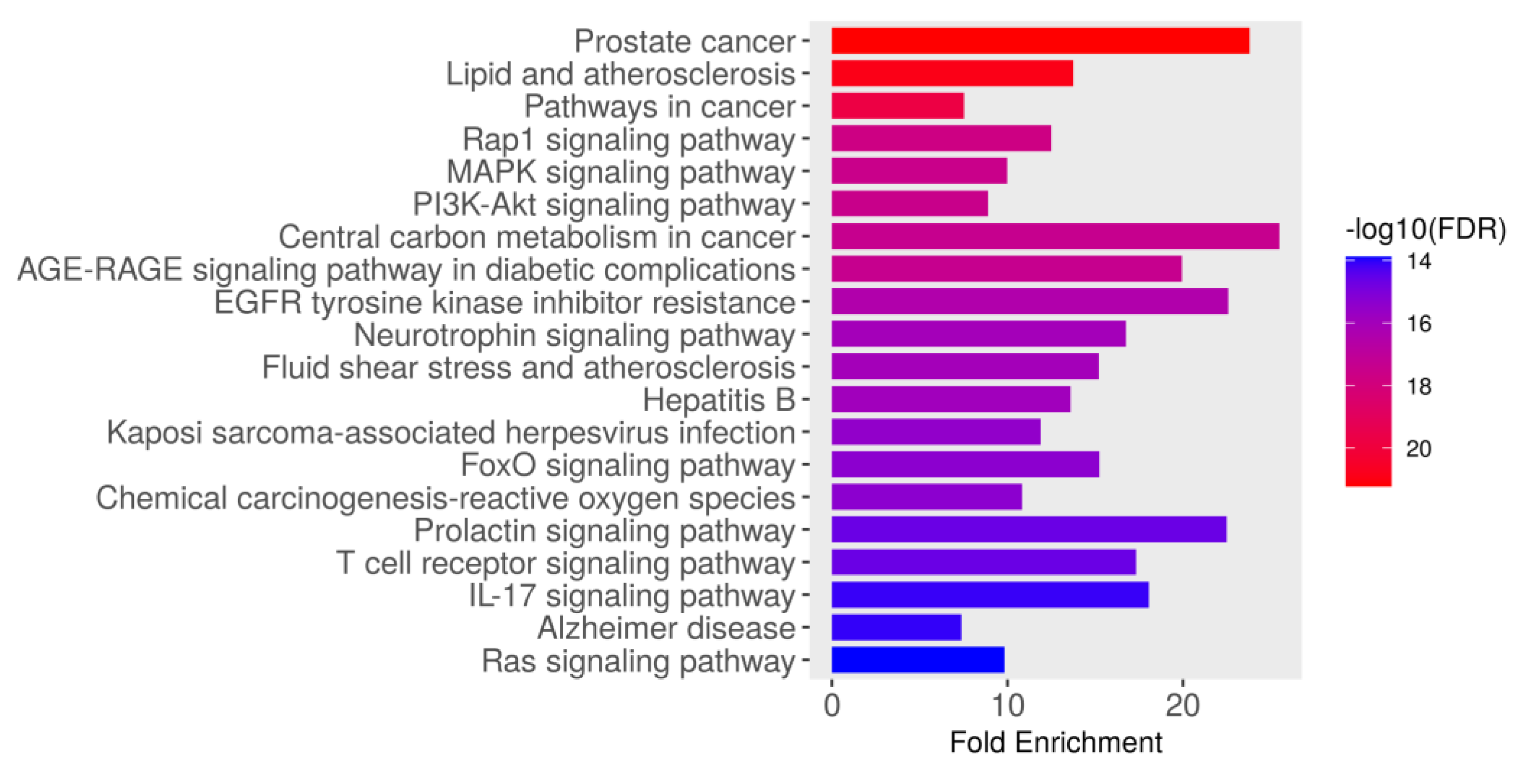
3.5.1. KEGG Pathway Enrichment Analysis
The KEGG pathway enrichment analysis identified the top 20 significantly enriched pathways associated with the intersecting targets of dapagliflozin and CKD based on their fold enrichment and −log10(FDR) values, as shown in Figure 3 and Table 3. The −log10(FDR) scores indicate the statistical significance of each pathway, with higher values reflecting greater significance. Among these, the most enriched pathway was prostate cancer (hsa05215), followed by lipid and atherosclerosis (hsa05417), pathways in cancer (hsa05200), Rap1 signaling pathway (hsa04015), MAPK signaling pathway (hsa04010), PI3K-Akt signaling pathway (hsa04151), AGE-RAGE signaling pathway in diabetic complications (hsa04933), central carbon metabolism in cancer (hsa05230), EGFR tyrosine kinase inhibitor resistance (hsa01521), neurotrophin signaling pathway (hsa04722), fluid shear stress and atherosclerosis (hsa05418), hepatitis B (hsa05161), Kaposi sarcoma-associated herpesvirus infection (hsa05167), FoxO signaling pathway (hsa04068), chemical carcinogenesis-reactive oxygen species (hsa05208), T cell receptor signaling pathway (hsa04660), prolactin signaling pathway (hsa04917), IL-17 signaling pathway (hsa04657), Alzheimer disease (hsa05010), and Ras signaling pathway (hsa04014). These findings highlight the importance of the pathways involved in biological processes, including cancer-related pathways, cardiovascular and metabolic pathways, cellular signaling pathways, infection-related pathways, and neurological pathways. These pathways may play a crucial role in the therapeutic mechanisms of dapagliflozin in the context of CKD.
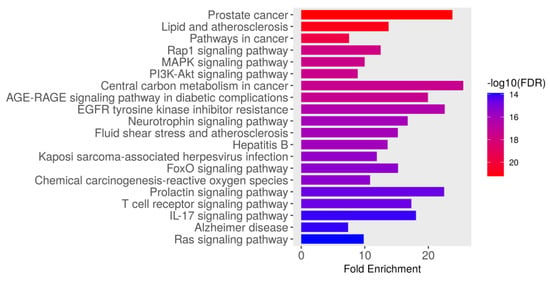
Figure 3.
The Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis of genes associated with dapagliflozin and chronic kidney disease (CKD). The bar plot illustrates the top enriched pathways based on fold enrichment, ranked from most to least enriched. The color gradient represents the −log10(FDR) values, with red indicating the highest statistical significance and blue indicating lower significance.

Table 3.
The Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis of 208 overlapping targets between dapagliflozin and chronic kidney disease.
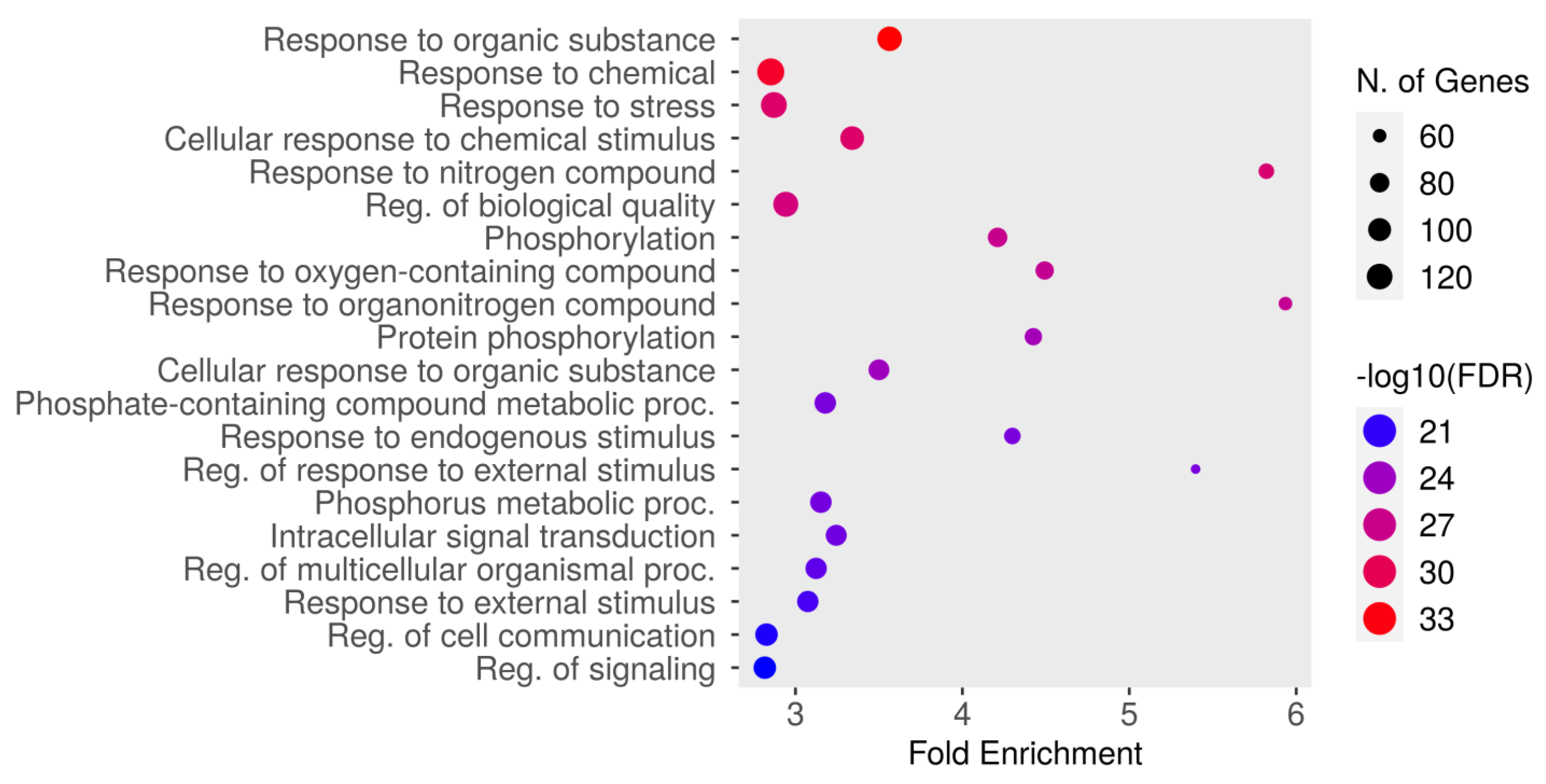
3.5.2. GO Biological Process Enrichment Analysis
The top 20 results from the biological process enrichment analysis in the GO enrichment analysis are presented in Figure 4 and Table 4, associated with the analyzed gene set. The GO enrichment analysis, a powerful tool used for gene function classification and functional distribution prediction, revealed key pathways and processes relevant to the gene set under study. The most enriched pathway was “response to organic substance” (GO:0010033) with an FDR of 4.6987 × 10−34 and a fold enrichment of 3.56, followed by “response to chemical” (GO:0042221; FDR = 9.3426 × 10−33, fold enrichment = 2.85), and “response to stress” (GO:0006950; FDR = 1.6161Í10-29, fold enrichment = 2.87). Other significantly enriched pathways included cellular response to chemical stimulus (GO:0070887), response to nitrogen compound (GO:1901698), and regulation of biological quality (GO:0065008). Additional notable pathways included phosphorylation (GO:0016310), response to oxygen-containing compound (GO:1901700), and response to organonitrogen compound (GO:0010243). Metabolic and signaling processes, such as protein phosphorylation (GO:0006468), cellular response to organic substance (GO:0071310), and phosphate-containing compound metabolic process (GO:0006796), were also enriched. Furthermore, pathways like response to endogenous stimulus (GO:0009719), regulation of response to external stimulus (GO:0032101), and phosphorus metabolic process (GO:0006793) demonstrated significant enrichment. Other important pathways included intracellular signal transduction (GO:0035556), regulation of multicellular organismal process (GO:0051239), and response to external stimulus (GO:0009605). The pathways “regulation of cell communication” (GO:0010646) and “regulation of signaling” (GO:0023051) were also enriched. These findings highlight the diverse biological processes potentially involved in the therapeutic mechanisms of dapagliflozin, including responses to chemical and environmental stimuli, metabolic regulation, and intracellular signaling.
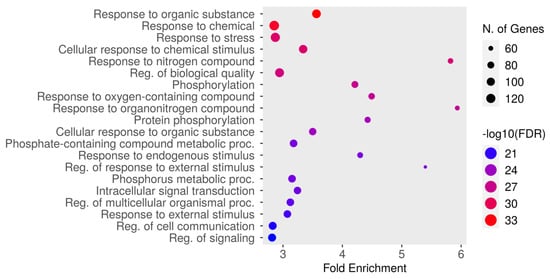
Figure 4.
The Gene Ontology (GO) enrichment analysis of biological processes associated with dapagliflozin and chronic kidney disease (CKD). The dot plot displays the top enriched biological processes, ranked by fold enrichment, with the size of each dot representing the number of genes associated with each process. The color gradient indicates the statistical significance (−log10(FDR)), with red representing the highest significance.

Table 4.
The GO biological process enrichment analysis of targets shared by dapagliflozin and chronic kidney disease.
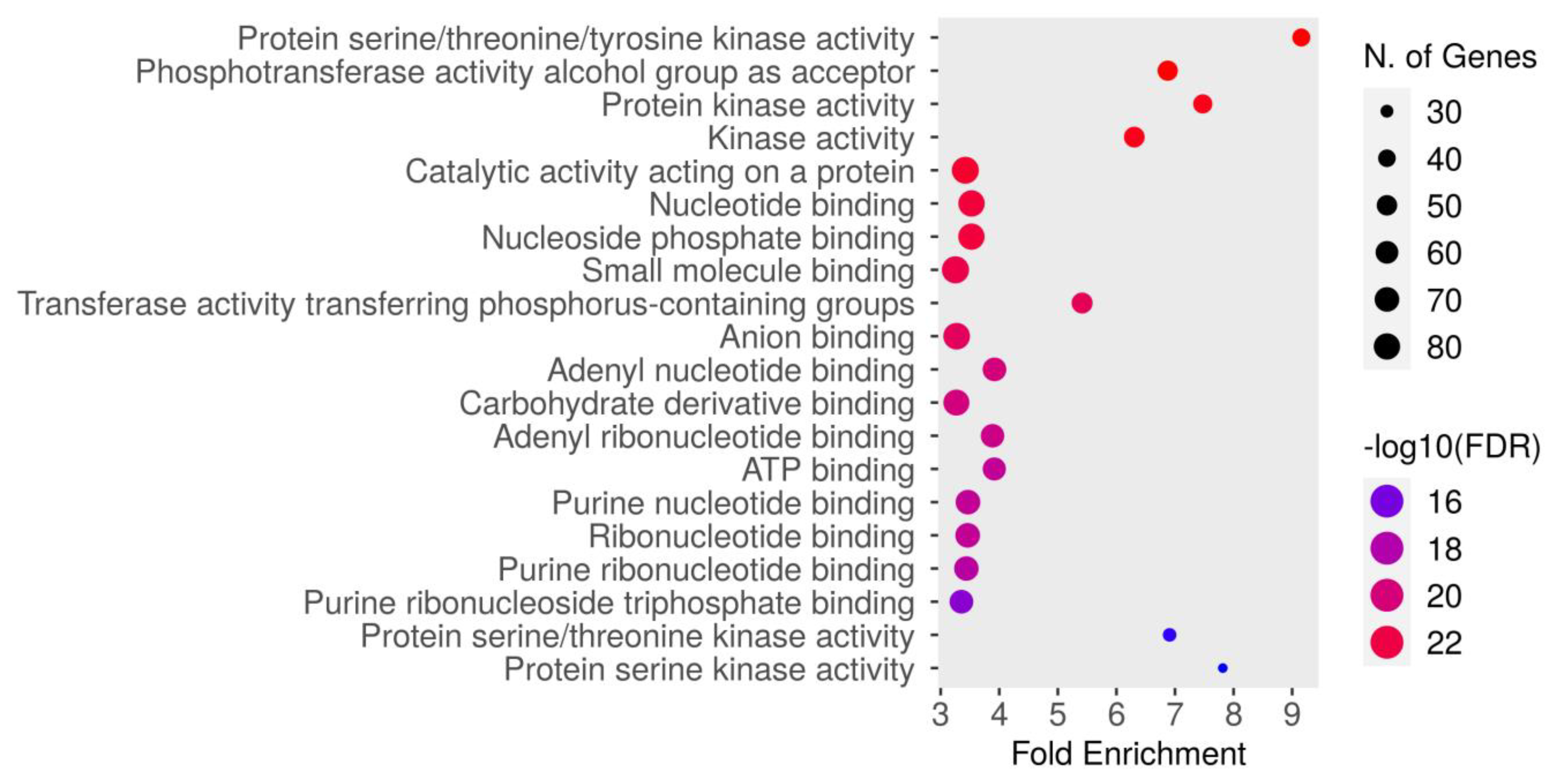
3.5.3. GO Molecular Function Enrichment Analysis
The molecular function enrichment analysis of dapagliflozin revealed significant enrichment of several key activities. As shown in Figure 5 and Table 5, the most enriched function was protein serine/threonine/tyrosine kinase activity (GO:0004712) with an FDR of 1.5084 × 10−24. This was followed by the phosphotransferase activity alcohol group as acceptor (GO:0016773), protein kinase activity (GO:0004672), kinase activity (GO:0016301), catalytic activity acting on a protein (GO:0140096), nucleotide binding (GO:0000166), nucleoside phosphate binding (GO:1901265), small molecule binding (GO:0036094), transferase activity transferring phosphorus-containing groups (GO:0016772), anion binding (GO:0043168), adenyl nucleotide binding (GO:0030554), carbohydrate derivative binding (GO:0097367), adenyl ribonucleotide binding (GO:0032559), ATP binding (GO:0005524), purine nucleotide binding (GO:0017076), ribonucleotide binding (GO:0032553), purine ribonucleotide binding (GO:0032555), purine ribonucleoside triphosphate binding (GO:0035639), protein serine/threonine kinase activity (GO:0004674), and protein serine kinase activity (GO:0106310). These findings emphasize the critical molecular functions, particularly kinase activity and nucleotide binding, which may contribute to the therapeutic mechanisms of dapagliflozin in CKD.
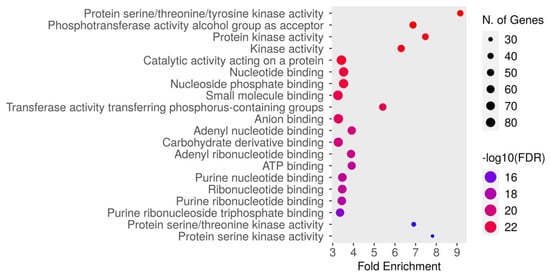
Figure 5.
The Gene Ontology (GO) molecular function enrichment analysis of intersecting targets of dapagliflozin and chronic kidney disease (CKD). The top enriched molecular functions are depicted, ranked by fold enrichment and statistical significance (−log10[FDR]). The size of the dots corresponds to the number of genes associated with each pathway, while the color represents the statistical significance, with red indicating higher −log10(FDR) values.

Table 5.
The GO molecular function enrichment analysis of intersecting targets shared by dapagliflozin and chronic kidney disease.
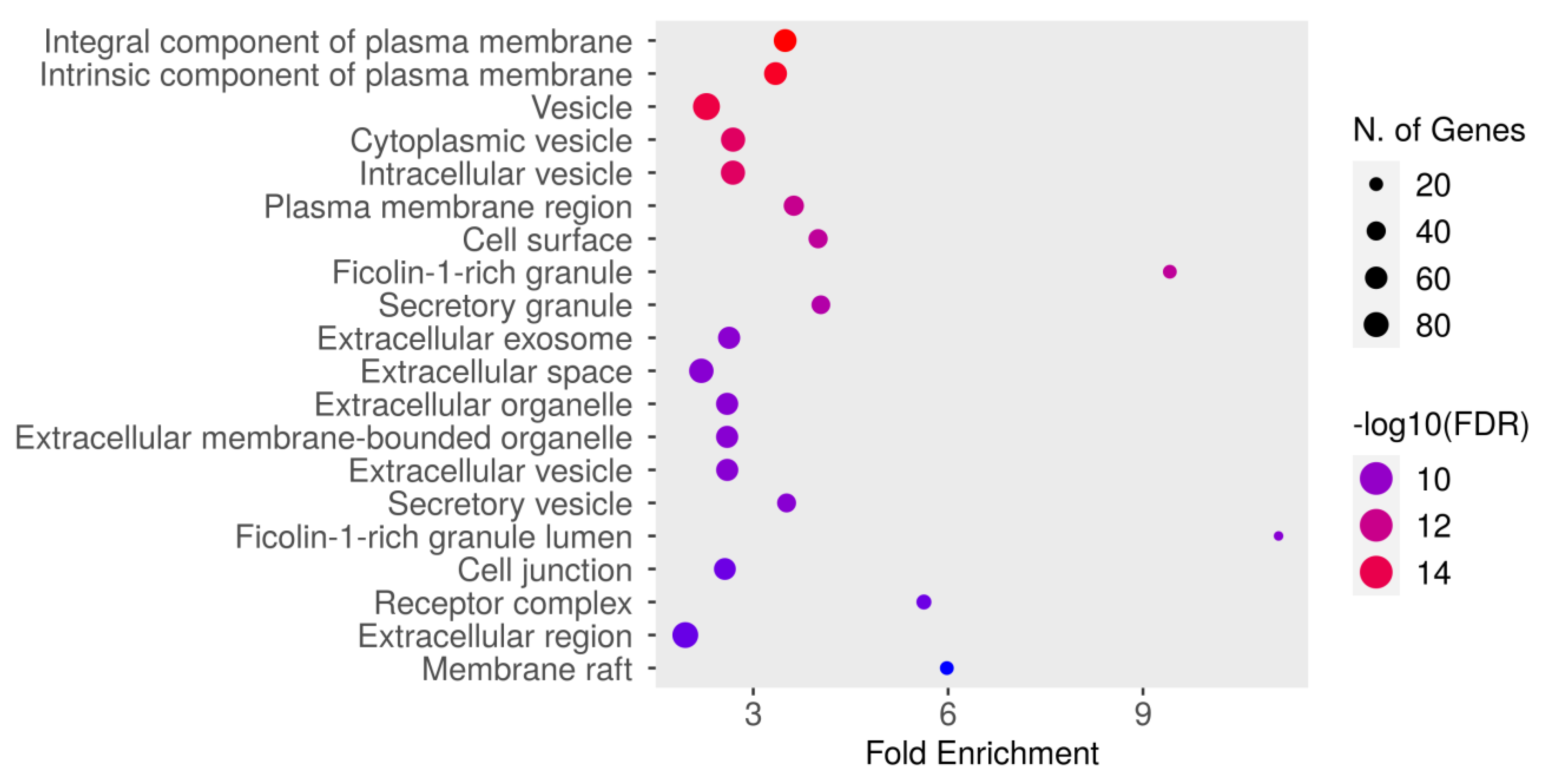
3.5.4. GO Cellular Component Enrichment Analysis
The GO cellular component enrichment analysis for dapagliflozin and chronic kidney disease (CKD) identified key cellular structures and regions significantly associated with the intersecting targets, ranked by FDR values and fold enrichment, as shown in Figure 6 and Table 6. The most enriched component was the integral component of plasma membrane (GO:0005887) with an FDR of 1.8106 × 10−16 and a fold enrichment of 3.491. This was closely followed by the intrinsic component of plasma membrane (GO:0031226) and vesicle (GO:0031982). Other significantly enriched components included cytoplasmic vesicle (GO:0031410), intracellular vesicle (GO:0097708), and plasma membrane region (GO:0098590). Enrichment was also observed in cell surface (GO:0009986) and ficolin-1-rich granule (GO:0101002). Further enriched components included secretory granule (GO:0030141) and extracellular exosome (GO:0070062). The analysis also identified extracellular space (GO:0005615), extracellular organelle (GO:0043230), and extracellular vesicle (GO:1903561). Other notable components included secretory vesicle (GO:0099503), ficolin-1-rich granule lumen (GO:1904813), and cell junction (GO:0030054). Additionally, receptor complex (GO:0043235), extracellular region (GO:0005576), and membrane raft (GO:0045121) were significantly enriched. These results highlight the diverse cellular components potentially involved in the mechanisms of dapagliflozin in CKD, with a focus on plasma membrane-related structures, vesicles, and extracellular components critical for cellular communication and signaling.
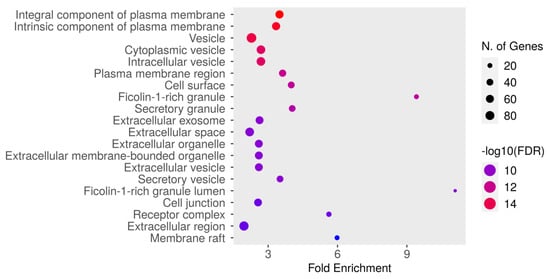
Figure 6.
The Gene Ontology (GO) cellular component enrichment analysis of intersecting targets of dapagliflozin and chronic kidney disease (CKD). The size of the dots represents the number of genes associated with each cellular component, and the color indicates the level of statistical significance, with red representing the most significant pathways.

Table 6.
GO cellular component enrichment analysis of intersecting targets shared by dapagliflozin and chronic kidney disease.
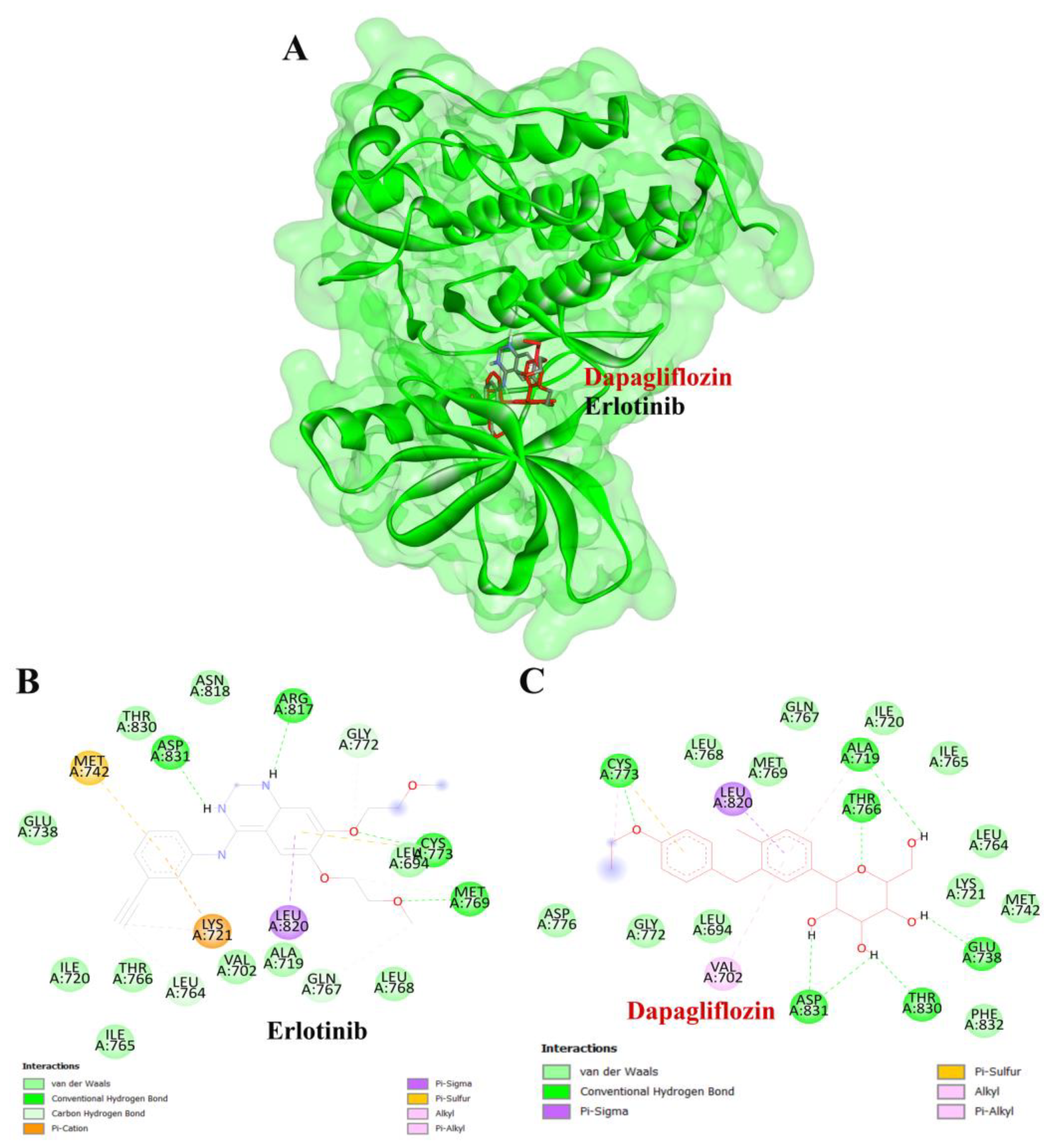
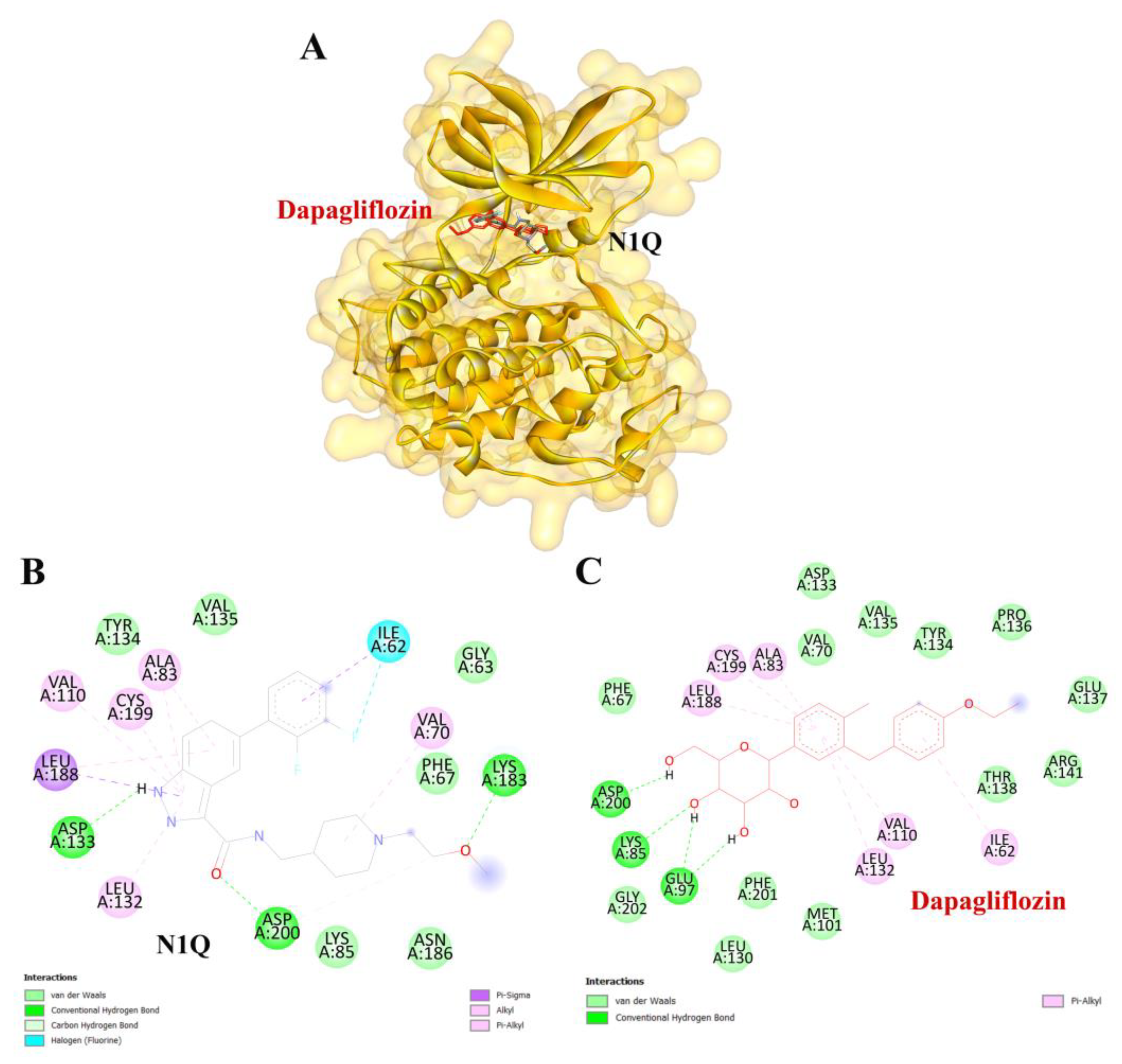
3.6. Molecular Docking Verification
To validate the credibility of drug–target interactions, molecular docking analysis was specifically conducted on the 10 hub proteins selected as targets. In this study, the stability and inhibitory potency of the ligand–receptor binding were assessed based on the binding energies between the ligand and protein. A binding energy below −8.0 kcal/mol or a docking score better than that of the positive control served as the criterion or cutoff, indicating a robust conformation of ligand binding to the receptor. The results of molecular docking for dapagliflozin are summarized in Table 7. Dapagliflozin exhibited significant inhibition against EGFR and GSK3β proteins, with docking scores of −8.42 and −7.70 kcal/mol, respectively. Moreover, dapagliflozin demonstrated a notable binding affinity to IL-6, with a binding energy better than that of HY-115910 (positive control). However, dapagliflozin bound to IL-6 at a different binding site compared to HY-115910 (Figure 7A,B). Additionally, dapagliflozin formed five hydrogen bonds with LEU64, LYS66, LYS86, GLU93, and THR138 of IL-6, along with hydrophobic interactions involving PRO65 and PRO139, as depicted in Figure 7C. As shown in Figure 8A, dapagliflozin also exhibited strong binding affinity against EGFR by binding at a site similar to that of erlotinib. Dapagliflozin formed seven hydrogen bonds with CYS773, THR766, ALA719, GLU738, THR830, and two with ASP831 (Figure 8C). Furthermore, dapagliflozin engaged in several hydrophobic interactions with CYS773, LEU820, ALA719, and VAL702 (Figure 8C). Notably, dapagliflozin demonstrated a significant binding affinity to GSK3β, with a binding energy of −7.70 kcal/mol, which was better than that of the positive control N1Q. Dapagliflozin formed four hydrogen bonds with ASP200, LYS85, and two with GLU97 in its interaction with GSK3β, binding at the same site as the positive control drug (Figure 9A–C). These findings highlight the bioactive potential of dapagliflozin, which exhibited notable binding energy and interactions with the top three key hub targets, indicating its significance in modulating these crucial molecular targets.

Table 7.
Docking score and inhibition constant of dapagliflozin against the top 10 hub targets compared to the positive control.

Figure 7.
Visualization of the protein–ligand docking interactions. (A) Three-dimensional view of dapagliflozin (red) and HY-115910 (black) docked with IL-6. (B) Two-dimensional schematic of the docking interaction between HY-115910 (positive control) and IL-6. (C) Two-dimensional schematic of the docking interaction between dapagliflozin and IL-6.
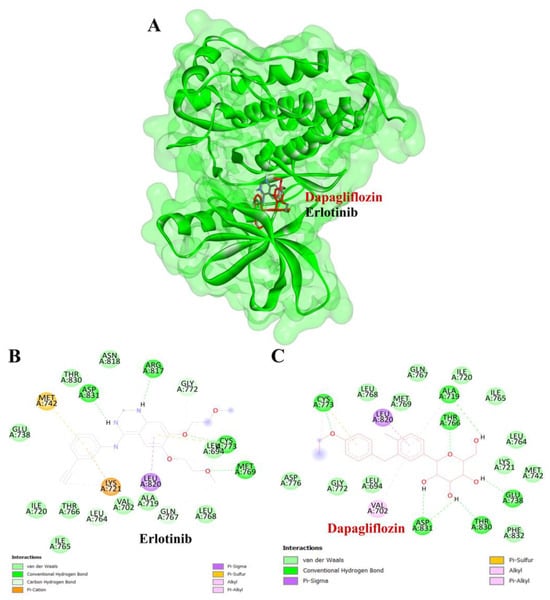
Figure 8.
Visualization of the protein–ligand docking interactions. (A) Three-dimensional view of dapagliflozin (red) and erlotinib (black) docked with EGFR. (B) Two-dimensional schematic of the docking interaction between erlotinib (positive control) and EGFR. (C) Two-dimensional schematic of the docking interaction between dapagliflozin and EGFR.
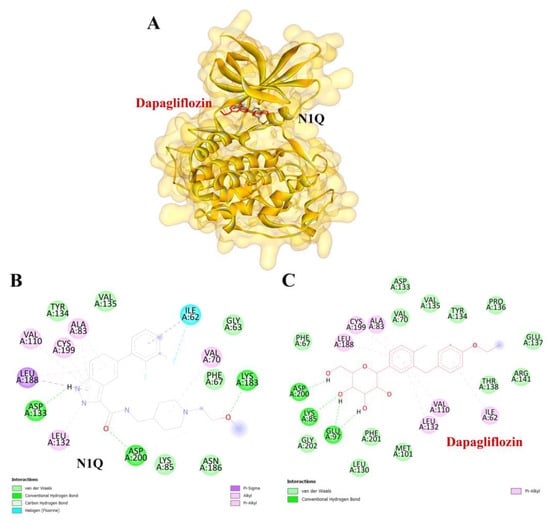
Figure 9.
Visualization of the protein–ligand docking interactions. (A) A 3D structure showing the docking of dapagliflozin (in red) and N1Q (in black) with the GSK3β protein. (B) A 2D schematic of N1Q (positive control) binding with GSK3β. (C) A 2D schematic of the docking interaction between dapagliflozin and GSK3β.
4. Discussion
This study demonstrates the therapeutic potential of dapagliflozin in CKD by identifying 208 shared molecular targets through network pharmacology approaches. These targets, derived from a combination of dapagliflozin-related and CKD-related gene datasets, highlight the drug’s ability to modulate key biological processes implicated in CKD. The analysis of the PPI network identified ten hub proteins, including GAPDH, IL-6, SRC, EGFR, HSP90AA1, NFKB1, CASP3, HSP90AB1, MAPK3, and GSK3β, which are central nodes in the network and may serve as pivotal mediators of dapagliflozin’s therapeutic effects [16].
The ADMET analysis affirmed dapagliflozin’s favorable pharmacokinetic and toxicity profiles, establishing it as a promising oral therapeutic for CKD. The drug demonstrated high gastrointestinal absorption, low toxicity risks, and no violations of Lipinski’s rule of five, ensuring good oral bioavailability [31]. Additionally, its low cardiac and hepatotoxicity profiles further reinforce its suitability for long-term use. The GO enrichment analysis provided valuable insights into biological processes, molecular functions, and cellular components related to dapagliflozin’s targets. Enriched biological processes included responses to chemical stimuli, signaling regulation, and metabolic processes, underscoring its role in mitigating inflammation and oxidative stress. Molecular function analysis emphasized kinase activity, nucleotide binding, and catalytic activity, which are essential for intracellular signaling and cellular regulation. Cellular component enrichment highlighted the significance of plasma membrane structures, vesicles, and extracellular regions as mediators of the drug’s effects [32]. The KEGG pathway analysis identified critical pathways, such as the PI3K-Akt signaling pathway, MAPK signaling pathway, and AGE-RAGE signaling in diabetic complications, which are closely associated with CKD pathophysiology [33,34,35]. The PI3K-Akt pathway is involved in renal cell survival, proliferation, and immune responses, and its dysregulation contributes to renal fibrosis, chronic inflammation, and oxidative damage. Excessive activation of PI3K-Akt promotes epithelial-to-mesenchymal transition (EMT) and mitochondrial dysfunction, exacerbating renal injury [33]. Conversely, the inhibition of this pathway has been shown to mitigate renal fibrosis and inflammation. Similarly, the MAPK pathway is implicated in CKD progression by inducing pro-inflammatory cytokines and fibrotic mediators, leading to tubulointerstitial fibrosis and glomerulosclerosis [36]. MAPK activation triggers oxidative stress and apoptosis in renal tubular cells, further contributing to CKD pathogenesis. The AGE-RAGE pathway, particularly relevant in diabetic nephropathy, accelerates CKD progression through the accumulation of advanced glycation end-products (AGEs), which activate NF-κB signaling, increase oxidative stress, and induce endothelial dysfunction and podocyte injury, resulting in inflammation and fibrosis, promoting proteinuria and renal function decline [35]. These pathways, involved in cellular proliferation, oxidative stress, inflammation, and metabolic regulation, provide mechanistic insights into dapagliflozin’s diverse effects.
While direct evidence of dapagliflozin’s modulation of the PI3K-Akt, MAPK, and AGE-RAGE pathways specifically in CKD models is limited, several studies suggest its influence on these pathways in related contexts. A recent in vitro study demonstrated that dapagliflozin attenuates isoproterenol-induced hypertrophy in cardiomyocytes by activating the AKT pathway, leading to reduced oxidative stress and inflammation. In aortic endothelial cells, dapagliflozin restored AKT and PI3K expression, enhanced MAPK activation, and downregulated inflammatory cytokines, indicating its potential to preserve vascular function and improve endothelial health. Additionally, dapagliflozin upregulated NRF2 expression, positively influencing β-cell function and stress response [37]. Regarding the AGE-RAGE pathway, the activation of RAGE is increased in CKD and contributes to cellular dysfunction, tissue injury, fibrosis, and inflammation. While direct modulation of the AGE-RAGE pathway by dapagliflozin in CKD models has not been conclusively demonstrated, the drug’s anti-inflammatory and antioxidative properties may indirectly influence this pathway, potentially mitigating RAGE-mediated effects [37]. Regarding the AGE-RAGE pathway, the activation of RAGE is increased in CKD and contributes to cellular dysfunction, tissue injury, fibrosis, and inflammation. While direct modulation of the AGE-RAGE pathway by dapagliflozin in CKD models has not been conclusively demonstrated, the drug’s anti-inflammatory and antioxidative properties may indirectly influence this pathway, potentially mitigating RAGE-mediated effects [38].
Findings from the DAPA-CKD trial provide strong clinical evidence of dapagliflozin’s renoprotective effects beyond glucose lowering. In this trial, dapagliflozin significantly reduced CKD progression by 39% and all-cause mortality by 31%, which are benefits observed regardless of diabetes status. These findings suggest that dapagliflozin may indirectly influence inflammation, oxidative stress, and fibrotic pathways, which are central to CKD progression [10]. Similarly, the DAPA-HF trial showed a 26% reduction in cardiovascular death or heart failure hospitalization, further supporting its disease-modulating effects [39]. Other pathways related to lipid metabolism, atherosclerosis, and cardiovascular processes further support the potential of dapagliflozin to manage CKD complications [40].
Interestingly, our analysis revealed a potential connection between prostate cancer, hepatitis B, and CKD progression. We hypothesize that this association may be attributed to shared pathophysiological mechanisms, including inflammation, immune activation, and cellular proliferation. Prostate cancer has been linked to a higher incidence of acute kidney injury (AKI) and CKD, with studies reporting a 1.47-fold increased risk of AKI in prostate cancer patients compared to those without cancer. Additionally, androgen deprivation therapy, a common treatment for prostate cancer, has been associated with renal complications, further supporting a possible connection between prostate cancer-related pathways and CKD progression [41]. Moreover, chronic hepatitis B virus (HBV) infection is a recognized risk factor for CKD development, with HBV-infected individuals exhibiting a higher prevalence of CKD and glomerular diseases, such as membranous nephropathy and polyarteritis nodosa, contributing to renal injury and dysfunction [42]. The identification of prostate cancer and hepatitis B pathways in our KEGG analysis suggests that these conditions may have a broader impact on renal pathology.
In a previous study, network pharmacology was utilized to examine the therapeutic roles of canagliflozin and dapagliflozin in atherosclerosis, revealing that these drugs act by targeting key molecules such as Akt1, MAPK1, MAPK14, SRC, and EGFR [43]. Building on this, our recent investigation employed network pharmacology and molecular docking to explore the therapeutic potential of dapagliflozin in chronic kidney disease (CKD). By integrating data from multiple databases, we identified 208 CKD-related targets for dapagliflozin, focusing specifically on the ten most interconnected proteins, which are integral to the biological mechanisms underlying CKD pathogenesis. These findings underscore dapagliflozin’s ability to modulate diverse biological pathways and functions relevant to CKD progression. Clinical evidence further supports dapagliflozin’s efficacy, demonstrating a significant reduction in the risk of a 50% or greater decline in the estimated glomerular filtration rate (eGFR), progression to end-stage kidney disease, or death from renal or cardiovascular causes, compared to the placebo, in CKD patients regardless of diabetes status [10]. Additionally, in patients with stage 4 CKD and albuminuria, dapagliflozin consistently mitigated major kidney and cardiovascular risks and slowed eGFR decline without increasing adverse outcomes, aligning with broader trial findings [44]. The results underscore dapagliflozin’s significance as a therapeutic option for effectively managing CKD in a wide range of patient populations.
To complement our network pharmacology analysis, molecular docking revealed significant binding affinities between dapagliflozin and key proteins. The analysis confirmed dapagliflozin’s high binding affinity for critical targets, including EGFR, GSK3β, and IL-6. Notably, dapagliflozin exhibited a binding energy of −8.42 kcal/mol with EGFR, surpassing that of erlotinib. This interaction was facilitated by hydrogen bonds and hydrophobic interactions, indicating a stable ligand-receptor conformation (Table 2). The EGFR pathway plays a vital role in kidney development, tissue repair, and electrolyte balance. Dysregulation of this pathway has been extensively linked to the onset and progression of chronic kidney diseases, such as diabetic nephropathy, chronic allograft nephropathy, and polycystic kidney disease. This is attributed to its involvement in promoting renal cell proliferation, fibrosis, and inflammation. Experimental evidence strongly supports that aberrant EGFR signaling contributes to many forms of chronic kidney disease. Furthermore, abnormal EGFR activation has been implicated in mediating progressive kidney injury, particularly in diabetic kidney disease [45]. Inhibiting EGFR expression or activity has been shown to slow the progression of diabetic kidney injury, suggesting that directly targeting EGFR or its associated signaling pathways may be an effective strategy for preventing progressive kidney damage caused by diabetes [46].
Similarly, dapagliflozin demonstrated a high level of inhibition toward glycogen synthase kinase 3 beta (GSK3β), with a docking score of −7.70 kcal/mol, outperforming the positive control, N1Q. The strong binding affinities with both EGFR and GSK3β underscore dapagliflozin’s potential as a multi-target therapeutic agent in CKD. GSK3β contributes to mitochondrial damage and apoptosis by directly phosphorylating and activating pro-apoptotic proteins Bax and Caspase-3 [47]. Additionally, GSK3β activates the p65 subunit of NF-κB, thereby amplifying inflammatory processes [48]. It also inhibits Nrf2, a key antioxidant defender, by phosphorylating it and promoting its nuclear exclusion. This suppression of Nrf2 leads to oxidative stress in the kidney and impedes the transition from acute kidney injury (AKI) to CKD [49]. Furthermore, GSK3β-mediated Keap1-independent regulation of the Nrf2 antioxidant response acts as a molecular rheostat in the AKI-to-CKD transition [50]. These processes slow tubular recovery and contribute to the progression from AKI to CKD [51].
Dapagliflozin also exhibited significant binding affinity to IL-6, surpassing the binding energy of the positive control, HY-115910. Circulating interleukin-6 (IL-6) levels are often elevated in type 2 diabetes mellitus (T2DM) [52]. Increasing evidence highlights the critical role of IL-6 in the pathophysiology of cardiovascular and renal dysfunction [53], with IL-6 being recognized as a major contributor to kidney diseases [54]. Notably, dapagliflozin has been shown to reduce IL-6 levels more effectively than other medications. The anti-inflammatory properties of SGLT2 inhibitors, including dapagliflozin, support their broader use in managing diabetic complications related to kidney inflammation [55,56,57]. Although EGFR activation contributes to tubulointerstitial fibrosis and renal dysfunction, direct evidence of dapagliflozin modulating this pathway in CKD is currently lacking. However, its anti-inflammatory and antifibrotic properties suggest potential indirect effects. Similarly, IL-6, a key pro-inflammatory cytokine in CKD, drives systemic inflammation and endothelial dysfunction. Clinical studies indicate that dapagliflozin reduces IL-6 levels in patients with CKD and diabetes, highlighting a direct anti-inflammatory effect. This aligns with dapagliflozin’s broader anti-inflammatory profile, reinforcing the relevance of IL-6 in CKD pathophysiology [58]. This study integrates network pharmacology and molecular docking to offer a comprehensive understanding of dapagliflozin’s mechanisms of action. It underscores the drug’s potential to function beyond its primary role as an SGLT2 inhibitor, providing a promising approach for CKD treatment through multi-target modulation.
The findings from this study also provide a strong foundation for future experimental research and clinical applications in CKD treatment. The identification of 208 overlapping molecular targets and key signaling pathways, including PI3K-Akt, MAPK, and AGE-RAGE, suggests potential therapeutic mechanisms for dapagliflozin. Future in vitro and in vivo studies should focus on validating these pathways’ roles in CKD progression and assessing dapagliflozin’s efficacy in modulating them. Additionally, given its ability to target multiple aspects of CKD pathophysiology—such as inflammation, oxidative stress, and metabolic dysregulation—dapagliflozin could be explored as part of combination therapies to enhance renoprotective effects. Investigating its interactions with key proteins such as EGFR, IL-6, and GSK3β may offer new insights into optimizing treatment strategies.
Furthermore, personalized medicine approaches should be considered to identify patient-specific factors that influence drug response. Biomarker-driven studies may help stratify patients based on CKD progression risk and predict responsiveness to dapagliflozin. While clinical trials have demonstrated its efficacy in reducing renal injury markers and slowing eGFR decline, additional studies are needed to evaluate its benefits in broader CKD populations, including non-diabetic CKD, polycystic kidney disease, and transplant recipients. Long-term trials should assess its role in delaying dialysis initiation and reducing cardiovascular events. Additionally, novel drug formulations, such as nanotechnology-based delivery systems, could be explored to improve dapagliflozin’s bioavailability and target specificity while minimizing systemic side effects.
5. Conclusions
This study demonstrates the potential of dapagliflozin as a therapeutic agent for chronic kidney disease (CKD) by identifying 208 overlapping targets and elucidating its multi-target mechanisms through network pharmacology and molecular docking. Key pathways, including PI3K-Akt, MAPK, and AGE-RAGE signaling, were identified as critical to CKD pathophysiology, with hub proteins such as EGFR, IL-6, and GSK3β validated for their strong binding affinity to dapagliflozin. These findings highlight dapagliflozin’s ability to modulate inflammation, oxidative stress, and metabolic dysregulation, suggesting that its therapeutic utility extends beyond its established role as an SGLT2 inhibitor. This study emphasizes the value of computational approaches in drug discovery and provides a foundation for the further experimental validation and clinical application of dapagliflozin in CKD management.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/life15030437/s1, Table S1: Comparison of ADMET results: SwissADME vs. PkCSM.
Author Contributions
Conceptualization, A.P., A.T. and M.C.; methodology, A.P., A.T., R.N., R.L., T.S., S.R., J.C.H. and M.C.; software, A.P., A.T., R.N. and M.C.; validation, A.P., A.T. and M.C.; formal analysis, A.P., A.T. and M.C.; investigation, A.P., A.T. and M.C.; resources, A.P., A.T. and M.C.; data curation, A.P., A.T. and M.C.; writing—original draft preparation, A.P., A.T. and M.C.; writing—review and editing, A.P., A.T., J.C.H. and M.C.; visualization, A.P., A.T. and M.C.; supervision, M.C.; project administration, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study did not involve human or animal subjects, as it was based solely on data obtained from databases. Ethical approval was waived by the Human Research Ethics Committee of the Faculty of Medicine, Prince of Songkla University, as it met the criteria for exemption review (Approval No. REC.68-047-14-1; Approval date: 5 February 2025).
Informed Consent Statement
Our study is based on publicly available datasets with de-identified data, inform consents was not required. No new patient recruitment or identified patient information was used in this research.
Data Availability Statement
The original contributions presented in this study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Acknowledgments
We would like to thank the Nephrology Unit, Division of Internal Medicine, Faculty of Medicine, Prince of Songkla University, and the Research Excellence Center for Innovation and Health Products (RECIHP), Walailak University, for their support of this research.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ADME | Absorption, distribution, metabolism, and excretion |
| ADMET | Absorption, distribution, metabolism, excretion, and toxicity |
| ADT | AutoDock Tools |
| AGE-RAGE | Advanced glycation end-products—Receptor for advanced glycation end-products |
| BBB | Blood–brain barrier |
| CASP3 | Caspase-3 |
| CKD | Chronic kidney disease |
| CYP | Cytochrome P450 |
| DC | Degree centrality |
| EGFR | Epidermal growth factor receptor |
| eGFR | Estimated glomerular filtration rate |
| ESOL | Estimation of solubility |
| ESRD | End-stage renal disease |
| FDR | False discovery rate |
| GAPDH | Glyceraldehyde 3-phosphate dehydrogenase |
| GA | Genetic algorithm |
| GO | Gene ontology |
| GSK3β | Glycogen synthase kinase 3 beta |
| HBV | Hepatitis B virus |
| HF | Heart failure |
| HSP90AA1 | Heat shock protein 90 alpha family class A member 1 |
| HSP90AB1 | Heat shock protein 90 alpha family class B member 1 |
| IL-6 | Interleukin-6 |
| KEGG | Kyoto Encyclopedia of Genes and Genomes |
| LD50 | Lethal dose, 50% |
| LOAEL | Lowest observed adverse effect level |
| MAPK | Mitogen-activated protein kinase |
| MAPK3 | Mitogen-activated protein kinase 3 |
| MAPK14 | Mitogen-activated protein kinase 14 |
| NFKB1 | Nuclear factor kappa B subunit 1 |
| Nrf2 | Nuclear factor erythroid 2–related factor 2 |
| PDB | Protein Data Bank |
| pkCSM | Pharmacokinetics of small molecules |
| PI3K-Akt | Phosphoinositide 3-kinase—Protein kinase B |
| PPI | Protein-protein interaction |
| SEA | Similarity ensemble approach |
| SMILES | Simplified molecular input line entry system |
| SRC | Proto-oncogene tyrosine-protein kinase Src |
| STRING | Search tool for the retrieval of interacting genes/proteins |
| SwissADME | Swiss absorption, distribution, metabolism, and excretion |
| TNF-α | Tumor necrosis factor-α |
| TPSA | Topological polar surface area |
| UniProt | Universal Protein Resource |
| SMILES | Simplified molecular input line entry system |
References
- Zhang, S.; Ren, H.-F.; Du, R.-X.; Sun, W.-L.; Fu, M.-L.; Zhang, X.-C. Global, regional, and national burden of kidney dysfunction from 1990 to 2019: A systematic analysis from the global burden of disease study 2019. BMC Public Health 2023, 23, 1218. [Google Scholar] [CrossRef] [PubMed]
- Bello, A.K.; Okpechi, I.G.; Levin, A.; Ye, F.; Damster, S.; Arruebo, S.; Donner, J.A.; Caskey, F.J.; Cho, Y.; Davids, M.R.; et al. An update on the global disparities in kidney disease burden and care across world countries and regions. Lancet Glob. Health 2024, 12, e382–e395. [Google Scholar] [CrossRef] [PubMed]
- Ebert, T.; Neytchev, O.; Witasp, A.; Kublickiene, K.; Stenvinkel, P.; Shiels, P.G. Inflammation and oxidative stress in chronic kidney disease and dialysis patients. Antioxid. Redox Signal. 2021, 35, 1426–1448. [Google Scholar] [CrossRef]
- Altamura, S.; Pietropaoli, D.; Lombardi, F.; Del Pinto, R.; Ferri, C. An overview of chronic kidney disease pathophysiology: The impact of gut dysbiosis and oral disease. Biomedicines 2023, 11, 3033. [Google Scholar] [CrossRef]
- Zhong, J.; Yang, H.C.; Fogo, A.B. A perspective on chronic kidney disease progression. Am. J. Physiol. Renal Physiol. 2017, 312, F375–F384. [Google Scholar] [CrossRef] [PubMed]
- Amdur, R.L.; Feldman, H.I.; Gupta, J.; Yang, W.; Kanetsky, P.; Shlipak, M.; Rahman, M.; Lash, J.P.; Townsend, R.R.; Ojo, A.; et al. Inflammation and progression of CKD: The CRIC study. Clin. J. Am. Soc. Nephrol. 2016, 11, 1546–1556. [Google Scholar] [CrossRef]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-related mechanisms in chronic kidney disease prediction, progression, and outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
- Ratliff, B.B.; Abdulmahdi, W.; Pawar, R.; Wolin, M.S. Oxidant mechanisms in renal injury and disease. Antioxid. Redox Signal. 2016, 25, 119–146. [Google Scholar] [CrossRef]
- Daenen, K.; Andries, A.; Mekahli, D.; Van Schepdael, A.; Jouret, F.; Bammens, B. Oxidative stress in chronic kidney disease. Pediatr. Nephrol. 2019, 34, 975–991. [Google Scholar] [CrossRef]
- Heerspink, H.J.L.; Stefánsson, B.V.; Correa-Rotter, R.; Chertow, G.M.; Greene, T.; Hou, F.F.; Mann, J.F.E.; McMurray, J.J.V.; Lindberg, M.; Rossing, P.; et al. Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 2020, 383, 1436–1446. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Raz, I.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; Silverman, M.G.; Zelniker, T.A.; Kuder, J.F.; Murphy, S.A.; et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N. Engl. J. Med. 2019, 380, 347–357. [Google Scholar] [CrossRef]
- Nishiyama, A.; Kitada, K. Possible renoprotective mechanisms of SGLT2 inhibitors. Front. Med. 2023, 10, 1115413. [Google Scholar] [CrossRef]
- Sun, X.; Wang, G. Renal outcomes with sodium-glucose cotransporters 2 inhibitors. Front. Endocrinol. 2022, 13, 1063341. [Google Scholar] [CrossRef]
- Nørgaard, S.A.; Briand, F.; Sand, F.W.; Galsgaard, E.D.; Søndergaard, H.; Sørensen, D.B.; Sulpice, T. Nephropathy in diabetic db/db mice is accelerated by high protein diet and improved by the SGLT2 inhibitor dapagliflozin. Eur. J. Pharmacol. 2019, 860, 172537. [Google Scholar] [CrossRef] [PubMed]
- Shibusawa, R.; Yamada, E.; Okada, S.; Nakajima, Y.; Bastie, C.C.; Maeshima, A.; Kaira, K.; Yamada, M. Dapagliflozin rescues endoplasmic reticulum stress-mediated cell death. Sci. Rep. 2019, 9, 9887. [Google Scholar] [CrossRef] [PubMed]
- Chertow, G.M.; Correa-Rotter, R.; Vart, P.; Jongs, N.; McMurray, J.J.V.; Rossing, P.; Langkilde, A.M.; Sjöström, C.D.; Toto, R.D.; Wheeler, D.C.; et al. Effects of dapagliflozin in chronic kidney disease, with and without other cardiovascular medications: DAPA-CKD trial. J. Am. Heart Assoc. 2023, 12, e028739. [Google Scholar] [CrossRef] [PubMed]
- Vart, P.; Correa-Rotter, R.; Hou, F.F.; Jongs, N.; Chertow, G.M.; Langkilde, A.M.; McMurray, J.J.V.; Rossing, P.; Sjöström, C.D.; Stefansson, B.V.; et al. Efficacy and safety of dapagliflozin in patients with CKD across major geographic regions. Kidney Int. Rep. 2022, 7, 699–707. [Google Scholar] [CrossRef]
- Zhang, P.; Zhang, D.; Zhou, W.; Wang, L.; Wang, B.; Zhang, T.; Li, S. Network pharmacology: Towards the artificial intelligence-based precision traditional Chinese medicine. Brief. Bioinform. 2023, 25, bbad518. [Google Scholar] [CrossRef]
- Tedasen, A.; Chiabchalard, A.; Tencomnao, T.; Yamasaki, K.; Majima, H.J.; Phongphithakchai, A.; Chatatikun, M. Anti-melanogenic activity of ethanolic Eextract from Garcinia atroviridis fruits using in vitro experiments, network pharmacology, molecular docking, and molecular dynamics simulation. Antioxidants 2024, 13, 713. [Google Scholar] [CrossRef]
- Ren, X.; Yan, C.-X.; Zhai, R.-X.; Xu, K.; Li, H.; Fu, X.-J. Comprehensive survey of target prediction web servers for Traditional Chinese Medicine. Heliyon 2023, 9, e19151. [Google Scholar] [CrossRef]
- Consortium, T.U. UniProt: The universal protein knowledgebase in 2025. Nucleic Acids Res. 2024, 53, D609–D617. [Google Scholar] [CrossRef] [PubMed]
- Stelzer, G.; Rosen, N.; Plaschkes, I.; Zimmerman, S.; Twik, M.; Fishilevich, S.; Stein, T.I.; Nudel, R.; Lieder, I.; Mazor, Y.; et al. The GeneCards suite: From gene data mining to disease genome sequence analyses. Curr. Protoc. Bioinf. 2016, 54, 1.30.1–1.30.33. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.; Chai, J.; Yuan, S.; Mai, C.; Cai, L.; Murphy, R.W.; Zhou, W.; Luo, J. VennPainter: A Tool for the comparison and identification of candidate genes based on venn diagrams. PLoS ONE 2016, 11, e0154315. [Google Scholar] [CrossRef]
- Szklarczyk, D.; Kirsch, R.; Koutrouli, M.; Nastou, K.; Mehryary, F.; Hachilif, R.; Gable, A.L.; Fang, T.; Doncheva, N.T.; Pyysalo, S.; et al. The STRING database in 2023: Protein–protein association networks and functional enrichment analyses for any sequenced genome of interest. Nucleic Acids Res. 2023, 51, D638–D646. [Google Scholar] [CrossRef]
- Franz, M.; Lopes, C.T.; Fong, D.; Kucera, M.; Cheung, M.; Siper, M.C.; Huck, G.; Dong, Y.; Sumer, O.; Bader, G.D. Cytoscape.js 2023 update: A graph theory library for visualization and analysis. Bioinformatics 2023, 39, btad031. [Google Scholar] [CrossRef]
- Ge, S.X.; Jung, D.; Yao, R. ShinyGO: A graphical gene-set enrichment tool for animals and plants. Bioinformatics 2020, 36, 2628–2629. [Google Scholar] [CrossRef]
- Burley, S.K.; Berman, H.M.; Duarte, J.M.; Feng, Z.; Flatt, J.W.; Hudson, B.P.; Lowe, R.; Peisach, E.; Piehl, D.W.; Rose, Y.; et al. Protein data bank: A comprehensive review of 3D structure holdings and worldwide utilization by researchers, educators, and students. Biomolecules 2022, 12, 1425. [Google Scholar] [CrossRef] [PubMed]
- Burley, S.K.; Bhikadiya, C.; Bi, C.; Bittrich, S.; Chao, H.; Chen, L.; Craig, P.A.; Crichlow, G.V.; Dalenberg, K.; Duarte, J.M.; et al. RCSB Protein Data Bank (RCSB.org): Delivery of experimentally-determined PDB structures alongside one million computed structure models of proteins from artificial intelligence/machine learning. Nucleic Acids Res. 2023, 51, D488–D508. [Google Scholar] [CrossRef]
- El-Hachem, N.; Haibe-Kains, B.; Khalil, A.; Kobeissy, F.H.; Nemer, G. AutoDock and AutoDockTools for protein-ligand docking: Beta-site amyloid precursor protein cleaving enzyme 1(BACE1) as a case study. Methods Mol. Biol. 2017, 1598, 391–403. [Google Scholar] [CrossRef]
- Pettersen, E.F.; Goddard, T.D.; Huang, C.C.; Meng, E.C.; Couch, G.S.; Croll, T.I.; Morris, J.H.; Ferrin, T.E. UCSF chimeraX: Structure visualization for researchers, educators, and developers. Protein Sci. 2021, 30, 70–82. [Google Scholar] [CrossRef]
- Daina, A.; Michielin, O.; Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 2017, 7, 42717. [Google Scholar] [CrossRef] [PubMed]
- Hyde, C.L.; Nagle, M.W.; Tian, C.; Chen, X.; Paciga, S.A.; Wendland, J.R.; Tung, J.Y.; Hinds, D.A.; Perlis, R.H.; Winslow, A.R. Identification of 15 genetic loci associated with risk of major depression in individuals of European descent. Nat. Genet. 2016, 48, 1031–1036. [Google Scholar] [CrossRef]
- Wang, H.; Gao, L.; Zhao, C.; Fang, F.; Liu, J.; Wang, Z.; Zhong, Y.; Wang, X. The role of PI3K/Akt signaling pathway in chronic kidney disease. Int. Urol. Nephrol. 2024, 56, 2623–2633. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Q.; Tang, B.; Zhang, C. Signaling pathways of chronic kidney diseases, implications for therapeutics. Signal Transduct. Target. Ther. 2022, 7, 182. [Google Scholar] [CrossRef]
- Fotheringham, A.K.; Gallo, L.A.; Borg, D.J.; Forbes, J.M. Advanced glycation end products (AGEs) and chronic kidney disease: Does the modern diet AGE the kidney? Nutrients 2022, 14, 2675. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, H.; Radford, R.; Slyne, J.; O’Connell, S.; Slattery, C.; Ryan, M.P.; McMorrow, T. The Role of MAPK in Drug-Induced Kidney Injury. J. Signal Transduct. 2012, 2012, 463617. [Google Scholar] [CrossRef]
- Alsereidi, F.R.; Khashim, Z.; Marzook, H.; Al-Rawi, A.M.; Salomon, T.; Almansoori, M.K.; Madkour, M.M.; Hamam, A.M.; Ramadan, M.M.; Peterson, Q.P.; et al. Dapagliflozin mitigates cellular stress and inflammation through PI3K/AKT pathway modulation in cardiomyocytes, aortic endothelial cells, and stem cell-derived β cells. Cardiovasc. Diabetol. 2024, 23, 388. [Google Scholar] [CrossRef]
- Curran, C.S.; Kopp, J.B. RAGE pathway activation and function in chronic kidney disease and COVID-19. Front. Med. 2022, 9, 970423. [Google Scholar] [CrossRef]
- McMurray, J.J.V.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
- Kanehisa, M.; Sato, Y.; Kawashima, M. KEGG mapping tools for uncovering hidden features in biological data. Protein Sci. 2022, 31, 47–53. [Google Scholar] [CrossRef]
- Cardwell, C.R.; O’Sullivan, J.M.; Jain, S.; Hicks, B.M.; Devine, P.A.; McMenamin, Ú.C. Hormone therapy use and the risk of acute kidney injury in patients with prostate cancer: A population-based cohort study. Prostate Cancer Prostatic Dis. 2021, 24, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.S.; Ryu, S.; Chang, Y.; Caínzos-Achirica, M.; Kwon, M.-J.; Zhao, D.; Shafi, T.; Lazo, M.; Pastor-Barriuso, R.; Shin, H.; et al. Hepatitis B virus infection and development of chronic kidney disease: A cohort study. BMC Nephrol. 2018, 19, 353. [Google Scholar] [CrossRef]
- Wang, J.; Li, D.; Ju, W.; Wang, H. A Network Pharmacology to Explore the Potential Targets of Canagliflozin and Dapagliflozin in Treating Atherosclerosis. J. Vasc. Dis. 2022, 1, 53–70. [Google Scholar] [CrossRef]
- Chertow, G.M.; Vart, P.; Jongs, N.; Toto, R.D.; Gorriz, J.L.; Hou, F.F.; McMurray, J.J.V.; Correa-Rotter, R.; Rossing, P.; Sjöström, C.D.; et al. Effects of dapagliflozin in stage 4 chronic kidney disease. J. Am. Soc. Nephrol. 2021, 32, 2352–2361. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.C. The role of the epidermal growth factor receptor in diabetic kidney disease. Cells 2022, 11, 3416. [Google Scholar] [CrossRef]
- Harskamp, L.R.; Gansevoort, R.T.; van Goor, H.; Meijer, E. The epidermal growth factor receptor pathway in chronic kidney diseases. Nat. Rev. Nephrol. 2016, 12, 496–506. [Google Scholar] [CrossRef]
- Wang, Z.; Havasi, A.; Gall, J.; Bonegio, R.; Li, Z.; Mao, H.; Schwartz, J.H.; Borkan, S.C. GSK3beta promotes apoptosis after renal ischemic injury. J. Am. Soc. Nephrol. 2010, 21, 284–294. [Google Scholar] [CrossRef]
- Zhao, K.; Chen, C.; Shi, Q.; Deng, W.; Zuo, T.; He, X.; Liu, T.; Zhao, L.; Wang, W. Inhibition of glycogen synthase kinase-3β attenuates acute kidney injury in sodium taurocholate-induced severe acute pancreatitis in rats. Mol. Med. Rep. 2014, 10, 3185–3192. [Google Scholar] [CrossRef]
- Lu, M.; Wang, P.; Qiao, Y.; Jiang, C.; Ge, Y.; Flickinger, B.; Malhotra, D.K.; Dworkin, L.D.; Liu, Z.; Gong, R. GSK3β-mediated Keap1-independent regulation of Nrf2 antioxidant response: A molecular rheostat of acute kidney injury to chronic kidney disease transition. Redox Biol. 2019, 26, 101275. [Google Scholar] [CrossRef]
- Bao, H.; Ge, Y.; Wang, Z.; Zhuang, S.; Dworkin, L.; Peng, A.; Gong, R. Delayed administration of a single dose of lithium promotes recovery from AKI. J. Am. Soc. Nephrol. 2014, 25, 488–500. [Google Scholar] [CrossRef]
- Jamadar, A.; Rao, R. Glycogen synthase kinase-3 signaling in acute kidney injury. Nephron 2020, 144, 609–612. [Google Scholar] [CrossRef] [PubMed]
- Mirza, S.; Hossain, M.; Mathews, C.; Martinez, P.; Pino, P.; Gay, J.L.; Rentfro, A.; McCormick, J.B.; Fisher-Hoch, S.P. Type 2-diabetes is associated with elevated levels of TNF-alpha, IL-6 and adiponectin and low levels of leptin in a population of Mexican Americans: A cross-sectional study. Cytokine 2012, 57, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Kreiner, F.F.; Kraaijenhof, J.M.; von Herrath, M.; Hovingh, G.K.K.; von Scholten, B.J. Interleukin 6 in diabetes, chronic kidney disease, and cardiovascular disease: Mechanisms and therapeutic perspectives. Expert Rev. Clin. Immunol. 2022, 18, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Magno, A.L.; Herat, L.Y.; Carnagarin, R.; Schlaich, M.P.; Matthews, V.B. Current knowledge of IL-6 cytokine family members in acute and chronic kidney disease. Biomedicines 2019, 7, 19. [Google Scholar] [CrossRef]
- Gohari, S.; Ismail-Beigi, F.; Mahjani, M.; Ghobadi, S.; Jafari, A.; Ahangar, H.; Gohari, S. The effect of sodium-glucose co-transporter-2 (SGLT2) inhibitors on blood interleukin-6 concentration: A systematic review and meta-analysis of randomized controlled trials. BMC Endocr. Disord. 2023, 23, 257. [Google Scholar] [CrossRef]
- Llerena-Velastegui, J.; Santamaria-Lasso, M.; Mejia-Mora, M.; Granda-Munoz, A.; Trujillo-Delgado, M.; Hurtado-Alzate, C.; de Jesus, A.; Coelho, P.M.; Baldelomar-Ortiz, J. Impact of sodium-glucose cotransporter 2 inhibitors on cardiovascular and Renal outcomes in heart failure patients with type 2 fiabetes: A literature review. J. Clin. Med. Res. 2024, 16, 398–410. [Google Scholar] [CrossRef] [PubMed]
- Tziastoudi, M.; Pissas, G.; Golfinopoulos, S.; Filippidis, G.; Dousdampanis, P.; Eleftheriadis, T.; Stefanidis, I. Sodium–glucose transporter 2 (SGLT2) inhibitors and iron deficiency in heart failure and chronic kidney disease: A literature review. Life 2023, 13, 2338. [Google Scholar] [CrossRef]
- Koshino, A.; Neuen, B.L.; Jongs, N.; Pollock, C.; Greasley, P.J.; Andersson, E.-M.; Hammarstedt, A.; Karlsson, C.; Langkilde, A.M.; Wada, T.; et al. Effects of dapagliflozin and dapagliflozin-saxagliptin on erythropoiesis, iron and inflammation markers in patients with type 2 diabetes and chronic kidney disease: Data from the DELIGHT trial. Cardiovasc. Diabetol. 2023, 22, 330. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).