Portal Vein Pulsatility: A Valuable Approach for Monitoring Venous Congestion and Prognostic Evaluation in Acute Decompensated Heart Failure
Abstract
1. Introduction
2. Materials and Methods
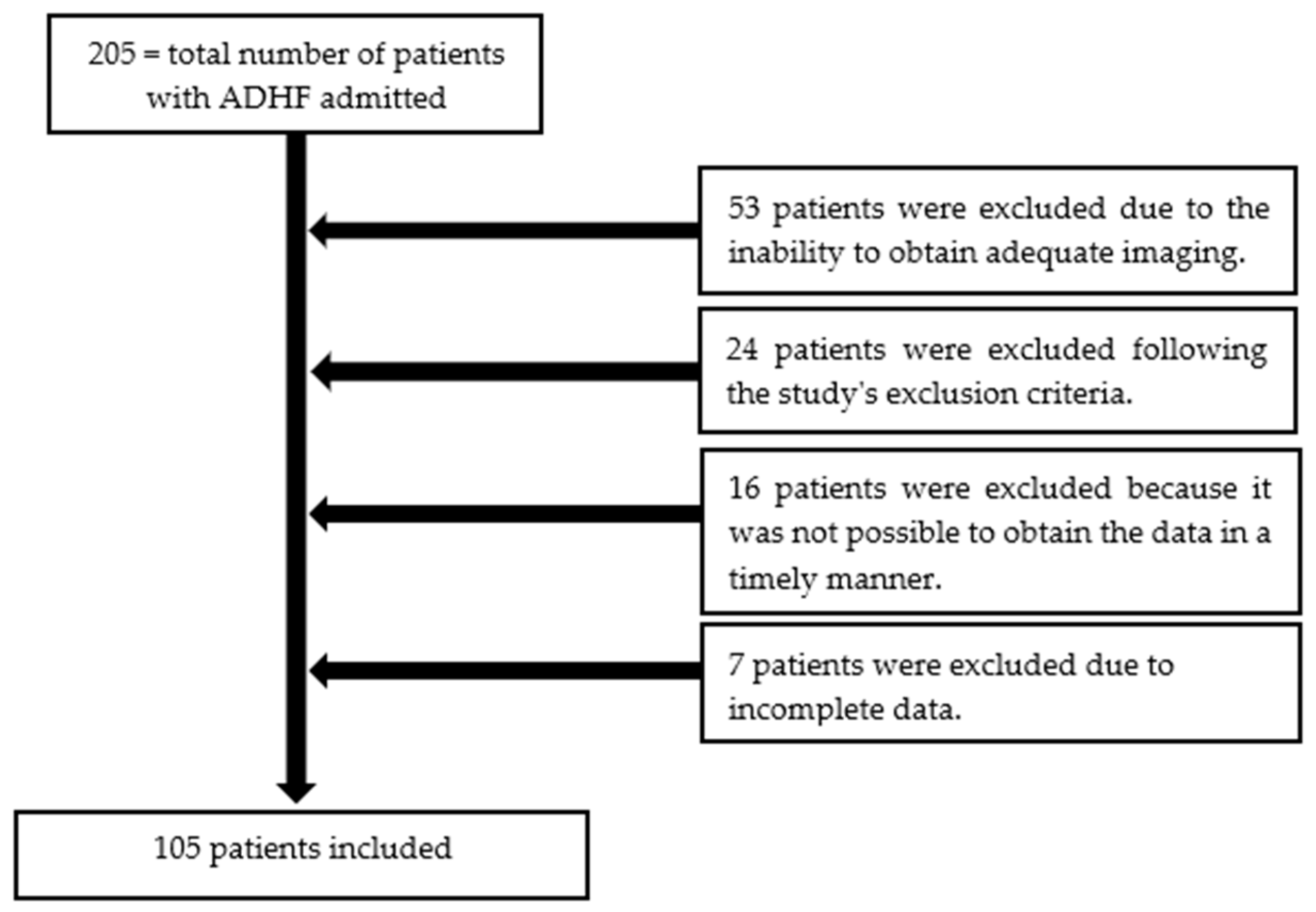
2.1. Population
- The inclusion criteria were as follows:
- Patients aged > 18 years.
- Patients with de novo HF, regardless of left ventricular ejection fraction.
- Patients with recurrent episodes of HF decompensation, regardless of left ventricular ejection fraction.
- Patients in cardiogenic shock.
- Patients with acute HF associated with acute coronary syndromes, acute myocarditis, and congenital heart diseases.
- Patients with dyspnea due to concomitant pulmonary diseases: severe pulmonary fibrosis/chronic obstructive pulmonary disease, patients with lung cancer or pneumonia.
- Patients with severe liver disease (Child-Pugh C).
- Patients with severe chronic kidney disease (glomerular filtration rate < 15 mL/min/1.73 m2) or on dialysis.
- Patients with severe anemia (hemoglobin < 7 g/dL).
- Patients with advanced neoplasms and a life expectancy < 1 year.
- Patients with septic shock.
- Difficult ultrasound imaging.
- Pregnant women.
2.2. Clinical and Biochemical Evaluation
2.3. Echocardiography and Portal Vein Ultrasonography
2.3.1. Echocardiography
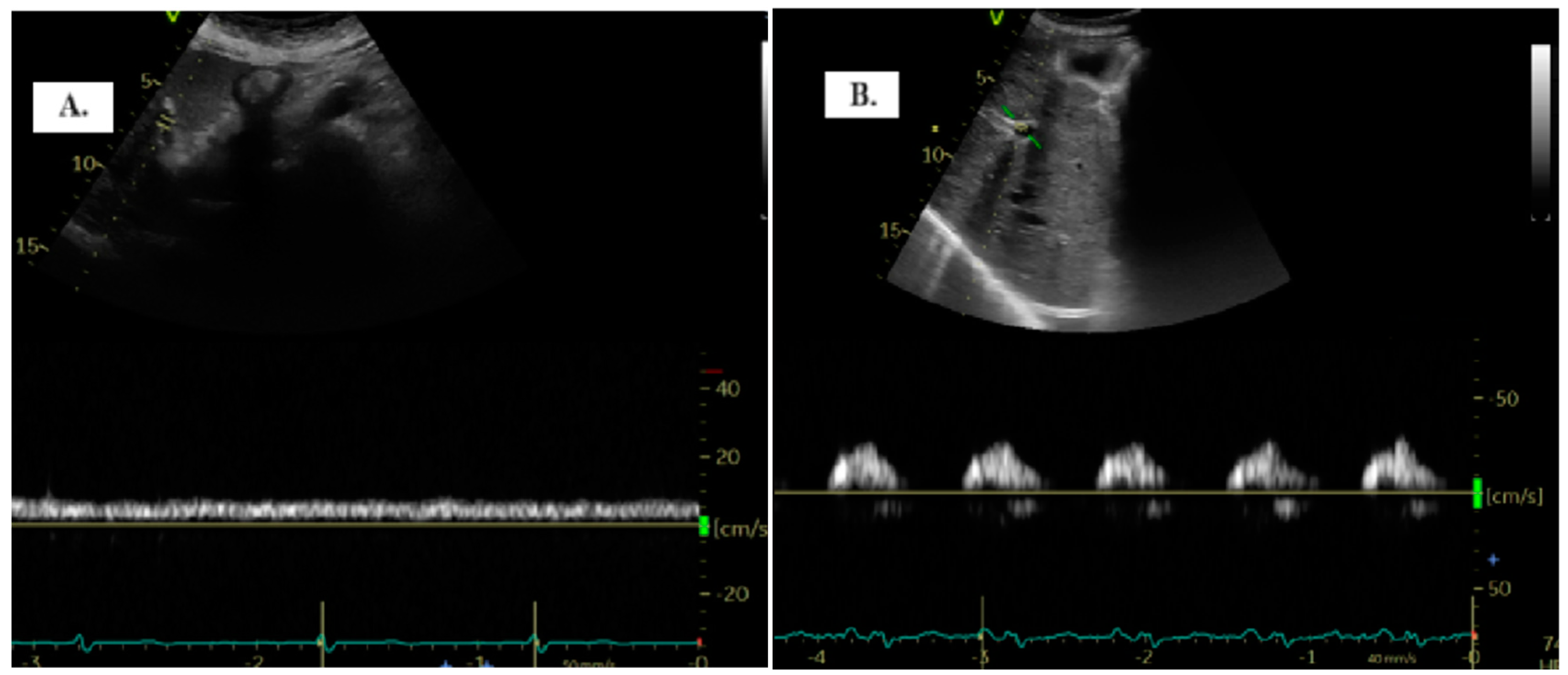
2.3.2. Portal Vein Ultrasonography
2.4. Statistical Analysis
3. Results
3.1. PVPI and Commonly Used Congestion Parameters
3.2. PVPI in Patients with Renal Dysfunction and Hyponatremia
3.3. Hospital Rehospitalization and Mortality
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pandhi, P.; ter Maaten, J.M.; Anker, S.D.; Ng, L.L.; Metra, M.; Samani, N.J.; Lang, C.C.; Dickstein, K.; de Boer, R.A.; van Veldhuisen, D.J.; et al. Pathophysiologic Processes and Novel Biomarkers Associated with Congestion in Heart Failure. JACC Heart Fail. 2022, 10, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Felker, G.M.; Fudim, M. Are We Getting Any Closer to Understanding Congestion? JACC Heart Fail. 2022, 10, 633–636. [Google Scholar] [CrossRef] [PubMed]
- Pellicori, P.; Platz, E.; Dauw, J.; ter Maaten, J.M.; Martens, P.; Pivetta, E.; Cleland, J.G.F.; McMurray, J.J.V.; Mullens, W.; Solomon, S.D.; et al. Ultrasound imaging of congestion in heart failure: Examinations beyond the heart. Eur. J. Heart Fail. 2021, 23, 703–712. [Google Scholar] [CrossRef] [PubMed]
- Verbrugge, F.H.; Guazzi, M.; Testani, J.M.; Borlaug, B.A. Altered Hemodynamics and End-Organ Damage in Heart Failure. Circulation 2020, 142, 998–1012. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, N.R.; Mazzola, M.; Bandini, G.; Barbieri, G.; Spinelli, S.; De Biase, N.; Masi, S.; Moggi-Pignone, A.; Ghiadoni, L.; Taddei, S.; et al. Prognostic Role of Sonographic Decongestion in Patients with Acute Heart Failure with Reduced and Preserved Ejection Fraction: A Multicentre Study. J. Clin. Med. 2023, 12, 773. [Google Scholar] [CrossRef]
- Girerd, N.; Seronde, M.F.; Coiro, S.; Chouihed, T.; Bilbault, P.; Braun, F.; Kenizou, D.; Maillier, B.; Nazeyrollas, P.; Roul, G.; et al. Integrative Assessment of Congestion in Heart Failure Throughout the Patient Journey. JACC Heart Fail. 2018, 6, 273–285. [Google Scholar] [CrossRef]
- Bozkurt, B. Targets for Success in Treatment of Patients Hospitalized for Heart Failure. JACC Heart Fail. 2022, 10, 782–784. [Google Scholar] [CrossRef]
- Anastasiou, V.; Peteinidou, E.; Moysidis, D.V.; Daios, S.; Gogos, C.; Liatsos, A.C.; Didagelos, M.; Gossios, T.; Efthimiadis, G.K.; Karamitsos, T.; et al. Multiorgan Congestion Assessment by Venous Excess Ultrasound Score in Acute Heart Failure. J. Am. Soc. Echocardiogr. 2024. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Soliman-Aboumarie, H.; Denault, A.Y. How to assess systemic venous congestion with point of care ultrasound. Eur. Heart J. Cardiovasc. Imaging 2023, 24, 177–180. [Google Scholar] [CrossRef]
- Singh, S.; Koratala, A. Utility of Doppler ultrasound derived hepatic and portal venous waveforms in the management of heart failure exacerbation. Clin. Case Rep. 2020, 8, 1489–1493. [Google Scholar] [CrossRef]
- Deschamps, J.; Denault, A.; Galarza, L.; Rola, P.; Ledoux-Hutchinson, L.; Huard, K.; Gebhard, C.E.; Calderone, A.; Canty, D.; Beaubien-Souligny, W. Venous Doppler to Assess Congestion: A Comprehensive Review of Current Evidence and Nomenclature. Ultrasound Med. Biol. 2023, 49, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Ilieșiu, A.M.; Hodorogea, A.S.; Balahura, A.M.; Bădilă, E. Non-Invasive Assessment of Congestion by Cardiovascular and Pulmonary Ultrasound and Biomarkers in Heart Failure. Diagn. 2022, 12, 962. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, Y.; Ishii, S.; Yazaki, M.; Fujita, T.; Iida, Y.; Kaida, T.; Nabeta, T.; Nakatani, E.; Maekawa, E.; Yanagisawa, T.; et al. Portal congestion and intestinal edema in hospitalized patients with heart failure. Heart Vessel. 2018, 33, 740–751. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726, Erratum in: Eur. Heart J. 2021, 42, 4901. [Google Scholar] [CrossRef] [PubMed]
- Bouabdallaoui, N.; Beaubien-Souligny, W.; Oussaïd, E.; Henri, C.; Racine, N.; Denault, A.Y.; Rouleau, J.L. Assessing Splanchnic Compartment Using Portal Venous Doppler and Impact of Adding It to the EVEREST Score for Risk Assessment in Heart Failure. CJC Open 2020, 2, 311–320. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging. 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Kuwahara, N.; Honjo, T.; Sone, N.; Imanishi, J.; Nakayama, K.; Kamemura, K.; Iwahashi, M.; Ohta, S.; Kaihotsu, K. Clinical impact of portal vein pulsatility on the prognosis of hospitalized patients with acute heart failure. World J. Cardiol. 2023, 15, 599–608. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Meani, P.; Pagnoni, M.; Mondellini, G.M.; Fiorenza, S.; Brunner-La Rocca, H.P. Impact of loop diuretic dosage in a population of patients with acute heart failure: A retrospective analysis. Front. Cardiovasc. Med. 2023, 10, 1267042. [Google Scholar] [CrossRef]
- Metra, M.; Davison, B.; Bettari, L.; Sun, H.; Edwards, C.; Lazzarini, V.; Piovanelli, B.; Carubelli, V.; Bugatti, S. Lombardi. Is worsening renal function an ominous prognostic sign in patients with acute heart failure? The role of congestion and its interaction with renal function. Circ. Heart Fail. 2012, 5, 54–62. [Google Scholar] [CrossRef] [PubMed]
- Filippatos, G.; Farmakis, D.; Parissis, J. Renal dysfunction and heart failure: Things are seldom what they seem. Eur. Heart J. 2014, 35, 416–418. [Google Scholar] [CrossRef]
- Singh, G.; Rachoin, J.S.; Chien, C.; Patel, S. The Use of Portal Vein Pulsatility to Differentiate Hypervolemic and Hypovolemic Hyponatremia. Case Rep. Crit. Care 2019, 2019, 9591823. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Signs/Symptoms | Scale |
|---|---|
| Dyspnea | 0 = None; 1 = Seldom; 2 = Frequent; 3 = Continuous |
| Ortopnea | 0 = None; 1 = Seldom; 2 = Frequent; 3 = Continuous |
| Jugular venous distention | 0 = ≤6; 1 = 6–9; 2 = 10–15; 3 = ≥ 15 |
| Rales | 0 = None; 1 = Bases; 2 = Up to < 50%; 3 ≥ 50% |
| Edema | 0 = Absent/trace; 1 = Slight; 2 = Moderate; 3 = Marked |
| Fatigue | 0 = None; 1 = Seldom; 2 = Frequent; 3 = Continuous |
| Baseline | Total (105 Patients) | Group 1 (54 Patients) | Group 2 (51 Patients) | p Value |
|---|---|---|---|---|
| Age, years, median (IQR) | 74 (66.5–82) | 72.5 (63–80) | 75 (68–84) | 0.17 |
| Sex, male (%) | 63 (60%) | 30 (56%) | 33 (65%) | 0.42 |
| HR, beats/min | 76 (70–100) | 77.5 (70–110) | 75 (65–100) | 0.18 |
| SBP, mmHg, median (IQR) | 130 (115–147) | 130 (115–150) | 130 (110–146) | 0.71 |
| IHD, (%) | 40 (38.1%) | 16 (29.63%) | 24 (47.06%) | 0.74 |
| HTN, (%) | 87 (82.86%) | 44 (81.48%) | 43 (84.31%) | 0.7 |
| DM (%) | 39 (37.14%) | 21 (38.89%) | 18 (35.29%) | 0.7 |
| AF (%) | 60 (57.14%) | 31 (57.41%) | 29 (48.33%) | 0.9 |
| LVEF (%) | 50 (35–60) | 50 (36–65) | 50 (34–60) | 0.95 |
| ACEi admission (%) | 34 (32%) | 22 (40%) | 12 (23%) | 0.06 |
| ARB admission (%) | 18 (17%) | 7 (12%) | 11 (21%) | 0.3 |
| ARNI admission (%) | 18 (17%) | 9 (16%) | 9 (17%) | 1 |
| Beta-blocker admission (%) | 88 (83%) | 50 (92%) | 38 (74%) | 0.01 |
| MRA admission (%) | 74 (70%) | 39 (72%) | 35 (68%) | 0.83 |
| SGLT2i admission (%) | 34 (32%) | 18 (17%) | 16 (15%) | 0.83 |
| Furosemide before admission (mg/day), median (IQR) | 20 (0–40) | 20 (0–35) | 20 (0–40) | 0.06 |
| Furosemide in hospital (mg/day), median (IQR) | 60 (40–80) | 60 (40–80) | 80 (40–80) | 0.02 |
| Parameters | Total (105 Patients) | Group 1 (54 Patients) | Group 2 (51 Patients) | p Value | Total (105 Patients) | Group 1 (54 Patients) | Group 2 (51 Patients) | p Value |
|---|---|---|---|---|---|---|---|---|
| Time | Admission | Discharge | ||||||
| EVEREST score, median | 12 (8–14) | 12 (8–14) | 11 (9–15) | 0.23 | 2 (2–3) | 2 (2–3) | 2 (2–4) | 0.50 |
| Weight (kg), mean | 84.47 (±18.16) | 83.63 (±17.5) | 84.25 (±19.29) | 0.87 | 82.41 (±17.33) | 81.83 (±16.86) | 83.06 (18.01) | 0.72 |
| GFR, (mL/min) | 54 (40.5–71) | 55 (45–71) | 52.5 (34–69) | 0.08 | 58.53(43.72–74.61) | 58.13 (43.14–67.16) | 61.84 (44.25–80.48) | 0.43 |
| NT-proBNP (pg/mL) | 4060 (1865–7085) | 4502 (2461–7085) | 3283 (1198–10839) | 0.27 | 1537 (926–2940) | 1476 (913–2741) | 1672 (1013–3912) | 0.44 |
| Na (mmol/L) | 138.86 (±3.73) | 139.46 (±3.82) | 138.28 (±3.56) | 0.14 | 135.76 (±15.14) | 138 (±3.33) | 132.58 (±23.08) | 0.03 |
| E/e’ median | 28.53 (20–37.12) | 27.45 (18.62–37.12) | 28.9 (23.87–38.66) | 0.41 | 14.82 (11.31–23.87) | 13.71 (10.22–18.25) | 20 (13.55–27) | 0.06 |
| TAPSE (mm) | 17 (14–19) | 17 (14–19) | 17 (14–18) | 0.78 | 17 (14–19) | 17 (14–20) | 16 (15–18) | 0.24 |
| IVC (mm) | 22 (19–24) | 21(19–23) | 22(18.5–25) | 0.08 | 17 (15–22) | 16 (15–19) | 20.5 (16–23) | 0.002 |
| PASP (mm Hg) | 50.89 (±14.57) | 49.73 (±14.63) | 52.18 (±14.54) | 0.39 | 38.16 (±12.49) | 33.43 (±9.72) | 45.11 (±12.98) | < 0.001 |
| TAPSE/PASP | 0.35 | 0.36 | 0.34 | 0.61 | 0.43 | 0.37 | 0.29 | 0.08 |
| Outcome | Total (105 Patients) | Group 1 (54 Patients) | Group 2 (51 Patients) | p Value |
|---|---|---|---|---|
| WRF | 58 (55.23%) | 26 (48.14%) | 32 (62.74%) | 0.17 |
| NT-proBNP drop > 30% | 69 (65.7%) | 42 (77%) | 27 (52.9%) | 0.01 |
| Rehospitalization % | 43 (40.95%) | 18 (33.33%) | 25 (49.01%) | 0.043 |
| Death, number, % | 16 (15.23%) | 2 (3.7%) | 14 (27.45%) | 0.0018 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grigore, M.; Grigore, A.-M.; Ilieșiu, A.-M. Portal Vein Pulsatility: A Valuable Approach for Monitoring Venous Congestion and Prognostic Evaluation in Acute Decompensated Heart Failure. Diagnostics 2024, 14, 2029. https://doi.org/10.3390/diagnostics14182029
Grigore M, Grigore A-M, Ilieșiu A-M. Portal Vein Pulsatility: A Valuable Approach for Monitoring Venous Congestion and Prognostic Evaluation in Acute Decompensated Heart Failure. Diagnostics. 2024; 14(18):2029. https://doi.org/10.3390/diagnostics14182029
Chicago/Turabian StyleGrigore, Mihai, Andreea-Maria Grigore, and Adriana-Mihaela Ilieșiu. 2024. "Portal Vein Pulsatility: A Valuable Approach for Monitoring Venous Congestion and Prognostic Evaluation in Acute Decompensated Heart Failure" Diagnostics 14, no. 18: 2029. https://doi.org/10.3390/diagnostics14182029
APA StyleGrigore, M., Grigore, A.-M., & Ilieșiu, A.-M. (2024). Portal Vein Pulsatility: A Valuable Approach for Monitoring Venous Congestion and Prognostic Evaluation in Acute Decompensated Heart Failure. Diagnostics, 14(18), 2029. https://doi.org/10.3390/diagnostics14182029








