One-Stage Soft Tissue Reconstruction Following Sarcoma Excision: A Personalized Multidisciplinary Approach Called “Orthoplasty”
Abstract
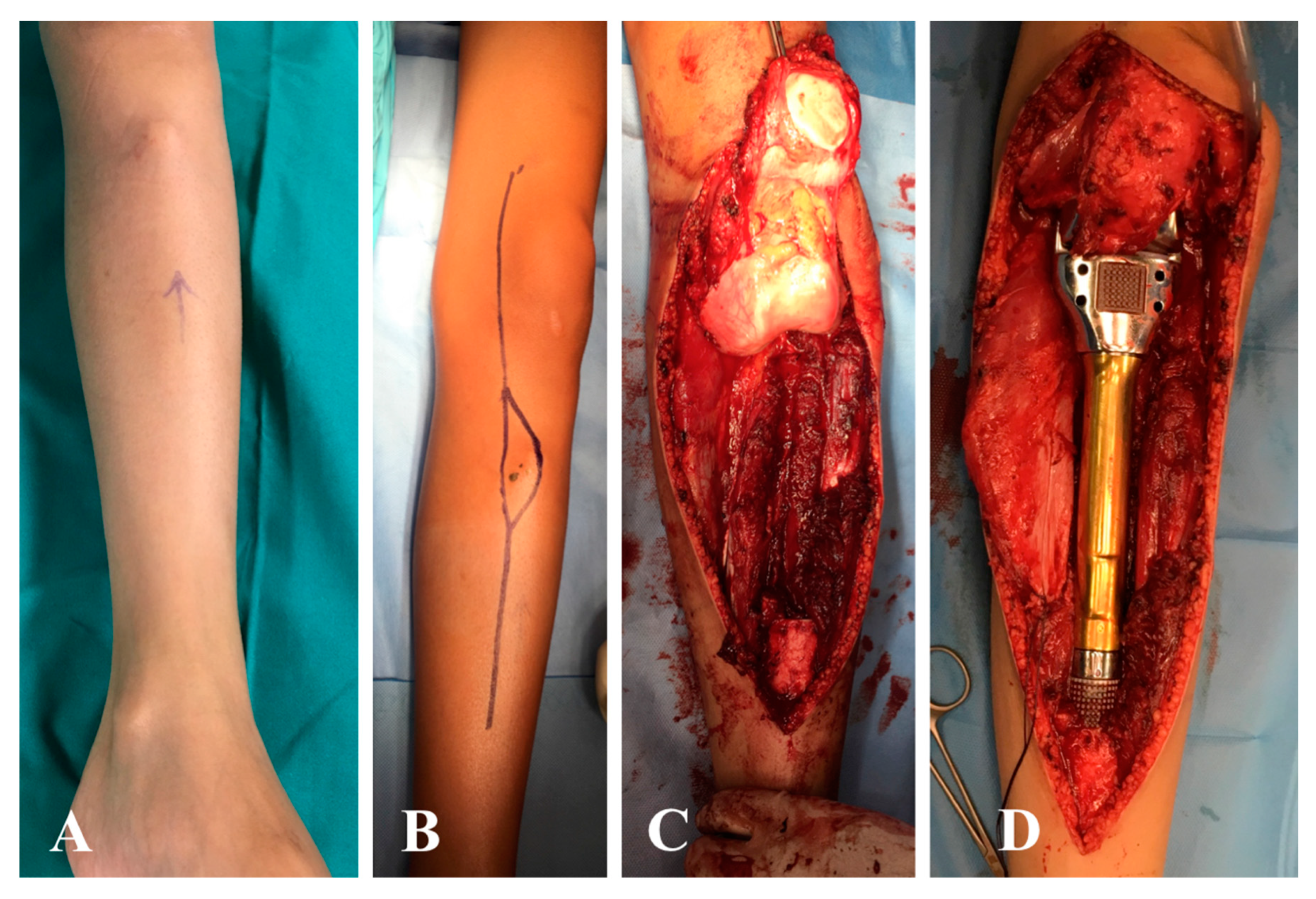
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Rosenberg, S.A.; Tepper, J.; Glatstein, E.; Costa, J.; Baker, A.; Brennan, M.; DeMoss, E.V.; Seipp, C.; Sindelar, W.F.; Sugarbaker, P.; et al. The treatment of soft-tissue sarcomas of the extremities: Prospective randomized evaluations of (1) limb-sparing surgery plus radiation therapy compared with amputation and (2) the role of adjuvant chemotherapy. Ann. Surg. 1982, 196, 305–315. [Google Scholar] [CrossRef]
- Pisters, P.W. Combined modality treatment of extremity soft tissue sarcomas. Ann. Surg. Oncol. 1998, 5, 464–472. [Google Scholar] [CrossRef]
- Agrawal, N.; Wan, D.; Bryan, Z.; Boehmler, J.; Miller, M.; Tiwari, P. Outcomes analysis of the role of plastic surgery in extremity sarcoma treatment. J. Reconstr. Microsurg. 2013, 29, 107–111. [Google Scholar] [CrossRef]
- Henderson, E.R.; Groundland, J.S.; Pala, E.; Dennis, J.A.; Wooten, R.; Cheong, D.; Windhager, R.; Kotz, R.I.; Mercuri, M.; Funovics, P.T.; et al. Failure mode classification for tumor endoprostheses: Retrospective review of five institutions and a literature review. J. Bone Joint Surg. Am. 2011, 93, 418–429. [Google Scholar] [CrossRef]
- Pala, E.; Trovarelli, G.; Angelini, A.; Maraldi, M.; Berizzi, A.; Ruggieri, P. Megaprosthesis of the knee in tumor and revision surgery. Acta Biomed. 2017, 88, 129–138. [Google Scholar] [CrossRef]
- Pala, E.; Trovarelli, G.; Calabrò, T.; Angelini, A.; Abati, C.N.; Ruggieri, P. Survival of Modern Knee Tumor Megaprostheses: Failures, Functional Results, and a Comparative Statistical Analysis. Clin. Orthop. Relat. Res. 2015, 473, 891–899. [Google Scholar] [CrossRef] [Green Version]
- Zagars, G.K.; Ballo, M.T.; Pisters, P.W.; Pollock, R.E.; Patel, S.R.; Benjamin, R.S.; Evans, H.L. Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: An analysis of 1225 patients. Cancer 2003, 97, 2530–2543. [Google Scholar] [CrossRef]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Enneking, W.F.; Dunham, W.; Gebhardt, M.C.; Malawar, M.; Pritchard, D.J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin. Orthop. Relat. Res. 1993, 286, 241–246. [Google Scholar] [CrossRef]
- Davis, A.M.; Wright, J.G.; Williams, J.I.; Bombardier, C.; Griffin, A.; Bell, R.S. Development of a measure of physical function for patients with bone and soft tissue sarcoma. Qual. Life Res. 1996, 5, 508–516. [Google Scholar] [CrossRef]
- Levin, L.S. The reconstructive ladder. An orthoplastic approach. Orthop. Clin. N. Am. 1993, 24, 393–409. [Google Scholar]
- Boriani, F.; Ul Haq, A.; Baldini, T.; Urso, R.; Granchi, D.; Baldini, N.; Tigani, D.; Tarar, M.; Khan, U. Orthoplastic surgical collaboration is required to optimise the treatment of severe limb injuries: A multi-centre, prospective cohort study. J. Plast. Reconstr. Aesthet. Surg. 2017, 70, 715–722. [Google Scholar] [CrossRef]
- Gans, I.; Baldwin, K.D.; Levin, L.S.; Nance, M.L.; Chang, B.; Kovach, S.J., 3rd; Serletti, J.M.; Flynn, J.M. A lower extremity musculo-skeletal and vascular trauma protocol in a children’s hospital may improve treatment response times and appropriate microvascular coverage. J. Orthop. Trauma 2015, 29, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Davidge, K.M.; Wunder, J.; Tomlinson, G.; Wong, R.; Lipa, J.; Davis, A.M. Function and health status outcomes following soft tissue reconstruction for limb preservation in extremity soft tissue sarcoma. Ann. Surg. Oncol. 2010, 17, 1052–1062. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Han, I.; Kim, S.; Lee, Y.H.; Kim, M.B.; Kim, H.S. Outcomes after flap reconstruction for extremity soft tissue sarcoma: A case-control study using propensity score analysis. Eur. J. Surg. Oncol. 2014, 40, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Subramanian, V.; Yousef, A.; Rogers, B.A.; Robb, G.L.; Chang, D.W. Upper extremity limb salvage with microvascular reconstruction in patients with advanced sarcoma. Plast. Reconstr. Surg. 2004, 114, 400–408. [Google Scholar] [CrossRef]
- Sanniec, K.J.; Velazco, C.S.; Bryant, L.A.; Zhang, N.; Casey, W.J., III; Mahabir, R.C.; Rebecca, A.M. Immediate versus Delayed Sarcoma Reconstruction: Impact on Outcomes. Sarcoma 2016, 2016, 7972318. [Google Scholar] [CrossRef] [Green Version]
- Slump, J.; Ferguson, P.C.; Wunder, J.S.; Griffin, A.M.; Hoekstra, H.J.; Liu, X.; Hofer, S.O.P.; O’Neill, A.C. Patient, tumour and treatment factors affect complication rates in soft tissue sarcoma flap reconstruction in a synergistic manner. Eur. J. Surg. Oncol. 2017, 43, 1126–1133. [Google Scholar] [CrossRef]
- Suh, H.S.; Lee, J.S.; Hong, J.P. Consideration in lower extremity reconstruction following oncologic surgery: Patient selection, surgical techniques, and outcomes. J. Surg. Oncol. 2016, 113, 955–961. [Google Scholar] [CrossRef]
- Beane, J.D.; Yang, J.C.; White, D.; Steinberg, S.M.; Rosenberg, S.A.; Rudloff, U. Efficacy of adjuvant radiation therapy in the treatment of soft tissue sarcoma of the extremity: 20-year follow-up of a randomized prospective trial. Ann. Surg. Oncol. 2014, 21, 2484–2489. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Papagelopoulos, P.J.; Romantini, M.; Angelini, A.; Ruggieri, P. Side effects of chemotherapy in musculoskeletal oncology. J. Long-Term Eff. Med. Implant. 2010, 20, 1–12. [Google Scholar] [CrossRef]
- Schwartz, D.L.; Einck, J.; Hunt, K.; Bruckner, J.; Conrad, E.; Koh, W.J.; Laramore, G.E. The effect of delayed postoperative irradiation on local control of soft tissue sarcomas of the extremity and torso. Int. J. Radiat. Oncol. Biol. Phys. 2002, 52, 1352–1359. [Google Scholar] [CrossRef]
- Davis, L.E.; Ryan, C.W. Preoperative therapy for extremity soft tissue sarcomas. Curr. Treat. Options Oncol. 2015, 16, 25. [Google Scholar] [CrossRef] [PubMed]
- Siegel, G.W.; Kuzon, W.M.; Hasen, J.M.; Biermann, J.S. Staged soft tissue reconstruction following sarcoma excision with anticipated large cutaneous defects: An oncologically safe alternative. IOWA Orthop. 2016, 36, 104–108. [Google Scholar]
- O’Sullivan, B.; Bell, R.; Catton, C.; Chabot, P.; Wunder, J.; Kandel, R.; Goddard, K.; Sadura, A.; Pater, J.; Zee, B. Preoperative versus post-operative radiotherapy in soft-tissue sarcoma of the limbs: A randomised trial. Lancet 2002, 359, 2235–2241. [Google Scholar] [CrossRef]
- Cannon, C.P.; Ballo, M.T.; Zagars, G.K.; Mirza, A.N.; Lin, P.P.; Lewis, V.O.; Yasko, A.W.; Benjamin, R.S.; Pisters, P.W. Complications of combined modality treatment of primary lower extremity soft-tissue sarcomas. Cancer 2006, 107, 2455–2461. [Google Scholar] [CrossRef]
- Peat, B.G.; Bell, R.S.; Davis, A.; O’Sullivan, B.; Mahoney, J.; Manktelow, R.T.; Bowen, V.; Catton, C.; Fornasier, V.L.; Langer, F. Wound-healing complications after soft-tissue sarcoma surgery. Plast. Reconstr. Surg. 1994, 93, 980–987. [Google Scholar] [CrossRef]
- Barwick, W.J.; Goldberg, J.A.; Scully, S.P.; Harrelson, J.M. Vascularized tissue transfer for closure of irradiated wounds after soft tissue sarcoma resection. Ann. Surg. 1992, 216, 591–595. [Google Scholar] [CrossRef]
- Temple, C.L.; Ross, D.C.; Magi, E.; DiFrancesco, L.M.; Kurien, E.; Temple, W.J. Preoperative chemoradiation and flap reconstruction provide high local control and low wound complication rates for patients undergoing limb salvage surgery for upper extremity tumors. J. Surg. Oncol. 2007, 95, 135–141. [Google Scholar] [CrossRef]
- Shaw, A.S.; Williams, M.V. The cancer reform strategy. Clin. Radiol. 2008, 63, 1292–1296. [Google Scholar] [CrossRef]
- Mavrogenis, A.F.; Angelini, A.; Pala, E.; Sakellariou, V.I.; Ruggieri, P.; Papagelopoulos, P.J. Reconstruction of the extensor mechanism after major knee resection. Orthopedics 2012, 35, e672–e680. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mavrogenis, A.F.; Pala, E.; Angelini, A.; Ferraro, A.; Ruggieri, P. Proximal tibial resections and reconstructions: Clinical outcome of 225 patients. J. Surg. Oncol. 2013, 107, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Angelini, A.; Trovarelli, G.; Berizzi, A.; Pala, E.; Breda, A.; Ruggieri, P. Three-dimension-printed custom-made prosthetic reconstructions: From revision surgery to oncologic reconstructions. Int. Orthop. 2019, 43, 123–132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Angelini, A.; Kotrych, D.; Trovarelli, G.; Szafrański, A.; Bohatyrewicz, A.; Ruggieri, P. Analysis of principles inspiring design of three-dimensional-printed custom-made prostheses in two referral centres. Int. Orthop. 2020. [Google Scholar] [CrossRef]
- Sun, W.; Li, J.; Li, Q.; Li, G.; Cai, Z. Clinical effectiveness of hemipelvic reconstruction using computer-aided custom-made prostheses after resection of malignant pelvic tumors. J. Arthroplasty. 2011, 26, 1508–1513. [Google Scholar] [CrossRef]
- Wang, B.; Hao, Y.; Pu, F.; Jiang, W.; Shao, Z. Computer-aided designed, three dimensional-printed hemipelvic prosthesis for peri-acetabularmalignant bone tumour. Int. Orthop. 2018, 42, 687–694. [Google Scholar] [CrossRef]
- Angelini, A.; Drago, G.; Trovarelli, G.; Calabrò, T.; Ruggieri, P. Infection after surgical resection for pelvic bone tumors: An analysis of 270 patients from one institution. Clin. Orthop. Relat. Res. 2014, 472, 349–359. [Google Scholar] [CrossRef] [Green Version]
- Lohman, R.F.; Nabawi, A.S.; Reece, G.P.; Pollock, R.E.; Evans, G.R. Soft tissue sarcoma of the upper extremity: A 5-year experience at two institutions emphasizing the role of soft tissue flap reconstruction. Cancer 2002, 94, 2256–2264. [Google Scholar] [CrossRef]
- Boyce, D.E.; Shokrollahi, K. Reconstructive surgery. BMJ 2006, 332, 710–712. [Google Scholar] [CrossRef] [Green Version]
- Engel, H.; Lin, C.H.; Wei, F.C. Role of microsurgery in lower extremity reconstruction. Plast. Reconstr. Surg. 2011, 127 (Suppl. 1), 228S–238S. [Google Scholar] [CrossRef]
- Turner, A.J.; Parkhouse, N. Revisiting the reconstructive ladder. Plast. Reconstr. Surg. 2006, 118, 267–268. [Google Scholar] [CrossRef] [PubMed]
- Tschoi, M.; Hoy, E.A.; Granick, M.S. Skin flaps. Clin. Plast. Surg. 2005, 32, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Roehl, K.R.; Mahabir, R.C. A practical guide to free tissue transfer. Plast. Reconstr. Surg. 2013, 132, 147e–158e. [Google Scholar] [CrossRef] [PubMed]
- Emory, C.L.; Montgomery, C.O.; Potter, B.K.; Keisch, M.E.; Conway, S.A. Early complications of high-dose- rate brachytherapy in soft tissue sarcoma: A comparison with traditional external-beam radiotherapy. Clin. Orthop. Relat. Res. 2012, 470, 751–758. [Google Scholar] [CrossRef] [Green Version]
- Hallock, G.G. A paradigm shift in flap selection protocols for zones of the lower extremity using perforator flaps. J. Reconstr. Microsurg. 2013, 29, 233–240. [Google Scholar] [CrossRef]
- Lawrenz, J.M.; Mesko, N.W.; Marshall, D.C.; Featherall, J.; George, J.; Gordon, J.; Vijayasekaran, A.; Nystrom, L.M.; Schwarz, G.S. Immediate Versus Staged Soft Tissue Reconstruction After Soft Tissue Sarcoma Resection Has Similar Wound and Oncologic Outcomes. Ann. Plast. Surg. 2020. [Google Scholar] [CrossRef]
- Bickels, J.; Kollender, Y.; Wittig, J.C.; Cohen, N.; Malawer, M.M. Vacuum-assisted wound closure after resection of musculoskeletal tumors. Clin. Orthop. Relat. Res. 2005, 441, 346–350. [Google Scholar] [CrossRef]
- McGough, R.L., III. The BrachyVAC: A new method for managing sarcomas requiring soft tissue reconstruction. Oper. Tech. Orthop. 2014, 24, 68–73. [Google Scholar] [CrossRef]
- Sanniec, K.J.; Swanson, S.; Casey, W.J., 3rd; Schwartz, A.; Bryant, L.; Rebecca, A.M. Predictive factors of wound complications after sarcoma resection requiring plastic surgeon involvement. Ann. Plast. Surg. 2013, 71, 283–285. [Google Scholar] [CrossRef]
- Nakamura, T.; Matsumine, A.; Matsubara, T.; Asanuma, K.; Uchida, A.; Sudo, A. Clinical characteristics of patients with large and deep soft tissue sarcomas. Oncol. Lett. 2015, 10, 841–844. [Google Scholar] [CrossRef] [Green Version]
- Saddegh, M.K.; Bauer, H.C. Wound complication in surgery of soft tissue sarcoma. Analysis of 103 consecutive patients managed without adjuvant therapy. Clin. Orthop. Relat. Res. 1993, 289, 247–253. [Google Scholar]
- Geller, D.S.; Hornicek, F.J.; Mankin, H.J.; Raskin, K.A. Soft tissue sarcoma resection volume associated with wound-healing complications. Clin. Orthop. 2007, 459, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration, HHS. Medical devices; general and plastic surgery devices; classification of non-powered suction apparatus device intended for negative pressure wound therapy. Final Rule Fed. Regist. 2010, 75, 70112–70114. [Google Scholar]
- Heller, L.; Kronowitz, S.J. Lower extremity reconstruction. J. Surg. Oncol. 2006, 94, 479–489. [Google Scholar] [CrossRef] [PubMed]






| Data | Patients | % | Age < 18 | Age > 18 |
|---|---|---|---|---|
| Age and gender | ||||
| Age (mean years) | 56 (range, 6–76) | |||
| Age < 18 years | ||||
| Gender (male/female) | 86/75 | |||
| Pathological diagnosis | ||||
| Soft tissue sarcomas | 136 | 84.5% | 14 | 122 |
| Bone tumors | 25 | 15.5% | 3 | 22 |
| Pre-surgical status | ||||
| Primarily treated | 120 | 74.5% | 16 | 104 |
| Referral after unplanned excision | 24 | 14.9% | 1 | 23 |
| Referral due to local recurrence | 17 | 10.6% | - | 17 |
| Comorbidities | ||||
| Hypertension | 62 | 38.5% | - | 62 |
| Cardiovascular disease or congestive heart failure | 31 | 19.3% | - | 31 |
| Diabetes | 23 | 14.3% | 2 | 21 |
| Cerebrovascular disease | 13 | 8.1% | - | 13 |
| Thyroid disease | 11 | 6.8% | 1 | 10 |
| Chronic obstructive pulmonary disease | 8 | 5.0% | - | 8 |
| Vascular disease | 6 | 3.7% | - | 6 |
| Other less representative diseases | 14 | 8.7% | 3 | 11 |
| Data | Patients | % | Age < 18 | Age > 18 |
|---|---|---|---|---|
| Soft tissue sarcoma (STS) | 136/161 | 84.5% | ||
| - Further treatments in pts with personal history of STS | 34/161 | 21.1% | 1 | 33 |
| - Head, face and neck | 28/161 | 17.4% | 2 | 26 |
| - Lower limb, including hip | 21/161 | 13.0% | 6 | 15 |
| - Upper limb, including shoulder | 18/161 | 11.2% | 4 | 14 |
| - Trunk | 6/161 | 3.7% | - | 6 |
| - Thorax | 6/161 | 3.7% | 1 | 5 |
| - Abdomen | 5/161 | 8.1% | - | 5 |
| - Pelvis | 3/161 | 1.8% | - | 3 |
| - Kaposi’s sarcoma | 5/161 | 8.1% | - | 5 |
| - Other body area | 10/161 | 6.2% | - | 10 |
| Bone tumors | 25/161 | 15.5% | ||
| - Further treatment in pts with personal history of bone tumors | 7/161 | 4.3% | 1 | 6 |
| - Lower limb | 3/161 | 1.8% | 2 | 1 |
| - Rib, sternum and clavicle | 3/161 | 1.8% | - | 3 |
| - Mandible | 6/161 | 3.7% | - | 6 |
| - Bone metastasis from carcinoma | 6/161 | 3.7% | - | 6 |
| Data | Patients | % | Age < 18 | Age > 18 |
|---|---|---|---|---|
| Flaps | 54/161 | 33.5% | ||
| - Pedicled flaps | 31/54 | 57.4% | ||
| Gastrocnemius | 3 | 5.6% | 2 | 1 |
| Latissimus dorsi | 7 | 13.0% | - | 7 |
| Radial forearm | 4 | 7.4% | 3 | |
| Anterolateral thigh | 2 | 3.7% | 1 | 2 |
| Rectus abdominus | 4 | 7.4% | - | 4 |
| Cutaneous perforator propeller | 2 | 3.7% | - | 1 |
| Gluteus maximus | 2 | 3.7% | 1 | 2 |
| Soleus | 2 | 3.7% | - | 2 |
| Tensor fascia lata | 3 | 5.6% | - | 3 |
| Pectoralis | 1 | 1.8% | - | 1 |
| Gracilis | 1 | 1.8% | - | 1 |
| - Microvascular free flaps | 23/54 | 42.6% | - | |
| Anterolateral thigh | 12 | 23.5% | 9 | |
| Latissimus dorsi | 7 | 13.0% | 3 | 7 |
| Radial forearm | 2 | 3.7% | - | 2 |
| Gracilis | 2 | 3.7% | - | 2 |
| Skin grafts | 42/161 | 26.1% | - | 38 |
| Wide surgical excision | 40/161 | 24.8% | 4 | 35 |
| Dermal substitute | 9/161 | 5.6% | 5 | 9 |
| Incisional biopsy in previous flaps | 7/161 | 4.3% | - | 7 |
| Allogenic skin grafts | 7/161 | 4.3% | - | 6 |
| Synthetic mesh prosthesis | 1/161 | 1.7% | 1 | 1 |
| Amputation | 1/161 | 1.7% | - | 1 |
| Data | Patients | % |
|---|---|---|
| Grade I | 48 | 77.4% |
| Including wound dehiscence, delayed wound healing, superficial infection, hematoma | ||
| Grade II | 8 | 12.9% |
| Including infection needing antibiotic administration, wound dehiscence, partial necrosis, medical aspects (anemia, deep vein thrombosis, urinary tract infection) | ||
| Grade III | 5 | 8.1% |
| Including deep infection, complete wound dehiscence, hematoma, partial or total flap loss | ||
| Grade IV | 1 | 1.6% |
| Including myocardial infarction, systemic sepsis | ||
| Grade V | - | -% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Angelini, A.; Tiengo, C.; Sonda, R.; Berizzi, A.; Bassetto, F.; Ruggieri, P. One-Stage Soft Tissue Reconstruction Following Sarcoma Excision: A Personalized Multidisciplinary Approach Called “Orthoplasty”. J. Pers. Med. 2020, 10, 278. https://doi.org/10.3390/jpm10040278
Angelini A, Tiengo C, Sonda R, Berizzi A, Bassetto F, Ruggieri P. One-Stage Soft Tissue Reconstruction Following Sarcoma Excision: A Personalized Multidisciplinary Approach Called “Orthoplasty”. Journal of Personalized Medicine. 2020; 10(4):278. https://doi.org/10.3390/jpm10040278
Chicago/Turabian StyleAngelini, Andrea, Cesare Tiengo, Regina Sonda, Antonio Berizzi, Franco Bassetto, and Pietro Ruggieri. 2020. "One-Stage Soft Tissue Reconstruction Following Sarcoma Excision: A Personalized Multidisciplinary Approach Called “Orthoplasty”" Journal of Personalized Medicine 10, no. 4: 278. https://doi.org/10.3390/jpm10040278
APA StyleAngelini, A., Tiengo, C., Sonda, R., Berizzi, A., Bassetto, F., & Ruggieri, P. (2020). One-Stage Soft Tissue Reconstruction Following Sarcoma Excision: A Personalized Multidisciplinary Approach Called “Orthoplasty”. Journal of Personalized Medicine, 10(4), 278. https://doi.org/10.3390/jpm10040278








