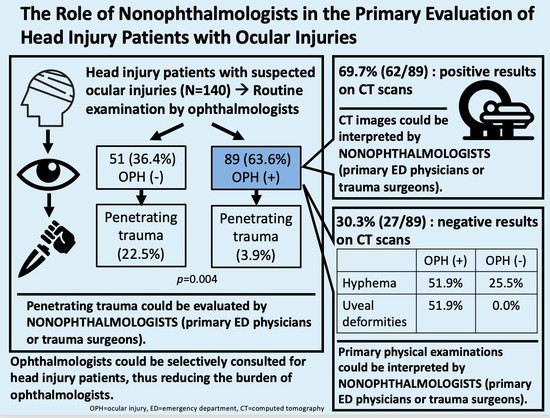
The Role of Nonophthalmologists in the Primary Evaluation of Head Injury Patients with Ocular Injuries
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Setting
2.2. Definitions
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sen, N. An insight into the vision impairment following traumatic brain injury. Neurochem. Int. 2017, 111, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, A.L.; MacGregor, A.J.; Han, P.P.; Heltemes, K.J.; Galarneau, M.R. Visual dysfunction following blast-related traumatic brain injury from the battlefield. Brain Inj. 2011, 25, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Heng, L.Z.; Hamilton, R.D. Ocular emergencies. Medicine 2018, 46, 754–759. [Google Scholar] [CrossRef]
- Merezhinskaya, N.; Mallia, R.K.; Park, D.; Bryden, D.W.; Mathur, K.; Barker, F.M.I. Visual deficits and dysfunctions associated with traumatic brain injury: A systematic review and meta-analysis. Optom. Vis. Sci. 2019, 96, 542–555. [Google Scholar] [CrossRef] [PubMed]
- Marano, R.; Lino, P.R.S.; Zanetti, F.; Tincani, A.J.; Oliveira, L. Is specialized ophthalmologic evaluation necessary after orbital fractures? A prospective 64-case study. Oral Maxillofac. Surg. 2019, 23, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Cook, T. Ocular and periocular injuries from orbital fractures. J. Am. Coll. Surg. 2002, 195, 831–834. [Google Scholar] [CrossRef]
- American College of Surgeons, Committee on Trauma. Advanced Trauma Life Support, 10th ed.; American College of Surgeons: Chicago, IL, USA, 2018. [Google Scholar]
- Kuhn, F.; Maisiak, R.; Mann, L.; Mester, V.; Morris, R.; Witherspoon, C.D. The ocular trauma score (OTS). Ophthalmol. Clin. N. Am. 2002, 15, 163–165. [Google Scholar] [CrossRef]
- Odebode, T.O.; Ademola-Popoola, D.S.; Ojo, T.A.; Ayanniyi, A.A. Ocular and visual complications of head injury. Eye 2005, 19, 561–566. [Google Scholar] [CrossRef] [PubMed]
- Al-Thowaibi, A.; Kumar, M.; Al-Matani, I. An overview of penetrating ocular trauma with retained intraocular foreign body. Saudi J. Ophthalmol. 2011, 25, 203–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loporchio, D.; Mukkamala, L.; Gorukanti, K.; Zarbin, M.; Langer, P.; Bhagat, N. Intraocular foreign bodies: A review. Surv. Ophthalmol. 2016, 61, 582–596. [Google Scholar] [CrossRef] [PubMed]
- Rossi, T.; Boccassini, B.; Iossa, M.; Mutolo, M.; Lesnoni, G.; Mutolo, P.A. Triaging and coding ophthalmic emergency—The rome eye scoring system for urgency and emergency (RESCUE): A pilot study of 1000 eye-dedicated emergency room patients. Eur. J. Ophthalmol. 2007, 17, 413–417. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Administration Ministry of Health and Welfare—Copayments. Available online: https://www.nhi.gov.tw/english/Content_List.aspx?n=E5509C8FE29950EA&topn=1D1ECC54F86E9050 (accessed on 1 November 2021).
- Juang, P.S.C.; Rosen, P. Ocular examination techniques for the emergency department. J. Emerg. Med. 1997, 15, 793–810. [Google Scholar] [CrossRef]
- Dhaliwal, A.; West, A.L.; Trobe, J.D.; Musch, D.C. Third, fourth, and sixth cranial nerve palsies following closed head injury. J. Neuroophthalmol. 2006, 26, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Margolin, E.; Lam, C.T.Y. Approach to a patient with diplopia in the emergency department. J. Emerg. Med. 2018, 54, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.Y.; Ngai, P.; Echegoyen, J.C.; Tao, J.P. Imaging in orbital trauma. Saudi J. Ophthalmol. 2012, 26, 427–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kisilevsky, E.; Kaplan, A.; Micieli, J.; McGowan, M.; Mackinnon, D.; Margolin, E. Computed tomography only useful for selected patients presenting with primary eye complaints in the emergency department. Am. J. Emerg. Med. 2018, 36, 162–164. [Google Scholar] [CrossRef] [PubMed]
- Joseph, D.P.; Pieramici, D.J.; Beauchamp, N.J., Jr. Computed tomography in the diagnosis and prognosis of open-globe injuries. Ophthalmology 2000, 107, 1899–1906. [Google Scholar] [CrossRef]
- Kubal, W.S. Imaging of orbital trauma. RadioGraphics 2008, 28, 1729–1739. [Google Scholar] [CrossRef] [PubMed]


| Ocular Lesion (+) (N = 89) | Ocular Lesion (−) (N = 51) | p-Value | |
|---|---|---|---|
| Age (years) | 45 (27) | 50 (36) | 0.170 * |
| Sex (N, %) | 0.611 † | ||
| Male | 63 (70.8%) | 34 (66.7%) | |
| Female | 26 (29.2%) | 17 (33.3%) | |
| Laterality (N, %) | 0.537 † | ||
| OD | 34 (38.2%) | 23 (45.1%) | |
| OS | 47 (52.8%) | 22 (43.1%) | |
| OU | 8 (9.0%) | 6 (11.8%) | |
| Trauma mechanism (N, %) | 0.004 † | ||
| Penetrating | 20 (22.5%) | 2 (3.9%) | |
| Blunt | 69 (77.5%) | 49 (96.1%) | |
| Associated symptoms (N, %) | |||
| Initial loss of consciousness | 26 (29.2%) | 12 (23.5%) | 0.467 † |
| Altered mental status | 4 (4.5%) | 4 (7.8%) | 0.411 † |
| Posttraumatic amnesia | 14 (15.7%) | 10 (19.6%) | 0.558 † |
| Dizziness | 6 (6.7%) | 5 (9.8%) | 0.517 † |
| Nausea | 5 (5.6%) | 2 (3.9%) | 0.658 † |
| Vomiting | 5 (5.6%) | 0 (0.0%) | 0.085 † |
| Headache | 6 (6.7%) | 4 (7.8%) | 0.808 † |
| Facial wounds | 41 (46.1%) | 22 (43.1%) | 0.737 † |
| Primary Eye Examination in the Emergency Department | Ocular Lesion (+) (N = 69, 58.5%) | Ocular Lesion (−) (N = 49, 41.5%) | p-Value † |
|---|---|---|---|
| Visual loss | 4 (5.8%) | 1 (2.0%) | 0.318 |
| Blurred vision | 37 (53.6%) | 26 (53.1%) | 0.952 |
| Diplopia | 18 (26.1%) | 4 (8.2%) | 0.014 |
| Extraocular movement limitation | 19 (27.5%) | 7 (14.3%) | 0.087 |
| Relative afferent pupillary defect | 7 (10.1%) | 3 (6.1%) | 0.439 |
| Periorbital swelling | 62 (89.9%) | 33 (67.3%) | 0.002 |
| Lid laceration | 18 (26.1%) | 10 (20.4%) | 0.475 |
| Hyphema | 19 (27.5%) | 13 (26.5%) | 0.904 |
| Uveal deformities | 4 (5.8%) | 0 (0.0%) | 0.086 |
| Ocular Lesion (+) (N = 27) | Ocular Lesion (−) (N = 51) | p-Value | |
|---|---|---|---|
| Age (years) | 52 (15) | 50 (36) | 0.950 * |
| Sex (N, %) | 0.011 † | ||
| Male | 25 (92.6%) | 34 (66.7%) | |
| Female | 2 (7.4%) | 17 (33.3%) | |
| Laterality (N, %) | 0.196 † | ||
| OD | 9 (33.3%) | 23 (45.1%) | |
| OS | 17 (63.0%) | 22 (43.1%) | |
| OU | 1 (3.7%) | 6 (11.8%) | |
| Type of injury (N, %) | <0.001 † | ||
| Penetrating | 19 (70.4%) | 2 (3.9%) | |
| Blunt | 8 (29.6%) | 49 (96.1%) | |
| Associated symptoms (N, %) | |||
| Initial loss of consciousness | 1 (3.7%) | 12 (23.5%) | 0.055 † |
| Altered mental status | 0 (0.0%) | 4 (7.8%) | 0.340 † |
| Posttraumatic amnesia | 1 (3.7%) | 10 (19.6%) | 0.115 † |
| Dizziness | 0 (0.0%) | 5 (9.8%) | 0.232 † |
| Nausea | 0 (0.0%) | 2 (3.9%) | 0.772 † |
| Headache | 1 (3.7%) | 4 (7.8%) | 0.823 † |
| Facial wounds | 5 (18.5%) | 22 (43.1%) | 0.054 † |
| Visual loss | 2 (7.4%) | 1 (2.0%) | 0.568 † |
| Blurred vision | 21 (77.8%) | 27 (52.9%) | 0.057 † |
| Diplopia | 0 (0.0%) | 4 (7.8%) | 0.340 † |
| Extraocular movement limitation | 1 (3.7%) | 7 (13.7%) | 0.319 † |
| Relative afferent pupillary defect | 0 (0.0%) | 3 (5.9%) | 0.505 † |
| Lid laceration | 7 (25.9%) | 10 (19.6%) | 0.723 † |
| Hyphema | 14 (51.9%) | 13 (25.5%) | 0.038 † |
| Uveal deformities | 14 (51.9%) | 0 (0.0%) | <0.001 † |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-H.; Ling, X.C.; Wu, W.-C.; Chen, K.-J.; Hsieh, C.-H.; Liao, C.-H.; Fu, C.-Y. The Role of Nonophthalmologists in the Primary Evaluation of Head Injury Patients with Ocular Injuries. J. Pers. Med. 2021, 11, 1220. https://doi.org/10.3390/jpm11111220
Lin C-H, Ling XC, Wu W-C, Chen K-J, Hsieh C-H, Liao C-H, Fu C-Y. The Role of Nonophthalmologists in the Primary Evaluation of Head Injury Patients with Ocular Injuries. Journal of Personalized Medicine. 2021; 11(11):1220. https://doi.org/10.3390/jpm11111220
Chicago/Turabian StyleLin, Chen-Hua, Xiao Chun Ling, Wei-Chi Wu, Kuan-Jen Chen, Chi-Hsun Hsieh, Chien-Hung Liao, and Chih-Yuan Fu. 2021. "The Role of Nonophthalmologists in the Primary Evaluation of Head Injury Patients with Ocular Injuries" Journal of Personalized Medicine 11, no. 11: 1220. https://doi.org/10.3390/jpm11111220