Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge
Abstract
:1. Introduction
2. Methods
3. Prevalence
4. Demography
4.1. Gender
4.2. Age
5. Tooth and Root Distribution of VRF
6. Diagnostic Methods
6.1. Coronally Positioned Sinus Tract
6.2. Biting Pain and Bite Test
6.3. Deep Periodontal Probing Depth
6.4. Pulp Vitality Test
6.5. Magnification
6.6. Radiographic Assessment
6.7. Exploratory Surgery
7. Etiology and Predisposing Factors
7.1. Iatrogenic Factors
7.1.1. Excessive Tooth Structure Removal or Over-Preparation during Root Canal Instrumentation
7.1.2. Excessive Force during Root Canal Obturation
7.1.3. Excessive Post Space Preparation
7.2. Predisposing Factors
7.2.1. Loss of Remaining or Internal Tooth Structure
7.2.2. Specific Anatomies of the Susceptible Roots
7.2.3. Age-Related Microstructural Changes
7.2.4. Implant-Related VRFs
7.2.5. Repetitive Heavy and Stressful Chewing Habits
8. Clinical Features
8.1. Pain
8.2. Soft Tissue Swelling and Sinus Tract
8.3. Deep Periodontal Probing Depth
8.4. Attrited Occlusal Surface
8.5. Other Clinical Symptoms and Signs
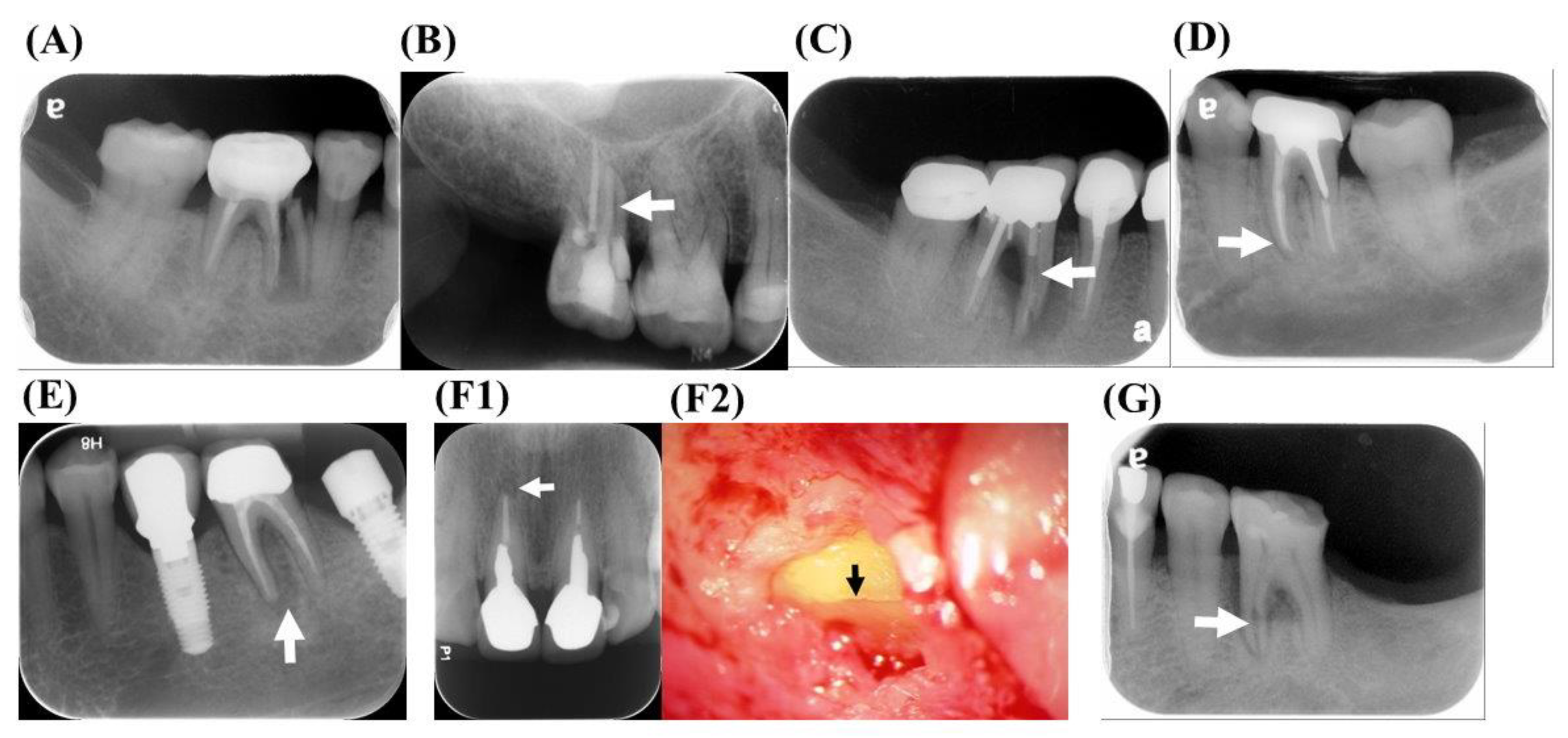
9. Radiographic Characteristics
9.1. Displacement of Fractured Fragment
9.2. Radiolucent Line within the Root Canal
9.3. Unusual Space between the Canal Wall and Intracanal Material
9.4. Widening PDL Space
9.5. Periradicular Radiolucent Halo
9.6. Angular Bony Destruction
9.7. Step-Like Bone Defect
9.8. V-Shaped Diffuse Bone Defect
9.9. Root Resorption Correspond to the Fracture Line (Figure 5F1,F2)
9.10. Widening of the Root Canal Space (Figure 5G)
9.11. Endodontic Failure after Healing has Occurred
9.12. No Evident Radiographic Finding
10. Treatment and Prevention of VRFs
11. Conclusions
Author Contributions
Funding
Institutional Review Board
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kumar, A.P.; Shemesh, H.; Jothilatha, S.; Vijayabharathi, R.; Jayalakshmi, S.; Kishen, A. Diagnosis of vertical root fractures in restored endodontically treated teeth: A time-dependent retrospective cohort study. J. Endod. 2016, 42, 1175–1180. [Google Scholar]
- Yang, S.F.; Rivera, E.M.; Walton, R.E. Vertical root fracture in nonendodontically treated teeth. J. Endod. 1995, 21, 337–339. [Google Scholar] [CrossRef]
- Yeh, C.J. Fatigue root fracture: A spontaneous root fracture in non-endodontically treated teeth. Br. Dent. J. 1997, 182, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.P.; Lin, C.P.; Tseng, S.C.; Jeng, J.H. Vertical root fracture in endodontically versus nonendodontically treated teeth: A survey of 315 cases in Chinese patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1999, 87, 504–507. [Google Scholar] [CrossRef]
- Yoshino, K.; Ito, K.; Kuroda, M.; Sugihara, N. Prevalence of vertical root fracture as the reason for tooth extraction in dental clinics. Clin. Oral Investig. 2015, 19, 1405–1409. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Berman, L.H.; Blanco, L.; Bakland, L.; Kim, J.S. A demographic analysis of vertical root fractures. J. Endod. 2006, 32, 1160–1163. [Google Scholar] [CrossRef] [PubMed]
- Morfis, A.S. Vertical root fractures. Oral Surg. Oral Med. Oral Pathol. 1990, 69, 631–635. [Google Scholar] [CrossRef]
- Vire, D.E. Failure of endodontically treated teeth: Classification and evaluation. J. Endod. 1991, 17, 338–342. [Google Scholar] [CrossRef]
- Touré, B.; Faye, B.; Kane, A.W.; Lo, C.M.; Niang, B.; Boucher, Y. Analysis of reasons for extraction of endodontically treated teeth: A prospective study. J. Endod. 2011, 37, 1512–1515. [Google Scholar] [CrossRef]
- Fuss, Z.; Lustig, J.; Tamse, A. Prevalence of vertical root fractures in extracted endodontically treated teeth. Int. Endod. J. 1999, 32, 283–286. [Google Scholar] [CrossRef]
- See, W.K.; Ho, J.C.; Huang, C.F.; Hung, W.C.; Chang, C.W. The association between clinical diagnostic factors and the prevalence of vertical root fracture in endodontic surgery. J. Formos. Med. Assoc. 2019, 118, 713–720. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.M.; Wölner-Hanssen, A.B.; Sendi, P.; Von Arx, T. Comparison of intraoral radiography and limited cone beam computed tomography for the assessment of root-fractured permanent teeth. Dent. Traumatol. 2009, 25, 571–577. [Google Scholar] [CrossRef] [PubMed]
- Meister, F., Jr.; Lommel, T.J.; Gerstein, H. Diagnosis and possible causes of vertical root fractures. Oral Surg. Oral Med. Oral Pathol. 1980, 49, 243–253. [Google Scholar] [CrossRef]
- Testori, T.; Badino, M.; Castagnola, M. Vertical root fractures in endodontically treated teeth: A clinical survey of 36 cases. J. Endod. 1993, 19, 87–90. [Google Scholar] [CrossRef]
- Torbjörner, A.; Karlsson, S.; Odman, P.A. Survival rate and failure characteristics for two post designs. J. Prosthet. Dent. 1995, 73, 439–444. [Google Scholar] [CrossRef]
- Hansen, E.K.; Asmussen, E.; Christiansen, N.C. In vivo fractures of endodontically treated posterior teeth restored with amalgam. Dent. Traumatol. 1990, 6, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Weine, F.S.; Wax, A.H.; Wenckus, C.S. Retrospective study of tapered, smooth post systems in place for 10 years or more. J. Endod. 1991, 17, 293–297. [Google Scholar] [CrossRef]
- Sugaya, T.; Nakatsuka, M.; Inoue, K.; Tanaka, S.; Miyaji, H.; Sakagami, R.; Kawamami, M. Comparison of fracture sites and post lengths in longitudinal root fractures. J. Endod. 2015, 41, 159–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, C.P.; Tseng, S.C.; Lin, C.P.; Huang, C.C.; Tsai, T.P.; Chen, C.C. Vertical root fracture in nonendontically treated teeth-a clinical report of 64 cases in Chinese patients. J. Endod. 1998, 24, 678–681. [Google Scholar] [CrossRef]
- Wei, P.; Ju, Y. Vertical root fracture-case report and clinical evaluation. Changgeng Yi Xue Za Zhi 1989, 12, 237–243. [Google Scholar]
- Gher, M.E., Jr.; Dunlap, R.M.; Anderson, M.H.; Kuhl, L.V. Clinical survey of fractured teeth. J. Am. Dent. Assoc. 1987, 114, 174–177. [Google Scholar] [CrossRef] [PubMed]
- Liao, W.C.; Tsai, Y.L.; Wang, C.Y.; Chang, M.C.; Huang, W.L.; Lin, H.J.; Liu, H.-C.; Chan, C.-P.; Chang, S.-H.; Jeng, J.H.; et al. Clinical and radiographic characteristics of vertical root fractures in endodontically and nonendodontically treated teeth. J. Endod. 2017, 43, 687–693. [Google Scholar] [CrossRef]
- Von Arx, T.; Maldonado, P.; Bornstein, M.M. Occurrence of vertical root fractures after apical surgery: A retrospective analysis. J. Endod. 2021, 47, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Llena-Puy, M.C.; Forner-Navarro, L.; Barbero-Navarro, I. Vertical root fracture in endodontically treated teeth: A review of 25 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2001, 92, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Tamse, A. Iatrogenic vertical root fractures in endodontically treated teeth. Dent. Traumatol. 1988, 4, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.P.; Su, L.P. Clinical observation in 2 representative cases of vertical root fracture in nonendodontically treated teeth. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, e39–e42. [Google Scholar] [CrossRef]
- Lertchirakarn, V.; Palamara, J.E.; Messer, H.H. Patterns of vertical root fracture: Factors affecting stress distribution in the root canal. J. Endod. 2003, 29, 523–528. [Google Scholar] [CrossRef] [Green Version]
- Tamse, A. Vertical root fractures in endodontically treated teeth: Diagnostic signs and clinical management. Endod. Top. 2006, 13, 84–94. [Google Scholar] [CrossRef]
- Huang, C.C.; Chang, Y.C.; Chang, M.C. Analysis of the width of vertical root fracture in endodontically treated teeth by 2 micro–computed tomography systems. J. Endod. 2014, 40, 698–702. [Google Scholar] [CrossRef]
- Tamse, A.; Fuss, Z.; Lustig, J.; Kaplavi, J. An evaluation of endodontically treated vertically fractured teeth. J. Endod. 1999, 25, 506–508. [Google Scholar] [CrossRef]
- Pitts, D.L.; Natkin, E. Diagnosis and treatment of vertical root fractures. J. Endod. 1983, 9, 338–346. [Google Scholar] [CrossRef]
- Moule, A.J.; Kahler, B. Diagnosis and management of teeth with vertical root fractures. Aust. Dent. J. 1999, 44, 75–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, S.; Blanco, L.; Berman, L. Vertical root fractures: Clinical and radiographic diagnosis. J. Am. Dent. Assoc. 2003, 134, 434–441. [Google Scholar] [CrossRef]
- Benson, P. An unusual vertical root fracture. Br. Dent. J. 1991, 170, 147–148. [Google Scholar] [CrossRef]
- Tsesis, I.; Rosen, E.; Tamse, A.; Taschiere, S.; Kfir, A. Diagnosis of vertical root fractures in endodontically treated teeth based on clinical and radiographic indices: A systematic review. J. Endod. 2021, 36, 1455–1458. [Google Scholar] [CrossRef] [PubMed]
- Walton, R.E. Vertical root fracture: Factors related to identification. J. Am. Dent. Assoc. 2017, 148, 100–105. [Google Scholar] [CrossRef]
- Long, H.; Zhou, Y.; Ye, N.; Liao, L.; Jian, F.; Wang, Y.; Lai, W.L. Diagnostic accuracy of CBCT for tooth fractures: A meta-analysis. J. Dent. 2014, 42, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Edlund, M.; Nair, M.K.; Nair, U.P. Detection of vertical root fractures by using cone-beam computed tomography: A clinical study. J. Endod. 2011, 37, 768–772. [Google Scholar] [CrossRef]
- Hassan, B.; Metska, M.E.; Ozok, A.R.; Van der Stelt, P.; Wesselink, P.R. Comparison of five cone be am computed tomography systems for the detection of vertical root fractures. J. Endod. 2010, 36, 126–129. [Google Scholar] [CrossRef]
- Dias, D.R.; Iwaki, L.C.V.; de Oliveira, A.C.A.; Martinhão, F.S.; Rossi, R.M.; Araújo, M.G.; Hayacibara, R.M. Accuracy of high-resolution small-volume cone-beam computed tomography in the diagnosis of vertical root fracture: An in vivo analysis. J. Endod. 2020, 46, 1059–1066. [Google Scholar] [CrossRef]
- Talwar, S.; Utneja, S.; Nawal, R.R.; Kaushik, A.; Srivastava, D.; Singh Oberoy, S. Role of cone-beam computed tomography in diagnosis of vertical root fractures: A systematic review and meta-analysis. J. Endod. 2016, 42, 12–24. [Google Scholar] [CrossRef]
- Lin, L.M.; Langeland, K. Vertical root fracture. J. Endod. 1982, 8, 558–562. [Google Scholar] [CrossRef]
- Alexandre Souza Bier, C.; Shemesh, H.; Tanomaru-Filho, M.; Wesselink, P.R.; Wu, M.K. The ability of different nickel-titanium rotary instruments to induce dentinal damage during canal preparation. J. Endod. 2009, 35, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Shemesh, H.; Bier, C.A.S.; Wu, M.K.; Tanomaru-Filho, M.; Wesselin, P.R. The effects of canal preparation and filling on the incidence of dentinal defects. Int. Endod. J. 2009, 42, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Azer, S.Y.; Anlu, G.; DeAer, Y. Diagnosis and treatment of endodontically treated teeth with vertical root fracture: Three case reports with two-year follow-up. J. Endod. 2011, 37, 97–102. [Google Scholar]
- Lertchirakarn, V.; Palamara, J.E.; Messer, H.H. Load and strain during lateral condensation and vertical root fracture. J. Endod. 1999, 25, 99–104. [Google Scholar] [CrossRef]
- Silver-Thorn, M.B.; Joyce, T.P. Finite element analysis of anterior tooth root stresses developed during endodontic treatment. J. Biomech. Eng. 1999, 121, 108–115. [Google Scholar] [CrossRef]
- Dang, D.A.; Walton, R.E. Vertical root fracture and root distortion: Effect of spreader design. J. Endod. 1989, 15, 294–301. [Google Scholar] [CrossRef]
- Murgel, C.A.F.; Walton, R.E. Vertical root fracture and dentin deformation in curved roots: The influence of spreader design. Dent. Traumatol. 1990, 6, 273–278. [Google Scholar] [CrossRef]
- Obermayr, G.; Walton, R.E.; Leary, J.M.; Krell, K.V. Vertical root fracture and relative deformation during obturation and post cementation. J. Prosthet. Dent. 1991, 66, 181–187. [Google Scholar] [CrossRef]
- Holcomb, J.Q.; Pitts, D.L.; Nicholls, J.I. Further investigation of spreader loads required to cause vertical root fracture during lateral condensation. J. Endod. 1987, 13, 277–284. [Google Scholar] [CrossRef]
- Lindauer, P.; Campbell, A.; Hicks, M.; Pelleu, G.B. Vertical root fractures in curved roots under simulated clinical conditions. J. Endod. 1989, 15, 345–349. [Google Scholar] [CrossRef]
- Yang, H.S.; Lang, L.A.; Molina, A.; Felton, D.A. The effects of dowel design and load direction on dowel-and-core restorations. J. Prosthet. Dent. 2001, 85, 558–567. [Google Scholar] [CrossRef]
- Kishen, A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod. Top. 2006, 13, 57–83. [Google Scholar] [CrossRef]
- Felton, D.; Webb, E.; Kanoy, B.; Dugoni, J. Threaded endodontic dowels: Effect of post design on incidence of root fracture. J. Prosthet. Dent. 1991, 65, 179–187. [Google Scholar] [CrossRef]
- Dean, J.P.; Jeansonne, B.G.; Sarkar, N. In vitro evaluation of a carbon fiber post. J. Endod. 1998, 24, 807–810. [Google Scholar] [CrossRef]
- Cagidiaco, M.; García-Godoy, F.; Vichi, A.; Grandini, S.; Goracci, C.; Ferrari, M. Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am. J. Dent. 2008, 21, 179–184. [Google Scholar]
- Sornkul, E.; Stannard, J.G. Strength of roots before and after endodontic treatment and restoration. J. Endod. 1992, 18, 440–443. [Google Scholar] [CrossRef]
- Trabert, K.; Caputo, A.; Abou-Rass, M. Tooth fracture-a comparison of endodontic and restorative treatments. J. Endod. 1978, 4, 341–345. [Google Scholar] [CrossRef]
- Gutmann, J.L. The dentin-root complex: Anatomic and biologic considerations in restoring endodontically treated teeth. J. Prosthet. Dent. 1992, 67, 458–467. [Google Scholar] [CrossRef]
- Pilo, R.; Tamse, A. Residual dentin thickness in mandibular premolars prepared with gates glidden and parapost drills. J. Prosthet. Dent. 2000, 83, 617–623. [Google Scholar] [CrossRef]
- Pilo, R.; Corcino, G.; Tamse, A. Residual dentin thickness in mandibular premolars prepared with hand and rotatory instruments. J. Endod. 1998, 24, 401–404. [Google Scholar] [CrossRef]
- Lertchirakarn, V.; Palamara, J.E.; Messer, H.H. Finite element analysis and strain-gauge studies of vertical root fracture. J. Endod. 2003, 29, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Arola, D.; Ivancik, J.; Majd, H.; Fouad, A.; Bajaj, D.; Zhang, X.Y.; Eidelman, N. Microstructure and mechanical behavior of radicular and coronal dentin. Endod. Top. 2012, 20, 30–51. [Google Scholar] [CrossRef]
- Xu, H.; Zheng, Q.; Shao, Y.; Song, F.; Zhang, L.; Huang, Q.; Huang, D.M. The effects of ageing on the biomechanical properties of root dentine and fracture. J. Dent. 2014, 42, 305–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinney, J.H.; Nalla, R.K.; Pople, J.A.; Breunig, T.M.; Ritchie, R.O. Age-related transparent root dentin: Mineral concentration, crystallite size, and mechanical properties. Biomaterials 2005, 26, 3363–3376. [Google Scholar] [CrossRef]
- Misch, C. Contemporary Implant Dentistry, 2nd ed.; Mosby: New York, NY, USA, 1999. [Google Scholar]
- Engelman, M.J.; Craig, J.A. Clinical Decision Making and Treatment Planning in Osseointegration; Quintessence Pub. Co.: Chicago, IL, USA, 1997. [Google Scholar]
- Kim, Y.; Oh, T.J.; Misch, C.E.; Wang, H.L. Occlusal considerations in implant therapy: Clinical guidelines with biomechanical rationale. Clin. Oral Implant Res. 2005, 16, 26–35. [Google Scholar] [CrossRef]
- Assif, D.; Nissan, J.; Gafni, Y.; Gordon, M. Assessment of the resistance to fracture of endodontically treated molars restored with amalgam. J. Prosthet. Dent. 2003, 89, 462–465. [Google Scholar] [CrossRef]
- Rosen, E.; Beitlitum, I.; Tamse, A.; Taschieri, S.; Tsesis, I. Implant-associated vertical root fracture in adjacent endodontically treated teeth: A case series and systematic review. J. Endod. 2016, 42, 948–952. [Google Scholar] [CrossRef]
- Cameron, C.E. Cracked-tooth syndrome. J. Am. Dent. Assoc. 1964, 68, 405–411. [Google Scholar] [CrossRef]
- Lee, C.Y.; Wu, C.F.; Chen, C.M.; Chang, Y.Y. Qualitative study for betel quid cessation among oral cancer patients. PLoS ONE 2018, 13, e0199503. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.J.; Yin, X.M.; Wu, H.J. Relationship between vertical root fracture and the habits of chewing betel nut. Hunan Yi Ke Da Xue Xue Bao 2001, 26, 161–162. [Google Scholar] [PubMed]
- Pegoretti, A.; Fambri, L.; Zappini, G.; Bianchetti, M. Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials 2002, 23, 2667–2682. [Google Scholar] [CrossRef]
- Tamse, A.; Fuss, Z.; Lustig, J.; Ganor, Y.; Kaffe, I. Radiographic features of vertically fractured, endodontically treated maxillary premolars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1999, 88, 348–352. [Google Scholar] [CrossRef]
- Nicopoulou-Karayianni, K.; Bragger, U.; Lang, N. Patterns of periodontal destruction associated with incomplete root fractures. Dentomaxillofac. Radiol. 1997, 26, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Tamse, A.; Kaffe, I.; Lustig, J.; Ganor, Y.; Fuss, Z. Radiographic features of vertically fractured endodontically treated mesial roots of mandibular molars. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2006, 101, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Abou-Rass, M. Crack lines: The precursors of tooth fractures-their diagnosis and treatment. Quint. Int. Dent. Dig. 1983, 14, 437–447. [Google Scholar]
- Bender, U.; Freedland, J.B. Adult root fracture. J. Am. Dent. Assoc. 1983, 107, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Borén, D.L.; Jonasson, P.; Kvist, T. Long-term survival of endodontically treated teeth at a public dental specialist clinic. J. Endod. 2015, 41, 176–181. [Google Scholar] [CrossRef]
- Siskin, M.; Lommel, T.J.; Meister, F., Jr.; Gerstein, H.; Davies, E.E.; Tilk, M.A. Alveolar bone loss associated with vertical root fractures: Report of six cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1978, 45, 909–919. [Google Scholar] [CrossRef]
- Anitha, S.; Rao, D.S. Hemisection: A treatment option for an endodontically treated molar with vertical root fracture. J. Contemp. Dent. Pract. 2015, 16, 163–165. [Google Scholar] [CrossRef] [PubMed]
- Tamse, A.; Zilburg, I.; Halpern, J. Vertical root fractures in adjacent maxillary premolars: An endodontic-prosthetic perplexity. Int. Endod. J. 1998, 31, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, S.; Iwai, K.; Ishihara, Y.; Amari, M.; Ohshima, K. Stress analysis of bridge abutment teeth with cemented dowels. Nihon Hotetsu Shika Gakkai Zasshi 1990, 34, 175–185. [Google Scholar] [CrossRef] [PubMed]
- Dederich, D.N. CO2 laser fustion of a vertical root fracture. J. Am. Dent. Assoc. 1999, 130, 1195–1199. [Google Scholar] [CrossRef] [PubMed]
- Stewart, G.G. The detection and treatment of vertical root fractures. J. Endod. 1988, 14, 47–53. [Google Scholar] [CrossRef]
- Barkhordar, R.A. Treatment of vertical root fracture: A case report. Quint. Int. 1991, 22, 707–709. [Google Scholar]
- Vertucci, F.J. Management of a vertical root fracture. J. Endod. 1985, 11, 126–131. [Google Scholar] [CrossRef]
- Matusow, R.J. Resolution of fused vertical molar root bridge abutment fracture: Report of case. J. Am. Dent. Assoc. 1988, 116, 658–660. [Google Scholar] [CrossRef]
- Trope, M.; Rosenberg, E.S. Multidisciplinary approach to the repair of vertically fractured teeth. J. Endod. 1992, 18, 460–463. [Google Scholar] [CrossRef]
- Selden, H.S. Repair of incomplete vertical root fractures in endodontically treated teeth-in vivo trials. J. Endod. 1996, 22, 426–429. [Google Scholar] [CrossRef]
- Oliet, S. Treating vertical root fractures. J. Endod. 1984, 10, 391–396. [Google Scholar] [CrossRef]
- Funato, A.; Funato, H.; Matsumoto, K. Treatment of a vertical root fracture. Dent. Traumatol. 1999, 15, 46–47. [Google Scholar] [CrossRef]
- Sugaya, T.; Kawanami, M.; Noguchi, H.; Kato, H.; Masaka, N. Periodontal healing after bonding treatment of vertical root fracture. Dent. Traumatol. 2001, 17, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Kinomoto, Y.; Miura, M.; Sato, I.; Takeshige, F.; Ebisu, S. Short-term evaluation of intentional replantation of vertically fractured roots reconstructed with dentin-bonded resin. J. Endod. 2002, 28, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Kawai, K.; Masaka, N. Vertical root fracture treated by bonding fragments and rotational replantation: Treatment of vertical root fractures. Dent. Traumatol. 2002, 18, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Kinomoto, Y.; Takeshige, F.; Ebisu, S. Prognosis of intentional replantation of vertically fractured roots reconstructed with dentin-bonded resin. J. Endod. 2004, 30, 145–148. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, M.; Unal, G.C. A successful treatment of vertical root fracture: A case report and 4-year follow-up. Dent. Traumatol. 2008, 24, e56–e60. [Google Scholar] [CrossRef]
- Da Silva, E.J.N.L.; dos Santos, G.R.; Krebs, R.L.; Coutinho-Filho, T.D.S. Surgical alternative for treatment of vertical root fracture: A case report. Iran. Endod. J. 2011, 7, 40–44. [Google Scholar]
- Moradi Majd, N.; Akhtari, F.; Araghi, S.; Homayouni, H. Treatment of a vertical root fracture using dual-curing resin cement: A case report. Case Rep. Dent. 2012, 2012, 985215. [Google Scholar] [CrossRef]
- Okaguchi, M.; Kuo, T.; Ho, Y.C. Successful treatment of vertical root fracture through intentional replantation and root fragment bonding with 4-META/MMA-TBB resin. J. Formos. Med. Assoc. 2019, 118, 671–678. [Google Scholar] [CrossRef]
- Taschieri, S.; Tamse, A.; Del Fabbro, M.; Rosano, G.; Tsesis, I. A new surgical technique for preservation of endodontically treated teeth with coronally located vertical root fractures: A prospective case series. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2010, 110, e45–e52. [Google Scholar] [CrossRef]
- Floratos, S.G.; Kratchman, S.I. Surgical management of vertical root fractures for posterior teeth: Report of four cases. J. Endod. 2012, 38, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Hadrossek, P.H.; Dammaschke, T. New treatment option for an incomplete vertical root fracture–A preliminary case report. Head Face Med. 2014, 10, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Von Arx, T.; Bosshardt, D. Vertical root fractures of endodontically treated posterior teeth. Swiss Dent. J. 2017, 127, 14–23. [Google Scholar] [PubMed]




| Author | Number of Teeth | Periodontal Pocket | Pain | Swelling Abscess | Sinus Tract |
|---|---|---|---|---|---|
| Meister et al., 1980 [13] | 32 | 93% | 66% | 28% | 13% |
| Chan et al., 1998 [19] | 64 | 84% | 52% | 30% | 11% |
| Tamse et al., 1999 [30] | 92 | 67% | 55% | 34% | 35% |
| Cohen et al., 2006 [6] | 227 | 40% | Pain on percussion: 69% Pain on palpation: 69% Pain on mastication: 61% | 15% | 18% |
| PradeepKumar et al., 2016 [1] | 197 | 81% | Pain on percussion: 60% Pain on palpation: 62% | 67% | |
| Liao et al., 2017 [22] | 65 | 91% | NA | NA | NA |
| Walton et al., 2017 [36] | 42 | 66% | No to mild pain: 100% | 77% | 31% |
| Von Arx and Bosshradt, 2017 [75] | 30 | 40% | Pain: 60% Percussion sensitivity: 6% Palpation sensitivity: 6% | 23% | 46% |
| See et al., 2019 [11] | 61 | 57% | Tenderness to percussion: 27% Tenderness to palpation: 29% | 36% | 60% |
| Author | Number of Teeth | Halo Radiolucency | Lateral Radiolucency | Apical Radiolucency | Fractured Root Displacement | Angular Defect | Normal Appearance | Other Findings |
|---|---|---|---|---|---|---|---|---|
| Meister et al., 1980 [13] | 32 | 75% | 22% | 3% | NA | NA | ||
| Nicopoulou- Karayianni et al., 1997 [77] | 22 | 45% | 27% | 5% | NA | 0% | 5% | |
| Chan et al., 1998 [19] | 64 | NA | NA | 27% | 20% | 63% | NA | PDL widening: 39% Root canal space widening: 25% |
| Tamse et al., 1999 [30] | 51 | 57% | 14% | 4% | NA | 14% | 2% | |
| Tamse et al., 1999 [76] | 92 | 39% | 24% | 24% | NA | NA | 13% | |
| Tamse et al., 2006 [78] | 49 | 37% | 29% | 10% | NA | 6% | 8% | |
| Cohen et al., 2006 [6] | 227 | 50% | 21% | 27% | NA | NA | ||
| Liao et al., 2017 [22] | 65 | NA | NA | 80% | 43% | 95% | NA | |
| Walton et al., 2017 [36] | 42 | NA | NA | 21% | 17% | 11% | 21% | |
| Von Arx and Bosshradt, 2017 [75] | 30 | 36% | 53% | NA | NA | 10% | ||
| See et al., 2019 [11] | 61 | 50% | 14% | 26% | NA | NA | 4% | |
| Category | VRFETT | VRFNETT |
|---|---|---|
| Prevalence | 2–25% [7,8,9,10,11,13,14,15,16,17] | Not reported |
| Gender | No preference in gender [1,4,6,18] | Male [2,4,19,20] |
| Age | Predominantly > 40 years old [3,4,6,14,19] Mean age: Non-endodontically treated group>Endodontically treated group [2,3,19,20,22] | |
| Tooth distribution | Maxillary premolars and mandibular molars [23,24,25] | Maxillary and mandibular first molars in the Chinese population [2,4,19,20,26] |
| Root distribution | Premolars and mesial roots of mandibular molars [14,23,24,25] | Mesiobuccal roots of maxillary molars and mesial roots of mandibular molars [2,3,4,19,20,26] |
| Etiology and predisposing factors | Iatrogenic factors
| |
| Specific anatomies of the susceptible roots [4,54,60,61,62] | ||
| Age-related microstructural changes [65,66,81] | ||
| Clinical features |
| |
| Attrited occlusal surface [4,19] | ||
| Radiographic characteristics | ||
| Author | Number of Teeth | Status of the VRF Teeth | Method | Management or Material Used to Seal the Fracture Interface | Follow-Up | Prognosis |
|---|---|---|---|---|---|---|
| Sinai et al., 1978 [89] | 1 | VRFETT | Intraoral | The root segment, canal filling material and the granulomatous tissue were all removed. | 10 years | Bone formation was observed at 7 months follow-up. However, the long-term outcome was unfavorable. |
| Vertucci, 1985 [90] | 1 | VRFETT | Intraoral | Removal of a major portion of the buccal half of the root and applying 20% citric acid solution for 5 min on all exposed root surfaces. | 3 years | The tooth functioned normally without periodontal defect and radiographic pathosis. However, the author considered that the long-term prognosis remained questionable. |
| Stewart, 1988 [87] | 3 | 1 VRFETT 2 VRFNETT | Intraoral | Canal dressing with calcium hydroxide plus the contrast medium. At least 9 to 12 months were needed to present bone formation and more cementum for healing. Then, the root canal was obturated with gutta-percha. | 4 months to 10 years | Healing of the periradicular tissue and increasing bony density were noted. |
| Matusow, 1988 [91] | 1 | VRFETT | Intraoral | Strip the fused fractured mesial root and leave the distal root fragment in the molar of a bridge abutment. | 14 months | The tooth was asymptomatic and showed bone repair. |
| Barkhordar, 1991 [88] | 1 | VRFNETT | Intraoral | Use calcium hydroxide dressing to induce healing of fractured roots. Glass–ionomer cement was further used as a root canal sealer to bond the fracture fragment. | 6 months | Healing of the osseous defect was observed. |
| Dederich, 1999 [86] | 1 | VRFETT | Intraoral | Apply CO2 laser fusion of the fracture interface and place a compressed collagen matrix barrier. | 1 year | No inflammation, pocket reduction and increased radiodensity at the osseous defect. |
| Author | Number of Teeth | Status of the VRF Teeth | Method | Management or Material used to Seal the Fracture Interface | FOLLOW-UP | Prognosis |
|---|---|---|---|---|---|---|
| Oliet, 1984 [94] | 3 | 1 VRFNETT 2 VRFETT | Extraoral and intentional replantation | Re-cementation of the fracture fragment with cyanoacrylate. | 3 to 16 months | Although the teeth functioned normally, the long-term prognosis remained poor. |
| Funato et al., 1999 [95] | 1 | VRFETT | Intraoral | 4-META/MMA-TBB dentin-bonded resin | 6 months | The tooth was asymptomatic and showed reduced radiolucent area. |
| Sugaya et al., 2001 [96] | 23 | VRFETT | Group A: Intraoral Group B: Extraoral and intentional replantation | 4-META/MMA-TBB dentin-bonded resin | 22 to 33 months | Group A: 9 out of 11 cases with good prognosis Group B: 9 out of 12 cases with good prognosis |
| Hayashi et al., 2002 [97] | 20 | VRFETT | Extraoral and intentional replantation | 4-META/MMA-TBB dentin-bonded resin | 4 to 45 months | Survival rates were 83.3% at 12 months and 36.3% at 24 months. |
| Kawai et al., 2002 [98] | 2 | VRFETT | Extraoral and intentional replantation | Apply adhesive resin cement to bond the fracture interface. | 3 years | The teeth were asymptomatic and displayed bone regeneration. |
| Hayashi et al., 2004 [99] | 26 | VRFETT | Extraoral and intentional replantation | 4-META/MMA-TBB dentin-bonded resin | 4 to 76 months | Survival rates were 88.5% at 12 months, 69.2% at 36 months and 59.3% at 60 months. |
| Öztürk and Ünal, 2008 [100] | 1 | VRFETT | Extraoral and intentional replantation | Apply self-etching dual-cured adhesive resin cement and place a membrane. | 4 years | The tooth was asymptomatic and bone regeneration was observed. |
| Özer et al., 2011 [45] | 3 | VRFETT | Extraoral and intentional replantation | Self-etching dual-cure adhesive resin cement | 2 years | The teeth were asymptomatic and showed reduced periapical radiolucency. |
| Nogueira Leal da Silva et al., 2012 [101] | 1 | VRFETT | Intraoral | Bond with composed resin and place a synthetic hydroxyapatite graft. | 2 years | The tooth showed no symptom and sign. |
| Moradi Majd et al., 2012 [102] | 1 | VRFETT | Extraoral and intentional replantation | Prepare the fracture line with an ultrasonic device and seal with dual-curing resin. | 12 months | The tooth was asymptomatic, and the apical radiolucency reduced in size. |
| Okaguchi et al., 2019 [103] | 6 | VRFETT | Extraoral and intentional replantation | 4-META/MMA-TBB dentin-bonded resin | 33 to 74 months | Tooth function was normal with successful clinical outcome and healing of radiolucent lesions. |
| Author | Number of Teeth | Status of the VRF Teeth | Method | Management or Material Used to Seal the Fracture Interface | Follow-Up | Prognosis |
|---|---|---|---|---|---|---|
| Trope et al., 1992 [92] | 1 | VRFETT | Extraoral and intentional replantation | Biocompatible glass–ionomer bone cement in conjunction with an expanded polytetrafluoroethylene (Gore-Tex) membrane. | 1 year | The tooth functioned normally without periodontal pocket and exhibited good healing outcome. |
| Selden, 1996 [93] | 6 | VRFETT | Intraoral | Apply silver glass–ionomer cement to bond the fracture fragment and perform guided tissue regeneration. | 2 to 12 months | Five cases failed within 2 to 11 months. The other one was asymptomatic but failed at 1 year due to exacerbation of the fracture line. |
| Floratos and Kratchman, 2012 [105] | 4 | VRFETT | Intraoral | The fracture line was removed by resecting the root fragment. Retrograde preparation and retrograde filling were performed with MTA. An absorbable collagen membrane was covered over the bone defect. | 8 to 24 months | The teeth were asymptomatic. Periapical healing with periodontal ligament re-formation was noted. |
| Hadrossek and Dammaschke, 2014 [106] | 1 | VRFETT | Extraoral and intentional replantation | Prepare the fracture gap with a small diamond bur and fill with Biodentine. Then, replant the tooth with fixation. | 24 months | The tooth was asymptomatic, and the periodontal pocket returned to normal. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, W.-C.; Chen, C.-H.; Pan, Y.-H.; Chang, M.-C.; Jeng, J.-H. Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge. J. Pers. Med. 2021, 11, 1375. https://doi.org/10.3390/jpm11121375
Liao W-C, Chen C-H, Pan Y-H, Chang M-C, Jeng J-H. Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge. Journal of Personalized Medicine. 2021; 11(12):1375. https://doi.org/10.3390/jpm11121375
Chicago/Turabian StyleLiao, Wan-Chuen, Chi-Hung Chen, Yu-Hwa Pan, Mei-Chi Chang, and Jiiang-Huei Jeng. 2021. "Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge" Journal of Personalized Medicine 11, no. 12: 1375. https://doi.org/10.3390/jpm11121375
APA StyleLiao, W.-C., Chen, C.-H., Pan, Y.-H., Chang, M.-C., & Jeng, J.-H. (2021). Vertical Root Fracture in Non-Endodontically and Endodontically Treated Teeth: Current Understanding and Future Challenge. Journal of Personalized Medicine, 11(12), 1375. https://doi.org/10.3390/jpm11121375







