To define and formulate the problem under investigation, we first describe the problem and list its assumptions. Then, we discuss the methodology and approaches used to apportion compensation among the available pairs in a kidney-exchange chain.
3.1. Problem Definition and Underlying Assumptions
As mentioned in the preceding section, the purpose of this article is to compare ECA and FCA approaches in the operation of apportioning the compensation of external donors who starts a kidney-exchange chain among the participating incompatible pairs and to present a mathematical mechanism for this goal under the FCA approach. The share of the total compensation allocated to each incompatible pair in the chain under the FCA approach must be according to the characteristics to both kidneys being receives and donated to the chain.
To describe the problem,
Figure 1 illustrates a kidney-exchange chain with a non-designated living donor, four incompatible pairs and a recipient from the waiting list. Intuitively, several recipients and donors in the chain have different characteristics, such as age, sex, blood type, and body size. Therefore, they need to find a donor whose kidney is compatible with the patient of pair 1. Though all incompatible pairs pay the compensation altogether, they may not have the same payment share due to their variant situation.
Several authors in the literature have discussed the notion of fairness and equity in the allocation of divisible and indivisible goods [
40,
41,
42,
43,
44]. In general, an allocation is defined as equitable if no agent envies another, i.e., no agent prefers another agent’s bundle to his own. Additionally, an allocation is defined as fair if it is both equitable and Pareto efficient. Therefore, to have a fair allocation, one must minimize envy between agents. In our problem, agents are incompatible pairs in the chain, and bundles are the recipients’ allocated kidneys. Therefore, it is possible that an incompatible pair envies another incompatible pair’s place in the chain if the exchange of places is feasible between those two agents. However, since an optimization model already forms the exchange chain, any exchange of places between its participating pairs will result in less overall transplant quality and, consequently, more overall envy. Therefore, the allocation of places in each chain between participating pairs has the minimum feasible overall envy.
The main question of this article is how this compensation should be apportioned among incompatible pairs to have the minimum overall envy after the operations. To answer this question, this study presents a mathematical mechanism to determine the share of compensation paid by each participating pair under the FCA approach. Then, the results from this mechanism are compared with the apportionment results under the ECA approach. The following major assumptions are considered:
The exchange chain is given in this study. To obtain this chain, one can employ approaches available in the literature [
5,
45,
46]. Therefore, the characteristics of incompatible pairs are known, and there is no limitation for the length of the chain used in the proposed approach.
Living donor’s cost apportionment is carried out to determine the share of each participating pair before the transplantation process.
The chain pairs have been chosen from a predefined pool and do not choose to move to another chain [
8]. That is because of two facts: first, they are not aware of the existence of any other chain; second, they are not aware whether the other chain, if available, is more appropriate for them or not.
All donor-recipient participants in the chain program are incompatible, and their orders in the chain have been defined based on the exchange program’s objective. Therefore, an incompatible pair cannot alter its corresponding pair for the kidney exchange [
8,
25].
It is assumed that all of the transplants in the chain would be performed successfully. In case of failure of the exchange chain due to last-minute failure of a transplant, the total share of subsequent incompatible pairs from the compensation is paid by the organization responsible for organ procurement and transplantation in the system.
The characteristics of the kidney initiating the chain program are known. The amount of compensation that should be paid to the initial donor to cover his costs associated with the donation process is also given, and all participants are informed about and have agreed to this value.
Although the last donor-recipient pair of the chain pays a share of the corresponding patient’s compensation, their donated kidney would be assigned to the first compatible patient on the waiting list.
3.2. Methodology
We compared two different approaches based on equality and equity to determine the share of the compensation for incompatible pairs. If
C is the total amount of compensation,
n is the number of participating incompatible pairs in the chain and
Ci is the portion of compensation allocated to incompatible pair
i. In the ECA approach,
Ci is easily calculated as follows:
However, the FCA approach is complicated. To develop this approach, we employ the Shapley value, one of the most prominent ways to allocate gains obtained by a set of players in coalitional cooperative games. The main idea of Shapley value is that members should receive payments or shares proportional to their marginal contributions in a cooperative game [
47]. Allocation of costs in a cooperative game is another application of the Shapley value [
48,
49,
50,
51]. To employ the Shapley value for the purpose of compensation apportionment in the problem under investigation, the expected marginal contributions of each incompatible pair must be calculated [
47]. In other words, compensation apportioning should match the characteristics of the kidney that participants are receiving from the system and the kidney they are donating to the system. For instance, receiving a younger kidney should result in a higher share, or conversely, donating a younger kidney should reduce the pair’s share.
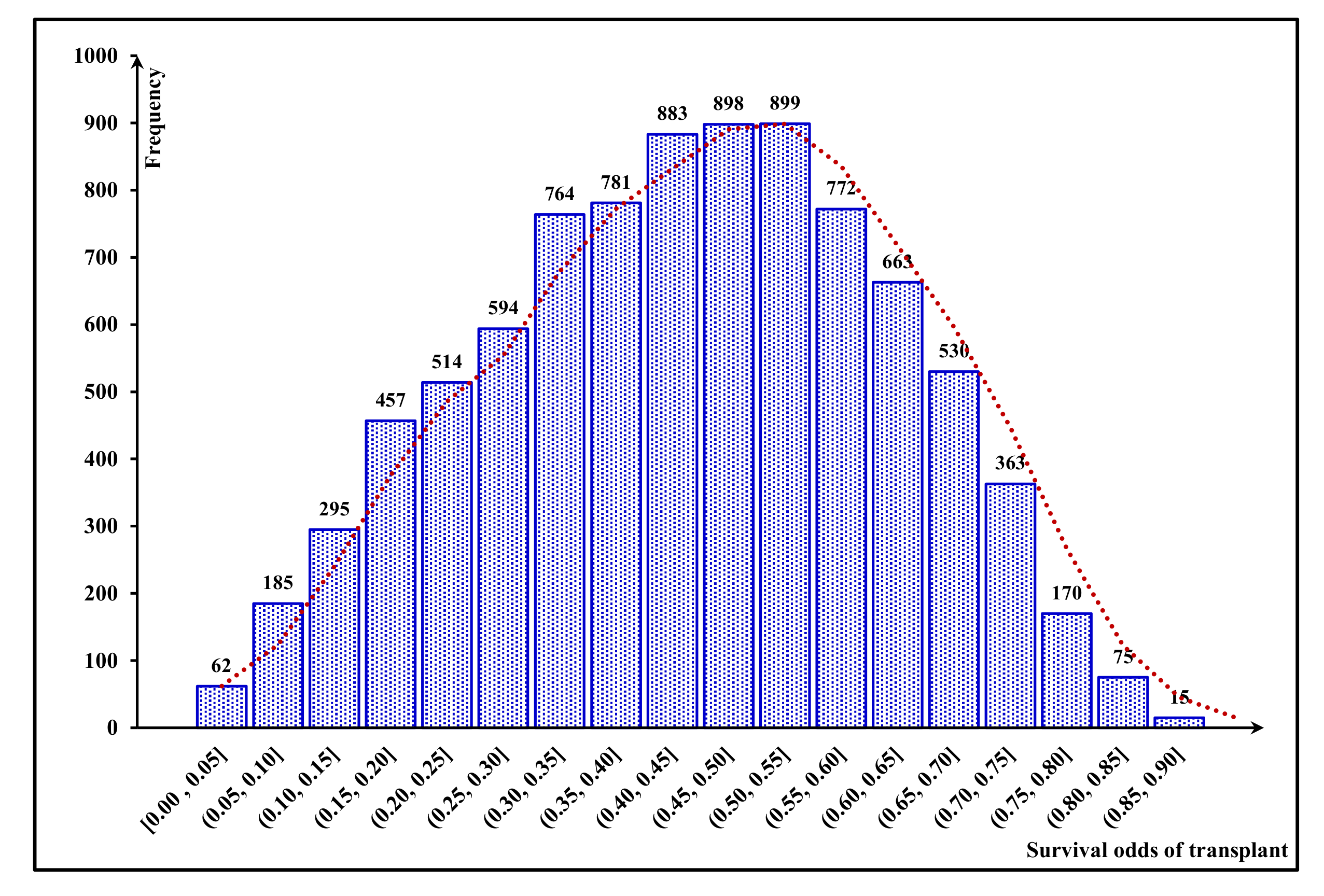
Taking into account all mentioned factors, we calculate the odds of graft survival and determine patients’ share in providing compensation according to these probabilities. To this end, we employ the utility function to capture the nonlinear impact of graft-survival probability on the satisfaction of the pairs. Afterwards, compensation is apportioned among all pairs of the chain, considering their utility to the system. Given
Ui is the utility that transplant
i brings about the system, the FCA approach is defined as:
where
ui is the utility donated by the
ith incompatible pair to the chain and equivalents to the utility of the
ith transplant, estimated based on the system administrator’s preferences as the entity responsible for matching donors and patients. In addition,
ui−1 indicates the amount of utility received by incompatible pair
i and, similarly, equals the utility of transplantation
i−1. Accordingly,
u0 indicates the utility of the initiating transplantation of the chain.
Note that each transplant has a utility value for the social planner, e.g., the IKF, aiming to maximize the number of patients receiving a kidney in the exchange program. Since Equation (2) takes the condition of both received and donated kidneys into account, it diminishes total envy between participants and consequently increases fairness.
Utility theory has been proposed by Von Neumann and Morgenstern [
52] to measure a decision maker’s preferences in a mathematical form. To apply this theory, a function known as a utility function can generally be estimated to calculate a decision maker’s preferences between various choices in a decision-making problem [
53]. According to this theory, if the decision maker prefers choice A to other choices, the utility of choice A must be higher than that of other choices [
52]. In addition, another characteristic of the corresponding utility function is monotonicity. A monotonically increasing utility function means that the decision maker prefers higher values of an attribute.
Conversely, the decision maker prefers lower values of an attribute if the utility function is monotonically decreasing. With a non-monotonic utility function, the decision maker’s preferences concerning different attribute levels may increase or decrease [
53]. Risk aversion is a characteristic of the decision maker that can be inferred from the utility function. In general, a decision maker is risk-averse if and only if his/her utility function is concave. On the contrary, risk-prone decision makers have convex utility functions [
53]. Utility theory has been widely used in healthcare problems, such as measuring patients’ quality of life based on their condition [
54,
55,
56] and measuring quality of life for ESKD patients on dialysis [
57].
To estimate the utility of a transplant, different characteristics of the recipient and the donor must be considered. Therefore, rather than directly estimating the utility function based on these attributes, we propose using these attributes to estimate the probability of graft survival and then defining each transplant’s utility based on its graft-survival probability. In this article, the likelihood of graft survival is estimated by a calculator based on the multivariate Cox regression survival analysis presented in [
20]. This calculator, called the kidney graft survival calculator (KGSC), developed based on 15 years of United States transplantation data from the Scientific Registry of Transplant Recipients (SRTR), can estimate the probability of graft survival 5 and 10 years post-transplant. It takes into account several attributes of donors and recipients, such as age, sex and body size. It also considers the type of the living donor (related/unrelated), number of HLA ABDR mismatches, ABO compatibility between donor and recipient, donor and recipient race, donor’s history of cigarette use, transplant year, recipient’s panel reactive antibody (PRA), time on dialysis, insurance type, history of previous transplants and recipient’s diabetes status the potential impact of these factors on the probability of graft survival. Regarding the variant of attributes utilized in this calculator and its ability to estimate the likelihood of graft survival for transplants with living donors [
20], we chose KGSC in our proposed equitable-cost-apportionment mechanism. Additionally, we established our mechanism based on the probability of graft survival 10 years after transplant, since this period is frequently considered and used in graft-survival predictions and evaluations in the literature [
20,
58,
59,
60,
61].
As mentioned, converting the graft-survival probability to the transplant’s utility requires definition of a utility function. This study estimated this function using the standard gamble (SG) technique [
62] on the data gathered from 10 selected experienced experts of the Iranian Kidney Foundation who are in charge of the matching process in Tehran, Iran. To utilize this technique, we designed an interview structure and asked these experts to state their preferences of different probability levels of graft survival. According to this structure, presented in
Figure 2, each interviewee was subjected to seven sets of lotteries in three stages. In each lottery, based on the SG technique, the participant was asked to imagine a situation where they had two alternatives to assign an unknown kidney to a recipient. The first alternative was participating in a gamble in which the graft-survival probability after transplant was one of two known values with a 50-50 chance. The second alternative was undergoing the transplant with a different fixed value of graft-survival probability. After knowing the graft-survival probability values of the two probable outcomes of the first alternative in each lottery, the respondents were asked to declare the minimum probability of graft survival they would still prefer as the second alternative rather than the first alternative. The utility of the declared value is the average of utilities of the outcomes of the first alternative. As presented in the
Appendix A, for simplicity, the participants were asked to declare this value as a number multiple of 5%. After calculating the utility of the declared value of survival probability, by replacing the gamble outcomes one by one with this value, two different lotteries of the next stage were designed. After receiving each of the interviewees’ responses to all seven lotteries, the average probabilities of graft survival in each level of utility were estimated. It is worth mentioning that since the utility values are defined in the interval between 0 and 1, we could not increase the number of the independent values extracted from the participants, so calculation of utility function was based on these values.
3.3. Mechanisms of Compensation Apportionment
As Equation (1) shows, the ECA approach apportions the identified compensation among all participants equally. However, the mechanism proposed under the FCA approach aims to apportion compensation among all participants regarding the characteristics of both kidneys they will receive and donate. These characteristics can be represented by the amount of utility provided for each participant. Due to the impacts of transplantation failure on the recipient’s quality of life and length of the waiting list, a kidney’s survival probability in the recipient’s body is usually considered the main factor in patient-utility estimation [
63]. According to this factor and based on our interview structure, presented in
Section 3.2, the utility values of transplants and the corresponding values of graft-survival probability were obtained from the interviewees. Utility values of 0.0% and 100.0% survival probability were assumed at 0.0 and 1.0, respectively, to initiate the interview process. The results of these interviews are presented in the
Appendix A. In addition, the average results of the interviews are shown in
Table 1. Based on these results,
Figure 3 illustrates the relationship between the probability of graft survival and transplant utility. As this figure shows, the obtained utility function is monotonically increasing and concave, demonstrating that decision makers are risk-averse [
53].
Regarding the collected data, provided in the
Appendix A and presented in
Table 1 and
Figure 3, and the characteristics of the utility function being appropriate to capture this behavior [
52], transplant’s utility function is estimated as follow:
where
U is the estimated utility of the transplant and
T is the probability of graft survival 10 years after transplantation.
Although the acquired utility function helps us estimate any transplantation utility, it could not be directly utilized to determine the share of an incompatible pair. Each pair grants an amount of utility to the chain and receives another amount from the chain. Therefore, the difference between the granted and the received utilities should be considered as an index to determine the share of compensation. To this end, let us assume that
n is the number of incompatible pairs,
is the difference between the granted and the received utilities for incompatible pair
i, that is the net utility, and be calculated as follows:
To avoid a negative value of Δ
u and to keep the share of incompatible pairs non-negative, Equation (4) is normalized as follows:
In this Equation
is the normalized value of the net utility of incompatible pair
i. Regarding Equation (5), an incompatible pair pays more portion of compensation if it has a higher value of normalized net utility. Therefore, each pair’s percentage of total compensation is calculated as follows:
where
Ci is the portion of the compensation allocated to incompatible pair
i and
C is the total amount of compensation that should be paid to the external donor. It is worth mentioning that if all pairs receive the same utility, the total normalized net utility would be zero. In this case, all pairs should pay an equal portion of the total compensation. Conversely, if the pairs receive variant normalized net utility, they would pay a different portion of the total compensation that could be obtained by Equation (6). Additionally, according to this Equation, the incompatible pair with the lowest Δ
u value does not pay any share of the compensation if its respective
.