A Personalized Approach to Percutaneous Coronary Interventions in the Left Main Coronary Artery—Is the Female Gender Associated with Worse Outcomes?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical and Angiographic Data
2.3. Study Endpoints
2.4. Statistical Analysis
3. Results
3.1. Baseline Study Population Characteristics
3.2. Procedure Details
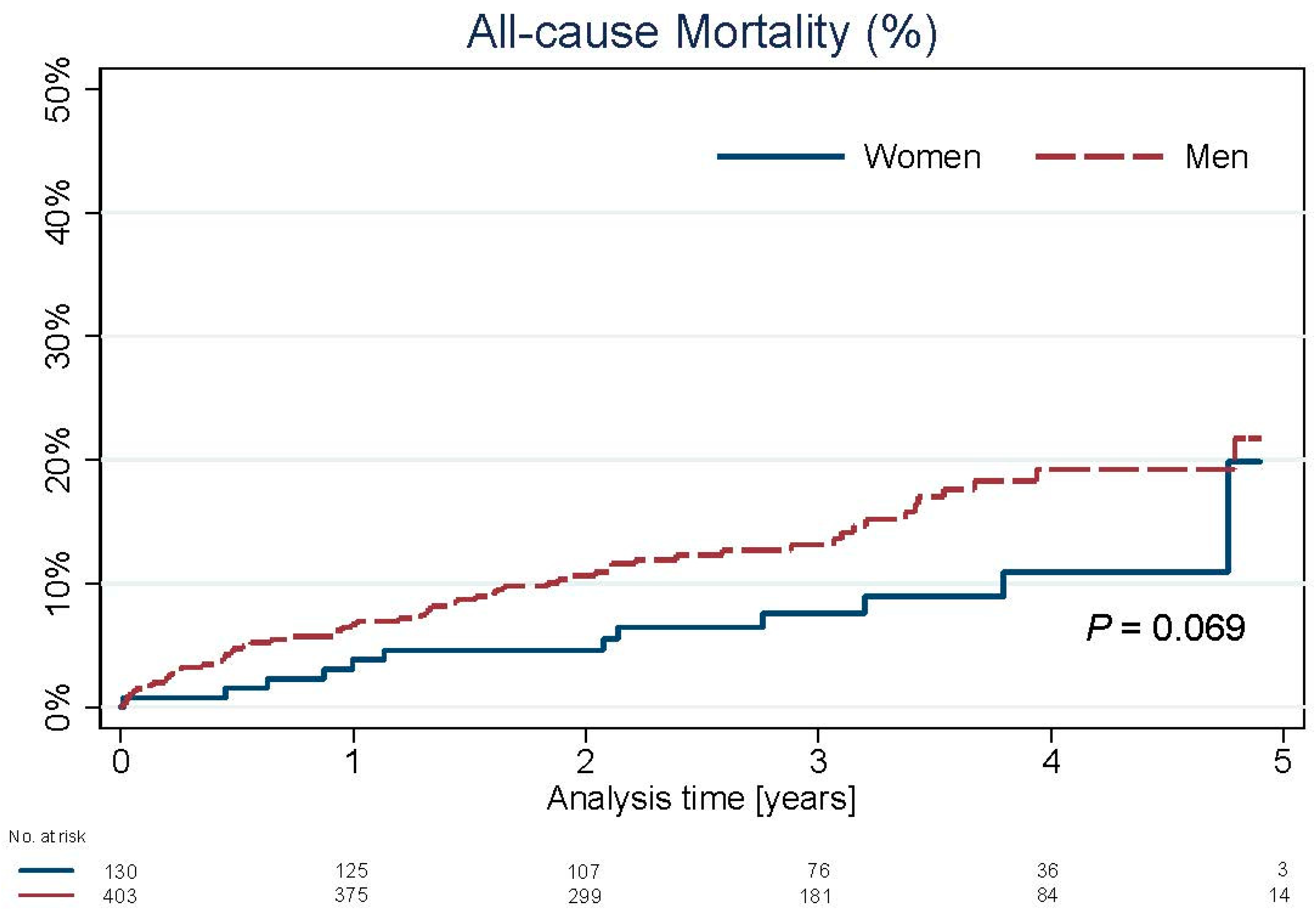
3.3. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stramba-Badiale, M.; Fox, K.M.; Priori, S.G.; Collins, P.; Daly, C.; Graham, I.; Jonsson, B.; Schenck-Gustafsson, K.; Tendera, M. Cardiovascular diseases in women: A statement from the policy conference of the European Society of Cardiology. Eur. Heart J. 2006, 27, 994–1005. [Google Scholar] [CrossRef] [Green Version]
- Cowley, M.J.; Mullin, S.M.; Kelsey, S.F.; Kent, K.M.; Gruentzig, A.R.; Detre, K.M.; Passamani, E.R. Sex differences in early and long-term results of coronary angioplasty in the NHLBI PTCA Registry. Circulation 1985, 71, 90–97. [Google Scholar] [CrossRef] [Green Version]
- Kelsey, S.F.; James, M.; Holubkov, A.L.; Holubkov, R.; Cowley, M.J.; Detre, K.M. Results of percutaneous transluminal coronary angioplasty in women. 1985-1986 National Heart, Lung, and Blood Institute’s Coronary Angioplasty Registry. Circulation 1993, 87, 720–727. [Google Scholar] [CrossRef] [Green Version]
- Lansky, A.J.; Costa, R.A.; Mooney, M.; Midei, M.G.; Lui, H.K.; Strickland, W.; Mehran, R.; Leon, M.B.; Russell, M.E.; Ellis, S.G.; et al. Gender-based outcomes after paclitaxel-eluting stent implantation in patients with coronary artery disease. J. Am. Coll. Cardiol. 2005, 45, 1180–1185. [Google Scholar] [CrossRef] [Green Version]
- Solinas, E.; Nikolsky, E.; Lansky, A.J.; Kirtane, A.J.; Morice, M.C.; Popma, J.J.; Schofer, J.; Schampaert, E.; Pucelikova, T.; Aoki, J.; et al. Gender-specific outcomes after sirolimus-eluting stent implantation. J. Am. Coll. Cardiol. 2007, 50, 2111–2116. [Google Scholar] [CrossRef] [Green Version]
- Mikhail, G.W.; Gerber, R.T.; Cox, D.A.; Ellis, S.G.; Lasala, J.M.; Ormiston, J.A.; Stone, G.W.; Turco, M.A.; Joshi, A.A.; Baim, D.S.; et al. Influence of sex on long-term outcomes after percutaneous coronary intervention with the paclitaxel-eluting coronary stent: Results of the “TAXUS Woman” analysis. JACC Cardiovasc. Interv. 2010, 3, 1250–1259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morice, M.C.; Serruys, P.W.; Kappetein, A.P.; Feldman, T.E.; Ståhle, E.; Colombo, A.; Mack, M.J.; Holmes, D.R.; Torracca, L.; van Es, G.A.; et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation 2010, 121, 2645–2653. [Google Scholar] [PubMed] [Green Version]
- Park, S.J.; Kim, Y.H.; Park, D.W.; Yun, S.C.; Ahn, J.M.; Song, H.G.; Lee, J.Y.; Kim, W.J.; Kang, S.J.; Lee, S.W.; et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N. Engl. J. Med. 2011, 364, 1718–1727. [Google Scholar] [CrossRef] [PubMed]
- Kowalewski, M.; Gozdek, M.; Zieliński, K.; Raffa, G.M.; Suwalski, P.; Lorusso, R. Long-term mortality after percutaneous coronary intervention with drug-eluting stents compared with coronary artery bypass grafting for multivessel and left main disease: A meta-analysis. Kardiol. Pol. 2020, 78, 759–761. [Google Scholar] [CrossRef] [PubMed]
- Serruys, P.W.; Morice, M.C.; Kappetein, A.P.; Colombo, A.; Holmes, D.R.; Mack, M.J.; Ståhle, E.; Feldman, T.E.; van den Brand, M.; Bass, E.J.; et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 2009, 360, 961–972. [Google Scholar] [CrossRef]
- Serruys, P.W.; Cavalcante, R.; Collet, C.; Kappetein, A.P.; Sabik, J.F., 3rd; Banning, A.P.; Taggart, D.P.; Sabaté, M.; Pomar, J.; Boonstra, P.W.; et al. Outcomes After Coronary Stenting or Bypass Surgery for Men and Women With Unprotected Left Main Disease: The EXCEL Trial. JACC Cardiovasc. Interv. 2018, 11, 1234–1243. [Google Scholar] [CrossRef]
- Sheiban, I.; Spina, L.C.; Cavallero, E.; Biondi-Zoccai, G.; Colombo, F.; Palmerini, T.; Marzocchi, A.; Tamburino, C.; Margheri, M.; Vecchi, G.; et al. Sex-related differences in patients undergoing percutaneous unprotected left main stenting. EuroIntervention 2010, 5, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Yang, Z.; Yuan, Y.; Xu, Z. Sex difference among patients with unprotected left main coronary artery disease undergoing percutaneous coronary intervention in northern China. Heart Surg. Forum 2018, 21, E322–E325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trabattoni, D.; Teruzzi, G.; Montorsi, P.; Fabbiocchi, F.; Gili, S.; Calligaris, G.; Grancini, L.; Galli, S.; Ravagnani, P.; Bartorelli, A. Comparison of the Effectiveness of Percutaneous Intervention of the Left-Main Coronary Artery With Everolimus-Eluting Stents in Women -Vs- Men. Am. J. Cardiol. 2019, 124, 1357–1362. [Google Scholar] [CrossRef] [PubMed]
- Shin, E.S.; Lee, C.W.; Ahn, J.M.; Lee, P.H.; Chang, M.; Kim, M.J.; Yoon, S.H.; Park, D.W.; Kang, S.J.; Lee, S.W.; et al. Sex differences in left main coronary artery stenting: Different characteristics but similar outcomes for women compared with men. Int. J. Cardiol. 2018, 253, 50–54. [Google Scholar] [CrossRef] [PubMed]
- Takagi, K.; Chieffo, A.; Shannon, J.; Naganuma, T.; Tahara, S.; Fujino, Y.; Latib, A.; Montorfano, M.; Carlino, M.; Kawamoto, H.; et al. Impact of gender on long-term mortality in patients with unprotected left main disease: The Milan and New-Tokyo (MITO) Registry. Cardiovasc. Revascularization Med. 2016, 17, 369–374. [Google Scholar] [CrossRef]
- Thandra, A.; Jhand, A.; Guddeti, R.; Pajjuru, V.; DelCore, M.; Lavie, C.J.; Alla, V.M. Sex differences in clinical outcomes following percutaneous coronary intervention of unprotected left main coronary artery: A systematic review and meta-analysis. Cardiovasc. Revascularization Med. 2020, 31, 30465–30466. [Google Scholar]
- Hogue Jr, C.W.; Barzilai, B.; Pieper, K.S.; Coombs, L.P.; DeLong, E.R.; Kouchoukos, N.T.; Dávila-Román, V.G. Sex differences in neurological outcomes and mortality after cardiac surgery: A society of thoracic surgery national database report. Circulation 2001, 103, 2133–2137. [Google Scholar] [CrossRef] [Green Version]
- Lerner, D.J.; Kannel, W.B. Patterns of coronary heart disease morbidity and mortality in the sexes: A 26-year follow-up of the Framingham population. Am. Heart J. 1986, 111, 383–390. [Google Scholar] [CrossRef]
- Vaccarino, V.; Parsons, L.; Every, N.R.; Barron, H.V.; Krumholz, H.M. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N. Engl. J. Med. 1999, 341, 217–225. [Google Scholar] [CrossRef]
- Farooq, V.; Serruys, P.W.; Bourantas, C.; Vranckx, P.; Diletti, R.; Garcia Garcia, H.M.; Holmes, D.R.; Kappetein, A.P.; Mack, M.; Feldman, T.; et al. Incidence and multivariable correlates of long-term mortality in patients treated with surgical or percutaneous revascularization in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial. Eur. Heart J. 2012, 33, 3105–3113. [Google Scholar] [CrossRef] [PubMed]
- Sotomi, Y.; Collet, C.; Cavalcante, R.; Morel, M.A.; Suwannasom, P.; Farooq, V.; van Gameren, M.; Onuma, Y.; Serruys, P.W. Tools and Techniques—Clinical: SYNTAX score II calculator. EuroIntervention 2016, 12, 120–123. [Google Scholar] [CrossRef]
- Medina, A.; de Lezo, J.S.; Pan, M. Una clasificación simple de las lesiones coronarias en bifurcación [A new classification of coronary bifurcation lesions]. Rev. Esp. Cardiol. 2006, 59, 183. [Google Scholar] [CrossRef] [Green Version]
- Stone, G.W.; Sabik, J.F.; Serruys, P.W.; Simonton, C.A.; Généreux, P.; Puskas, J.; Kandzari, D.E.; Morice, M.C.; Lembo, N.; Brown, W.M., 3rd; et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N. Engl. J. Med. 2016, 375, 2223–2235. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; The Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, N.M.; Mahfouz, A.; Achkar, K.; Rafie, I.M.; Hajar, R. Contrast-induced Nephropathy. Heart Views 2013, 14, 106–116. [Google Scholar] [CrossRef]
- Kovacic, J.C.; Mehran, R.; Karajgikar, R.; Baber, U.; Suleman, J.; Kim, M.C.; Krishnan, P.; Dangas, G.; Sharma, S.K.; Kini, A. Female gender and mortality after percutaneous coronary intervention: Results from a large registry. Catheter. Cardiovasc. Interv. 2012, 80, 514–521. [Google Scholar] [CrossRef]
- O’Connor, G.T.; Morton, J.R.; Diehl, M.J.; Olmstead, E.M.; Coffin, L.H.; Levy, D.G.; Maloney, C.T.; Plume, S.K.; Nugent, W.; Malenka, D.J.; et al. Differences between men and women in hospital mortality associated with coronary artery bypass graft surgery. The Northern New England Cardiovascular Disease Study Group. Circulation 1993, 88, 2104–2110. [Google Scholar] [CrossRef] [Green Version]
- Kwok, C.S.; Kontopantelis, E.; Kunadian, V.; Anderson, S.; Ratib, K.; Sperrin, M.; Zaman, A.; Ludman, P.F.; de Belder, M.A.; Nolan, J.; et al. Effect of access site, gender, and indication on clinical outcomes after percutaneous coronary intervention: Insights from the British Cardiovascular Intervention Society (BCIS). Am. Heart J. 2015, 170, 164–172. [Google Scholar] [CrossRef]
- Mueller, C.; Buerkle, G.; Perruchoud, A.P.; Buettner, H.J. Female sex and risk of contrast nephropathy after percutaneous coronary intervention. Can. J. Cardiol. 2004, 20, 505–509. [Google Scholar]
| Variable | Women n = 130 | Men n = 403 | p-Value |
|---|---|---|---|
| Age (y) | 70.0 ± 9.4 | 67.7 ± 9.2 | 0.006 |
| BMI (kg/m2) | 29.1 ± 4.9 | 28.2 ± 4.4 | 0.052 |
| Hypertension | 118 (90.8%) | 326 (80.9%) | 0.009 |
| Hyperlipidemia | 63 (48.5%) | 202 (50.1%) | 0.742 |
| Chronic kidney disease | 55 (42.3%) | 124 (30.8%) | 0.015 |
| Diabetes | 59 (45.4%) | 137 (34.0%) | 0.019 |
| Stroke/TIA | 7 (5.4%) | 37 (9.2%) | 0.171 |
| COPD | 8 (6.2%) | 35 (8.7%) | 0.357 |
| Peripheral artery disease | 19 (14.6%) | 60 (14.9%) | 0.939 |
| Atrial fibrillation | 16 (12.3%) | 51 (12.7%) | 0.917 |
| Cigarette smoking (current) | 46 (35.4%) | 159 (39.5%) | 0.407 |
| Prior MI | 49 (37.7%) | 211 (52.4%) | 0.004 |
| Prior PCI LAD | 24 (18.5%) | 98 (24.3%) | 0.167 |
| Prior PCI LCx | 12 (9.2%) | 66 (16.4%) | 0.045 |
| Prior PCI RCA | 33 (25.4%) | 130 (32.3%) | 0.139 |
| Prior CABG | 23 (17.7%) | 92 (22.8%) | 0.216 |
| Clinical presentation: | |||
| Stable angina | 78 (60.0%) | 240 (59.6%) | 0.928 |
| Unstable angina | 35 (26.9%) | 107 (26.6%) | 0.933 |
| NSTEMI | 16 (12.3%) | 38 (9.4%) | 0.344 |
| STEMI | 2 (1.5%) | 13 (3.2%) | 0.312 |
| LVEDD (mm) | 47.1 ± 5.9 | 53.1 ± 7.3 | <0.001 |
| LVEF (%) | 53.5 ± 9.4 | 49.5 ± 11.2 | 0.001 |
| EuroScore II | 2.32 ± 1.93 | 2.29 ± 1.87 | 0.826 |
| Syntax Score: | 23.5 ± 9.3 | 24.8 ± 10.2 | 0.301 |
| 0–22 (low) | 63 (48.5%) | 182 (45.2%) | 0.511 |
| 23–32 (intermediate) | 39 (30.0%) | 124 (30.8%) | 0.869 |
| ≥33 (high) | 28 (21.5%) | 94 (23.3%) | 0.673 |
| Variable | Women n = 130 | Men n = 403 | p-Value |
|---|---|---|---|
| LM distal | 102 (78.5%) | 323 (80.1%) | 0.677 |
| LM bifurcation | 84 (64.6%) | 256 (63.5%) | 0.828 |
| LM trifurcation | 10 (7.7%) | 57 (14.1%) | 0.054 |
| LM calcification | 19 (14.6%) | 55 (13.6%) | 0.781 |
| LAD disease (not ostial) | 8 (6.2%) | 34 (8.4%) | 0.401 |
| LCx disease (not ostial) | 9 (6.9%) | 22 (5.5%) | 0.535 |
| Protected LM | 12 (9.2%) | 65 (16.1%) | 0.052 |
| RCA recessive (a) | 8 (6.2%) | 30 (7.4%) | 0.619 |
| RCA with significant stenosis (b) | 20 (15.4%) | 60 (14.9%) | 0.890 |
| RCA total occlusion (c) | 13 (10.0%) | 85 (21.1%) | 0.005 |
| Lack of RCA support (a + b + c) | 41 (31.5%) | 175 (43.4%) | 0.016 |
| CTO of RCA with collateral circulation from LCA | 9 (6.9%) | 55 (13.6%) | 0.040 |
| Extent of diseased vessels: | |||
| LM plus 2-vessel disease | 28 (21.5%) | 109 (27.0%) | 0.211 |
| LM plus 3-vessel disease | 9 (8.3%) | 54 (13.4%) | 0.047 |
| Medina classification: | n = 84 | n = 256 | |
| 1-0-0 | 22 (26.2%) | 84 (32.8%) | 0.256 |
| 1-0-1 | 10 (11.9%) | 35 (13.7%) | 0.678 |
| 1-1-0 | 30 (35.7%) | 76 (29.7%) | 0.301 |
| 1-1-1 | 22 (26.2%) | 61 (23.8%) | 0.662 |
| Variable | Women n = 130 | Men n = 403 | p-Value |
|---|---|---|---|
| PCI success | 129 (99.2%) | 402 (99.8%) | 0.984 |
| Number of stents | 1.82 ± 0.93 | 1.67 ± 0.82 | 0.097 |
| Total length of implanted stents [mm] | 39.7 ± 22.8 | 38.7 ± 22.5 | 0.612 |
| Radiation time [min] | 17.9 ± 8.9 | 17.8 ± 9.6 | 0.647 |
| Radiation dose [mGy] | 1215 ± 812 | 1497 ± 884 | <0.001 |
| Contrast volume [mL] | 242.6 ± 99.9 | 254.9 ± 92.4 | 0.166 |
| Arterial access site | |||
| Radial | 75 (57.7%) | 229 (56.8%) | 0.862 |
| Femoral | 55 (42.3%) | 174 (43.2%) | |
| Stenting LM only | 17 (13.1%) | 47 (11.7%) | 0.666 |
| Stenting LM bifurcation | |||
| One-stent technique | 79 (60.8%) | 278 (69.0%) | 0.083 |
| Two-stent technique | 34 (26.2%) | 78 (19.4%) | 0.098 |
| Two-stent techniques: | n = 34 | n = 78 | |
| Crush | 16 (47.1%) | 30 (38.5%) | 0.395 |
| DK-crush | 2 (5.9%) | 12 (15.4%) | 0.162 |
| Cullote | 1 (2.9%) | 0 (0.0%) | 0.668 |
| T-stenting | 6 (17.6%) | 16 (20.5%) | 0.726 |
| Provisional stenting | 9 (26.5%) | 20 (25.6%) | 0.927 |
| Variable | Women n = 130 | Men n = 403 | p-Value |
|---|---|---|---|
| Myocardial infarction | 9 (6.9%) | 14 (3.5%) | 0.092 |
| In-hospital death | 0 (0.0%) | 2 (0.5%) | 0.984 |
| Stroke | 0 (0.0%) | 1 (0.2%) | 0.551 |
| Tamponade | 0 (0.0%) | 2 (0.5%) | 0.984 |
| Pulmonary edema | 0 (0.0%) | 1 (0.2%) | 0.551 |
| Dissection of aorta | 0 (0.0%) | 1 (0.2%) | 0.551 |
| Perforation of femoral artery | 0 (0.0%) | 2 (0.5%) | 0.984 |
| Contrast-induced nephropathy | 9 (6.9%) | 12 (3.0%) | 0.044 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kałużna-Oleksy, M.; Skorupski, W.J.; Grygier, M.; Araszkiewicz, A.; Skorupski, W.; Grajek, S.; Mitkowski, P.; Pyda, M.; Lesiak, M. A Personalized Approach to Percutaneous Coronary Interventions in the Left Main Coronary Artery—Is the Female Gender Associated with Worse Outcomes? J. Pers. Med. 2021, 11, 581. https://doi.org/10.3390/jpm11060581
Kałużna-Oleksy M, Skorupski WJ, Grygier M, Araszkiewicz A, Skorupski W, Grajek S, Mitkowski P, Pyda M, Lesiak M. A Personalized Approach to Percutaneous Coronary Interventions in the Left Main Coronary Artery—Is the Female Gender Associated with Worse Outcomes? Journal of Personalized Medicine. 2021; 11(6):581. https://doi.org/10.3390/jpm11060581
Chicago/Turabian StyleKałużna-Oleksy, Marta, Wojciech Jan Skorupski, Marek Grygier, Aleksander Araszkiewicz, Włodzimierz Skorupski, Stefan Grajek, Przemysław Mitkowski, Małgorzata Pyda, and Maciej Lesiak. 2021. "A Personalized Approach to Percutaneous Coronary Interventions in the Left Main Coronary Artery—Is the Female Gender Associated with Worse Outcomes?" Journal of Personalized Medicine 11, no. 6: 581. https://doi.org/10.3390/jpm11060581
APA StyleKałużna-Oleksy, M., Skorupski, W. J., Grygier, M., Araszkiewicz, A., Skorupski, W., Grajek, S., Mitkowski, P., Pyda, M., & Lesiak, M. (2021). A Personalized Approach to Percutaneous Coronary Interventions in the Left Main Coronary Artery—Is the Female Gender Associated with Worse Outcomes? Journal of Personalized Medicine, 11(6), 581. https://doi.org/10.3390/jpm11060581









