Personalized Medicine in Parkinson’s Disease: New Options for Advanced Treatments
Abstract
:1. Introduction
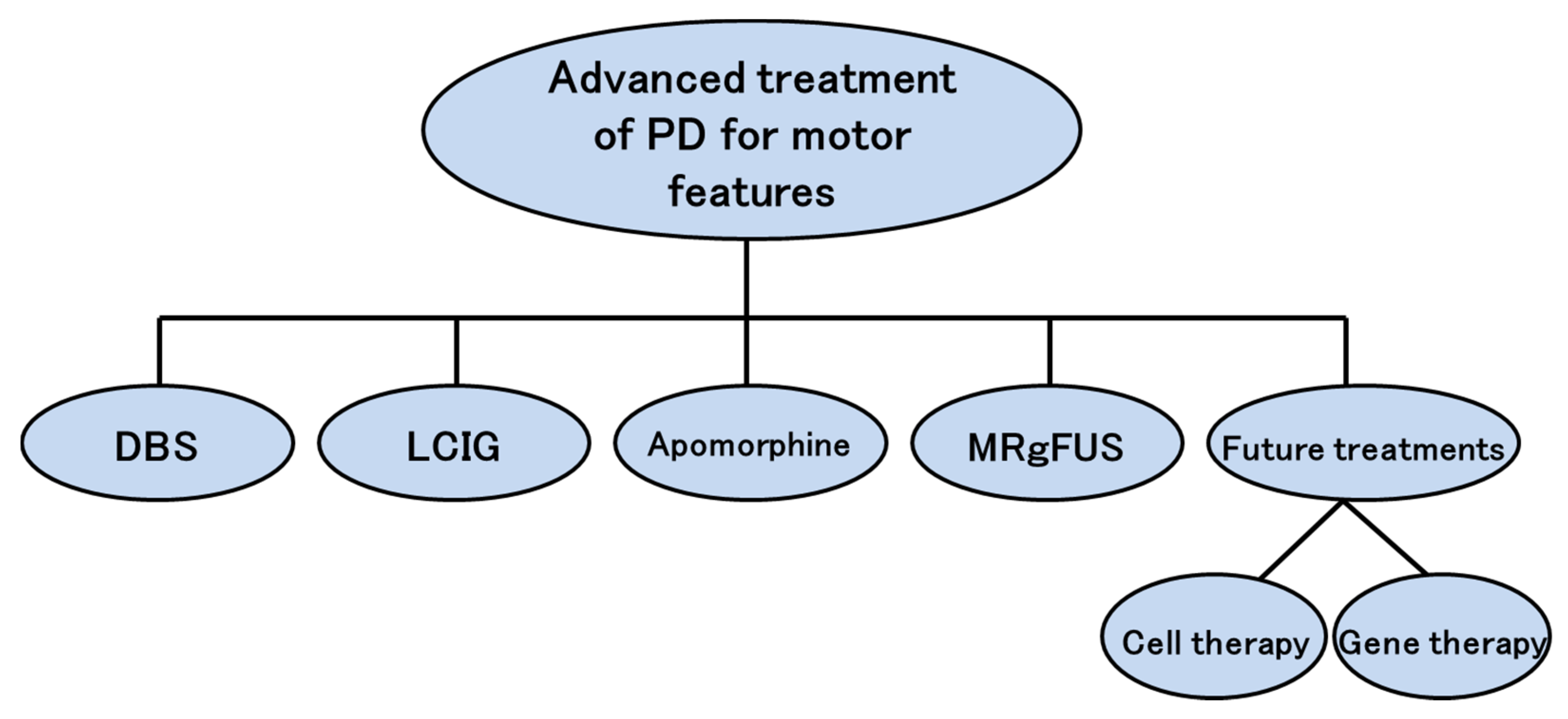
2. Advanced Treatments
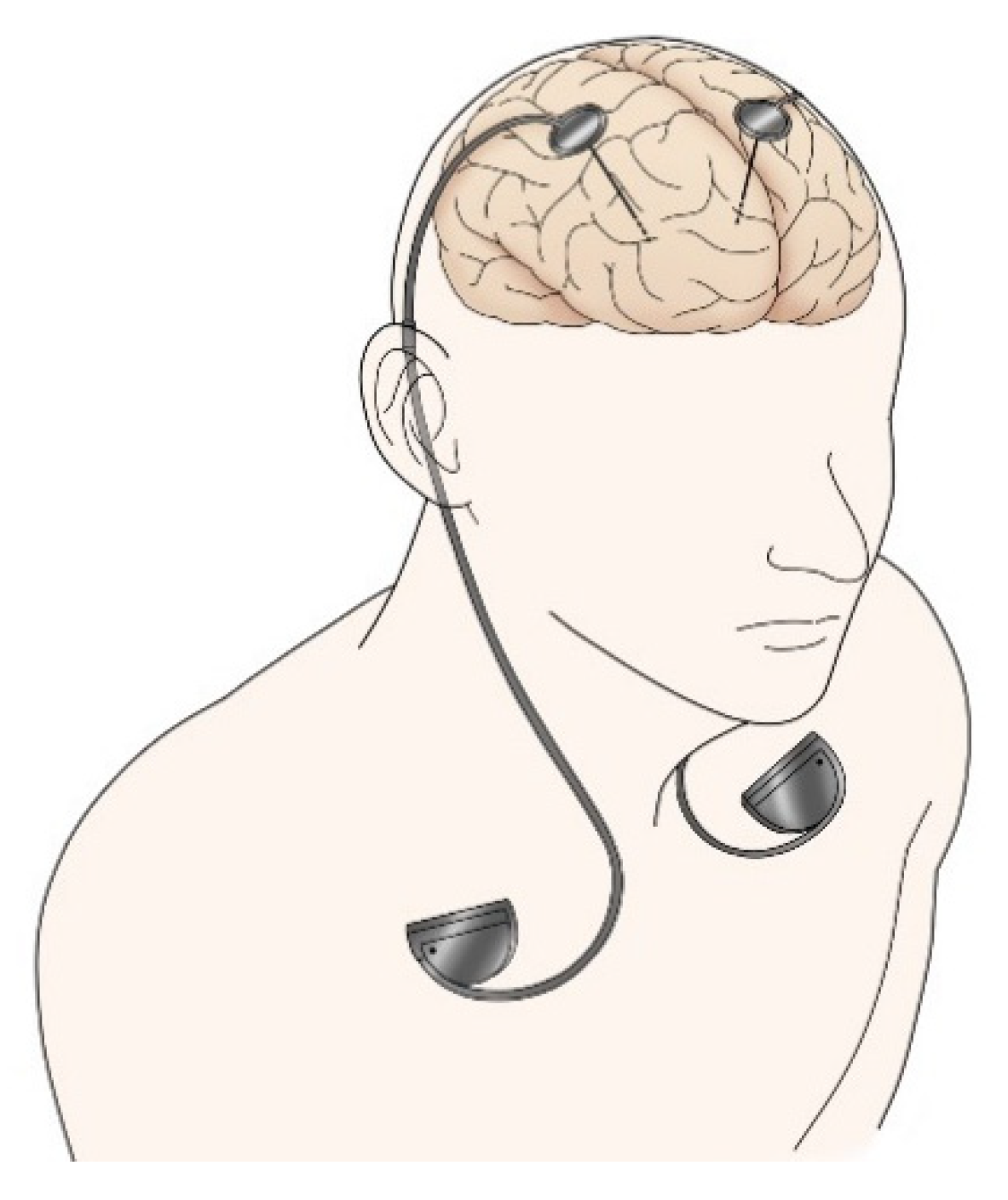
2.1. Deep Brain Stimulation (DBS)
2.2. Levodopa-Carbidopa Intestinal Gel (LCIG)
2.3. Apomorphine
2.4. Ablative Surgery
2.4.1. Radiofrequency Lesioning
2.4.2. Gamma Knife
2.4.3. MR–Guided Focused Ultrasound (MRgFUS)
2.5. Comparison of DBS and LCIG
2.6. Combination Therapy
2.7. Future Surgical Treatments
2.7.1. Cell Therapy
2.7.2. Gene Therapy
3. Evaluation of the Efficacy of Advanced Treatment
4. Team Approach
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Titova, N.; Chaudhuri, K.R. Personalized medicine in Parkinson’s disease: Time to be precise. Mov. Disord. 2017, 32, 1147–1154. [Google Scholar] [CrossRef] [PubMed]
- Jameson, J.L.; Longo, D.L. Precision medicine—Personalized, problematic, and promising. N. Engl. J. Med. 2015, 372, 2229–2234. [Google Scholar] [CrossRef] [Green Version]
- Schneider, S.A.; Alcalay, R.N. Precision medicine in Parkinson’s disease: Emerging treatments for genetic Parkinson’s disease. J. Neurol. 2020, 267, 860–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Juengst, E.; McGowan, M.L.; Fishman, J.R.; Settersten, R.A., Jr. From “Personalized” to “Precision” Medicine: The Ethical and Social Implications of Rhetorical Reform in Genomic Medicine. Hastings Cent. Rep. 2016, 46, 21–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, A.; Chang, H.; Lee, K.J. Action Research on Development and Application of Internet of Things Services in Hospital. Healthc. Inform. Res. 2017, 23, 25–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandres-Ciga, S.; Diez-Fairen, M.; Kim, J.J.; Singleton, A.B. Genetics of Parkinson’s disease: An introspection of its journey towards precision medicine. Neurobiol. Dis. 2020, 137, 104782. [Google Scholar] [CrossRef] [PubMed]
- Gulilat, M.; Lamb, T.; Teft, W.A.; Wang, J.; Dron, J.S.; Robinson, J.F.; Tirona, R.G.; Hegele, R.A.; Kim, R.B.; Schwarz, U.I. Targeted next generation sequencing as a tool for precision medicine. BMC Med. Genom. 2019, 12, 81. [Google Scholar] [CrossRef]
- Titova, N.; Padmakumar, C.; Lewis, S.J.G.; Chaudhuri, K.R. Parkinson’s: A syndrome rather than a disease? J. Neural Transm. 2017, 124, 907–914. [Google Scholar] [CrossRef] [Green Version]
- Gibb, W.R.; Lees, A.J. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 1988, 51, 745–752. [Google Scholar] [CrossRef] [Green Version]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Jankovic, J.; Kapadia, A.S. Functional decline in Parkinson disease. Arch. Neurol. 2001, 58, 1611–1615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fereshtehnejad, S.M.; Zeighami, Y.; Dagher, A.; Postuma, R.B. Clinical criteria for subtyping Parkinson’s disease: Biomarkers and longitudinal progression. Brain 2017, 140, 1959–1976. [Google Scholar] [CrossRef] [PubMed]
- Bloem, B.R.; Marks, W.J., Jr.; Silva de Lima, A.L.; Kuijf, M.L.; van Laar, T.; Jacobs, B.P.F.; Verbeek, M.M.; Helmich, R.C.; van de Warrenburg, B.P.; Evers, L.J.W.; et al. The Personalized Parkinson Project: Examining disease progression through broad biomarkers in early Parkinson’s disease. BMC Neurol. 2019, 19, 160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narabayashi, H.; Okuma, T.; Shikiba, S. Procaine oil blocking of the globus pallidus. AMA Arch. Neurol. Psychiatry 1956, 75, 36–48. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S. The medical treatment of Parkinson disease from James Parkinson to George Cotzias. Mov. Disord. 2015, 30, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, L.V. Brain targets in surgery for Parkinson’s disease. Results of a survey of neurosurgeons. J Neurosurg. 1985, 62, 349–351. [Google Scholar] [CrossRef]
- Laitinen, L.V.; Bergenheim, A.T.; Hariz, M.I. Leksell’s posteroventral pallidotomy in the treatment of Parkinson’s disease. J. Neurosurg. 1992, 76, 53–61. [Google Scholar] [CrossRef] [Green Version]
- Schuepbach, W.M.; Rau, J.; Knudsen, K.; Volkmann, J.; Krack, P.; Timmermann, L.; Hälbig, T.D.; Hesekamp, H.; Navarro, S.M.; Meier, N.; et al. Neurostimulation for Parkinson’s disease with early motor complications. N. Engl. J. Med. 2013, 368, 610–622. [Google Scholar] [CrossRef] [Green Version]
- Fox, S.H.; Katzenschlager, R.; Lim, S.Y.; Barton, B.; de Bie, R.M.A.; Seppi, K.; Coelho, M.; Sampaio, C. Movement Disorder Society. Evidence-Based Medicine Committee. International Parkinson and movement disorder society evidence-based medicine review: Update on treatments for the motor symptoms of Parkinson’s disease. Mov. Disord. 2018, 33, 248–1266. [Google Scholar] [CrossRef]
- Ferreira, J.J.; Katzenschlager, R.; Bloem, B.R.; Bonuccelli, U.; Burn, D.; Deuschl, G.; Dietrichs, E.; Fabbrini, G.; Friedman, A.; Kanovsky, P.; et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson’s disease. Eur. J. Neurol. 2013, 20, 5–15. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Parkinson’s Disease in Adults. NICE Guideline [NG71]. July 2017. Available online: www.nice.org.uk/guidance/ng71 (accessed on 19 July 2017).
- Jost, S.T.; Sauerbier, A.; Visser-Vandewalle, V.; Ashkan, K.; Silverdale, M.; Evans, J.; Loehrer, P.A.; Rizos, A.; Petry-Schmelzer, J.N.; Reker, P.; et al. A prospective, controlled study of non-motor effects of subthalamic stimulation in Parkinson’s disease: Results at the 36-month follow-up. J. Neurol. Neurosurg. Psychiatry 2020, 91, 687–694. [Google Scholar] [CrossRef]
- Antonini, A.; Stoessl, A.J.; Kleinman, L.S.; Skalicky, A.M.; Marshall, T.S.; Sail, K.R.; Onuk, K.; Odin, P.L.A. Developing consensus among movement disorder specialists on clinical indicators for identification and management of advanced Parkinson’s disease: A multi-country Delphi-panel approach. Curr. Med. Res. Opin. 2018, 12, 2063–2073. [Google Scholar] [CrossRef]
- Negida, A.; Elminawy, M.; El Ashal, G.; Essam, A.; Eysa, A.; Abd Elalem Aziz, M. Subthalamic and Pallidal Deep Brain Stimulation for Parkinson’s Disease. Cureus 2018, 10, e2232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, Z.; Ling, Z.; Pan, L.; Xu, X.; Cui, Z.; Liang, S.; Yu, X. Comparison of Efficacy of Deep Brain Stimulation of Different Targets in Parkinson’s Disease: A Network Meta-Analysis. Front. Aging Neurosci. 2019, 11, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, J.W.; Zhang, Y.Q.; Zhang, X.H.; Wang, Y.P.; Li, J.P.; Li, Y.J. Deep Brain Stimulation of Pedunculopontine Nucleus for Postural Instability and Gait Disorder After Parkinson Disease: A Meta-Analysis of Individual Patient Data. World Neurosurg. 2017, 102, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Takahashi, K.; Bloom, L.; Quaynor, S.D.; Xie, T. Effect of Deep Brain Stimulation on Swallowing Function: A Systematic Review. Front. Neurol. 2020, 11, 547. [Google Scholar] [CrossRef]
- Walker, H.C.; Watts, R.L.; Guthrie, S.; Wang, D.; Guthrie, B.L. Bilateral effects of unilateral subthalamic deep brain stimulation on Parkinson’s disease at 1 year. Neurosurgery 2009, 2, 302–309. [Google Scholar] [CrossRef]
- Okun, M.S.; Wu, S.S.; Fayad, S.; Ward, H.; Bowers, D.; Rosado, C.; Bowen, L.; Jacobson, C.; Butson, C.; Foote, K.D. Acute and Chronic Mood and Apathy Outcomes from a randomized study of unilateral STN and GPi DBS. PLoS ONE 2014, 12, e114140. [Google Scholar] [CrossRef] [PubMed]
- Cernera, S.; Eisinger, R.S.; Wong, J.K.; Ho, K.W.D.; Lopes, J.L.; To, K.; Carbunaru, S.; Ramirez-Zamora, A.; Almeida, L.; Foote, K.D.; et al. Long-term Parkinson’s disease quality of life after staged DBS: STN vs GPi and first vs second lead. NPJ. Parkinsons Dis. 2020, 6, 13. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, L.; Hu, W.; Wang, T.; Zhao, Y.; Pan, Y.; Almeida, L.; Ramirez-Zamora, A.; Sun, B.; Li, D. Combined Unilateral Subthalamic Nucleus and Contralateral Globus Pallidus Interna Deep Brain Stimulation for Treatment of Parkinson Disease: A Pilot Study of Symptom-Tailored Stimulation. Neurosurgery 2020, 87, 1139–1147. [Google Scholar]
- Morishita, T.; Higuchi, M.A.; Kobayashi, H.; Abe, H.; Higashi, T.; Inoue, T. A retrospective evaluation of thalamic targeting for tremor deep brain stimulation using high-resolution anatomical imaging with supplementary fiber tractography. J. Neurol. Sci. 2019, 398, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Horn, A.; Reich, M.; Vorwerk, J.; Li, N.; Wenzel, G.; Fang, Q.; Schmitz-Hübsch, T.; Nickl, R.; Kupsch, A.; Volkmann, J.; et al. Connectivity Predicts deep brain stimulation outcome in Parkinson disease. Ann. Neurol. 2017, 82, 67–78. [Google Scholar] [CrossRef]
- Eleopra, R.; Rinaldo, S.; Devigili, G.; Lettieri, C.; Mondani, M.; D’Auria, S.; Piacentino, M.; Pilleri, M. Brain impedance variation of directional leads implanted in subthalamic nuclei of Parkinsonian patients. Clin. Neurophysiol. 2019, 130, 1562–1569. [Google Scholar] [CrossRef]
- Shao, M.M.; Liss, A.; Park, Y.L.; DiMarzio, M.; Prusik, J.; Hobson, E.; Adam, O.; Durphy, J.; Sukul, V.; Danisi, F.; et al. Early Experience With New Generation Deep Brain Stimulation Leads in Parkinson’s Disease and Essential Tremor Patients. Neuromodulation 2020, 23, 537–542. [Google Scholar] [CrossRef]
- Pollo, C.; Kaelin-Lang, A.; Oertel, M.F.; Stieglitz, L.; Taub, E.; Fuhr, P.; Lozano, A.M.; Raabe, A.; Schüpbach, M. Directional deep brain stimulation: An intraoperative double-blind pilot study. Brain 2014, 137, 2015–2026. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Contarino, M.F.; Bour, L.J.; Verhagen, R.; Lourens, M.A.; de Bie, R.M.; van den Munckhof, P.; Schuurman, P.R. Directional steering: A novel approach to deep brain stimulation. Neurology 2014, 83, 1163–1169. [Google Scholar] [CrossRef] [PubMed]
- Steigerwald, F.; Müller, L.; Johannes, S.; Matthies, C.; Volkmann, J. Directional deep brain stimulation of the subthalamic nucleus: A pilot study using a novel neurostimulation device. Mov. Disord. 2016, 31, 1240–1243. [Google Scholar] [CrossRef]
- Dembek, T.A.; Reker, P.; Visser-Vandewalle, V.; Wirths, J.; Treuer, H.; Klehr, M.; Roediger, J.; Dafsari, H.S.; Barbe, M.T.; Timmermann, L. Directional DBS increases side-effect thresholds-A prospective, double-blind trial. Mov. Disord. 2017, 32, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Krüger, M.T.; Avecillas-Chasin, J.M.; Tamber, M.S.; Heran, M.K.S.; Sandhu, M.K.; Polyhronopoulos, N.E.; Sarai, N.; Honey, C.R. Tremor and Quality of Life in Patients With Advanced Essential Tremor Before and After Replacing Their Standard Deep Brain Stimulation With a Directional System. Neuromodulation 2021, 24, 353–360. [Google Scholar] [CrossRef]
- Meidahl, A.C.; Tinkhauser, G.; Herz, D.M.; Cagnan, H.; Debarros, J.; Brown, P. Adaptive Deep Brain Stimulation for Movement Disorders: The Long Road to Clinical Therapy. Mov. Disord. 2017, 32, 810–819. [Google Scholar] [CrossRef]
- Little, S.; Pogosyan, A.; Neal, S.; Zavala, B.; Zrinzo, L.; Hariz, M.; Foltynie, T.; Limousin, P.; Ashkan, K.; FitzGerald, J.; et al. Adaptive deep brain stimulation in advanced Parkinson disease. Ann. Neurol. 2013, 74, 449–457. [Google Scholar] [CrossRef] [Green Version]
- Jia, F.; Wagle Shukla, A.; Hu, W.; Almeida, L.; Holanda, V.; Zhang, J.; Meng, F.; Okun, M.S.; Li, L. Deep Brain Stimulation at Variable Frequency to Improve Motor Outcomes in Parkinson’s Disease. Mov. Disord. Clin. Pract. 2018, 5, 538–541. [Google Scholar] [CrossRef] [Green Version]
- Enatsu, R.; Kitagawa, M.; Morishita, T.; Sasagawa, A.; Kuribara, T.; Hirano, T.; Arihara, M.; Mikami, T.; Mikuni, N. Effect of Cycling Thalamosubthalamic Stimulation on Tremor Habituation and Rebound in Parkinson Disease. World Neurosurg. 2020, 144, 64–67. [Google Scholar] [CrossRef]
- Watanabe, H.; Sano, H.; Chiken, S.; Kobayashi, K.; Fukata, Y.; Fukata, M.; Mushiake, H.; Nambu, A. Forelimb movements evoked by optogenetic stimulation of the macaque motor cortex. Nat. Commun. 2020, 11, 3253. [Google Scholar] [CrossRef]
- Nimpf, S.; Keays, D.A. Is magnetogenetics the new optogenetics? EMBO J. 2017, 36, 1643–1646. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Meng, W.; Ren, Z.; Li, B.; Zhu, T.; Chen, H.; Wang, Z.; He, B.; Zhao, D.; Jiang, H. Ultrasonic Neuromodulation and Sonogenetics: A New Era for Neural Modulation. Front. Physiol. 2020, 11, 787. [Google Scholar] [CrossRef] [PubMed]
- Politis, M.; Sauerbier, A.; Loane, C.; Pavese, N.; Martin, A.; Corcoran, B.; Brooks, D.J.; Ray-Chaudhuri, K.; Piccini, P. Sustained striatal dopamine levels following intestinal levodopa infusions in Parkinson’s disease patients. Mov. Disord. 2017, 32, 235–240. [Google Scholar] [CrossRef]
- Antonini, A.; Poewe, W.; Chaudhuri, K.R.; Jech, R.; Pickut, B.; Pirtošek, Z.; Szasz, J.; Valldeoriola, F.; Winkler, C.; Bergmann, L.; et al. Levodopa-carbidopa intestinal gel in advanced Parkinson’s: Final results of the GLORIA registry. Parkinsonism Relat. Disord. 2017, 45, 13–20. [Google Scholar] [CrossRef] [Green Version]
- Zibetti, M.; Angrisano, S.; Dematteis, F.; Artusi, C.A.; Romagnolo, A.; Merola, A.; Lopiano, L. Effects of intestinal Levodopa infusion on freezing of gait in Parkinson disease. J. Neurol. Sci. 2018, 385, 105–108. [Google Scholar] [CrossRef] [PubMed]
- Valldeoriola, F.; Santacruz, P.; Ríos, J.; Compta, Y.; Rumià, J.; Muñoz, J.E.; Martí, M.J.; Tolosa, E. l-Dopa/carbidopa intestinal gel and subthalamic nucleus stimulation: Effects on cognition and behavior. Brain Behav. 2017, 7, e00848. [Google Scholar] [CrossRef] [Green Version]
- Catalan, M.J.; Molina-Arjona, J.A.; Mir, P.; Cubo, E.; Arbelo, J.M.; Martinez-Martin, P.; EDIS Study Group. Improvement of impulse control disorders associated with levodopa-carbidopa intestinal gel treatment in advanced Parkinson’s disease. J. Neurol. 2018, 265, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Olanow, C.W.; Kieburtz, K.; Odin, P.; Espay, A.J.; Standaert, D.G.; Fernandez, H.H.; Vanagunas, A.; Othman, A.A.; Widnell, K.L.; Robieson, W.Z.; et al. Continuous intrajejunal infusion of levodopa-carbidopa intestinal gel for patients with advanced Parkinson’s disease: A randomised, controlled, double-blind, double-dummy study. Lancet Neurol. 2014, 13, 141–149. [Google Scholar] [CrossRef] [Green Version]
- Fabbri, M.; Zibetti, M.; Beccaria, L.; Merola, A.; Romagnolo, A.; Montanaro, E.; Ferreira, J.J.; Palermo, S.; Lopiano, L. Levodopa/carbidopa intestinal gel infusion and weight loss in Parkinson’s disease. Eur. J. Neurol. 2019, 26, 490–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nose, K.; Fujioka, S.; Umemoto, G.; Yamashita, K.; Shiwaku, H.; Hayashi, Y.; Mishima, T.; Fukae, J.; Hasegawa, S.; Tsuboi, Y. Acute cholecystitis induced by surgery for levodopa-carbidopa intestinal gel therapy: Possible relationship to pre-existing gallstones. Parkinsonism Relat. Disord. 2018, 54, 107–109. [Google Scholar] [CrossRef]
- Merola, A.; Romagnolo, A.; Zibetti, M.; Bernardini, A.; Cocito, D.; Lopiano, L. Peripheral neuropathy associated with levodopa-carbidopa intestinal infusion: A long-term prospective assessment. Eur. J. Neurol. 2016, 23, 501–509. [Google Scholar] [CrossRef]
- Pessoa, R.R.; Moro, A.; Munhoz, R.P.; Teive, H.A.G.; Lees, A.J. Apomorphine in the treatment of Parkinson’s disease: A review. Arq. Neuropsiquiatr. 2018, 76, 840–848. [Google Scholar] [CrossRef]
- Ray Chaudhuri, K.; Qamar, M.A.; Rajah, T.; Loehrer, P.; Sauerbier, A.; Odin, P.; Jenner, P. Non-oral dopaminergic therapies for Parkinson’s disease: Current treatments and the future. NPJ. Parkinsons Dis. 2016, 2, 16023. [Google Scholar] [CrossRef] [Green Version]
- Katzenschlager, R.; Poewe, W.; Rascol, O.; Trenkwalder, C.; Deuschl, G.; Chaudhuri, K.R.; Henriksen, T.; van Laar, T.; Spivey, K.; Vel, S.; et al. Apomorphine subcutaneous infusion in patients with Parkinson’s disease with persistent motor fluctuations (TOLEDO): A multicentre, double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2018, 17, 749–759. [Google Scholar] [CrossRef]
- Tasker, R.R. Deep brain stimulation is preferable to thalamotomy for tremor suppression. Surg. Neurol. 1998, 49, 145–153. [Google Scholar] [CrossRef]
- Schreglmann, S.R.; Krauss, J.K.; Chang, J.W.; Martin, E.; Werner, B.; Bauer, R.; Hägele-Link, S.; Bhatia, K.P.; Kägi, G. Functional lesional neurosurgery for tremor: back to the future? J. Neurol. Neurosurg. Psychiatry 2018, 89, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Kapadia, A.N.; Elias, G.J.B.; Boutet, A.; Germann, J.; Pancholi, A.; Chu, P.; Zhong, J.; Fasano, A.; Munhoz, R.; Chow, C.; et al. Multimodal MRI for MRgFUS in essential tremor: Post-treatment radiological markers of clinical outcome. J. Neurol. Neurosurg. Psychiatry 2020, 91, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, Y.; Matsuda, S.; Serizawa, T. Gamma knife radiosurgery in movement disorders: Indications and limitations. Mov. Disord. 2017, 32, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Cahan, L.D.; Young, R.F.; Li, F. Radiosurgical Pallidotomy for Parkinson’s Disease. Prog. Neurol. Surg. 2018, 33, 149–157. [Google Scholar] [PubMed]
- Drummond, P.S.; Pourfar, M.H.; Hill, T.C.; Mogilner, A.Y.; Kondziolka, D.S. Subthalamic Gamma Knife Radiosurgery in Parkinson’s Disease: A Cautionary Tale. Stereotact. Funct. Neurosurg. 2020, 98, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Giordano, M.; Caccavella, V.M.; Zaed, I.; Foglia Manzillo, L.; Montano, N.; Olivi, A.; Polli, F.M. Comparison between deep brain stimulation and magnetic resonance-guided focused ultrasound in the treatment of essential tremor: A systematic review and pooled analysis of functional outcomes. J. Neurol. Neurosurg. Psychiatry 2020, 91, 1270–1278. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Fernández, R.; Máñez-Miró, J.U.; Rodríguez-Rojas, R.; Del Álamo, M.; Shah, B.B.; Hernández-Fernández, F.; Pineda-Pardo, J.A.; Monje, M.H.G.; Fernández-Rodríguez, B.; Sperling, S.A.; et al. Randomized Trial of Focused Ultrasound Subthalamotomy for Parkinson’s Disease. N. Engl. J. Med. 2020, 383, 2501–2513. [Google Scholar] [CrossRef]
- Alvarez, L.; Macias, R.; Guridi, J.; Lopez, G.; Alvarez, E.; Maragoto, C.; Teijeiro, J.; Torres, A.; Pavon, N.; Rodriguez-Oroz, M.C.; et al. Dorsal subthalamotomy for Parkinson’s disease. Mov. Disord. 2001, 16, 72–78. [Google Scholar] [CrossRef]
- Bond, A.E.; Shah, B.B.; Huss, D.S.; Dallapiazza, R.F.; Warren, A.; Harrison, M.B.; Sperling, S.A.; Wang, X.Q.; Gwinn, R.; Witt, J.; et al. Safety and Efficacy of Focused Ultrasound Thalamotomy for Patients With Medication-Refractory, Tremor-Dominant Parkinson Disease A Randomized Clinical Trial. JAMA Neurol. 2017, 74, 1412–1418. [Google Scholar] [CrossRef]
- Gallay, M.N.; Moser, D.; Rossi, F.; Magara, A.E.; Strasser, M.; Bühler, R.; Kowalski, M.; Pourtehrani, P.; Dragalina, C.; Federau, C.; et al. MRgFUS Pallidothalamic Tractotomy for Chronic Therapy-Resistant Parkinson’s Disease in 51 Consecutive Patients: Single Center Experience. Front. Surg. 2020, 6, 76. [Google Scholar] [CrossRef] [Green Version]
- Mahajan, U.V.; Ravikumar, V.K.; Kumar, K.K.; Ku, S.; Ojukwu, D.I.; Kilbane, C.; Ghanouni, P.; Rosenow, J.M.; Stein, S.C.; Halpern, C.H. Bilateral deep brain stimulation is the procedure to beat for advanced Parkinson Disease: A meta-analytic, cost-effective threshold analysis for focused ultra-sound. Neurosurgery 2021, 88, 487–496. [Google Scholar] [CrossRef]
- Liu, X.D.; Bao, Y.; Liu, G.J. Comparison Between Levodopa-Carbidopa Intestinal Gel Infusion and Subthalamic Nucleus Deep-Brain Stimulation for Advanced Parkinson’s Disease: A Systematic Review and Meta-Analysis. Front. Neurol. 2019, 10, 934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dafsari, H.S.; Martinez-Martin, P.; Rizos, A.; Trost, M.; Dos Santos Ghilardi, M.G.; Reddy, P.; Sauerbier, A.; Petry-Schmelzer, J.N.; Kramberger, M.; Borgemeester, R.W.K.; et al. EuroInf 2: Subthalamic stimulation, apomorphine, and levodopa infusion in Parkinson’s disease. Mov. Disord. 2019, 34, 353–365. [Google Scholar] [CrossRef] [Green Version]
- Elkouzi, A.; Ramirez-Zamora, A.; Zeilman, P.; Barabas, M.; Eisinger, R.S.; Malaty, I.A.; Okun, M.S.; Almeida, L. Rescue levodopa-carbidopa intestinal gel (LCIG) therapy in Parkinson’s disease patients with suboptimal response to deep brain stimulation. Ann. Clin. Transl. Neurol. 2019, 10, 1989–1995. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barker, R.A.; Barrett, J.; Mason, S.L.; Björklund, A.F. Fetal dopaminergic transplantation trials and the future of neural grafting in Parkinson’s disease. Lancet Neurol. 2013, 12, 84–91. [Google Scholar] [CrossRef]
- Barker, R.A.; Drouin-Ouellet, J.; Parmar, M. Cell–based therapies for Parkinson disease—Past insights and future potential. Nat. Rev. Neurol. 2015, 11, 492–503. [Google Scholar] [CrossRef]
- Kikuchi, T.; Morizane, A.; Doi, D.; Magotani, H.; Onoe, H.; Hayashi, T.; Mizuma, H.; Takara, S.; Takahashi, R.; Inoue, H.; et al. Human iPS cell-derived dopaminergic neurons function in a primate Parkinson’s disease model. Nature 2017, 548, 592–596. [Google Scholar] [CrossRef]
- UMIN. Kyoto Trial to Evaluate the Safety and Efficacy of iPSC-Derived Dopaminergic Progenitors in the Treatment of Parkinson’s Disease. Available online: https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000038278 (accessed on 21 December 2018).
- Schweitzer, J.S.; Song, B.; Herrington, T.M.; Park, T.Y.; Lee, N.; Ko, S.; Jeon, J.; Cha, Y.; Kim, K.; Li, Q.; et al. Personalized iPSC-Derived Dopamine Progenitor Cells for Parkinson’s Disease. N. Engl. J. Med. 2020, 382, 1926–1932. [Google Scholar] [CrossRef]
- Torikoshi, S.; Morizane, A.; Shimogawa, T.; Samata, B.; Miyamoto, S.; Takahashi, J. Exercise Promotes Neurite Extensions from Grafted Dopaminergic Neurons in the Direction of the Dorsolateral Striatum in Parkinson’s Disease Model Rats. J. Parkinsons Dis. 2020, 10, 511–521. [Google Scholar] [CrossRef] [Green Version]
- Muramatsu, S.; Fujimoto, K.; Kato, S.; Mizukami, H.; Asari, S.; Ikeguchi, K.; Kawakami, T.; Urabe, M.; Kume, A.; Sato, T.; et al. A phase I study of aromatic L-amino acid decarboxylase gene therapy for Parkinson’s disease. Mol. Ther. 2010, 18, 1731–1735. [Google Scholar] [CrossRef] [Green Version]
- Christine, C.W.; Starr, P.A.; Larson, P.S.; Eberling, J.L.; Jagust, W.J.; Hawkins, R.A.; VanBrocklin, H.F.; Wright, J.F.; Bankiewicz, K.S.; Aminoff, M.J. Safety and tolerability of putaminal AADC gene therapy for Parkinson disease. Neurology 2009, 73, 1662–1669. [Google Scholar] [CrossRef] [Green Version]
- Christine, C.W.; Bankiewicz, K.S.; Van Laar, A.D.; Richardson, R.M.; Ravina, B.; Kells, A.P.; Boot, B.; Martin, A.J.; Nutt, J.; Thompson, M.E.; et al. Magnetic resonance imaging-guided phase 1 trial of putaminal AADC gene therapy for Parkinson’s disease. Ann. Neurol. 2019, 85, 704–714. [Google Scholar] [CrossRef] [Green Version]
- Palfi, S.; Gurruchaga, J.M.; Lepetit, H.; Howard, K.; Ralph, G.S.; Mason, S.; Gouello, G.; Domenech, P.; Buttery, P.C.; Hantraye, P.; et al. Long-Term Follow-Up of a Phase I/II Study of ProSavin, a Lentiviral Vector Gene Therapy for Parkinson’s Disease. Hum. Gene Ther. Clin. Dev. 2018, 29, 148–155. [Google Scholar] [CrossRef]
- Marks, W.J., Jr.; Bartus, R.T.; Siffert, J.; Davis, C.S.; Lozano, A.; Boulis, N.; Vitek, J.; Stacy, M.; Turner, D.; Verhagen, L.; et al. Gene delivery of AAV2-neurturin for Parkinson’s disease: A double-blind, randomised, controlled trial. Lancet Neurol. 2010, 9, 1164–1172. [Google Scholar] [CrossRef]
- Niethammer, M.; Tang, C.C.; LeWitt, P.A.; Rezai, A.R.; Leehey, M.A.; Ojemann, S.G.; Flaherty, A.W.; Eskandar, E.N.; Kostyk, S.K.; Sarkar, A.; et al. Long-term follow-up of a randomized AAV2- GAD gene therapy trial for Parkinson’s disease. JCI Insight 2017, 2, e90133. [Google Scholar] [CrossRef] [Green Version]
- Elsayed, G.A.; Menendez, J.Y.; Tabibian, B.E.; Chagoya, G.; Omar, N.B.; Zeiger, E.; Walters, B.C.; Walker, H.; Guthrie, B.L. Patient Satisfaction in Surgery for Parkinson’s Disease: A Systematic Review of the Literature. Cureus 2019, 11, e4316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skorvanek, M.; Martinez-Martin, P.; Kovacs, N.; Zezula, I.; Rodriguez-Violante, M.; Corvol, J.C.; Taba, P.; Seppi, K.; Levin, O.; Schrag, A.; et al. Relationship between the MDS-UPDRS and Quality of Life: A large multicenter study of 3206 patients. Parkinsonism Relat. Disord. 2018, 52, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Neff, C.; Wang, M.C.; Martel, H. Using the PDQ-39 in routine care for Parkinson’s disease. Parkinsonism Relat. Disord. 2018, 53, 105–107. [Google Scholar] [CrossRef] [PubMed]
- Kurihara, K.; Nakagawa, R.; Ishido, M.; Yoshinaga, Y.; Watanabe, J.; Hayashi, Y.; Mishima, T.; Fujioka, S.; Tsuboi, Y. Impact of motor and nonmotor symptoms in Parkinson disease for the quality of life: The Japanese Quality-of-Life Survey of Parkinson Disease (JAQPAD) study. J. Neurol. Sci. 2020, 419, 117172. [Google Scholar] [CrossRef] [PubMed]
- Onozawa, R.; Tsugawa, J.; Tsuboi, Y.; Fukae, J.; Mishima, T.; Fujioka, S. The impact of early morning off in Parkinson’s disease on patient quality of life and caregiver burden. J. Neurol. Sci. 2016, 364, 1–5. [Google Scholar] [CrossRef]
- Radder, D.L.M.; Nonnekes, J.; van Nimwegen, M.; Eggers, C.; Abbruzzese, G.; Alves, G.; Browner, N.; Chaudhuri, K.R.; Ebersbach, G.; Ferreira, J.J.; et al. Recommendations for the Organization of Multidisciplinary Clinical Care Teams in Parkinson’s Disease. J. Parkinsons Dis. 2020, 10, 1087–1098. [Google Scholar] [CrossRef]
- Higuchi, M.A.; Martinez-Ramirez, D.; Morita, H.; Topiol, D.; Bowers, D.; Ward, H.; Warren, L.; DeFranco, M.; Hicks, J.A.; Hegland, K.W.; et al. Interdisciplinary Parkinson’s Disease Deep Brain Stimulation Screening and the Relationship to Unintended Hospitalizations and Quality of Life. PLoS ONE 2016, 11, e0153785. [Google Scholar] [CrossRef] [PubMed]
- Timpka, J.; Nitu, B.; Datieva, V.; Odin, P.; Antonini, A. Device-Aided Treatment Strategies in Advanced Parkinson’s Disease. Int. Rev. Neurobiol. 2017, 132, 453–474. [Google Scholar] [PubMed]
- Bhidayasiri, R.; Virameteekul, S.; Kim, J.M.; Pal, P.K.; Chung, S.J. COVID-19: An Early Review of Its Global Impact and Considerations for Parkinson’s Disease Patient Care. J. Mov. Disord. 2020, 13, 105–114. [Google Scholar] [CrossRef]
- Fasano, A.; Antonini, A.; Katzenschlager, R.; Krack, P.; Odin, P.; Evans, A.H.; Foltynie, T.; Volkmann, J.; Merello, M. Management of Advanced Therapies in Parkinson’s Disease Patients in Times of Humanitarian Crisis: The COVID-19 Experience. Mov. Disord. Clin. Pract. 2020, 7, 361–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papa, S.M.; Brundin, P.; Fung, V.S.C.; Kang, U.J.; Burn, D.J.; Colosimo, C.; Chiang, H.L.; Alcalay, R.N.; Trenkwalder, C.; MDS-Scientific Issues Committee. Impact of the COVID-19 Pandemic on Parkinson’s Disease and Movement Disorders. Mov. Disord. 2020, 35, 711–715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurihara, K.; Nakagawa, K.; Inoue, K.; Yamamoto, S.; Mishima, T.; Fujioka, S.; Ouma, S.; Tsuboi, Y. Attitudes toward telemedicine of patients with Parkinson’s disease during the COVID-19 pandemic. Neurol. Clin. Neurosci. 2021, 9, 77–82. [Google Scholar] [CrossRef]
- Jitkritsadakul, O.; Rajalingam, R.; Toenjes, C.; Munhoz, R.P.; Fasano, A. Tele-health for patients with deep brain stimulation: The experience of the Ontario Telemedicine Network. Mov. Disord. 2018, 33, 491–492. [Google Scholar] [CrossRef]
- Willows, T.; Dizdar, N.; Nyholm, D.; Widner, H.; Grenholm, P.; Schmiauke, U.; Urbom, A.; Growth, K.; Larsson, J.; Permert, J.; et al. Initiation of Levodopa-Carbidopa Intestinal Gel Infusion Using Telemedicine (Video Communication System) Facilitates Efficient and Well-Accepted Home Titration in Patients with Advanced Parkinson’s Disease. J. Parkinsons Dis. 2017, 7, 719–728. [Google Scholar] [CrossRef] [Green Version]



| DBS | LCIG | Apomorphine | |
|---|---|---|---|
| Indication | Motor complications (especially dyskinesia) | Motor complications | Motor complications (especially motor fluctuations) |
| Advantages | Dopaminergic medication reduction | No age limit | Minimally invasive procedures |
| Disadvantages | Invasive procedures | Requires caregivers to handle devices | Requires caregivers to handle devices |
| Adverse effects | Psychiatric and cognitive changes | Tube trouble | Skin reaction or trouble |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mishima, T.; Fujioka, S.; Morishita, T.; Inoue, T.; Tsuboi, Y. Personalized Medicine in Parkinson’s Disease: New Options for Advanced Treatments. J. Pers. Med. 2021, 11, 650. https://doi.org/10.3390/jpm11070650
Mishima T, Fujioka S, Morishita T, Inoue T, Tsuboi Y. Personalized Medicine in Parkinson’s Disease: New Options for Advanced Treatments. Journal of Personalized Medicine. 2021; 11(7):650. https://doi.org/10.3390/jpm11070650
Chicago/Turabian StyleMishima, Takayasu, Shinsuke Fujioka, Takashi Morishita, Tooru Inoue, and Yoshio Tsuboi. 2021. "Personalized Medicine in Parkinson’s Disease: New Options for Advanced Treatments" Journal of Personalized Medicine 11, no. 7: 650. https://doi.org/10.3390/jpm11070650







