Pros and Cons for Automated Breast Ultrasound (ABUS): A Narrative Review
Abstract
:1. Introduction
2. Pros regarding ABUS
2.1. Screening
ABUS Associated with Full-Field Digital Mammography (FFDM)
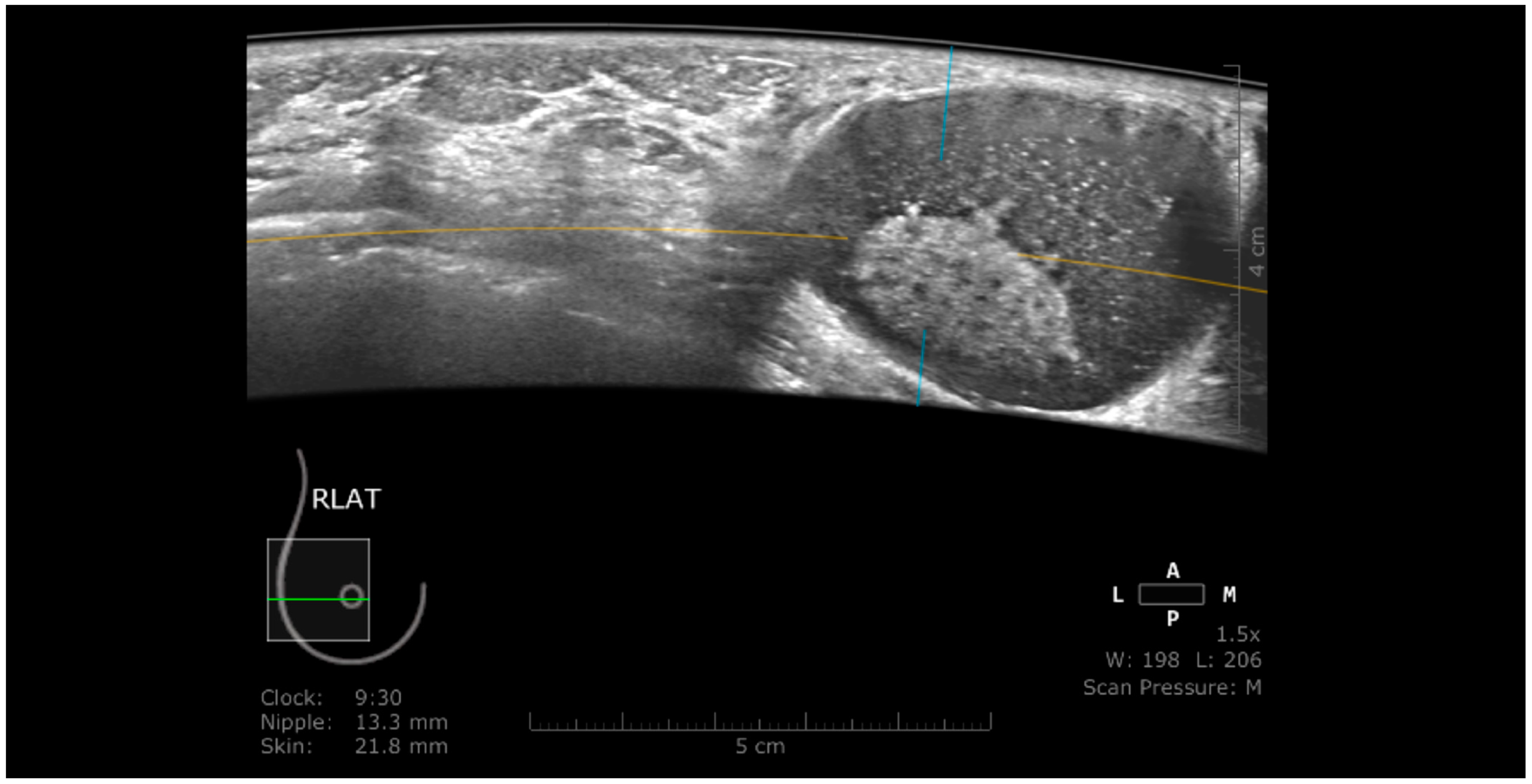
2.2. Technique and Breast Cancer Detection
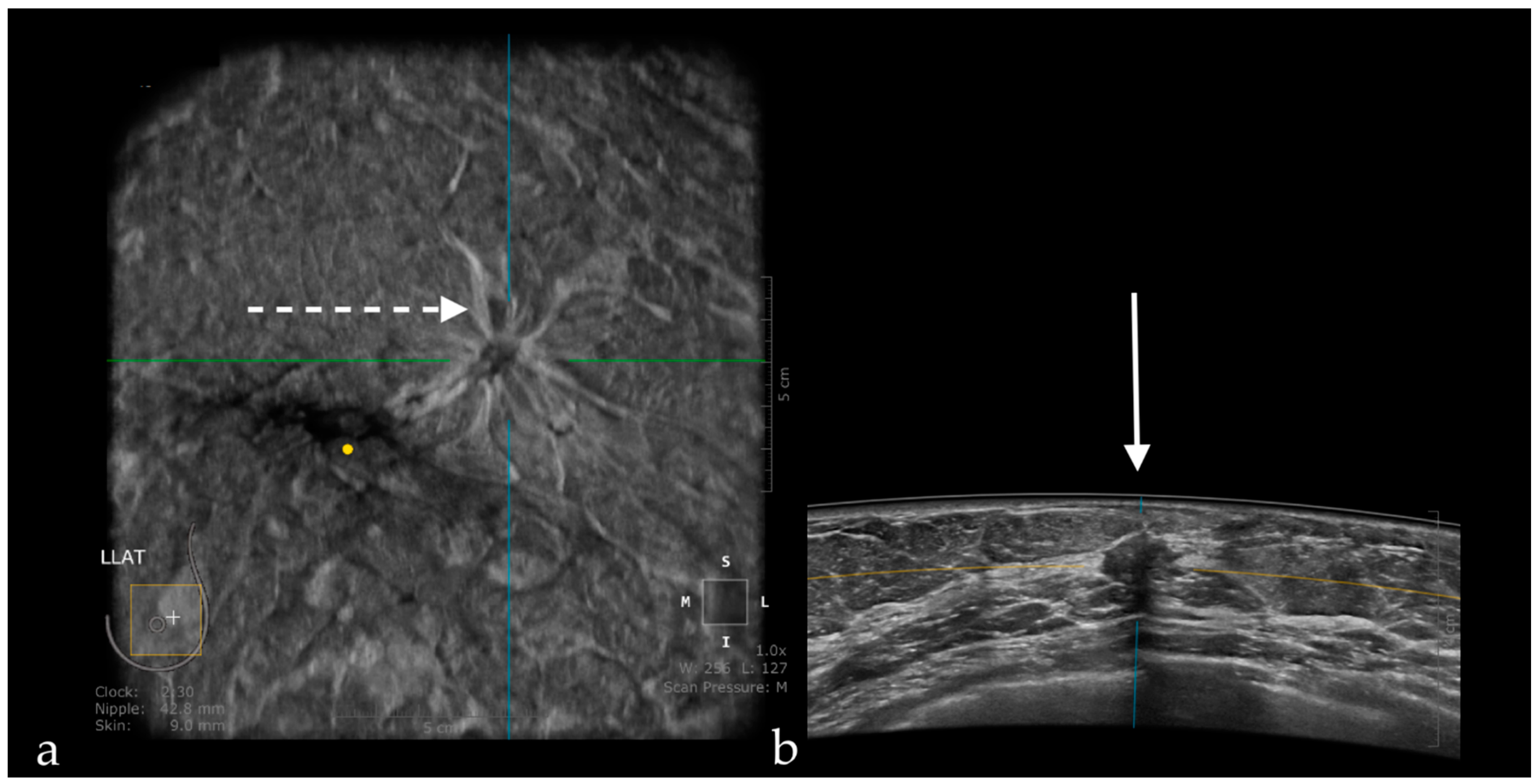
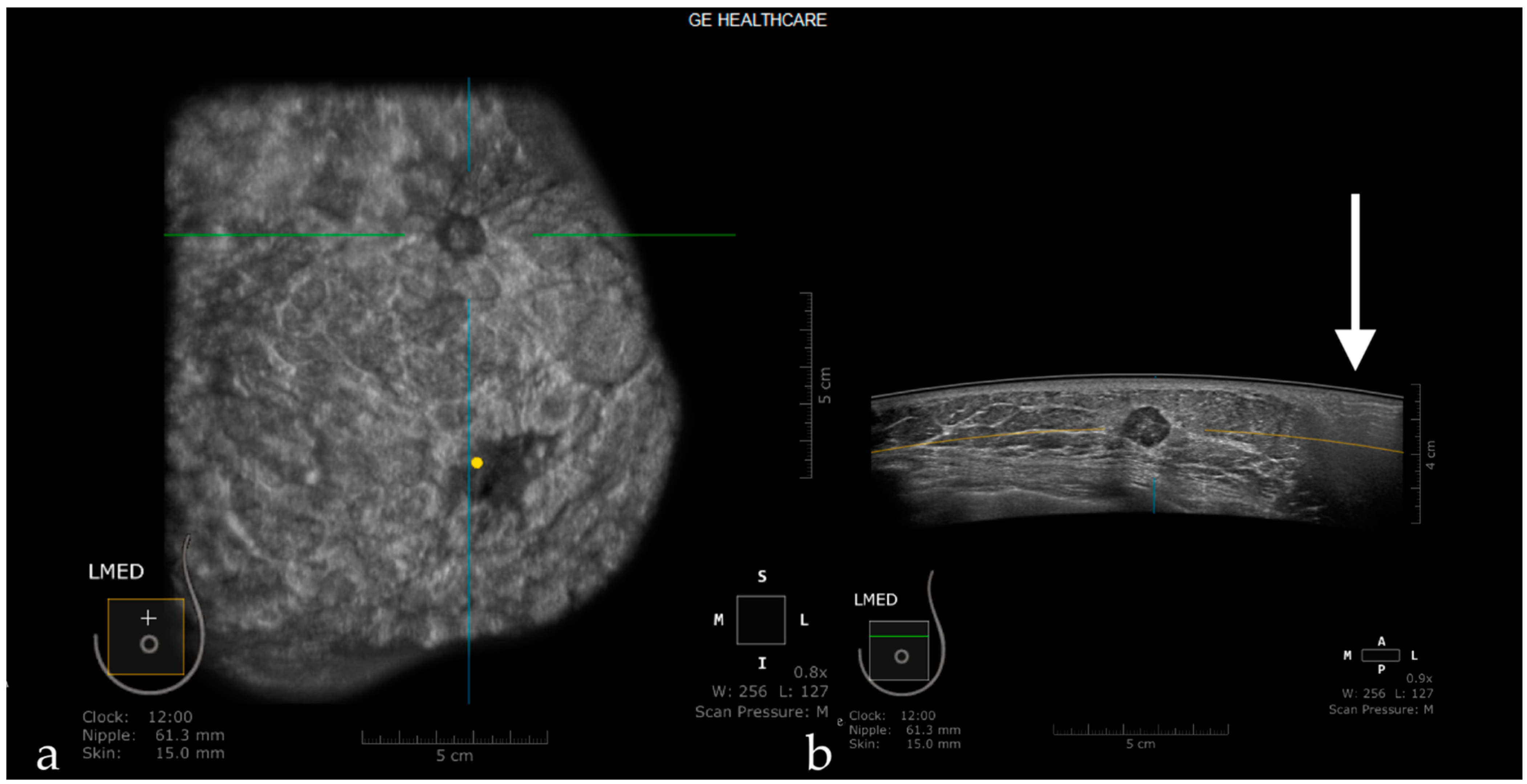
The Usefulness of the Coronal Plane
2.3. ABUS as a Reproducible Method
2.4. ABUS Associated with Digital Breast Tomosynthesis (DBT)
2.5. ABUS Compared with HHUS
2.6. ABUS Compared with MRI
2.7. ABUS as a Time-Saving Method
2.8. ABUS as a Money-Saving Method
2.9. Computer-Aided Detection (CAD) Adapted to ABUS
3. Cons Regarding ABUS
3.1. Technique and Artifacts
3.1.1. Limitations Related to the Technique
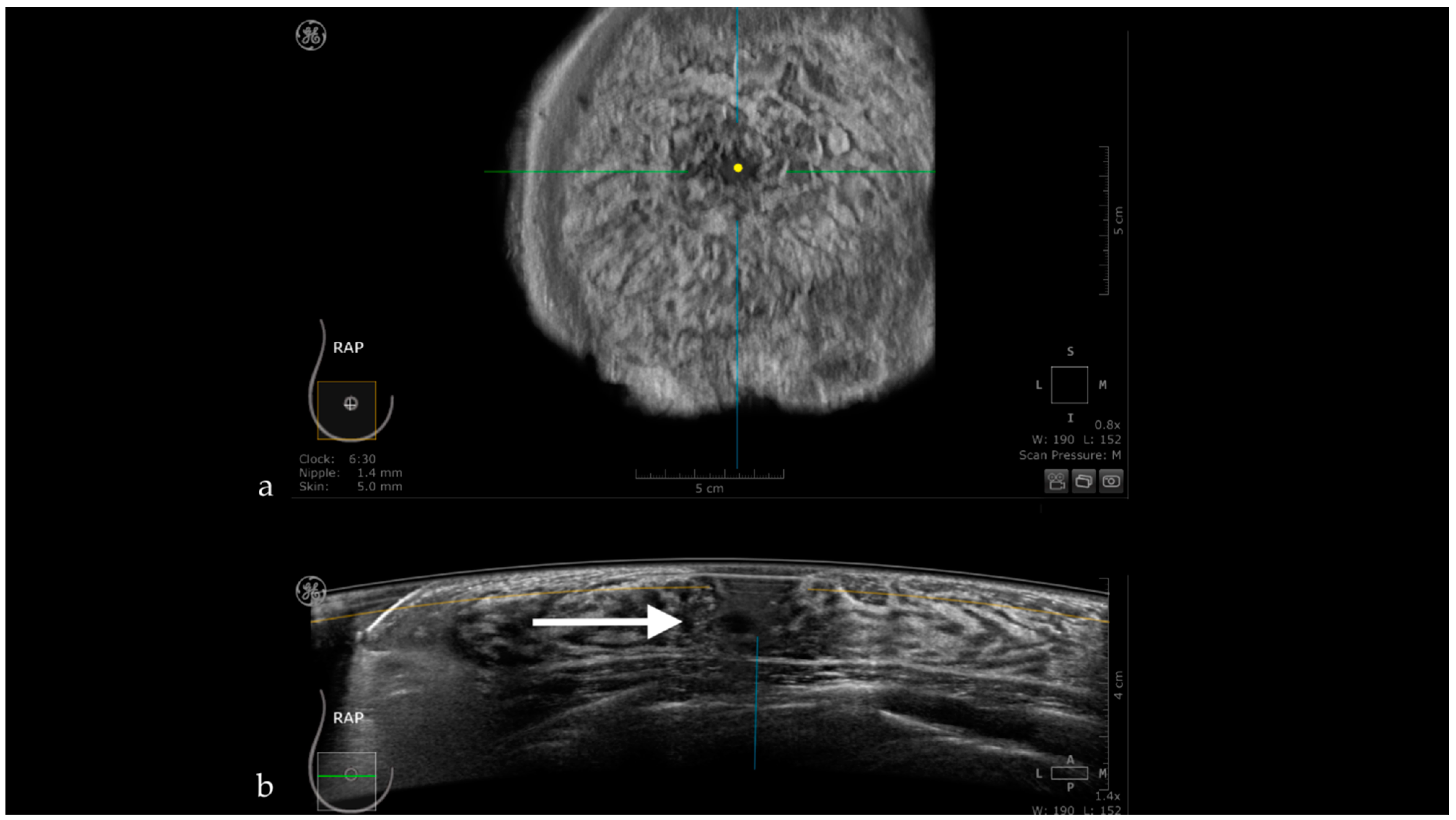
3.1.2. Artifacts
Artifacts Induced by the Use of Ultrasound Gel
Air Interposition
Insufficient Compression
Probe Motion Artifacts
Breathing Artifacts
Skip Artifact
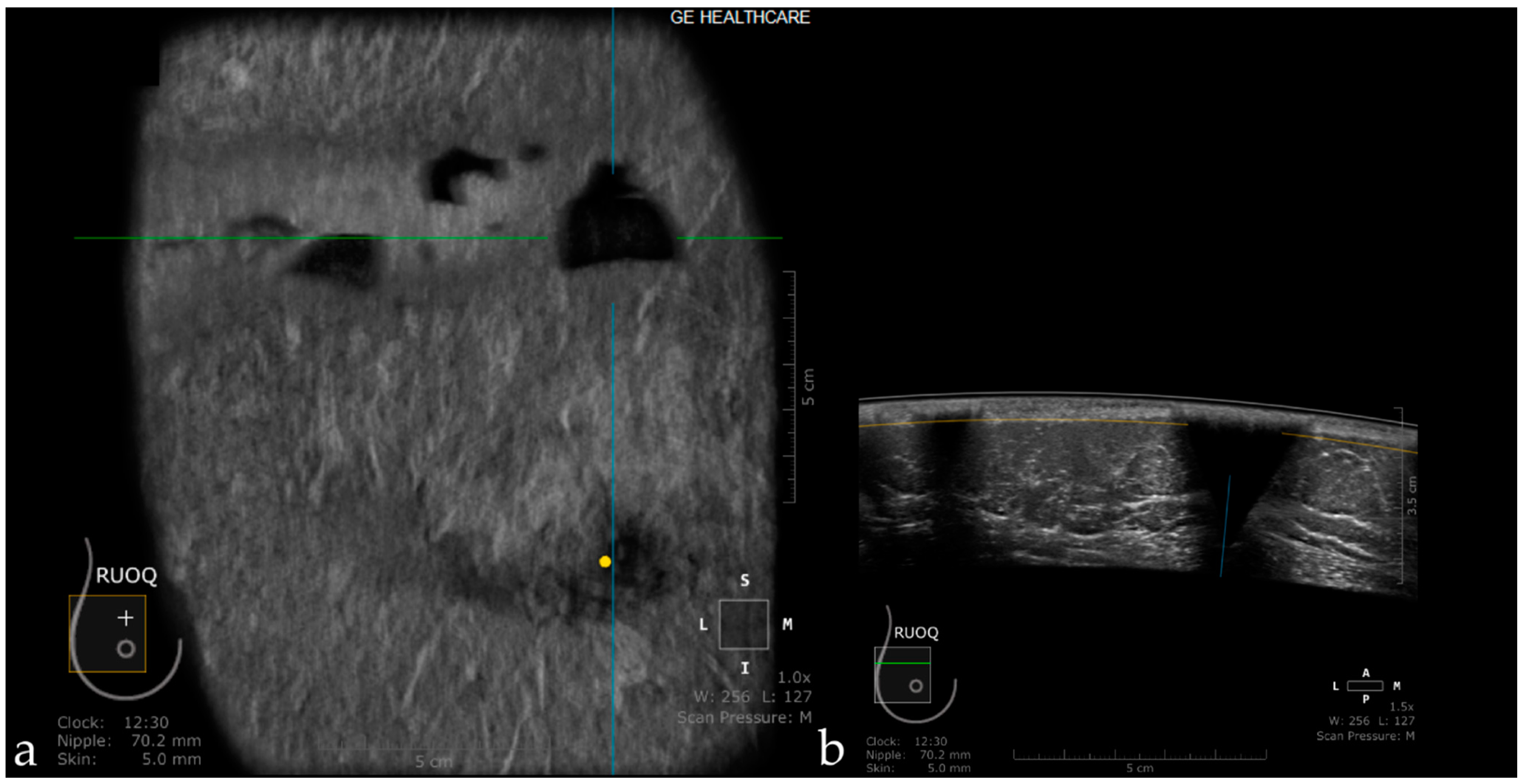
Nipple Artifact
Attenuation Areas
White Wall Sign
3.2. False-Positive Results
3.3. False-Negative Results
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Martin, L.J.; Melnichouk, O.; Guo, H.; Chiarelli, A.M.; Hislop, T.G.; Yaffe, M.J.; Minkin, S.; Hopper, J.L.; Boyd, N.F. Family history, mammographic density, and risk of breast cancer. Cancer Epidemiol. Biomark. Prev. 2010, 19, 456–463. [Google Scholar] [CrossRef] [Green Version]
- Linver, M.N. Mammographic Density and the Risk and Detection of Breast Cancer. Breast Dis. 2008, 18, 364–365. [Google Scholar] [CrossRef]
- Burkett, B.J.; Hanemann, C.W. A Review of Supplemental Screening Ultrasound for Breast Cancer: Certain Populations of Women with Dense Breast Tissue May Benefit. Acad. Radiol. 2016, 23, 1604–1609. [Google Scholar] [CrossRef] [PubMed]
- Zanotel, M.; Bednarova, I.; Londero, V.; Linda, A.; Lorenzon, M.; Girometti, R.; Zuiani, C. Automated breast ultrasound: Basic principles and emerging clinical applications. Radiol. Med. 2018, 123, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Brem, R.F.; Tabár, L.; Duffy, S.W.; Inciardi, M.F.; Guingrich, J.A.; Hashimoto, B.E.; Lander, M.R.; Lapidus, R.L.; Peterson, M.K.; Rapelyea, J.A.; et al. Assessing improvement in detection of breast cancer with three-dimensional automated breast US in women with dense breast tissue: The somoinsight study. Radiology 2015, 274, 663–673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.M.; Partridge, S.C.; Liao, G.J.; Hippe, D.S.; Kim, A.E.; Lee, C.I.; Rahbar, H.; Scheel, J.R.; Lehman, C.D. Double reading of automated breast ultrasound with digital mammography or digital breast tomosynthesis for breast cancer screening. Clin. Imaging 2019, 55, 119–125. [Google Scholar] [CrossRef]
- Kelly, K.M.; Dean, J.; Lee, S.J.; Comulada, W.S. Breast cancer detection: Radiologists’ performance using mammography with and without automated whole-breast ultrasound. Eur. Radiol. 2010, 20, 2557–2564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giuliano, V.; Giuliano, C. Improved breast cancer detection in asymptomatic women using 3D-automated breast ultrasound in mammographically dense breasts. Clin. Imaging 2013, 37, 480–486. [Google Scholar] [CrossRef]
- Wilczek, B.; Wilczek, H.E.; Rasouliyan, L.; Leifland, K. Adding 3D automated breast ultrasound to mammography screening in women with heterogeneously and extremely dense breasts: Report from a hospital-based, high-volume, single-center breast cancer screening program. Eur. J. Radiol. 2016, 85, 1554–1563. [Google Scholar] [CrossRef] [Green Version]
- Rella, R.; Belli, P.; Giuliani, M.; Bufi, E.; Carlino, G.; Rinaldi, P.; Manfredi, R. Automated Breast Ultrasonography (ABUS) in the Screening and Diagnostic Setting: Indications and Practical Use. Acad. Radiol. 2018, 25, 1457–1470. [Google Scholar] [CrossRef]
- Golatta, M.; Baggs, C.; Schweitzer-Martin, M.; Domschke, C.; Schott, S.; Harcos, A.; Scharf, A.; Junkermann, H.; Rauch, G.; Rom, J.; et al. Evaluation of an automated breast 3D-ultrasound system by comparing it with hand-held ultrasound (HHUS) and mammography. Arch. Gynecol. Obstet. 2015, 291, 889–895. [Google Scholar] [CrossRef]
- Wang, H.Y.; Jiang, Y.X.; Zhu, Q.L.; Zhang, J.; Dai, Q.; Liu, H.; Lai, X.J.; Sun, Q. Differentiation of benign and malignant breast lesions: A comparison between automatically generated breast volume scans and handheld ultrasound examinations. Eur. J. Radiol. 2012, 81, 3190–3200. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Chen, Y.; Diao, X.H.; Fang, L.; Pang, Y.; Cheng, A.Q.; Li, W.P.; Wang, Y. Comparative Study of Automated Breast 3-D Ultrasound and Handheld B-Mode Ultrasound for Differentiation of Benign and Malignant Breast Masses. Ultrasound Med. Biol. 2013, 39, 1735–1742. [Google Scholar] [CrossRef] [PubMed]
- Skaane, P.; Gullien, R.; Eben, E.B.; Sandhaug, M.; Schulz-Wendtland, R.; Stoeblen, F. Interpretation of automated breast ultrasound (ABUS) with and without knowledge of mammography: A reader performance study. Acta Radiol. 2015, 56, 404–412. [Google Scholar] [CrossRef] [Green Version]
- Zheng, F.Y.; Yan, L.X.; Huang, B.J.; Xia, H.S.; Wang, X.; Lu, Q.; Li, C.X.; Wang, W.P. Comparison of retraction phenomenon and BI-RADS-US descriptors in differentiating benign and malignant breast masses using an automated breast volume scanner. Eur. J. Radiol. 2015, 84, 2123–2129. [Google Scholar] [CrossRef] [PubMed]
- Van Zelst, J.C.M.; Platel, B.; Karssemeijer, N.; Mann, R.M. Multiplanar Reconstructions of 3D Automated Breast Ultrasound Improve Lesion Differentiation by Radiologists. Acad. Radiol. 2015, 22, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Chen, Y.Q.; Xu, Y.Z.; Chen, M.L.; Zhu, Y.K.; Guan, W.B.; Wang, X.J. Correlation between three-dimensional ultrasound features and pathological prognostic factors in breast cancer. Eur. Radiol. 2014, 24, 1186–1196. [Google Scholar] [CrossRef]
- Zhu, Q.L.; Zhang, J.; Lai, X.J.; Wang, H.Y.; Xiao, M.S.; Jiang, Y.X. Characterisation of breast papillary neoplasm on automated breast ultrasound. Br. J. Radiol. 2013, 86, 20130215. [Google Scholar] [CrossRef] [Green Version]
- Huang, A.; Zhu, L.; Tan, Y.; Liu, J.; Xiang, J.; Zhu, Q.; Bao, L. Evaluation of automated breast volume scanner for breast conservation surgery in ductal carcinoma in situ. Oncol. Lett. 2016, 12, 2481–2484. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Huo, L.; He, Y.; Fan, Z.; Wang, T.; Xie, Y.; Li, J.; Ouyang, T. Early prediction of pathological outcomes to neoadjuvant chemotherapy in breast cancer patients using automated breast ultrasound. Chin. J. Cancer Res. 2016, 28, 478–485. [Google Scholar] [CrossRef] [Green Version]
- Chang, J.M.; Cha, J.H.; Park, J.S.; Kim, S.J.; Moon, W.K. Automated breast ultrasound system (ABUS): Reproducibility of mass localization, size measurement, and characterization on serial examinations. Acta Radiol. 2015, 56, 1163–1170. [Google Scholar] [CrossRef]
- Rocha García, A.M.; Mera Fernández, D. Breast tomosynthesis: State of the art. Radiologia 2019, 61, 274–285. [Google Scholar] [CrossRef]
- Girometti, R.; Tomkova, L.; Cereser, L.; Zuiani, C. Breast cancer staging: Combined digital breast tomosynthesis and automated breast ultrasound versus magnetic resonance imaging. Eur. J. Radiol. 2018, 107, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Hellgren, R.; Dickman, P.; Leifland, K.; Saracco, A.; Hall, P.; Celebioglu, F. Comparison of handheld ultrasound and automated breast ultrasound in women recalled after mammography screening. Acta Radiol. 2017, 58, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Berg, W.A.; Blume, J.D.; Cormack, J.B.; Mendelson, E.B. Operator dependence of physician-performed whole-breast US: Lesion detection and characterization. Radiology 2006, 241, 355–365. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.L.; Xw, J.H.; Li, J.L.; Huang, Y.; Tang, J. Comparison of automated breast volume scanning to hand-held ultrasound and mammography. Radiol. Med. 2012, 117, 1287–1293. [Google Scholar] [CrossRef]
- Zhang, Q.; Hu, B.; Hu, B.; Li, W.B. Detection of breast lesions using an automated breast volume scanner system. J. Int. Med. Res. 2012, 40, 300–306. [Google Scholar] [CrossRef] [Green Version]
- Xiao, Y.M.; Chen, Z.H.; Zhou, Q.C.; Wang, Z. The efficacy of automated breast volume scanning over conventional ultrasonography among patients with breast lesions. Int. J. Gynecol. Obstet. 2015, 131, 293–296. [Google Scholar] [CrossRef]
- Jeh, S.K.; Kim, S.H.; Choi, J.J.; Jung, S.S.; Choe, B.J.; Park, S.; Park, M.S. Comparison of automated breast ultrasonography to handheld ultrasonography in detecting and diagnosing breast lesions. Acta Radiol. 2016, 57, 162–169. [Google Scholar] [CrossRef]
- Niu, L.; Bao, L.; Zhu, L.; Tan, Y.; Xu, X.; Shan, Y.; Liu, J.; Zhu, Q.; Jiang, C.; Shen, Y. Diagnostic Performance of Automated Breast Ultrasound in Differentiating Benign and Malignant Breast Masses in Asymptomatic Women: A Comparison Study With Handheld Ultrasound. J. Ultrasound Med. 2019, 38, 2871–2880. [Google Scholar] [CrossRef]
- Schmachtenberg, C.; Fischer, T.; Hamm, B.; Bick, U. Diagnostic Performance of Automated Breast Volume Scanning (ABVS) Compared to Handheld Ultrasonography With Breast MRI as the Gold Standard. Acad. Radiol. 2017, 24, 954–961. [Google Scholar] [CrossRef]
- Girometti, R.; Zanotel, M.; Londero, V.; Bazzocchi, M.; Zuiani, C. Comparison between automated breast volume scanner (ABVS) versus hand-held ultrasound as a second look procedure after magnetic resonance imaging. Eur. Radiol. 2017, 27, 3767–3775. [Google Scholar] [CrossRef] [PubMed]
- Chae, E.Y.; Shin, H.J.; Kim, H.J.; Yoo, H.; Baek, S.; Cha, J.H.; Kim, H.H. Diagnostic Performance of Automated Breast Ultrasound as a Replacement for a Hand-Held Second-Look Ultrasound for Breast Lesions Detected Initially on Magnetic Resonance Imaging. Ultrasound Med. Biol. 2013, 39, 2246–2254. [Google Scholar] [CrossRef]
- Chae, E.Y.; Cha, J.H.; Kim, H.H.; Shin, H.J. Comparison of lesion detection in the transverse and coronal views on automated breast sonography. J. Ultrasound Med. 2015, 34, 125–135. [Google Scholar] [CrossRef]
- Huppe, A.I.; Inciardi, M.F.; Redick, M.; Carroll, M.; Buckley, J.; Hill, J.D.; Gatewood, J.B. Automated Breast Ultrasound Interpretation Times: A Reader Performance Study. Acad. Radiol. 2018, 25, 1577–1581. [Google Scholar] [CrossRef]
- Foglia, E.; Marinelli, S.; Garagiola, E.; Ferrario, L.; Depretto, C.; Cartia, F.; Ferranti, C.; Porazzi, E.; Scaperrotta, G. Budget impact analysis of breast cancer screening in Italy: The role of new technologies. Health Serv. Manag. Res. 2020, 33, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Inciardi, M.F.; Edwards, A.V.; Papaioannou, J. Interpretation time using a concurrent-read computer-aided detection system for automated breast ultrasound in breast cancer screening of women with dense breast tissue. AJR Am. J. Roentgenol. 2018, 211, 452–461. [Google Scholar] [CrossRef]
- Kaplan, S.S. Automated Whole Breast Ultrasound. Radiol. Clin. N. Am. 2014, 52, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Hendriks, G.A.G.M.; Hollnder, B.; Menssen, J.; Milkowski, A.; Hansen, H.H.G.; De Korte, C.L. Automated 3D ultrasound elastography of the breast: A phantom validation study. Phys. Med. Biol. 2016, 61, 2665–2679. [Google Scholar] [CrossRef]
- Wang, Y.; Nasief, H.G.; Kohn, S.; Milkowski, A.; Clary, T.; Barnes, S.; Barbone, P.E.; Hall, T.J. Three-dimensional Ultrasound Elasticity Imaging on an Automated Breast Volume Scanning System. Ultrason. Imaging 2017, 39, 369–392. [Google Scholar] [CrossRef] [PubMed]
- Schwaab, J.; Diez, Y.; Martı, J.M.R.; van Zelst, J.; Tan, B.P.T.; Gregori, J.; Wirtz, S.; Kramme, J.; Günther, M. Image quality in automated breast ultrasound images: A preliminary study for the development of automated image quality assessment. Proc. MICCAI Int. Workshop Breast Image Anal. 2013, 1, 122–129. [Google Scholar]
- Arleo, E.K.; Saleh, M.; Ionescu, D.; Drotman, M.; Min, R.J.; Hentel, K. Recall rate of screening ultrasound with automated breast volumetric scanning (ABVS) in women with dense breasts: A first quarter experience. Clin. Imaging 2014, 38, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Zhou, Q.; Chen, Z. Automated breast volume scanning versus conventional ultrasound in breast cancer screening. Acad. Radiol. 2015, 22, 387–399. [Google Scholar] [CrossRef]
- Isobe, S.; Tozaki, M.; Yamaguchi, M.; Ogawa, Y.; Homma, K.; Satomi, R.; Saito, M.; Joo, C.; Fukuma, E. Detectability of breast lesions under the nipple using an automated breast volume scanner: Comparison with handheld ultrasonography. JPN J. Radiol. 2011, 29, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Karst, I.; Henley, C.; Gottschalk, N.; Floyd, S.; Mendelson, E.B. Three-dimensional automated breast us: Facts and artifacts. Radiographics 2019, 39, 913–931. [Google Scholar] [CrossRef]
- Kim, S.H.; Kim, H.H.; Moon, W.K. Automated breast ultrasound screening for dense breasts. Korean J. Radiol. 2020, 21, 15–24. [Google Scholar] [CrossRef]





| Author | Year of Publication | Number of Patients | Sensitivity (%) | Specificity (%) | ||
|---|---|---|---|---|---|---|
| FFDM | FFDM + ABUS | FFDM | FFDM + ABUS | |||
| Brem et al. (SomoInsigh) [5] | 2014 | 15,318 | 73.2 | 100 | 85.4 | 72 |
| Kelly et al. [7] | 2010 | 4419 | 40 | 81 | 95.15 | 98.7 |
| Giuliano et al. [8] | 2012 | 3418 | 76 | 96.7 | 99.70 | 98.2 |
| Wilczek et al. [9] | 2016 | 1668 | 63.6 | 100 | 99 | 98.4 |
| ABUS + DBT % (95% CI) | MRI % (95% CI) | |
|---|---|---|
| Sensitivity | 76.5 (58.8–89.3) | 91.7 (84.6–96.1) |
| Positive predictive value | 78.8 (61–91) | 93.4 (86.9–97.3) |
| Diagnostic accuracy | 90 (84.3–94.2) | 93.8 (88–97) |
| Author | Year of Publication | Number of Participants | Sensitivity (%) | Specificity (%) | ||
|---|---|---|---|---|---|---|
| ABUS | HHUS | ABUS | HHUS | |||
| Wang et al. [12] | 2012 | 213 | 95.3 | 90.6 | 80.5 | 82.5 |
| Wang et al. [26] | 2012 | 155 | 96.1 | 93.2 | 91.9 | 88.7 |
| Chen et al. [13] | 2013 | 175 | 92.5 | 88.1 | 86.2 | 87.5 |
| Jen et al. [29] | 2016 | 173 | 88 | 95.7 | 76.2 | 49.4 |
| Niu et al. [30] | 2019 | 398 | 92.23 | 82.52 | 77.62 | 80.24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boca, I.; Ciurea, A.I.; Ciortea, C.A.; Dudea, S.M. Pros and Cons for Automated Breast Ultrasound (ABUS): A Narrative Review. J. Pers. Med. 2021, 11, 703. https://doi.org/10.3390/jpm11080703
Boca I, Ciurea AI, Ciortea CA, Dudea SM. Pros and Cons for Automated Breast Ultrasound (ABUS): A Narrative Review. Journal of Personalized Medicine. 2021; 11(8):703. https://doi.org/10.3390/jpm11080703
Chicago/Turabian StyleBoca (Bene), Ioana, Anca Ileana Ciurea, Cristiana Augusta Ciortea, and Sorin Marian Dudea. 2021. "Pros and Cons for Automated Breast Ultrasound (ABUS): A Narrative Review" Journal of Personalized Medicine 11, no. 8: 703. https://doi.org/10.3390/jpm11080703
APA StyleBoca, I., Ciurea, A. I., Ciortea, C. A., & Dudea, S. M. (2021). Pros and Cons for Automated Breast Ultrasound (ABUS): A Narrative Review. Journal of Personalized Medicine, 11(8), 703. https://doi.org/10.3390/jpm11080703







