Ethnical Differences in Knee Phenotypes Indicate the Need for a More Individualized Approach in Knee Arthroplasty: A Comparison of 80 Asian Knees with 308 Caucasian Knees
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Basic Alignment Parameters
3.2. Phenotypes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vandekerckhove, P.-J.; Lanting, B.; Bellemans, J.; Victor, J.; Macdonald, S. The current role of coronal plane alignment in Total Knee Arthroplasty in a preoperative varus aligned population: An evidence based review. Acta Orthop. Belg. 2016, 82, 129–142. [Google Scholar]
- Hess, S.; Moser, L.B.; Amsler, F.; Behrend, H.; Hirschmann, M.T. Highly variable coronal tibial and femoral alignment in osteoarthritic knees: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1368–1377. [Google Scholar] [CrossRef] [PubMed]
- Moser, L.B.; Hess, S.; Amsler, F.; Behrend, H.; Hirschmann, M.T. Native non-osteoarthritic knees have a highly variable coronal alignment: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1359–1367. [Google Scholar] [CrossRef]
- Hinman, A.D.; Chan, P.H.; Prentice, H.; Paxton, E.W.; Okike, K.M.; Navarro, R. The Association of Race/Ethnicity and Total Knee Arthroplasty Outcomes in a Universally Insured Population. J. Arthroplast. 2020, 35, 1474–1479. [Google Scholar] [CrossRef] [PubMed]
- Adelani, M.A.; Keller, M.R.; Barrack, R.L.; Olsen, M.A. The Impact of Hospital Volume on Racial Differences in Complications, Readmissions, and Emergency Department Visits Following Total Joint Arthroplasty. J. Arthroplast. 2018, 33, 309–315.e20. [Google Scholar] [CrossRef] [PubMed]
- McNamara, C.A.; Hanano, A.A.; Villa, J.M.; Huaman, G.M.; Patel, P.D.; Suarez, J.C. Anthropometric Measurements of Knee Joints in the Hispanic Population. J. Arthroplast. 2018, 33, 2640–2646. [Google Scholar] [CrossRef]
- Shah, S.; Agarwal, N.; Jain, A.; Srivastav, S.; Thomas, S.; Agarwal, S. MRI Based Comparison of Tibial Bone Coverage by Five Knee Prosthesis: Anthropometric Study in Indians. J. Arthroplast. 2015, 30, 1643–1646. [Google Scholar] [CrossRef]
- Chung, B.J.; Kang, J.Y.; Kang, Y.G.; Kim, S.J.; Kim, T.K. Clinical Implications of Femoral Anthropometrical Features for Total Knee Arthroplasty in Koreans. J. Arthroplast. 2015, 30, 1220–1227. [Google Scholar] [CrossRef]
- Harvey, W.F.; Niu, J.; Zhang, Y.; McCree, P.I.; Felson, D.; Nevitt, M.; Xu, L.; Aliabadi, P.; Hunter, D.J. Knee alignment differences between Chinese and Caucasian subjects without osteoarthritis. Ann. Rheum. Dis. 2008, 67, 1524–1528. [Google Scholar] [CrossRef]
- Zeng, Y.-M.; Wang, Y.; Zhu, Z.-A.; Dai, K.-R. Effects of sex and lower extremity alignment on orientation of the knee joint line in knee surgery. Chin. Med. J. 2012, 125, 2126–2131. [Google Scholar]
- Mullaji, A.B.; Sharma, A.K.; Marawar, S.V.; Kohli, A.F.; Singh, D.P. Distal Femoral Rotational Axes in Indian Knees. J. Orthop. Surg. 2009, 17, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Moser, L.B.; Amsler, F.; Behrend, H.; Leclerq, V.; Hess, S. Functional knee phenotypes: A novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1394–1402. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Hess, S.; Behrend, H.; Amsler, F.; Leclercq, V.; Moser, L.B. Phenotyping of hip–knee–ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1378–1384. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Moser, L.B.; Amsler, F.; Behrend, H.; Leclercq, V.; Hess, S. Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1385–1393. [Google Scholar] [CrossRef]
- Schmidt, W.; LiArno, S.; Khlopas, A.; Petersik, A.; Mont, M.A. Stryker Orthopaedic Modeling and Analytics (SOMA): A Review. Surg. Technol. Int. 2018, 32, 315–324. [Google Scholar]
- Gottschling, H.; Schröder, M.; Reimers, N.; Fischer, F.; Homeier, A.; Burgkart, R. A System for Performing Automated Measurements on Large Bone Databases. In Proceedings of the World Congress on Medical Physics and Biomedical Engineering, Munich, Germany, 7–12 September 2009; Dössel, O., Schlegel, W.C., Eds.; Springer: Berlin/Heidelberg, Germany, 2010; pp. 910–913. [Google Scholar]
- Schröder, M.; Gottschling, H.; Reimers, N.; Hauschild, M.; Burgkart, R. Automated Morphometric Analysis of the Femur on Large Anatomical Databases with Highly Accurate Correspondence Detection. Open Med. J. 2014, 1, 15–22. [Google Scholar] [CrossRef]
- Banerjee, S.; Faizan, A.; Nevelos, J.; Kreuzer, S.; Burgkart, R.; Harwin, S.F.; Mont, M.A. Innovations in hip arthroplasty three-dimensional modeling and analytical technology (SOMA). Surg. Technol. Int. 2014, 24, 288–294. [Google Scholar]
- Laumonerie, P.; Ollivier, M.; LiArno, S.; Faizan, A.; Cavaignac, E.; Argenson, J.-N. Which factors influence proximal femoral asymmetry? Bone Jt. J. 2018, 100, 839–844. [Google Scholar] [CrossRef]
- Beckers, L.; Colyn, W.; Bellemans, J.; Victor, J.; Vandekerckhove, P.-J. The contralateral limb is no reliable reference to restore coronal alignment in TKA. Knee Surg. Sports Traumatol. Arthrosc. 2020, 1–11. [Google Scholar] [CrossRef]
- Tang, W.M.; Zhu, Y.H.; Chiu, K.-Y. Axial Alignment of the Lower Extremity in Chinese Adults. J. Bone Jt. Surg. 2000, 82, 1603–1608. [Google Scholar] [CrossRef]
- Hovinga, K.R.; Lerner, A.L. Anatomic variations between Japanese and Caucasian populations in the healthy young adult knee joint. J. Orthop. Res. 2009, 27, 1191–1196. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Konala, P.; Amsler, F.; Golshan-Iranpour, F.; Friederich, N.F.; Cobb, J.P. The position and orientation of total knee replacement components. J. Bone Jt. Surgery. Br. Vol. 2011, 93, 629–633. [Google Scholar] [CrossRef] [Green Version]
- Sailhan, F.; Jacob, L.; Hamadouche, M. Differences in limb alignment and femoral mechanical-anatomical angles using two dimension versus three dimension radiographic imaging. Int. Orthop. 2017, 41, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Chareancholvanich, K.; Pikulkaew, T.; Pornrattanamaneewong, C. Varus inclination of the tibial plateau in Thai adults: A concise radiographic evaluation. J. Med. Assoc. Thail. 2012, 95, 41–46. [Google Scholar]
- Jabalameli, M.; Moghimi, J.; Yeganeh, A.; Nojomi, M. Parameters of lower extremities alignment view in Iranian adult population. Acta Med. Iran. 2015, 53, 293–296. [Google Scholar] [PubMed]
- Maini, L.; Singh, S.; Kushwaha, N.S.; Saini, A.; Rohilla, S.; Sharma, H.; Sharma, V. Radiographic analysis of the axial alignment of the lower extremity in Indian adult males. J. Arthrosc. Jt. Surg. 2015, 2, 128–131. [Google Scholar] [CrossRef]
- Shetty, G.M.; Mullaji, A.; Bhayde, S.; Nha, K.W.; Oh, H.K. Factors contributing to inherent varus alignment of lower limb in normal Asian adults: Role of tibial plateau inclination. Knee 2014, 21, 544–548. [Google Scholar] [CrossRef]
- Song, M.-H.; Yoo, S.-H.; Kang, S.-W.; Kim, Y.-J.; Park, G.-T.; Pyeun, Y.-S. Coronal Alignment of the Lower Limb and the Incidence of Constitutional Varus Knee in Korean Females. Knee Surg. Relat. Res. 2015, 27, 49–55. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, T.; Takayama, K.; Hashimoto, S.; Kanzaki, N.; Hayashi, S.; Kuroda, R.; Matsumoto, T. Radiographic analysis of the lower limbs using the hip–calcaneus line in healthy individuals and in patients with varus knee osteoarthritis. Knee 2017, 24, 1146–1152. [Google Scholar] [CrossRef]
- Insall, J.N.; Binazzi, R.; Soudry, M.; Mestriner, L.A. Total Knee Arthroplasty. Clin. Orthop. Relat. Res. 1985, 192, 13–22. [Google Scholar] [CrossRef] [Green Version]
- Moreland, J.R.; Bassett, L.W.; Hanker, G.J. Radiographic analysis of the axial alignment of the lower extremity. J. Bone Jt. Surg. 1987, 69, 745–749. [Google Scholar] [CrossRef]
- Delport, H.; Labey, L.; Innocenti, B.; De Corte, R.; Sloten, J.V.; Bellemans, J. Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 2159–2169. [Google Scholar] [CrossRef] [PubMed]
- Hungerford, D.S.; Krackow, K.A. Total joint arthroplasty of the knee. Clin. Orthop. Relat. Res. 1985, 23–33. [Google Scholar] [CrossRef]
- Lee, Y.S.; Howell, S.M.; Won, Y.-Y.; Lee, O.-S.; Lee, S.H.; Vahedi, H.; Teo, S.H. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3467–3479. [Google Scholar] [CrossRef]
- Howell, S.M.; Papadopoulos, S.; Kuznik, K.T.; Hull, M.L. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 2271–2280. [Google Scholar] [CrossRef] [PubMed]
- Hirschmann, M.T.; Karlsson, J.; Becker, R. Hot topic: Alignment in total knee arthroplasty—systematic versus more individualised alignment strategies. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1587–1588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nayak, M.; Kumar, V.; Yadav, R.; Maredupaka, S.; Srivastava, D.N.; Malhotra, R.; Pandit, H. Coronal Alignment of the Lower Extremity: A Gender-Based Radio-Graphic Analysis in Indian Patients. Indian J. Orthop. 2020, 54, 504–512. [Google Scholar] [CrossRef] [PubMed]
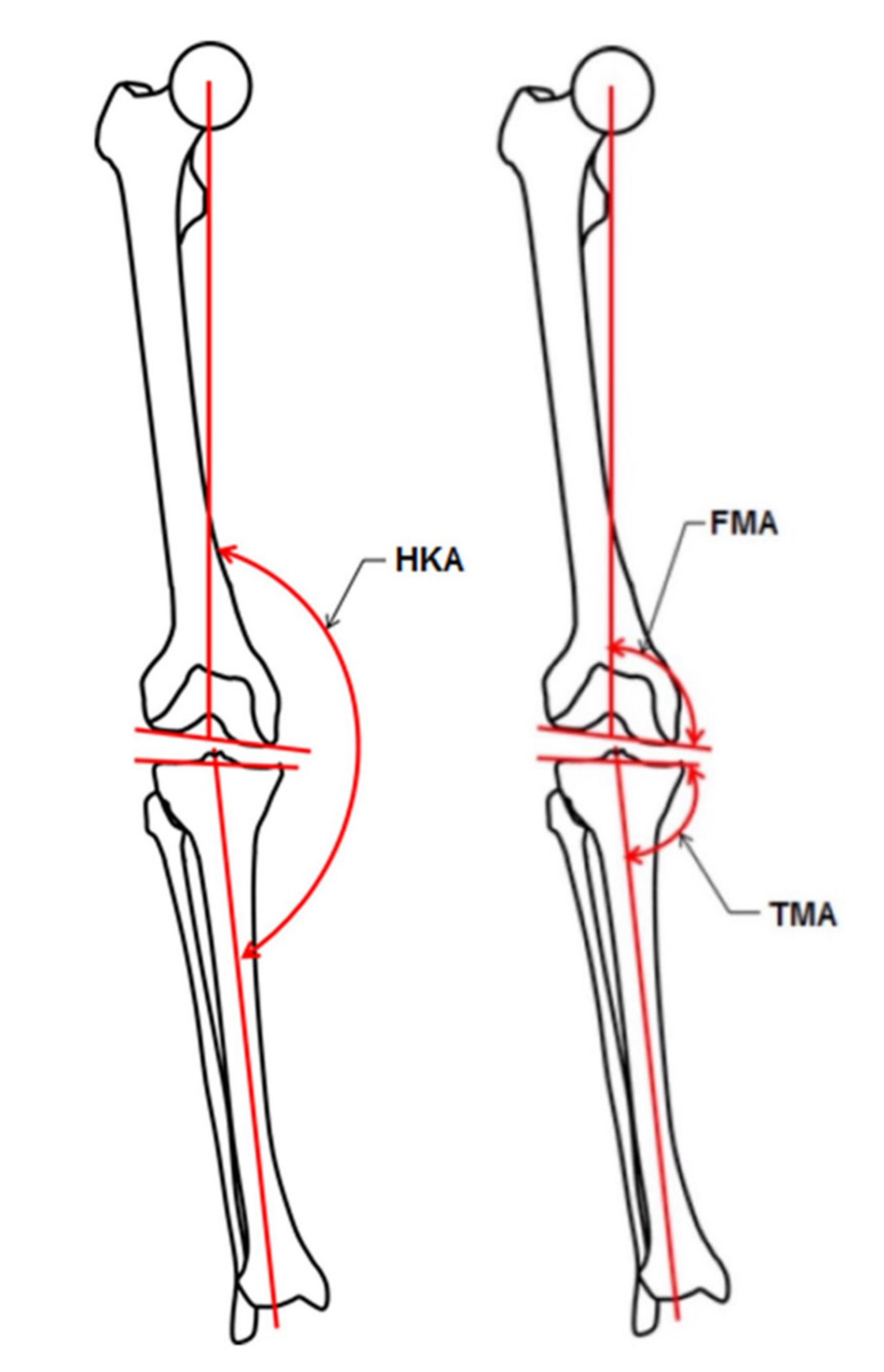



| Coronal Alignment | Average Value | |||
|---|---|---|---|---|
| HKA | VARHKA9° | 169.5° < HKA < 172.5° | 171° | |
| VARHKA | VARHKA6° | 172.5° < HKA < 175.5° | 174° | |
| VARHKA3° | 175.5° < HKA < 178.5° | 177° | ||
| NEUHKA | NEUHKA0° | 178.5° < HKA < 181.5° | 180° | |
| VALHKA | VALHKA3° | 181.5° < HKA < 184.5° | 183° | |
| VALHKA6° | 184.5° < HKA < 187.5° | 186° | ||
| VALHKA9° | 187.5° < HKA < 190.5° | 189° | ||
| FMA | VARFMA | VARFMA6° | 85.5° < FMA < 88.5° | 87° |
| VARFMA3° | 88.5° < FMA < 91.5° | 90° | ||
| NEUFMA | NEUFMA0° | 91.5° < FMA < 94.5° | 93° | |
| VALFMA | VALFMA3° | 94.5° < FMA < 97.5° | 96° | |
| VALFMA6° | 97.5° < FMA < 100.5° | 99° | ||
| TMA | VARTMA | VARTMA6° | 79.5° < TMA < 82.5° | 81° |
| VARTMA3° | 82.5° < TMA < 85.5° | 84° | ||
| NEUTMA | NEUTMA0° | 85.5° < TMA < 88.5° | 87° | |
| VALTMA | VALTMA3° | 88.5° < TMA < 91.5° | 90° | |
| VALTMA6° | 91.5° < TMA < 94.5° | 93° | ||
| Asian | Caucasian 1 | p-Value * | ||||||
|---|---|---|---|---|---|---|---|---|
| Angle | N | Mean ± SD | Range | N | Mean ± SD | Range | ||
| Male | HKA | 48/24 | 178.5° ± 2.0° | 173.7–182.9° | 195/102 | 179.2° ± 2.8° | 172.6–184.9° | 0.15 |
| TMA | 84.1° ± 1.4° | 81.1–86.7° | 86.7° ± 2.3° | 81.3–94.6° | <0.001 | |||
| FMA | 94.1° ± 2.0° | 87.5–97.4° | 93.1° ± 2.1° | 87.9–100.0° | 0.03 | |||
| Female | HKA | 32/16 | 180.5° ± 2.8° | 174–185.3° | 113/58 | 180.5° ± 2.7° | 172.9–187.1° | 0.99 |
| TMA | 84.2° ± 2.7° | 77.5–89° | 88.0° ± 2.3° | 82.3–94.0° | <0.001 | |||
| FMA | 96.6° ± 1.6° | 93.7–99.8° | 93.8° ± 1.8° | 90.1–98.1° | <0.001 | |||
| Male vs. female (p-value) | HKA | 0.02 | <0.007 | |||||
| TMA | 0.90 | 0.001 | ||||||
| FMA | <0.001 | 0.03 | ||||||
| Females | Femoral Phenotypes | VAR 9 | VAR 6 | VAR 3 | NEU | VAL 3 | VAL 6 | VAL 9 |
|---|---|---|---|---|---|---|---|---|
| Tibial phenotypes | Ranges | 82.5°–85.5° | 85.5–88.5° | 88.5–91.5° | 91.5–94.5° | 94.5–97.5° | 97.5–100.5° | 100.5–102.5° |
| VAR 9 | 79.5–82.5° | 1 (3%) | ||||||
| VAR 6 | 82.5–85.5° | 2 (6%) | 6 (19%) | 2 (6%) | ||||
| VAR 3 | 85.5–88.5° | 7 (22%) | 4 (13%) | |||||
| NEU | 88.5–91.5° | 1 (3%) | 4 (13%) | 4 (13%) | ||||
| VAL 3 | 91.5–94.5° | 1 (3%) | ||||||
| VAL 6 | 94.5–97.5° | |||||||
| VAL 9 | 97.5–100.5° | |||||||
| Males | Femoral Phenotypes | VAR 9 | VAR 6 | VAR 3 | NEU | VAL 3 | VAL 6 | VAL 9 |
| Tibial phenotypes | Ranges | 82.5–85.5° | 85.5–88.5° | 88.5–91.5° | 91.5–94.5° | 94.5–97.5° | 97.5–100.5° | 100.5–102.5° |
| VAR 9 | 79.5–82.5° | |||||||
| VAR 6 | 82.5–85.5° | 3 (6%) | 3 (6%) | |||||
| VAR 3 | 85.5–88.5° | 2 (4%) | 1 (2%) | 13 (27%) | 14 (29%) | |||
| NEU | 88.5–91.5° | 1 (2%) | 3 (6%) | 8 (17%) | ||||
| VAL 3 | 91.5–94.5° | |||||||
| VAL 6 | 94.5–97.5° | |||||||
| VAL 9 | 97.5–100.5° |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moser, L.B.; Hess, S.; de Villeneuve Bargemon, J.-B.; Faizan, A.; LiArno, S.; Amsler, F.; Hirschmann, M.T.; Ollivier, M. Ethnical Differences in Knee Phenotypes Indicate the Need for a More Individualized Approach in Knee Arthroplasty: A Comparison of 80 Asian Knees with 308 Caucasian Knees. J. Pers. Med. 2022, 12, 121. https://doi.org/10.3390/jpm12010121
Moser LB, Hess S, de Villeneuve Bargemon J-B, Faizan A, LiArno S, Amsler F, Hirschmann MT, Ollivier M. Ethnical Differences in Knee Phenotypes Indicate the Need for a More Individualized Approach in Knee Arthroplasty: A Comparison of 80 Asian Knees with 308 Caucasian Knees. Journal of Personalized Medicine. 2022; 12(1):121. https://doi.org/10.3390/jpm12010121
Chicago/Turabian StyleMoser, Lukas B., Silvan Hess, Jean-Baptiste de Villeneuve Bargemon, Ahmad Faizan, Sally LiArno, Felix Amsler, Michael T. Hirschmann, and Matthieu Ollivier. 2022. "Ethnical Differences in Knee Phenotypes Indicate the Need for a More Individualized Approach in Knee Arthroplasty: A Comparison of 80 Asian Knees with 308 Caucasian Knees" Journal of Personalized Medicine 12, no. 1: 121. https://doi.org/10.3390/jpm12010121






