The Determinants of the 13-Year Risk of Incident Atrial Fibrillation in a Russian Population Cohort of Middle and Elderly Age
Abstract
:1. Introduction
2. Materials and Methods
Study Population
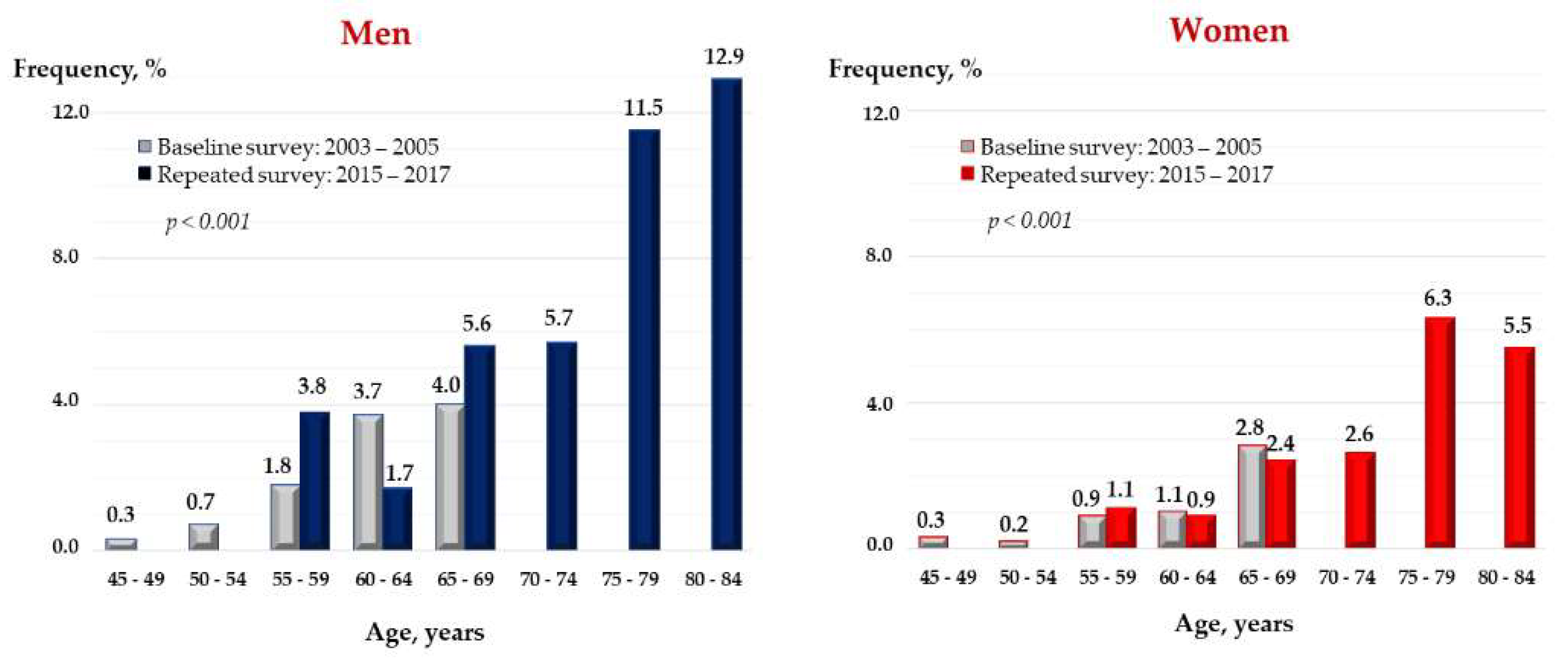
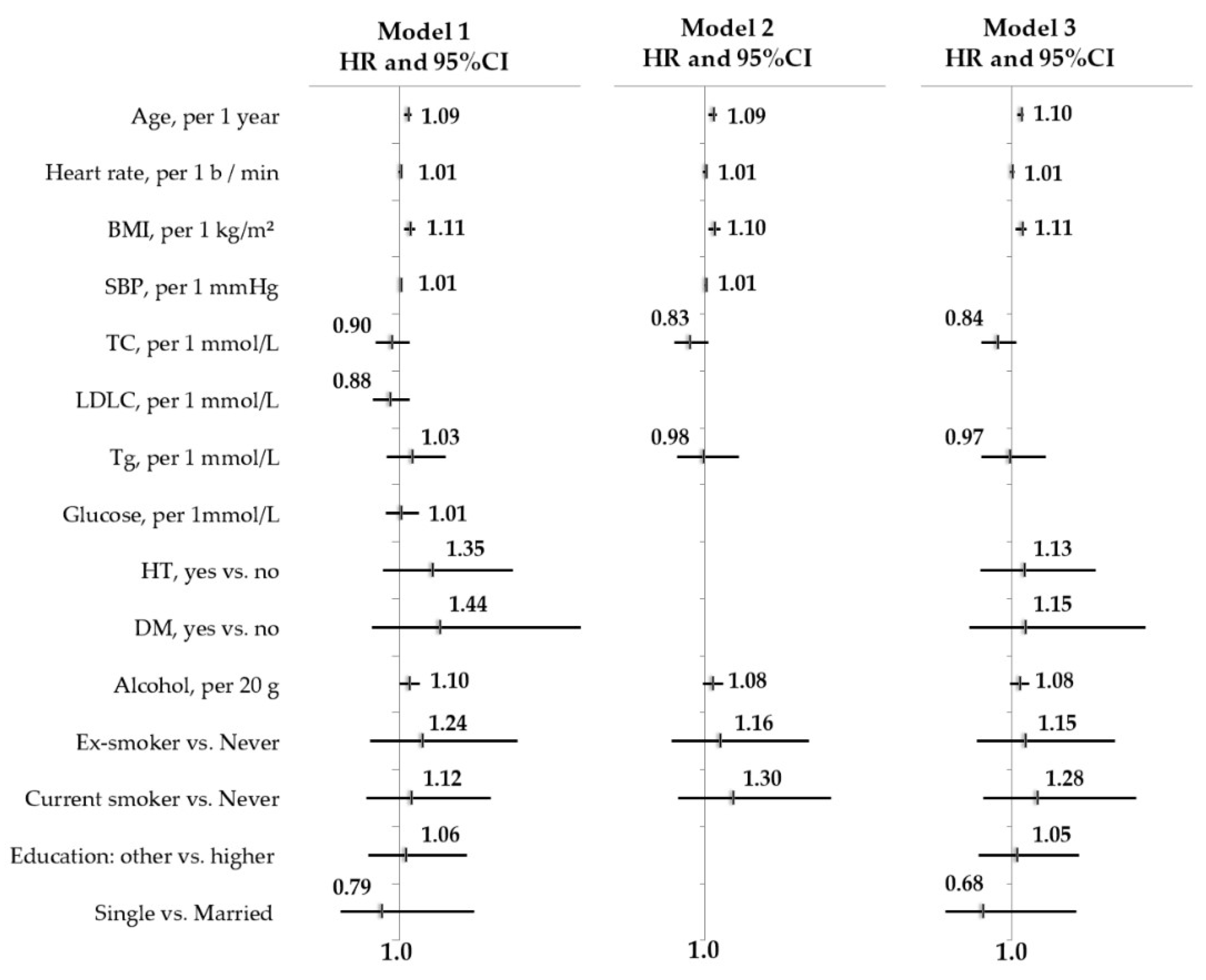
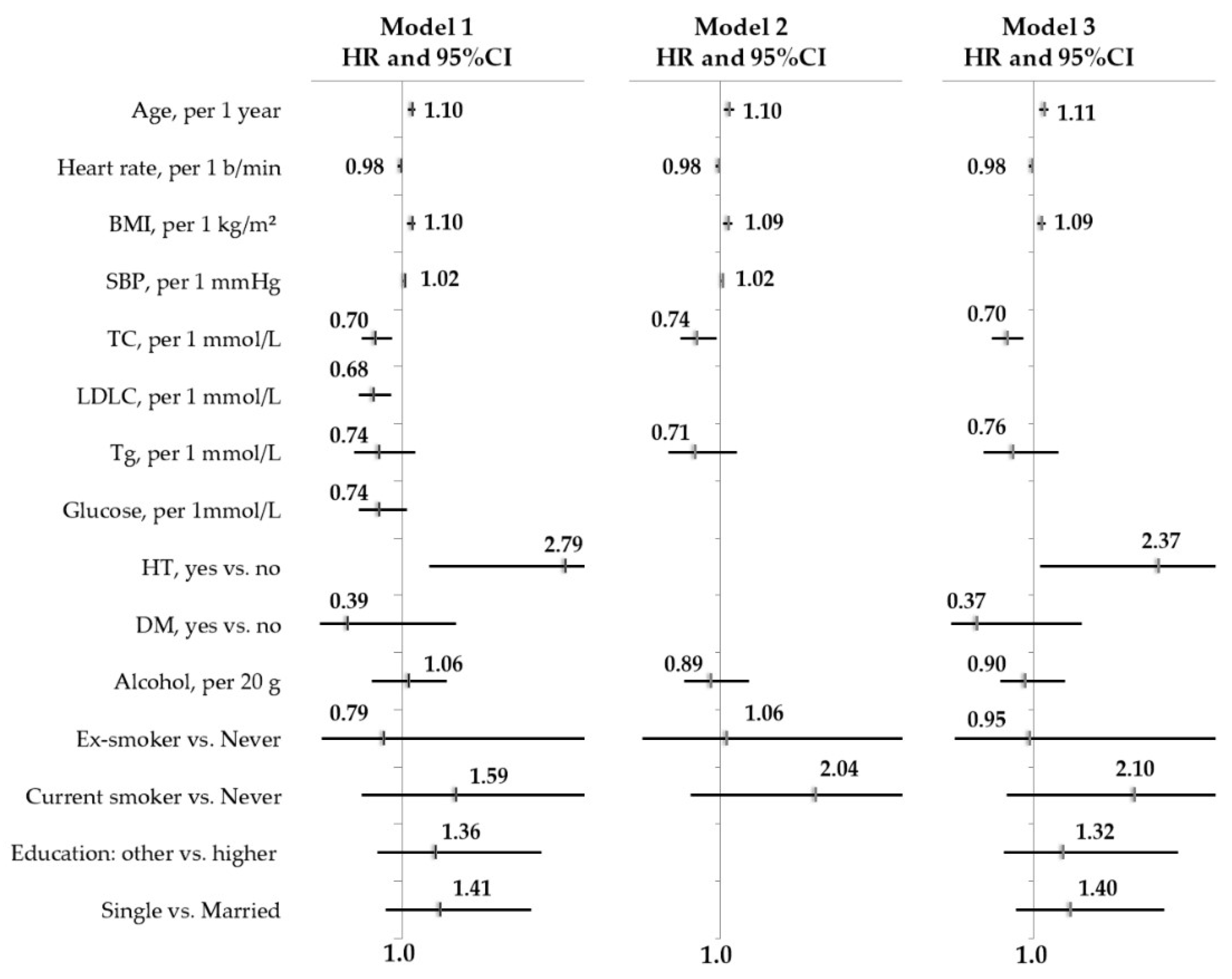
3. Results
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gillis, A.M. Atrial Fibrillation and Ventricular Arrhythmias. Circulation 2017, 135, 593–608. [Google Scholar] [CrossRef]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.-C.; Heidbuchel, H.; Hendriks, J.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. J. Cardio.-Thorac. Surg. 2016, 50, e1–e88. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Timmis, A.; Townsend, N.; Gale, C.; Grobbee, R.; Maniadakis, N.; Flather, M.; Wilkins, E.; Wright, L.; Vos, R.; Bax, J.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2017. Eur. Heart J. 2017, 39, 508–579. [Google Scholar] [CrossRef] [Green Version]
- Ball, J.; Carrington, M.J.; Mcmurray, J.; Stewart, S. Atrial fibrillation: Profile and burden of an evolving epidemic in the 21st century. Int. J. Cardiol. 2013, 167, 1807–1824. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Hylek, E.M.; Phillips, K.A.; Chang, Y.; Henault, L.E.; Selby, J.V.; Singer, D.E. Prevalence of Diagnosed Atrial Fibrillation in Adults. JAMA 2001, 285, 2370–2375. [Google Scholar] [CrossRef] [PubMed]
- Miyasaka, Y.; Barnes, M.E.; Gersh, B.J.; Cha, S.S.; Bailey, K.R.; Abhayaratna, W.P.; Seward, J.B.; Tsang, T.S. Secular Trends in Incidence of Atrial Fibrillation in Olmsted County, Minnesota, 1980 to 2000, and Implications on the Projections for Future Prevalence. Circulation 2006, 114, 119–125. [Google Scholar] [CrossRef] [Green Version]
- Naccarelli, G.V.; Varker, H.; Lin, J.; Schulman, K.L. Increasing Prevalence of Atrial Fibrillation and Flutter in the United States. Am. J. Cardiol. 2009, 104, 1534–1539. [Google Scholar] [CrossRef] [PubMed]
- Krijthe, B.P.; Kunst, A.; Benjamin, E.; Lip, G.Y.; Franco, O.; Hofman, A.; Witteman, J.C.; Stricker, B.H.; Heeringa, J. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur. Heart J. 2013, 34, 2746–2751. [Google Scholar] [CrossRef] [Green Version]
- Chugh, S.S.; Havmoeller, R.; Narayanan, K.; Singh, D.; Rienstra, M.; Benjamin, E.J.; Gillum, R.F.; Kim, Y.-H.; McAnulty, J.H., Jr.; Zheng, Z.-J.; et al. Worldwide Epidemiology of Atrial Fibrillation: A Global Burden of Disease 2010 Study. Circulation 2014, 129, 837–847. [Google Scholar] [CrossRef] [Green Version]
- Zoni-Berisso, M.; Lercari, F.; Carazza, T.; Domenicucci, S. Epidemiology of atrial fibrillation: European perspective. Clin. Epidemiol. 2014, 6, 213–220. [Google Scholar] [CrossRef] [Green Version]
- McManus, D.D.; Rienstra, M.; Benjamin, E. An Update on the Prognosis of Patients With Atrial Fibrillation. Circulation 2012, 126, e143–e146. [Google Scholar] [CrossRef] [Green Version]
- Kannel, W.; Wolf, P.; Benjamin, E.; Levy, D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: Population-based estimates. Am. J. Cardiol. 1998, 82, 2N–9N. [Google Scholar] [CrossRef]
- Nguyen, T.N.; Hilmer, S.N.; Cumming, R.G. Review of epidemiology and management of atrial fibrillation in developing countries. Int. J. Cardiol. 2013, 167, 2412–2420. [Google Scholar] [CrossRef]
- Oldgren, J.; Healey, J.S.; Ezekowitz, M.; Commerford, P.; Avezum, A.; Pais, P.; Zhu, J.; Jansky, P.; Sigamani, A.; Morillo, C.A.; et al. Variations in Cause and Management of Atrial Fibrillation in a Prospective Registry of 15 400 Emergency Department Patients in 46 Countries. Circulation 2014, 129, 1568–1576. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiang, C.-E.; Naditch-Brûlé, L.; Murin, J.; Goethals, M.; Inoue, H.; O’Neill, J.; Silva-Cardoso, J.; Zharinov, O.; Gamra, H.; Alam, S.; et al. Distribution and Risk Profile of Paroxysmal, Persistent, and Permanent Atrial Fibrillation in Routine Clinical Practice. Circ. Arrhythmia Electrophysiol. 2012, 5, 632–639. [Google Scholar] [CrossRef] [Green Version]
- Kishore, A.; Vail, A.; Majid, A.; Dawson, J.; Lees, K.R.; Tyrrell, P.J.; Smith, C. Detection of Atrial Fibrillation After Ischemic Stroke or Transient Ischemic Attack. Stroke 2014, 45, 520–526. [Google Scholar] [CrossRef] [Green Version]
- Henriksson, K.M.; Farahmand, B.; Åsberg, S.; Edvardsson, N.; Terént, A. Comparison of Cardiovascular Risk Factors and Survival in Patients with Ischemic or Hemorrhagic Stroke. Int. J. Stroke 2011, 7, 276–281. [Google Scholar] [CrossRef] [PubMed]
- Grond, M.; Jauss, M.; Hamann, G.; Stark, E.; Veltkamp, R.; Nabavi, D.; Horn, M.; Weimar, C.; Köhrmann, M.; Wachter, R.; et al. Improved Detection of Silent Atrial Fibrillation Using 72-Hour Holter ECG in Patients With Ischemic Stroke. Stroke 2013, 44, 3357–3364. [Google Scholar] [CrossRef] [Green Version]
- Ott, A.; Breteler, M.M.; de Bruyne, M.C.; van Harskamp, F.; Grobbee, D.E.; Hofman, A. Atrial Fibrillation and Dementia in a Population-Based Study. Stroke 1997, 28, 316–321. [Google Scholar] [CrossRef]
- Knecht, S.; Oelschläger, C.; Duning, T.; Lohmann, H.; Albers, J.; Stehling, C.; Heindel, W.; Breithardt, G.; Berger, K.; Ringelstein, E.B.; et al. Atrial fibrillation in stroke-free patients is associated with memory impairment and hippocampal atrophy. Eur. Hear. J. 2008, 29, 2125–2132. [Google Scholar] [CrossRef]
- Ball, J.; Carrington, M.J.; Stewart, S.; On Behalf of the SAFETY Investigators. Mild Cognitive Impairment in high-risk patients with chronic atrial fibrillation: A forgotten component of clinical management? Heart 2013, 99, 542–547. [Google Scholar] [CrossRef] [Green Version]
- Marzona, I.; O’Donnell, M.; Teo, K.; Gao, P.; Anderson, C.; Bosch, J.; Yusuf, S. Increased risk of cognitive and functional decline in patients with atrial fibrillation: Results of the ONTARGET and TRANSCEND studies. Can. Med. Assoc. J. 2012, 184, E329–E336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thrall, G.; Lane, D.; Carroll, D.; Lip, G.Y. Quality of Life in Patients with Atrial Fibrillation: A Systematic Review. Am. J. Med. 2006, 119, 448.e1–448.e19. [Google Scholar] [CrossRef]
- Rothe, A.V.E.; Hutt, F.; Baumert, J.; Breithardt, G.; Goette, A.; Kirchhof, P.; Ladwig, K.-H. Depressed mood amplifies heart-related symptoms in persistent and paroxysmal atrial fibrillation patients: A longitudinal analysis—Data from the German Competence Network on Atrial Fibrillation. Europace 2015, 17, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Santangeli, P.; Di Biase, L.; Bai, R.; Mohanty, S.; Pump, A.; Brantes, M.C.; Horton, R.; Burkhardt, J.D.; Lakkireddy, D.; Reddy, Y.M.; et al. Atrial fibrillation and the risk of incident dementia: A meta-analysis. Heart Rhythm 2012, 9, 1761–1768.e2. [Google Scholar] [CrossRef]
- Peasey, A.; Bobak, M.; Kubinova, R.; Malyutina, S.; Pajak, A.; Tamosiunas, A.; Pikhart, H.; Nicholson, A.; Marmot, M. Determinants of cardiovascular disease and other non-communicable diseases in Central and Eastern Europe: Rationale and design of the HAPIEE study. BMC Public Health 2006, 6, 255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rydén, L.; Standl, E.; Bartnik, M.; Berghe, G.V.D.; Betteridge, J.; De Boer, M.-J.; Cosentino, F.; Jonsson, B.; Laakso, M.; Malmberg, K.; et al. Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: Executive summary: The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur. Hear. J. 2006, 28, 88–136. [Google Scholar] [CrossRef]
- Rose, G.A.; Blackburn, H.; Gillum, R.F. Cardiovascular Survey Methods, 2nd ed.; WHO: Geneva, Switzerland, 1984; p. 223. ISBN 9242400564. [Google Scholar]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Rydén, L.; Grant, P.J.; Anker, S.D.; Berne, C.; Cosentino, F.; Danchin, N.; Deaton, C.; Escaned, J.; Hammes, H.-P.; Huikuri, H.; et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2013, 34, 3035–3087. [Google Scholar] [CrossRef] [Green Version]
- Kim, E.-J.; Yin, X.; Fontes, J.D.; Magnani, J.W.; Lubitz, S.A.; McManus, D.D.; Seshadri, S.; Vasan, R.S.; Ellinor, P.T.; Larson, M.G.; et al. Atrial fibrillation without comorbidities: Prevalence, incidence and prognosis (from the Framingham Heart Study). Am. Heart J. 2016, 177, 138–144. [Google Scholar] [CrossRef]
- Stewart, S.; Hart, C.L.; Hole, D.J.; McMurray, J.J. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am. J. Med. 2002, 113, 359–364. [Google Scholar] [CrossRef]
- Andersson, T.; Magnuson, A.; Bryngelsson, I.-L.; Frøbert, O.; Henriksson, K.M.; Edvardsson, N.; Poçi, D. Gender-related differences in risk of cardiovascular morbidity and all-cause mortality in patients hospitalized with incident atrial fibrillation without concomitant diseases: A nationwide cohort study of 9519 patients. Int. J. Cardiol. 2014, 177, 91–99. [Google Scholar] [CrossRef]
- Singleton, M.J.; Ahmad, M.I.; Kamel, H.; O’Neal, W.T.; Judd, S.E.; Howard, V.J.; Howard, G.; Soliman, E.Z.; Bhave, P.D. Association of Atrial Fibrillation Without Cardiovascular Comorbidities and Stroke Risk: From the REGARDS Study. J. Am. Hear. Assoc. 2020, 9, e016380. [Google Scholar] [CrossRef]
- Heeringa, J.; Van Der Kuip, D.A.M.; Hofman, A.; Kors, J.A.; Van Herpen, G.; Stricker, B.H.C.; Stijnen, T.; Lip, G.Y.H.; Witteman, J.C.M. Prevalence, incidence and lifetime risk of atrial fibrillation: The Rotterdam study. Eur. Heart J. 2006, 27, 949–953. [Google Scholar] [CrossRef] [Green Version]
- Schnabel, R.B.; Yin, X.; Gona, P.; Larson, M.G.; Beiser, A.; McManus, D.D.; Newton-Cheh, C.; Lubitz, S.A.; Magnani, J.W.; Ellinor, P.; et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: A cohort study. Lancet 2015, 386, 154–162. [Google Scholar] [CrossRef] [Green Version]
- Alonso, A.; Krijthe, B.P.; Aspelund, T.; Stepas, K.A.; Pencina, M.J.; Moser, C.B.; Sinner, M.F.; Sotoodehnia, N.; Fontes, J.D.; Janssens, A.C.; et al. Simple Risk Model Predicts Incidence of Atrial Fibrillation in a Racially and Geographically Diverse Population: The CHARGE-AF Consortium. J. Am. Hear. Assoc. 2013, 2, e000102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharashova, E.; Wilsgaard, T.; Ball, J.; Morseth, B.; Gerdts, E.; Hopstock, L.A.; Mathiesen, E.B.; Schirmer, H.; Løchen, M.-L. Long-term blood pressure trajectories and incident atrial fibrillation in women and men: The Tromsø Study. Eur. Heart J. 2019, 41, 1554–1562. [Google Scholar] [CrossRef]
- Wang, T.J.; Parise, H.; Levy, D.; D’Agostino, R.B., Sr.; Wolf, P.A.; Vasan, R.S.; Benjamin, E.J. Obesity and the Risk of New-Onset Atrial Fibrillation. JAMA 2004, 292, 2471–2477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frost, L.; Hune, L.J.; Vestergaard, P. Overweight and obesity as risk factors for atrial fibrillation or flutter: The Danish Diet, Cancer, and Health Study. Am. J. Med. 2005, 118, 489–495. [Google Scholar] [CrossRef]
- Murphy, N.F.; Macintyre, K.; Stewart, S.; Hart, C.L.; Hole, D.; McMurray, J.J.V. Long-term cardiovascular consequences of obesity: 20-year follow-up of more than 15 000 middle-aged men and women (the Renfrew–Paisley study). Eur. Heart J. 2005, 27, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Tedrow, U.B.; Conen, D.; Ridker, P.M.; Cook, N.R.; Koplan, B.A.; Manson, J.E.; Buring, J.E.; Albert, C. The Long- and Short-Term Impact of Elevated Body Mass Index on the Risk of New Atrial Fibrillation: The WHS (Women’s Health Study). J. Am. Coll. Cardiol. 2010, 55, 2319–2327. [Google Scholar] [CrossRef] [Green Version]
- Gami, A.S.; Hodge, D.O.; Herges, R.M.; Olson, E.J.; Nykodym, J.; Kara, T.; Somers, V.K. Obstructive Sleep Apnea, Obesity, and the Risk of Incident Atrial Fibrillation. J. Am. Coll. Cardiol. 2007, 49, 565–571. [Google Scholar] [CrossRef] [Green Version]
- Alonso, A.; Yin, X.; Roetker, N.S.; Magnani, J.W.; Kronmal, R.A.; Ellinor, P.; Chen, L.; Lubitz, S.A.; McClelland, R.L.; McManus, D.D.; et al. Blood Lipids and the Incidence of Atrial Fibrillation: The Multi-Ethnic Study of Atherosclerosis and the Framingham Heart Study. J. Am. Hear. Assoc. 2014, 3, e001211. [Google Scholar] [CrossRef] [Green Version]
- Lopez, F.L.; Agarwal, S.K.; MacLehose, R.F.; Soliman, E.Z.; Sharrett, A.R.; Huxley, R.; Konety, S.; Ballantyne, C.M.; Alonso, A. Blood Lipid Levels, Lipid-Lowering Medications, and the Incidence of Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2012, 5, 155–162. [Google Scholar] [CrossRef] [Green Version]
- Mora, S.; Akinkuolie, A.O.; Sandhu, R.K.; Conen, D.; Albert, C.M. Paradoxical Association of Lipoprotein Measures With Incident Atrial Fibrillation. Circ. Arrhythmia Electrophysiol. 2014, 7, 612–619. [Google Scholar] [CrossRef] [Green Version]
- Goonasekara, C.L.; Balse, E.; Hatem, S.; Steele, D.F.; Fedida, D. Cholesterol and cardiac arrhythmias. Expert Rev. Cardiovasc. Ther. 2010, 8, 965–979. [Google Scholar] [CrossRef]
- Levitan, I.; Christian, A.E.; Tulenko, T.N.; Rothblat, G.H. Membrane Cholesterol Content Modulates Activation of Volume-Regulated Anion Current in Bovine Endothelial Cells. J. Gen. Physiol. 2000, 115, 405–416. [Google Scholar] [CrossRef] [Green Version]
- Abi-Char, J.; Maguy, A.; Coulombe, A.; Balse, E.; Ratajczak, P.; Samuel, J.-L.; Nattel, S.; Hatem, S.N. Membrane cholesterol modulates Kv1.5 potassium channel distribution and function in rat cardiomyocytes. J. Physiol. 2007, 582, 1205–1217. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.; Dokainish, H.; Tsai, P.; Lakkis, N. Update on the Association of Inflammation and Atrial Fibrillation. J. Cardiovasc. Electrophysiol. 2010, 21, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Rizos, C. Effects of Thyroid Dysfunction on Lipid Profile. Open Cardiovasc. Med. J. 2011, 5, 76–84. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denissova, D.; (Dr., Chief Researcher, the Laboratory of Preventive Medicine, Institute of Internal and Preventive Medicine—Branch of Federal State Budgeted Research Institution, “Federal Research Center, Institute of Cytology and Genetics, Siberian Branch of the Russian Academy of Sciences”, Novosibirsk, Russia). Personal communication, 2015.
| Risk Factors | Men, Mean (SD)/n (%) | Women, Mean (SD)/n (%) | ||||
|---|---|---|---|---|---|---|
| iAF(−) n = 1707 | iAF(+) n = 68 | p1 | iAF(−) n = 2042 | iAF(+) n = 54 | p2 | |
| Age, years | 57.6 (6.99) | 60.6 (6.30) | <0.001 | 57.2 (6.95) | 61.4 (5.76) | <0.001 |
| Heart rate, b/min | 71.1 (12.48) | 70.7 (12.16) | 0.807 | 71.2 (10.33) | 68.7 (10.7) | 0.078 |
| BMI, kg/m2 | 26.0 (4.13) | 28.0 (4.25) | <0.001 | 29.5 (5.42) | 32.5 (5.70) | <0.001 |
| SBP, mmHg | 142.3 (22.98) | 151.0 (24.89) | 0.002 | 141.5 (24.89) | 158.9 (27.46) | <0.001 |
| DBP, mmHg | 89.8 (13.18) | 93.1 (13.29) | 0.045 | 89.0 (13.01) | 96.1 (15.40) | <0.001 |
| HT | 1002 (58.7%) | 45 (66.2%) | 0.134 | 1272 (62.3%) | 46 (85.2%) | <0.001 |
| DM | 152 (9.0%) | 8 (12.1%) | 0.253 | 175 (8.7%) | 2 (3.8%) | 0.160 |
| TC, mmol/L | 5.9 (1.21) | 5.9 (1.21) | 0.585 | 6.5 (1.26) | 6.2 (1.12) | 0.077 |
| LDLC, mmol/L | 3.8 (1.08) | 3.7 (1.01) | 0.690 | 4.2 (1.13) | 3.9 (0.98) | 0.060 |
| HDLC, mmol/L | 1.5 (0.38) | 1.5 (0.30) | 0.230 | 1.6 (0.34) | 1.6 (0.37) | 0.521 |
| TG, mmol/L | 1.4 (0.75) | 1.5 (0.69) | 0.514 | 1.5 (0.82) | 1.4 (0.76) | 0.403 |
| GGTP, U/L | 38.3 (45.03) | 35.1 (20.01) | 0.566 | 28.1 (30.40) | 28.7 (17.15) | 0.891 |
| Glucose, mmol/L | 5.9 (1.49) | 5.9 (0.87) | 0.916 | 5.9 (1.39) | 5.6 (0.61) | 0.193 |
| Alcohol per occasion, g | 55.4 (45.89) | 62.5 (48.11) | 0.216 | 22.0 (16.83) | 20.4 (12.89) | 0.482 |
| Smoking status: | ||||||
| Never smoked | 458 (26.8) | 21 (30.9) | 0.215 | 1756 (86.0) | 49.0 (90.7) | 0.559 |
| Former smoker | 390 (22.9) | 20 (29.4) | 87 (4.3) | 1 (1.9) | ||
| Current smoker | 858 (50.3) | 27 (39.7) | 199 (9.7) | 4 (7.4) | ||
| The level of education: | 0.257 | 0.212 | ||||
| Higher | 575 (33.7) | 26 (38.2) | 615 (30.1) | 13 (24.1) | ||
| Other | 1132 (66.3) | 42 (61.8) | 1427(69.9) | 41 (75.9) | ||
| Marital status: | ||||||
| Married | 1495 (87.6) | 62 (91.2) | 0.250 | 1255 (61.5) | 27.0 (50.0) | 0.060 |
| Single | 212 (12.4) | 6 (8.8) | 787 (38.5) | 27,0 (50.0) | ||
| Risk Factors | Model 1 HR (95% CI) | Model 2 HR (95% CI) | Model 3 HR (95% CI) |
|---|---|---|---|
| Age, per 1 years | 1.09 (1.05–1.13) | 1.09 (1.04–1.13) | 1.10 (1.06–1.14) |
| Heart rate, per 1 b/min | 1.01 (0.99-1.03) | 1.00 (0.98–1.03) | 1.01 (0.99–1.03) |
| BMI, per 1 kg/m2 | 1.11 (1.05–1.17) | 1.10 (1.04–1.17) | 1.11 (1.04–1.17) |
| SBP, per 1 mmHg | 1.01 (1.00–1.02) | 1.01 (1.00–1.02) | |
| TC, per 1 mmol/L | 0.90 (0.73–1.11) | 0.83 (0.66–1.04) | 0.84 (0.67–1.05) |
| LDLC, per 1 mmol/L | 0.88 (0.70–1.11) | ||
| TG, per 1 mmol/L | 1.13 (0.85–1.51) | 0.97 (0.67–1.40) | |
| Glucose, per 1 mmol/L | 1.01 (0.84–1.21) | ||
| GGTP, per 1 U/L | 1.00 (1.00–1.01) | ||
| HT, yes vs. no | 1.35 (0.81–2.25) | 1.13 (0.66–1.93) | |
| DM, yes vs. no | 1.44 (0.69–3.01) | 1.15 (0.53–2.48) | |
| Alcohol, per 20 g | 1.10 (1.00–1.22) | 1.08 (0.98–1.20) | 1.00 (1.00–1.01) |
| Smoking status: | |||
| - Former smoker vs. Never | 1.24 (0.67–2.23) | 1.16 (0.63–2.15) | 1.15 (0.61–2.15) |
| - Current smoker vs. Never | 1.12 (0.63–2.01) | 1.30 (0.70–2.40) | 1.28 (0.69–2.38) |
| Level of education: | |||
| - Other vs. higher | 1.06 (0.65–1.74) | 1.05 (0.63–1.75) | |
| Marital status: | |||
| - Single vs. married | 0.79 (0.34–1.82) | 0.68 (0.27–1.72) |
| Risk Factors | Model 1 HR (95% CI) | Model 2 HR (95% CI) | Model 3 HR (95% CI) |
|---|---|---|---|
| Age, per 1 years | 1.10 (1.06–1.15) | 1.09 (1.06–1.12) | 1.10 (1.07–1.14) |
| Heart rate, per 1 b/min | 0.98 (0.95–1.00) | 0.98 (0.95–1.00) | 0.98 (0.95–1.00) |
| BMI, per 1 kg/m2 | 1.10 (1.05–1.15) | 1.09 (1.04–1.14) | 1.09 (1.04–1.14) |
| SBP, per 1 mmHg | 1.02 (1.01–1.03) | 1.02 (1.01–1.03) | |
| TC, per 1 mmol/L | 0.70 (0.55–0.89) | 0.74 (0.57–0.96) | 0.70 (0.54–0.89) |
| LDLC, per 1 mmol/L | 0.68 (0.52–0.88) | ||
| TG, per 1 mmol/L | 0.74 (0.47–1.15) | 0.76 (0.45–1.28) | |
| Glucose, per 1 mmol/L | 0.74 (0.52–1.05) | ||
| GGT, per 1 U/L | 1.01 (1.00–1.01) | ||
| HT, yes vs. no | 2.79 (1.30–5.98) | 2.37 (1.07–5.22) | |
| DM, yes vs. no | 0.39 (0.09–1.60) | 0.37 (0.09–1.53) | |
| Alcohol, per 20 g | 1.06 (0.67–1.49) | 0.89 (0.60–1.32) | 0.90 (0.63–1.35) |
| Smoking status: | |||
| - Former smoker vs. Never | 0.79 (0.11–5.79) | 1.06 (0.14–7.93) | 0.95 (0.13–7.11) |
| - Current smoker vs. Never | 1.59 (0.55–4.64) | 2.04 (0.68–6.15) | 2.10 (0.70–6.27) |
| Level of education: | |||
| - Other vs. Higher | 1.36 (0.73–2.54) | 1.32 (0.67–2.58) | |
| Marital status: | |||
| - Single vs. Married | 1.41 (0.82–2.42) | 1.40 (0.81–2.44) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shapkina, M.; Ryabikov, A.; Mazdorova, E.; Titarenko, A.; Avdeeva, E.; Mazurenko, E.; Shcherbakova, L.; Pikhart, H.; Bobak, M.; Malyutina, S. The Determinants of the 13-Year Risk of Incident Atrial Fibrillation in a Russian Population Cohort of Middle and Elderly Age. J. Pers. Med. 2022, 12, 122. https://doi.org/10.3390/jpm12010122
Shapkina M, Ryabikov A, Mazdorova E, Titarenko A, Avdeeva E, Mazurenko E, Shcherbakova L, Pikhart H, Bobak M, Malyutina S. The Determinants of the 13-Year Risk of Incident Atrial Fibrillation in a Russian Population Cohort of Middle and Elderly Age. Journal of Personalized Medicine. 2022; 12(1):122. https://doi.org/10.3390/jpm12010122
Chicago/Turabian StyleShapkina, Marina, Andrey Ryabikov, Ekaterina Mazdorova, Anastasia Titarenko, Ekaterina Avdeeva, Elena Mazurenko, Lilia Shcherbakova, Hynek Pikhart, Martin Bobak, and Sofia Malyutina. 2022. "The Determinants of the 13-Year Risk of Incident Atrial Fibrillation in a Russian Population Cohort of Middle and Elderly Age" Journal of Personalized Medicine 12, no. 1: 122. https://doi.org/10.3390/jpm12010122
APA StyleShapkina, M., Ryabikov, A., Mazdorova, E., Titarenko, A., Avdeeva, E., Mazurenko, E., Shcherbakova, L., Pikhart, H., Bobak, M., & Malyutina, S. (2022). The Determinants of the 13-Year Risk of Incident Atrial Fibrillation in a Russian Population Cohort of Middle and Elderly Age. Journal of Personalized Medicine, 12(1), 122. https://doi.org/10.3390/jpm12010122






