Improving the Process of Shared Decision-Making by Integrating Online Structured Information and Self-Assessment Tools
Abstract
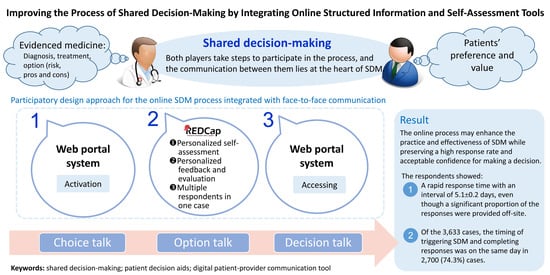
:1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Participatory Design Approach
2.3. Participants, Data Source, and Measurements
2.4. Statistical Analysis
3. Results
3.1. Establishment of the Online SDM Structure and Process
- Displaying all established institutional SDM topics in the HIS to initiate and record the SDM process (Figure S1a).
- Documenting the SDM process in a structured format. Healthcare workers are guided to enter the necessary information, which is automatically transformed into records in the EMR (electronic medical records) (Figure S1b).
- Providing online information for the participants of SDM. A topic-specific, case-sensitive, QR code-containing print-out sheet or email is provided to every participant, who can access the information at any time after the face-to-face discussion (Figure S1c).
- Independently accessing online self-assessment tools through the QR code with a structured self-assessment tool to understand the patient’s clinical situation, options, matters, values, preferences, preparedness, and certainty for further talks with regard to decision-making (Figure S1d).
- Transferring feedback evaluation regarding the SDM process from the participants through the structured questionnaire based on the methods proposed in the literature [11,12,13,14] (Figure S1e).
3.2. Establishment of the Electronic SDM Topics
3.3. SDM Processes and Completed Self-Assessment Responses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rapaport, S.; Leshno, M.; Fink, L. A design process for using normative models in shared decision making: A case study in the context of prenatal testing. Health Expect. 2014, 17, 863–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charles, C.; Gafni, A.; Whelan, T. Decision-making in the physician–patient encounter: Revisiting the shared treatment decision-making model. Soc. Sci. Med. 1999, 49, 651–661. [Google Scholar] [CrossRef]
- Kremer, H.; Ironson, G.; Schneiderman, N.; Hautzinger, M. “It’s My Body”: Does Patient Involvement in Decision Making Reduce Decisional Conflict? Med. Decis. Mak. 2007, 27, 522–532. [Google Scholar] [CrossRef] [PubMed]
- Musbahi, A.; Brown, L.; Reddy, A.; Viswanath, Y.; Rao, M.; Gopinath, B. Systematic review of online patient resources to support shared decision making for bariatric surgery. Int. J. Surg. 2020, 74, 34–38. [Google Scholar] [CrossRef]
- Wickramasekera, N.; Taylor, S.K.; Lumley, E.; Gray, T.; Wilson, E.; Radley, S. Can electronic assessment tools improve the process of shared decision-making? A systematic review. Health Inf. Manag. 2020, 1833358320954385. [Google Scholar] [CrossRef]
- Ozdemir, S.; Malhotra, C.; Teo, I.; Tan, S.N.G.; Wong, W.H.M.; Joad, A.S.K.; Hapuarachchi, T.; Palat, G.; Tuong, P.N.; Bhatnagar, S. Patient-Reported Roles in Decision-Making Among Asian Patients With Advanced Cancer: A Multicountry Study. MDM Policy Pract. 2021, 6, 23814683211061398. [Google Scholar] [CrossRef]
- Chou, T.-J.; Wu, Y.-R.; Tsai, J.-S.; Cheng, S.-Y.; Yao, C.-A.; Peng, J.-K.; Chiu, T.-Y.; Huang, H.-L. Telehealth-Based Family Conferences with Implementation of Shared Decision Making Concepts and Humanistic Communication Approach: A Mixed-Methods Prospective Cohort Study. Int. J. Env. Res. Public Health 2021, 18, 10801. [Google Scholar] [CrossRef]
- Waddell, A.; Lennox, A.; Spassova, G.; Bragge, P. Barriers and facilitators to shared decision-making in hospitals from policy to practice: A systematic review. Implement Sci. 2021, 16, 74. [Google Scholar] [CrossRef]
- Jagosh, J.; Macaulay, A.C.; Pluye, P.; Salsberg, J.; Bush, P.L.; Henderson, J.; Sirett, E.; Wong, G.; Cargo, M.; Herbert, C.P. Uncovering the benefits of participatory research: Implications of a realist review for health research and practice. Milbank Q 2012, 90, 311–346. [Google Scholar] [CrossRef] [Green Version]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 2009, 42, 377–381. [Google Scholar] [CrossRef] [Green Version]
- Kriston, L.; Scholl, I.; Hölzel, L.; Simon, D.; Loh, A.; Härter, M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ. Couns. 2010, 80, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C.; Graham, I.D.; Kristjansson, E.; Kearing, S.A.; Clay, K.F.; O’Connor, A.M. Validation of a preparation for decision making scale. Patient Educ. Couns. 2010, 78, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Légaré, F.; Kearing, S.; Clay, K.; Gagnon, S.; D’Amours, D.; Rousseau, M.; O’Connor, A. Are you SURE?: Assessing patient decisional conflict with a 4-item screening test. Can. Fam. Physician 2010, 56, e308–e314. [Google Scholar] [PubMed]
- Scholl, I.; Kriston, L.; Dirmaier, J.; Buchholz, A.; Härter, M. Development and psychometric properties of the Shared Decision Making Questionnaire–physician version (SDM-Q-Doc). Patient Educ. Couns. 2012, 88, 284–290. [Google Scholar] [CrossRef]
- Elwyn, G.; Frosch, D.; Thomson, R.; Joseph-Williams, N.; Lloyd, A.; Kinnersley, P.; Cording, E.; Tomson, D.; Dodd, C.; Rollnick, S. Shared decision making: A model for clinical practice. J. Gen. Intern. Med. 2012, 27, 1361–1367. [Google Scholar] [CrossRef] [Green Version]
- Sferra, S.; Erkmen, C.; Ma, G.; Cheng, J.; Kaiser, L.; DiSesa, V. Online decision AID vs option grid in shared decision making prior to lung cancer screening. Chest 2017, 152, A1122. [Google Scholar] [CrossRef]
- Ved, R.; Cobbold, N.; Igbagiri, K.; Willis, M.; Leach, P.; Zaben, M. Online patient information on Vagus Nerve Stimulation: How reliable is it for facilitating shared decision making? Seizure 2017, 50, 125–129. [Google Scholar] [CrossRef] [Green Version]
- Streufert, B.; Reed, S.D.; Orlando, L.A.; Taylor, D.C.; Huber, J.C.; Mather, R.C., III. Understanding preferences for treatment after hypothetical first-time anterior shoulder dislocation: Surveying an online panel utilizing a novel shared decision-making tool. Orthop. J. Sports Med. 2017, 5, 2325967117695788. [Google Scholar] [CrossRef]
- Washington, K.; Shacklady, C. Patients’ experience of shared decision making using an online patient decision aid for osteoarthritis of the knee–a service evaluation. Musculoskelet. Care 2015, 13, 116–126. [Google Scholar] [CrossRef]
- Thunnissen, F.M.; Schreurs, B.W.; Latenstein, C.S.; Meinders, M.J.; Adang, E.M.; Elwyn, G.; Boersma, D.; Bosmans, B.; Bosscha, K.; Ginsel, B.L. Evaluation of a shared decision-making strategy with online decision aids in surgical and orthopaedic practice: Study protocol for the E-valuAID, a multicentre study with a stepped-wedge design. BMC Med. Inf. Decis. Mak. 2021, 21, 110. [Google Scholar] [CrossRef]
- Søndergaard, S.R.; Madsen, P.H.; Hilberg, O.; Bechmann, T.; Jakobsen, E.; Jensen, K.M.; Olling, K.; Steffensen, K.D. The impact of shared decision making on time consumption and clinical decisions. A prospective cohort study. Patient Educ. Couns. 2021, 104, 1560–1567. [Google Scholar] [CrossRef] [PubMed]
- Resnicow, K.; Catley, D.; Goggin, K.; Hawley, S.; Williams, G.C. Shared Decision Making in Health Care: Theoretical Perspectives for Why It Works and For Whom. Med. Decis. Mak. 2021, 0272989X211058068. [Google Scholar] [CrossRef] [PubMed]
- Valentine, K.; Mancini, B.; Vo, H.; Brodney, S.; Cosenza, C.; Barry, M.J.; Sepucha, K.R. Using Standardized Videos to Examine the Validity of the Shared Decision Making Process Scale: Results of a Randomized Online Experiment. Med. Decis. Mak. 2022, 42, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Humphries, B.; León-García, M.; de Guzman Quispe, E.N.; Canelo-Aybar, C.; Valli, C.; Barrios, K.P.; Agarwal, A.; Mirabi, S.; Eckman, M.H.; Guyatt, G. More work needed on decision analysis for shared decision-making: A scoping review. J. Clin. Epidemiol. 2021, 141, 106–120. [Google Scholar] [CrossRef]
- Sanftenberg, L.; Kuehne, F.; Lukaschek, K.; Meissner, K.; Gensichen, J. Shared Decision Making–A Key Competence of All Health Care Professionals. Evaluation and Adaptation of a Digitally Enhanced Learning and Teaching Unit. J. Eur. CME 2021, 10, 1987119. [Google Scholar] [CrossRef]
- Jayakumar, P.; Moore, M.G.; Furlough, K.A.; Uhler, L.M.; Andrawis, J.P.; Koenig, K.M.; Aksan, N.; Rathouz, P.J.; Bozic, K.J. Comparison of an Artificial Intelligence–Enabled Patient Decision Aid vs Educational Material on Decision Quality, Shared Decision-Making, Patient Experience, and Functional Outcomes in Adults With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2037107. [Google Scholar] [CrossRef]
- Bjerring, J.C.; Busch, J. Artificial intelligence and patient-centered decision-making. Philos. Technol. 2021, 34, 349–371. [Google Scholar] [CrossRef] [Green Version]
- Garvelink, M.M.; Emond, J.; Menear, M.; Brière, N.; Freitas, A.; Boland, L.; Perez, M.M.B.; Blair, L.; Stacey, D.; Légaré, F. Development of a decision guide to support the elderly in decision making about location of care: An iterative, user-centered design. Res. Involv. Engag. 2016, 2, 26. [Google Scholar] [CrossRef] [Green Version]
- Stacey, D.; Ludwig, C.; Archambault, P.; Babulic, K.; Edwards, N.; Lavoie, J.; Sinha, S.; O’Connor, A.M. Feasibility of rapidly developing and widely disseminating patient decision aids to respond to urgent decisional needs due to the COVID-19 pandemic. Med. Decis. Mak. 2021, 41, 233–239. [Google Scholar] [CrossRef]
- Stacey, D.; Taljaard, M.; Smylie, J.; Boland, L.; Breau, R.H.; Carley, M.; Jana, K.; Peckford, L.; Blackmore, T.; Waldie, M. Implementation of a patient decision aid for men with localized prostate cancer: Evaluation of patient outcomes and practice variation. Implement Sci. 2015, 11, 87. [Google Scholar] [CrossRef] [Green Version]
- Toupin-April, K.; Barton, J.; Fraenkel, L.; Li, L.C.; Brooks, P.; De Wit, M.; Stacey, D.; Légaré, F.; Meara, A.; Shea, B. Toward the development of a core set of outcome domains to assess shared decision-making interventions in rheumatology: Results from an OMERACT Delphi survey and consensus meeting. J. Rheumatol. 2017, 44, 1544–1550. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, C.; King, M.T.; Butow, P.; Legare, F.; Lyddiatt, A.; Souli, I.; Rincones, O.; Stacey, D. Is quality of life a suitable measure of patient decision aid effectiveness? Sub-analysis of a Cochrane systematic review. Qual. Life Res. 2019, 28, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Brousseau, L.; Charette, M.; Poitras, S.; Stacey, D. Effectiveness of patient decision aids for total hip and knee arthroplasty decision-making: A systematic review. Osteoarthr. Cartil. 2021, 29, 1399–1411. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.H.; Medleg, F.; Choi, D.; Spagnuolo, C.M.; Pinnaduwage, L.; Straus, S.E.; Cantarutti, P.; Chu, K.; Frydrych, P.; Hoang-Kim, A. Integrating shared decision-making into primary care: Lessons learned from a multi-centre feasibility randomized controlled trial. BMC Med. Inf. Decis. Mak. 2021, 21, 323. [Google Scholar] [CrossRef]
- Yu, C.; Choi, D.; Bruno, B.A.; Thorpe, K.E.; Straus, S.E.; Cantarutti, P.; Chu, K.; Frydrych, P.; Hoang-Kim, A.; Ivers, N. Impact of MyDiabetesPlan, a web-based patient decision aid on decisional conflict, diabetes distress, quality of life, and chronic illness care in patients with diabetes: Cluster randomized controlled trial. J. Med. Internet Res. 2020, 22, e16984. [Google Scholar] [CrossRef]
- Légaré, F.; Brière, N.; Stacey, D.; Lacroix, G.; Desroches, S.; Dumont, S.; Fraser, K.D.; Rivest, L.-P.; Durand, P.J.; Turcotte, S. Implementing shared decision-making in interprofessional home care teams (the IPSDM-SW study): Protocol for a stepped wedge cluster randomised trial. BMJ Open 2016, 6, e014023. [Google Scholar] [CrossRef] [Green Version]



| Topic | Topic |
|---|---|
| Long-term care settings for ventilator dependence | Options for smoking cessation |
| Tracheostomy for prolonged mechanical ventilation | The choice of hospice location |
| Choice of dialysis treatment | Treatment for traumatic rib fractures |
| Long-term nasogastric tube or gastric tube | Indwelling catheter for neurogenic bladder |
| Medications for poor oral hypoglycemic drug responders | Discharge preparation from rehabilitation ward |
| Choice of heart valves | Post-discharge care for elderly with reduced function |
| Treatment for severe brain damage | Post-stroke rehabilitation treatment |
| Intervention for heart failure with renal insufficiency | Rehabilitation after hip or knee fracture surgery |
| Reconstructing missing teeth | Treatment for poorly controlled atopic dermatitis |
| Choice of orthodontic device | Treating tuberous sclerosis & cutaneous angiofibroma |
| Treatment to assist upper jaw teeth pullback | Re-allocation after an occupational disaster |
| Method of obtaining head and neck tumor tissues | Integrated rehabilitative care for cancer patients |
| Hypothermia treatment after resuscitation | Treatment of children with urinary tract reflux |
| Follow-up medical care after first aid | Location of children’s end-of-life hospice |
| Wait in the emergency room or transfer | Management of teeth growth problem |
| Artificial joint replacement surgery | Nutrition for severe trauma/critically ill patients |
| Treatment for osteoporosis | Care for ventilator-dependent severe stroke |
| Integrated palliative care options for cancer patients | Radiation therapy for head and neck cancer |
| Use of unconventional sleeping drugs | Interventions for benign prostatic hyperplasia |
| Patient-controlled pain relief | Integrated psychological care for cancer patients |
| Treatment for Guillain-Barre syndrome | Integrated nutritional care for cancer patients |
| Treatment for high-risk metastatic prostate cancer | Integrated social worker management for cancer patients |
| Reproduction method for those at high risk | Integrated pain management for cancer patients |
| Treatment for advanced ovarian cancer | Multiple integrated care for cancer patients |
| Characteristic | Data |
|---|---|
| Department | |
| Internal Medicine | 1447 (39.8%) |
| Family Medicine | 500 (13.8%) |
| Surgery | 284 (7.8%) |
| Otolaryngology | 281 (7.7%) |
| Psychiatry | 268 (7.4%) |
| Dentistry | 218 (6.0%) |
| Orthopedic | 124 (3.4%) |
| Physical medicine and rehabilitation | 87 (2.4%) |
| Medical Genetics | 81 (2.2%) |
| Others | 322 (8.9%) |
| Setting | |
| Outpatient | 1476 (40.6%) |
| Inpatient | 1404 (38.7%) |
| Emergency service | 753 (20.7%) |
| Preparedness, evaluated by the SDM team | |
| Ready for decision-making | 2015 (74.0%) |
| Not ready for decision-making | 708 (26.0%) |
| Characteristic | Data |
|---|---|
| Respondents (n = 3633) | |
| Age, years | 56.5 ± 0.3 |
| Gender, male (%) | 1883 (51.8%) |
| Relationship with the patient (n = 3606) | |
| The patient | 2298 (63.7%) |
| Spouse | 229 (6.4%) |
| Parent | 240 (6.7%) |
| Child | 742 (20.6%) |
| Sibling | 94 (2.6%) |
| Other | 3 (0.1%) |
| Interval between triggering SDM and response, days | 5.1 ± 0.2 |
| Online preliminary response for the choice | |
| Ready for decision-making | 3208 (88.3%) |
| Not yet ready for decision-making | 424 (11.7%) |
| Variable | Coefficient | 95% Confidence Interval | p-Value |
|---|---|---|---|
| The patient as the respondent | 2.168 | 1.080–3.257 | <0.001 |
| Female | −0.267 | −1.229–0696 | 0.59 |
| Age | 0.092 | 0.067–0.117 | <0.001 |
| Surgical encounter for SDM | 4.752 | 3.587–5.918 | <0.001 |
| Emergency department encounter | −4.754 | −6.086–−3.422 | <0.001 |
| Inpatient encounter | −0.349 | −1.506–0.808 | 0.56 |
| Constant | −1.740 | −3.760–0.280 | 0.09 |
| Variable | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| The patient as the respondent | 3.480 | 2.715–4.459 | <0.001 |
| Female | 0.825 | 0.665–1.025 | 0.08 |
| Age | 0.997 | 0.992–1.003 | 0.37 |
| Surgical encounter for SDM | 1.056 | 0.828–1.346 | 0.66 |
| Emergency department encounter | 24.963 | 12.122–51.407 | <0.001 |
| Inpatient encounter | 1.753 | 1.372–2.240 | <0.001 |
| Variable | Coefficient | 95% Confidence Interval | p-Value |
|---|---|---|---|
| The patient as the respondent | 0.021 | 0.010–0.033 | <0.001 |
| Female | −0.038 | −0.049–−0.028 | <0.001 |
| Age | 0.001 | <0.001–0.001 | <0.001 |
| Surgical encounter for SDM | 0.025 | 0.012–0.037 | <0.001 |
| Emergency department encounter | 0.138 | 0.123–0.153 | <0.001 |
| Inpatient encounter | −0.013 | −0.026–<−0.001 | 0.04 |
| Constant | 0.821 | 0.799–0.843 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, P.-J.; Wu, C.-Y.; Kuo, L.-C.; Chen, M.-Y.; Chen, Y.-L.; Huang, S.-F.; Chuang, P.-Y.; Jerng, J.-S.; Chen, S.-Y. Improving the Process of Shared Decision-Making by Integrating Online Structured Information and Self-Assessment Tools. J. Pers. Med. 2022, 12, 256. https://doi.org/10.3390/jpm12020256
Hsu P-J, Wu C-Y, Kuo L-C, Chen M-Y, Chen Y-L, Huang S-F, Chuang P-Y, Jerng J-S, Chen S-Y. Improving the Process of Shared Decision-Making by Integrating Online Structured Information and Self-Assessment Tools. Journal of Personalized Medicine. 2022; 12(2):256. https://doi.org/10.3390/jpm12020256
Chicago/Turabian StyleHsu, Pei-Jung, Chia-Ying Wu, Lu-Cheng Kuo, Ming-Yuan Chen, Yu-Ling Chen, Szu-Fen Huang, Pao-Yu Chuang, Jih-Shuin Jerng, and Shey-Ying Chen. 2022. "Improving the Process of Shared Decision-Making by Integrating Online Structured Information and Self-Assessment Tools" Journal of Personalized Medicine 12, no. 2: 256. https://doi.org/10.3390/jpm12020256
APA StyleHsu, P.-J., Wu, C.-Y., Kuo, L.-C., Chen, M.-Y., Chen, Y.-L., Huang, S.-F., Chuang, P.-Y., Jerng, J.-S., & Chen, S.-Y. (2022). Improving the Process of Shared Decision-Making by Integrating Online Structured Information and Self-Assessment Tools. Journal of Personalized Medicine, 12(2), 256. https://doi.org/10.3390/jpm12020256