Inflammation and Oxidative Stress in Seminal Plasma: Search for Biomarkers in Diagnostic Approach to Male Infertility
Abstract
:1. Introduction
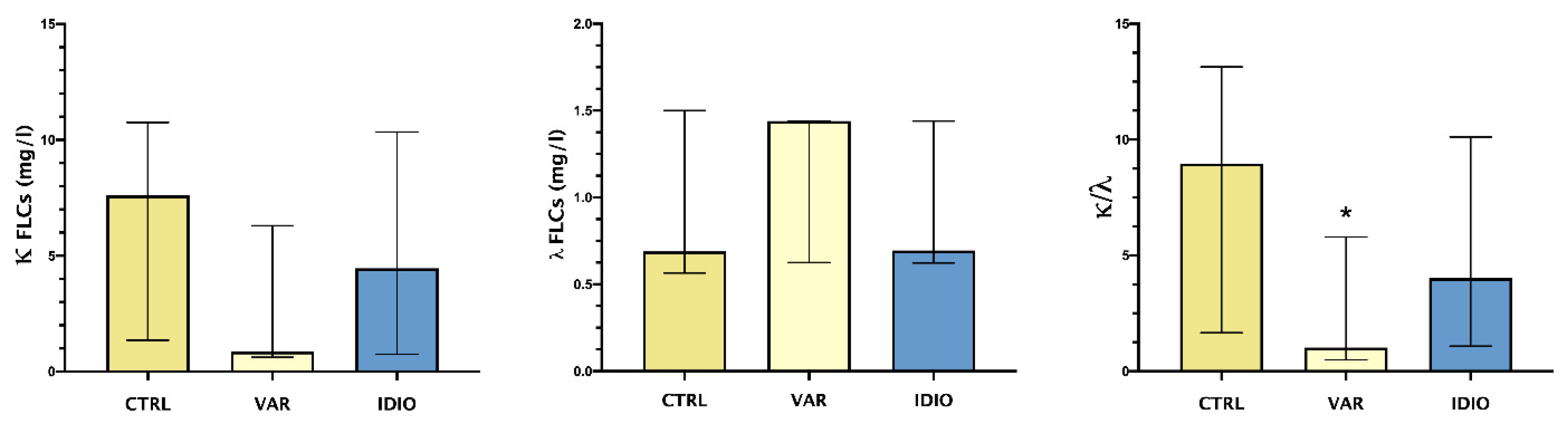
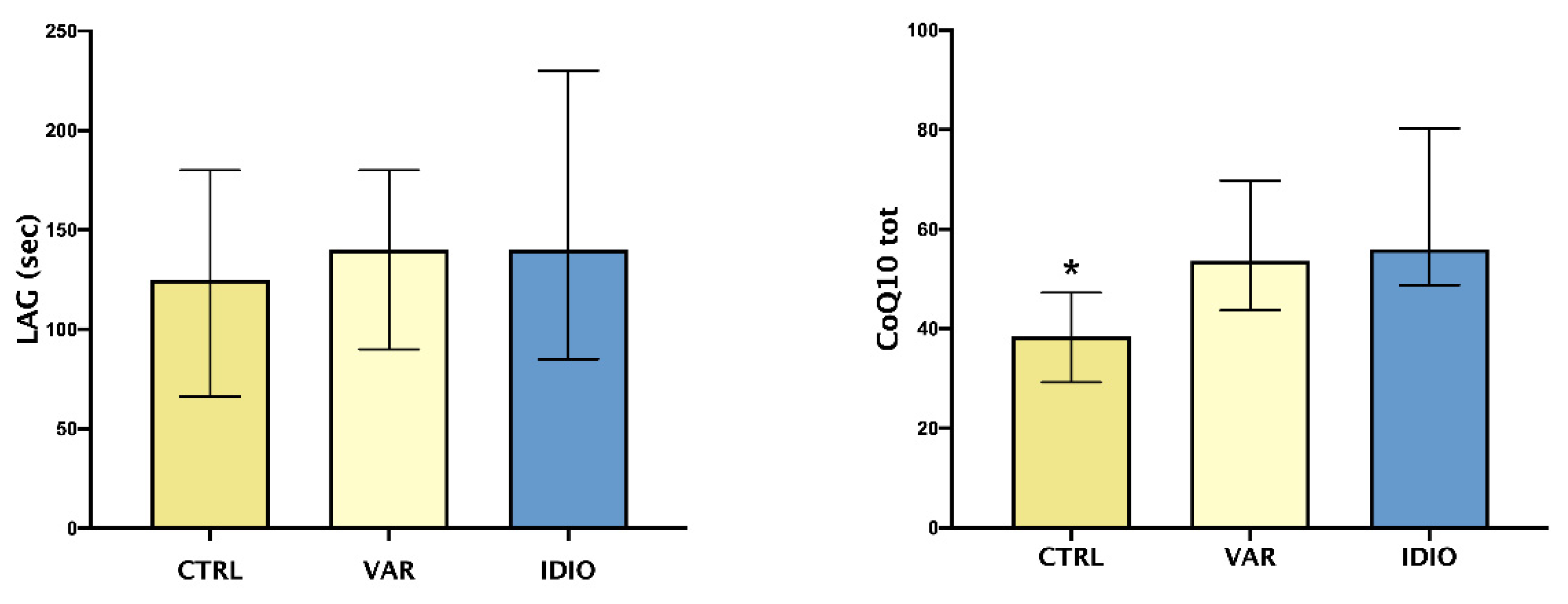
2. Results
3. Discussion
4. Materials and Methods
- A.
- Controls (normozoospermic) 12 patients, median age and interquartile range 34 (33–41) years, BMI 21 (18–23) kg/m2, 33% smokers.
- B.
- Varicocele (VAR), 29 patients, median age and interquartile range 33 (26–37) years, BMI 21 (19–26) kg/m2, 40% smokers.
- C.
- Idiopathic oligo-, asteno-, oligoastenozoospermia (IDIO), 24 patients, median age and interquartile range 37 (33.5–40.5) years, BMI 24 (20–27) kg/m2, 30% smokers. We used the term “idiopathic” referring to seminal abnormalities of unknown etiologies, according to literature indication [51,52,53,54].
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Basile, U.; Gulli, F.; Gragnani, L.; Napodano, C.; Pocino, K.; Rapaccini, G.L.; Mussap, M.; Zignego, A.L. Free Light Chains: Eclectic Multipurpose Biomarker. J. Immunol. Methods 2017, 451, 11–19. [Google Scholar] [CrossRef]
- Napodano, C.; Pocino, K.; Rigante, D.; Stefanile, A.; Gulli, F.; Marino, M.; Basile, V.; Rapaccini, G.L.; Basile, U. Free Light Chains and Autoimmunity. Autoimmun. Rev. 2019, 18, 484–492. [Google Scholar] [CrossRef]
- Boivin, D.; Provençal, M.; Gendron, S.; Ratel, D.; Demeule, M.; Gingras, D.; Béliveau, R. Purification and Characterization of a Stimulator of Plasmin Generation from the Antiangiogenic Agent Neovastat: Identification as Immunoglobulin Kappa Light Chain. Arch. Biochem. Biophys. 2004, 431, 197–206. [Google Scholar] [CrossRef]
- Thiagarajan, P.; Dannenbring, R.; Matsuura, K.; Tramontano, A.; Gololobov, G.; Paul, S. Monoclonal Antibody Light Chain with Prothrombinase Activity. Biochemistry 2000, 39, 6459–6465. [Google Scholar] [CrossRef]
- Paul, S.; Li, L.; Kalaga, R.; Wilkins-Stevens, P.; Stevens, F.J.; Solomon, A. Natural Catalytic Antibodies: Peptide-Hydrolyzing Activities of Bence Jones Proteins and VL Fragment. J. Biol. Chem. 1995, 270, 15257–15261. [Google Scholar] [CrossRef] [Green Version]
- Sun, M.; Gao, Q.S.; Li, L.; Paul, S. Proteolytic Activity of an Antibody Light Chain. J. Immunol. 1994, 153, 5121–5126. [Google Scholar]
- Jokiranta, T.S.; Solomon, A.; Pangburn, M.K.; Zipfel, P.F.; Meri, S. Nephritogenic Lambda Light Chain Dimer: A Unique Human Miniautoantibody against Complement Factor H. J. Immunol. 1999, 163, 4590–4596. [Google Scholar]
- Redegeld, F.A.; Van der Heijden, M.W.; Kool, M.; Heijdra, B.M.; Garssen, J.; Kraneveld, A.D.; Van Loveren, H.; Roholl, P.; Saito, T.; Verbeek, J.S.; et al. Immunoglobulin-Free Light Chains Elicit Immediate Hypersensitivity-like Responses. Nat. Med. 2002, 8, 694–701. [Google Scholar] [CrossRef]
- Meixlsperger, S.; Köhler, F.; Wossning, T.; Reppel, M.; Müschen, M.; Jumaa, H. Conventional Light Chains Inhibit the Autonomous Signaling Capacity of the B Cell Receptor. Immunity 2007, 26, 323–333. [Google Scholar] [CrossRef] [Green Version]
- Foy, S.P.; Matsuuchi, L. Association of B Lymphocyte Antigen Receptor Polypeptides with Multiple Chaperone Proteins. Immunol. Lett. 2001, 78, 149–160. [Google Scholar] [CrossRef]
- Rajkumar, S.V. Updated Diagnostic Criteria and Staging System for Multiple Myeloma. Am. Soc. Clin. Oncol. Educ. Book 2016, 35, e418–e423. [Google Scholar] [CrossRef]
- Napodano, C.; Marino, M.; Stefanile, A.; Pocino, K.; Scatena, R.; Gulli, F.; Rapaccini, G.L.; Delli Noci, S.; Capozio, G.; Rigante, D.; et al. Immunological Role of IgG Subclasses. Immunol. Invest. 2020, 50, 1–18. [Google Scholar] [CrossRef]
- Basile, U.; Vergani, E.; Napodano, C.; Bruno, C.; Marino, M.; Oliva, A.; Gulli, F.; Mancini, A. Evaluation of Free Light Chains of Immunoglobulins in Normal and Pathological Seminal Fluids: Preliminary Data. Andrologia 2022, 54, e14317. [Google Scholar] [CrossRef]
- Agarwal, A.; Prabakaran, S.; Allamaneni, S.S.S.R. Relationship between Oxidative Stress, Varicocele and Infertility: A Meta-Analysis. Reprod. Biomed. Online 2006, 12, 630–633. [Google Scholar] [CrossRef]
- Iwasaki, A.; Gagnon, C. Formation of Reactive Oxygen Species in Spermatozoa of Infertile Patients. Fertil. Steril. 1992, 57, 409–416. [Google Scholar] [CrossRef]
- Allamaneni, S.S.R.; Naughton, C.K.; Sharma, R.K.; Thomas, A.J.; Agarwal, A. Increased Seminal Reactive Oxygen Species Levels in Patients with Varicoceles Correlate with Varicocele Grade but Not with Testis Size. Fertil. Steril. 2004, 82, 1684–1686. [Google Scholar] [CrossRef]
- Agarwal, A. Mechanism, Measurement, and Prevention of Oxidative Stress in Male Reproductive Physiology. Indian J. Exp. Biol. 2005, 43, 963–974. [Google Scholar]
- Mancini, A.; Milardi, D.; Bianchi, A.; Festa, R.; Silvestrini, A.; De Marinis, L.; Pontecorvi, A.; Meucci, E. Increased Total Antioxidant Capacity in Seminal Plasma of Varicocele Patients: A Multivariate Analysis. Arch. Androl. 2007, 53, 37–42. [Google Scholar] [CrossRef]
- Zini, A.; Blumenfeld, A.; Libman, J.; Willis, J. Beneficial Effect of Microsurgical Varicocelectomy on Human Sperm DNA Integrity. Hum. Reprod. 2005, 20, 1018–1021. [Google Scholar] [CrossRef] [Green Version]
- Mancini, A.; Balercia, G. Coenzyme Q 10 in Male Infertility: Physiopathology and Therapy. BioFactors 2011, 37, 374–380. [Google Scholar] [CrossRef]
- Mancini, A.; de Marinis, L.; Oradei, A.; Hallgass, M.E.; Conte, G.; Pozza, D.; Littarru, G.P. Coenzyme Q10 Concentrations in Normal and Pathological Human Seminal Fluid. J. Androl. 1994, 15, 591–594. [Google Scholar] [CrossRef]
- Agarwal, A.; Parekh, N.; Selvam, M.K.P.; Henkel, R.; Shah, R.; Homa, S.T.; Ramasamy, R.; Ko, E.; Tremellen, K.; Esteves, S.; et al. Male Oxidative Stress Infertility (MOSI): Proposed Terminology and Clinical Practice Guidelines for Management of Idiopathic Male Infertility. World J. Mens. Health 2019, 37, 296. [Google Scholar] [CrossRef]
- Mancini, A.; Meucci, E.; Milardi, D.; Giacchi, E.; Bianchi, A.; Pantano, A.L.; Mordente, A.; Martorana, G.E.; De Marinis, L. Seminal Antioxidant Capacity in Pre- and Postoperative Varicocele. J. Androl. 2004, 25, 44–49. [Google Scholar] [CrossRef] [Green Version]
- Alleva, R.; Scararmucci, A.; Mantero, F.; Bompadre, S.; Leoni, L.; Littarru, G.P. The Protective Role of Ubiquinol-10 against Formation of Lipid Hydroperoxides in Human Seminal Fluid. Mol. Aspects Med. 1997, 18, 221–228. [Google Scholar] [CrossRef]
- Groneberg, D.A.; Kindermann, B.; Althammer, M.; Klapper, M.; Vormann, J.; Littarru, G.P.; Döring, F. Coenzyme Q10 Affects Expression of Genes Involved in Cell Signalling, Metabolism and Transport in Human CaCo-2 Cells. Int. J. Biochem. Cell Biol. 2005, 37, 1208–1218. [Google Scholar] [CrossRef]
- Lee, B.J.; Lin, Y.C.; Huang, Y.C.; Ko, Y.W.; Hsia, S.; Lin, P.T. The Relationship between Coenzyme Q10, Oxidative Stress, and Antioxidant Enzymes Activities and Coronary Artery Disease. Sci. World J. 2012, 2012, 792756. [Google Scholar] [CrossRef] [Green Version]
- Nesami, N.B.; Mozaffari-Khosravi, H.; Najarzadeh, A.; Salehifar, E. The Effect of Coenzyme Q10 Supplementation on Pro-Inflammatory Factors and Adiponectin in Mildly Hypertensive Patients: A Randomized, Double-Blind, Placebo-Controlled Trial. Int. J. Vitam. Nutr. Res. 2016, 85, 156–164. [Google Scholar] [CrossRef]
- Mancini, A.; Milardi, D.; Conte, G.; Festa, R.; De Marinis, L.; Littarru, G.P. Seminal Antioxidants in Humans: Preoperative and Postoperative Evaluation of Coenzyme Q10 in Varicocele Patients. Horm. Metab. Res. 2005, 37, 428–432. [Google Scholar] [CrossRef]
- Mancini, A.; Milardi, D.; Conte, G.; Bianchi, A.; Balercia, G.; De Marinis, L.; Littarru, G.P. Coenzyme Q10: Another Biochemical Alteration Linked to Infertility in Varicocele Patients? Metabolism 2003, 52, 402–406. [Google Scholar] [CrossRef]
- Agarwal, A.; Sharma, R.; Harlev, A.; Esteves, S. Effect of Varicocele on Semen Characteristics According to the New 2010 World Health Organization Criteria: A Systematic Review and Meta-Analysis. Asian J. Androl. 2016, 18, 163–170. [Google Scholar] [CrossRef]
- Zeinali, M.; Hadian Amree, A.; Khorramdelazad, H.; Karami, H.; Abedinzadeh, M. Inflammatory and Anti-Inflammatory Cytokines in the Seminal Plasma of Infertile Men Suffering from Varicocele. Andrologia 2017, 49, 12685. [Google Scholar] [CrossRef]
- Pasqualotto, F.F.; Sharma, R.K.; Potts, J.M.; Nelson, D.R.; Thomas, A.J.; Agarwal, A. Seminal Oxidative Stress in Patients with Chronic Prostatitis. Urology 2000, 35, 304–308. [Google Scholar] [CrossRef]
- Schmelzer, C.; Lindner, I.; Rimbach, G.; Niklowitz, P.; Menke, T.; Döring, F. Functions of Coenzyme Q10 in Inflammation and Gene Expression. BioFactors 2008, 32, 179–183. [Google Scholar] [CrossRef]
- Olivieri, F.; Lazzarini, R.; Babini, L.; Prattichizzo, F.; Rippo, M.R.; Tiano, L.; Di Nuzzo, S.; Graciotti, L.; Festa, R.; Brugè, F.; et al. Anti-Inflammatory Effect of Ubiquinol-10 on Young and Senescent Endothelial Cells via MiR-146a Modulation. Free Radic. Biol. Med. 2013, 63, 410–420. [Google Scholar] [CrossRef]
- Farsi, F.; Heshmati, J.; Janani, L.; Irandoost, P.; Mesri Alamdari, N.; Keshtkar, A.; Akbari, A.; Vafa, M. Can Coenzyme Q10 Supplementation Effectively Reduce Human Tumour Necrosis Factor-α and Interleukin-6 Levels in Chronic Diseases? Protocol for a Systematic Review and Meta-Analysis of Randomised Controlled Trials. BMJ Open 2017, 7, e016841. [Google Scholar] [CrossRef]
- Engeli, S.; Feldpausch, M.; Gorzelniak, K.; Hartwig, F.; Heintze, U.; Janke, J.; Möhlig, M.; Pfeiffer, A.F.H.; Luft, F.C.; Sharma, A.M. Association between Adiponectin and Mediators of Inflammation in Obese Women. Diabetes 2003, 52, 942–947. [Google Scholar] [CrossRef] [Green Version]
- Meucci, E.; Milardi, D.; Mordente, A.; Martorana, G.E.; Giacchi, E.; De Marinis, L.; Mancini, A. Total Antioxidant Capacity in Patients with Varicoceles. Fertil. Steril. 2003, 79, 1577–1583. [Google Scholar] [CrossRef]
- Littarru, G.P.; Tiano, L. Clinical Aspects of Coenzyme Q10: An Update. Nutrition 2010, 26, 250–254. [Google Scholar] [CrossRef]
- Littarru, G.P.; Tiano, L. Bioenergetic and Antioxidant Properties of Coenzyme Q10: Recent Developments. Mol. Biotechnol. 2007, 37, 31–37. [Google Scholar] [CrossRef]
- Zhai, J.; Bo, Y.; Lu, Y.; Liu, C.; Zhang, L. Effects of Coenzyme Q10 on Markers of Inflammation: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0170172. [Google Scholar] [CrossRef] [Green Version]
- Balercia, G.; Mosca, F.; Mantero, F.; Boscaro, M.; Mancini, A.; Ricciardo-Lamonica, G.; Littarru, G.P. Coenzyme Q(10) Supplementation in Infertile Men with Idiopathic Asthenozoospermia: An Open, Uncontrolled Pilot Study. Fertil. Steril. 2004, 81, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Balercia, G.; Buldreghini, E.; Vignini, A.; Tiano, L.; Paggi, F.; Amoroso, S.; Ricciardo-Lamonica, G.; Boscaro, M.; Lenzi, A.; Littarru, G.P. Coenzyme Q10 Treatment in Infertile Men with Idiopathic Asthenozoospermia: A Placebo-Controlled, Double-Blind Randomized Trial. Fertil. Steril. 2009, 91, 1785–1792. [Google Scholar] [CrossRef] [PubMed]
- Chandra, A.; Copen, C.E.; Stephen, E.H. Infertility Service Use in the United States: Data From the National Survey of Family Growth, 1982–2010. Natl. Health Stat. Rep. 2014, 73, 1–21. [Google Scholar]
- Kumar, N.; Singh, A. Trends of Male Factor Infertility, an Important Cause of Infertility: A Review of Literature. J. Hum. Reprod. Sci. 2015, 8, 191. [Google Scholar] [CrossRef] [PubMed]
- Barbonetti, A.; Calogero, A.E.; Balercia, G.; Garolla, A.; Krausz, C.; Vignera, S.; La Lombardo, F.; Jannini, E.A.; Maggi, M.; Lenzi, A.; et al. The Use of Follicle Stimulating Hormone (FSH) for the Treatment of the Infertile Man: Position Statement from the Italian Society of Andrology and Sexual Medicine (SIAMS). J. Endocrinol. Invest. 2018, 41, 1107–1122. [Google Scholar] [CrossRef]
- Agarwal, A.; Sharma, R.; Roychoudhury, S.; Du Plessis, S.; Sabanegh, E. MiOXSYS: A Novel Method of Measuring Oxidation Reduction Potential in Semen and Seminal Plasma. Fertil. Steril. 2016, 106, 566–573. [Google Scholar] [CrossRef] [Green Version]
- Friebe, K.; Bohring, C.; Skrzypek, J.; Krause, W. Levels of Interleukin-6 and Interleukin-8 in Seminal Fluid of Men Attending an Andrological Clinic. Andrologia 2003, 35, 126–129. [Google Scholar] [CrossRef]
- Eggert-Kruse, W.; Kiefer, I.; Beck, C.; Demirakca, T.; Strowitzki, T. Role for Tumor Necrosis Factor Alpha (TNF-α) and Interleukin 1-Beta (IL-1β) Determination in Seminal Plasma during Infertility Investigation. Fertil. Steril. 2007, 87, 810–823. [Google Scholar] [CrossRef]
- Castiglione, R.; Salemi, M.; Vicari, L.O.; Vicari, E. Relationship of Semen Hyperviscosity with IL-6, TNF-α, IL-10 and ROS Production in Seminal Plasma of Infertile Patients with Prostatitis and Prostato-Vesiculitis. Andrologia 2014, 46, 1148–1155. [Google Scholar] [CrossRef]
- Ferlin, A.; Calogero, A.E.; Krausz, C.; Lombardo, F.; Paoli, D.; Rago, R.; Scarica, C.; Simoni, M.; Foresta, C.; Rochira, V.; et al. Management of Male Factor Infertility: Position Statement from the Italian Society of Andrology and Sexual Medicine (SIAMS): Endorsing Organization: Italian Society of Embryology, Reproduction, and Research (SIERR). J. Endocrinol. Invest. 2022, 45, 1085–1113. [Google Scholar] [CrossRef]
- Grimes, D.A.; Lopez, L.M. “Oligozoospermia” “Azoospermia” and Other Semen-Analysis Terminology: The Need for Better Science. Fertil. Steril. 2007, 88, 1491–1494. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.-C.; Huang, Y.-F. Diagnosis and Treatment of Idiopathic Semen Quality Abnormalities. Zhonghua Nan Ke Xue 2012, 18, 3–10. [Google Scholar] [PubMed]
- Koukkou, E.; Billa, E.; Kapolla, N.; Pappa, A.; Venaki, E.; Andreou, L.; Nicopoulou, S.C.; Adamopoulos, D.A. An Empiric Treatment for Idiopathic Oligozoospermia Revisited: A 20-Year Investigative Saga. Andrologia 2012, 44, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Maretti, C.; Cavallini, G. The Association of a Probiotic with a Prebiotic (Flortec, Bracco) to Improve the Quality/Quantity of Spermatozoa in Infertile Patients with Idiopathic Oligoasthenoteratospermia: A Pilot Study. Andrology 2017, 5, 439–444. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Vol (mL) | C (×106/mL) | Total Count (×106) | PR (%) | n (%) | |
|---|---|---|---|---|---|
| Controls | 3 (3–4) | 43 (27.4–56.5) | 120 (81–212) | 39 (34.5–45) | 6.4 (5.2–7.9) |
| Varicocele | 4 (3–4.4) | 43 (17.50–67) | 149 (80–216) | 20 (9–31) * | 5.3 (4.3–5.8) |
| Idiopathic | 4 (3–4.25) | 22.50 (8–61.3) *° | 66 (30–294) | 19.50 (7–23.25) * | 4.9 (3.4–5.7) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bruno, C.; Basile, U.; Vergani, E.; Napodano, C.; Oliva, A.; Gulli, F.; Meucci, E.; Silvestrini, A.; Orlando, P.; Silvestri, S.; et al. Inflammation and Oxidative Stress in Seminal Plasma: Search for Biomarkers in Diagnostic Approach to Male Infertility. J. Pers. Med. 2022, 12, 857. https://doi.org/10.3390/jpm12060857
Bruno C, Basile U, Vergani E, Napodano C, Oliva A, Gulli F, Meucci E, Silvestrini A, Orlando P, Silvestri S, et al. Inflammation and Oxidative Stress in Seminal Plasma: Search for Biomarkers in Diagnostic Approach to Male Infertility. Journal of Personalized Medicine. 2022; 12(6):857. https://doi.org/10.3390/jpm12060857
Chicago/Turabian StyleBruno, Carmine, Umberto Basile, Edoardo Vergani, Cecilia Napodano, Alessandro Oliva, Francesca Gulli, Elisabetta Meucci, Andrea Silvestrini, Patrick Orlando, Sonia Silvestri, and et al. 2022. "Inflammation and Oxidative Stress in Seminal Plasma: Search for Biomarkers in Diagnostic Approach to Male Infertility" Journal of Personalized Medicine 12, no. 6: 857. https://doi.org/10.3390/jpm12060857
APA StyleBruno, C., Basile, U., Vergani, E., Napodano, C., Oliva, A., Gulli, F., Meucci, E., Silvestrini, A., Orlando, P., Silvestri, S., Tiano, L., & Mancini, A. (2022). Inflammation and Oxidative Stress in Seminal Plasma: Search for Biomarkers in Diagnostic Approach to Male Infertility. Journal of Personalized Medicine, 12(6), 857. https://doi.org/10.3390/jpm12060857











