Abstract
Background: There have been concerns regarding increased perioperative mortality, length of hospital stay, and rates of graft loss in kidney transplant recipients with functional limitations. The application of machine learning consensus clustering approach may provide a novel understanding of unique phenotypes of functionally limited kidney transplant recipients with distinct outcomes in order to identify strategies to improve outcomes. Methods: Consensus cluster analysis was performed based on recipient-, donor-, and transplant-related characteristics in 3205 functionally limited kidney transplant recipients (Karnofsky Performance Scale (KPS) < 40% at transplant) in the OPTN/UNOS database from 2010 to 2019. Each cluster’s key characteristics were identified using the standardized mean difference. Posttransplant outcomes, including death-censored graft failure, patient death, and acute allograft rejection were compared among the clusters Results: Consensus cluster analysis identified two distinct clusters that best represented the clinical characteristics of kidney transplant recipients with limited functional status prior to transplant. Cluster 1 patients were older in age and were more likely to receive deceased donor kidney transplant with a higher number of HLA mismatches. In contrast, cluster 2 patients were younger, had shorter dialysis duration, were more likely to be retransplants, and were more likely to receive living donor kidney transplants from HLA mismatched donors. As such, cluster 2 recipients had a higher PRA, less cold ischemia time, and lower proportion of machine-perfused kidneys. Despite having a low KPS, 5-year patient survival was 79.1 and 83.9% for clusters 1 and 2; 5-year death-censored graft survival was 86.9 and 91.9%. Cluster 1 had lower death-censored graft survival and patient survival but higher acute rejection, compared to cluster 2. Conclusion: Our study used an unsupervised machine learning approach to characterize kidney transplant recipients with limited functional status into two clinically distinct clusters with differing posttransplant outcomes.
1. Introduction
Functional status, or the capacity to perform daily activities to meet basic needs and maintain health and wellbeing, is recognized as a useful tool for evaluating patients in various clinical settings, including patients undergoing organ transplantation [1,2,3,4]. Among kidney transplant recipients, significant associations between low functional status and poor outcomes after kidney transplant have been reported, including increased mortality [5,6,7,8,9]. In the United States (U.S.), the Karnofsky Performance Scale (KPS), a physician-reported measure of functional status ranging from 0 to 100%, [10] is routinely collected among transplant candidates and recipients and has become a requirement by the Organ Procurement and Transplantation Network (OPTN) for risk adjustment of transplant outcomes [4,11,12,13,14].
Prior studies have demonstrated an association between low KPS scores and poor outcomes after kidney transplantation, including mortality and all-cause graft loss [4,11]. Additionally, recipients with low functional scores are often found to be ineligible for kidney transplantation due to a combination of limited transplant resources and anticipation of a lessened survival benefit post kidney transplantation. As a result, the majority of kidney transplant surgeries in the U.S. are performed for kidney transplant recipients with satisfactory functional status [11]. Only 3% of kidney transplant surgeries are performed for patients with KPS of ≤40% [11]. While patients with a low functional status have a higher risk of post-operative complications and death following kidney transplant as compared to those with higher physical functioning scores, this risk is likely still less than remaining on dialysis [1,11,15]. Furthermore, kidney transplant patients, including recipients with low functional status, are likely heterogenous, and there are many factors, including recipient, donor, and transplant-related variables, that can result in varying outcomes contrary to what has historically been reported in the literature [11,16,17].
Artificial intelligence and machine learning (ML) have been utilized to provide clinical decision support tools and individualize patient care, including in organ transplantation [18,19,20,21,22,23,24]. Unsupervised consensus clustering is ML applied to discover novel data patterns and distinct subtypes [25,26,27]. It can discover similarities and heterogeneities among various data variables and distinguish them into clinically meaningful clusters [25,26]. Recent studies have demonstrated that distinct subtypes identified by the ML consensus clustering approach can forecast different clinical outcomes [28,29]. Given data on characteristics of kidney transplant recipients with KPS of ≤40% in the U.S. are limited, the application of ML consensus clustering approach may provide a novel understanding of unique phenotypes of disabled kidney transplant recipients with distinct outcomes in order to identify strategies to improve their outcomes.
In this study, we analyzed the United Network for Organ Sharing database (UNOS)/OPTN database from 2010 through 2019 using an unsupervised ML clustering approach to identify distinct clusters of kidney transplant recipients whose functional status at transplant were impaired (KPS of ≤40%) and assess clinical outcomes among these unique clusters.
2. Methods
2.1. Data Source and Study Population
This study was conducted using the UNOS/OPTN database to screen adult kidney-only transplant recipients in the United States from 2010 to 2019 with low functional status. Low functional status recipients were defined as having a KPS of ≤40% at the time of kidney transplantation. This study received approval from the Mayo Clinic Institutional Review Board (IRB number 21-007698).
2.2. Data Collection
The following recipient-, donor-, and transplant-related variables in the OPTN/UNOS database were abstracted for inclusion in cluster analysis: recipient age, sex, race, body mass index (BMI), kidney retransplant, dialysis duration, causes of end-stage kidney disease, comorbidities, panel reactive antibody (PRA), hepatitis C, hepatitis B and human immunodeficiency virus (HIV) serostatus, KPS, working income, insurance, US residency status, education, serum albumin, kidney donor type, ABO incompatibility, donor age, sex, race, history of hypertension in donor, kidney donor profile index (KDPI), HLA mismatch, cold ischemia time, kidney on pump, delay graft function, allocation type, Ebstein–Barr virus (EBV) and Cytomegalovirus (CMV) status, induction, and maintenance immunosuppression.
Functional status at the time of transplant for kidney transplant recipients was defined by center-reported KPS. KPS, as shown in Table S1, is a categorical classification system with progressive but arbitrary increase in assigned performance status at 10% intervals without use of the intervening numbers, so it was treated as ordinal for statistical purposes. Patients were further categorized into four groups: normal (80–100%), capable of self-care (70%), requires assistance (50–60%), and disabled (10–40%). Among those with KPS of ≤40%, detailed definitions as following: KPS of 40%: disabled and requires special care and assistance; KPS of 30%: severely disabled, hospital admission is indicated although death is not imminent; KPS of 20%: very sick, hospital admission and active supportive treatments are necessary; KPS of 10%: moribund, fatal processes progress rapidly. All extracted variables had missing data less than 5% (Table S2). Missing data were imputed through multivariable imputation by chained equation (MICE) method [30].
2.3. Clustering Analysis
Unsupervised ML was applied by conducting a consensus clustering approach to categorize clinical phenotypes of functionally disabled kidney transplant recipients (KPS at transplant of ≤40%) [31]. A pre-specified subsampling parameter of 80% with 100 iterations and the number of potential clusters (k) ranging from 2 to 10 were used to avoid producing an excessive number of clusters that would not be clinically useful. The optimal number of clusters was determined by examining the consensus matrix (CM) heat map, cumulative distribution function (CDF), cluster-consensus plots with the within-cluster consensus scores, and the proportion of ambiguously clustered pairs (PAC). The within-cluster consensus score, ranging between 0 and 1, was defined as the average consensus value for all pairs of individuals belonging to the same cluster [32]. A value closer to one indicates better cluster stability. PAC, ranging between 0 and 1, was calculated as the proportion of all sample pairs with consensus values falling within the predetermined boundaries [33]. A value closer to zero indicates better cluster stability [33]. The PAC was calculated using two criteria (1) the strict criteria consisting of a predetermined boundary of (0, 1), where a pair of individuals who had a consensus value >0 or <1 was considered ambiguously clustered, and (2) the relaxed criteria consisting of a predetermined boundary of (0.1, 0.9), where a pair of individuals who had consensus value >0.1 or <0.9 was considered ambiguously clustered [33]. The detailed consensus cluster algorithms used in this study for reproducibility are provided in Supplementary Materials.
Outcomes
Posttransplant outcomes consisted of death-censored graft survival, patient survival within 1 and 5 years after kidney transplant, and acute allograft rejection within 1 year after kidney transplant. We defined death-censored graft failure as the need for dialysis or kidney retransplant, while censoring patients for death or at last follow-up date reported to the OPTN/UNOS database.
2.4. Statistical Analysis
After an individual functionally impaired kidney transplant patient was assigned a cluster using the consensus clustering approach, statistical analyses were subsequently performed to compare the characteristics and outcomes among the assigned clusters. The differences in clinical characteristics among the assigned clusters were tested using Student’s t-test for continuous variables and Chi-squared test for categorical variables. The key characteristics of each cluster were determined using the standardized mean difference between each cluster and the overall cohort with the cut-off of >0.3.
The difference in posttransplant outcomes were evaluated among the assigned clusters. The hazard ratios (HR) for death-censored graft failure and patient death based on the assigned clusters were obtained using Cox proportional hazard analysis. Because the OPTN/UNOS database did not specify the date of allograft rejection occurrence, the odds ratio (OR) for 1-year allograft rejection based on the assigned clusters was obtained using logistic regression analysis. The hazard ratio or odds ratio were not adjusted for the between-cluster difference in clinical characteristics since an unsupervised consensus clustering approach was conducted to purposefully generate clinically distinct clusters.
All analyses were carried out using R, version 4.0.3 (RStudio, Inc., Boston, MA, USA; http://www.rstudio.com/, accessed on 21 July 2021), ConsensusClusterPlus package (version 1.46.0) for consensus clustering analysis, and the MICE command in R for multivariable imputation by chained equation [30].
3. Results
There were 158,367 kidney transplant recipients from 2010 to 2019 in the United States. Of these, 3205 (2%) had severely limited functional status with KPS ≤40% at the time of kidney transplant. Therefore, consensus clustering analysis was performed in a total of 3205 functionally impaired kidney transplant recipients. Table 1 shows recipient-, donor-, and transplant-related characteristics of included patients. Most of the included patients (90%) had KPS of 40%.

Table 1.
Clinical characteristics according to clusters of functionally disabled kidney transplant recipients.
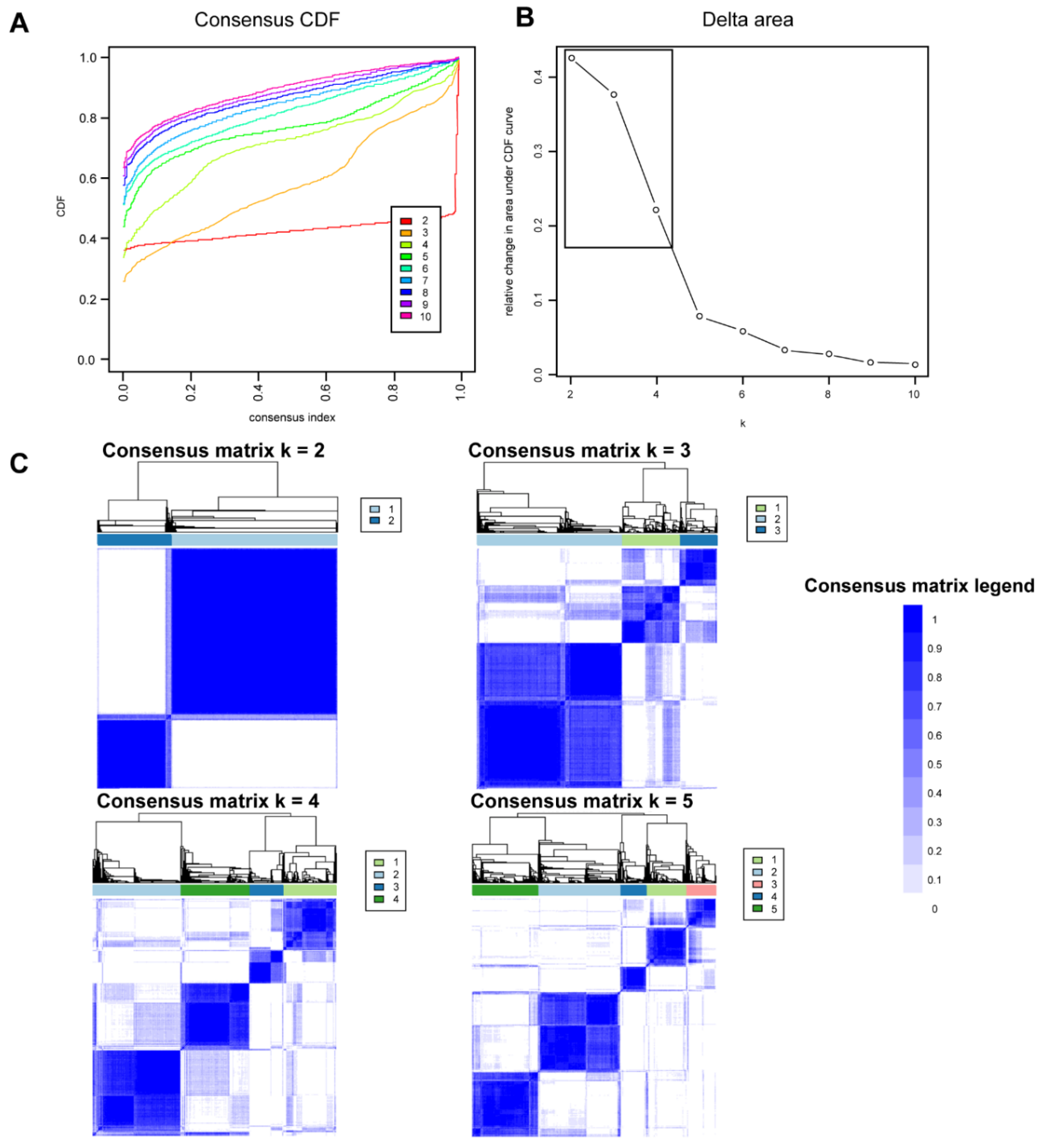
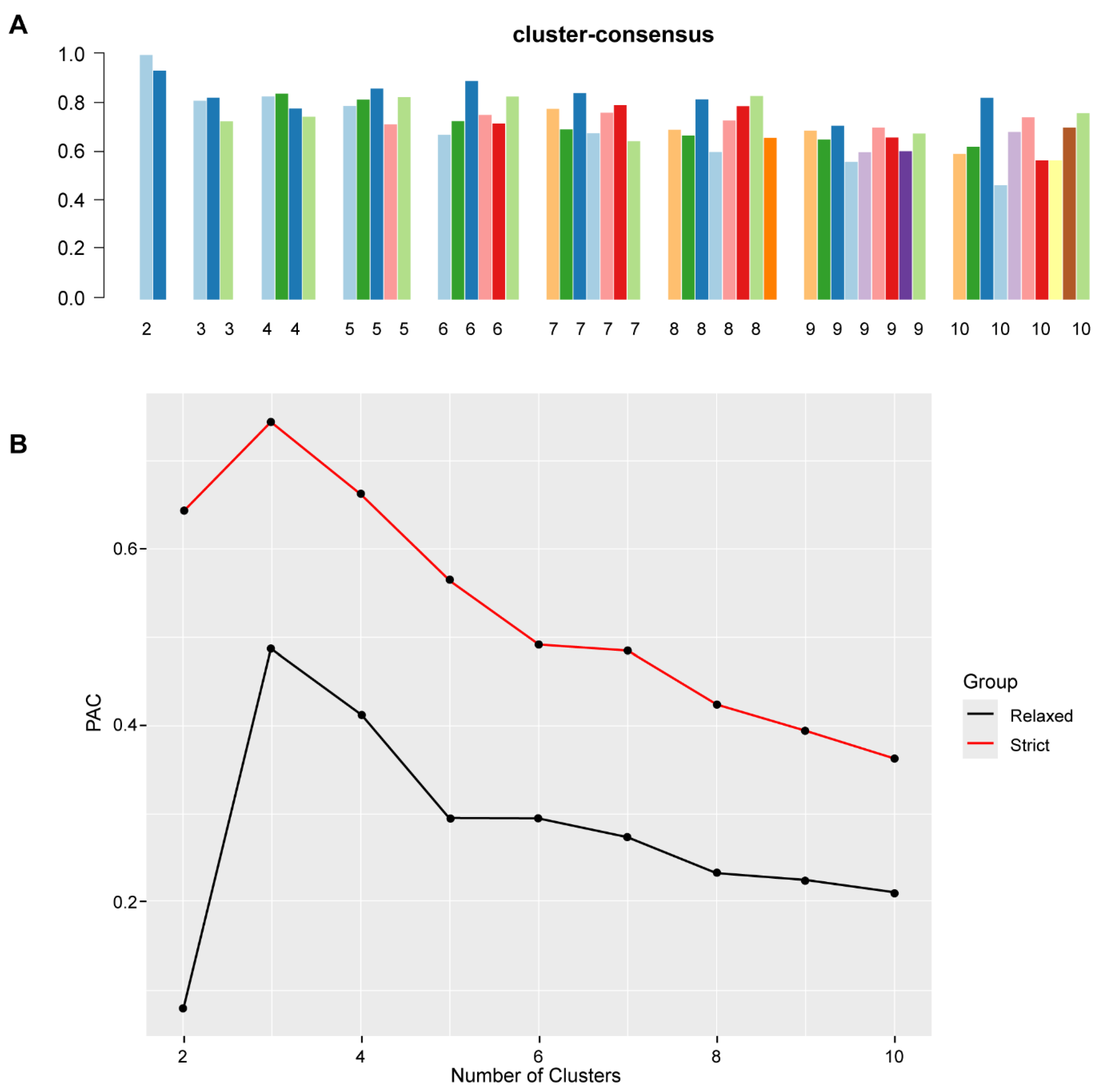
Figure 1A shows the CDF plot consensus distributions for each cluster of functionally disabled kidney transplant recipients. The CDF curve showed the best stability for 2 clusters with the curve being flat in the middle part. The delta area plot shows the relative change in the area under the CDF curve (Figure 1B). The largest changes in area occurred between k = 2 and k = 4, at which point the relative increase in area became noticeably smaller. As shown in the CM heat map (Figure 1C, Supplementary Figures S1–S9), the ML algorithm identified cluster 2 with clear boundaries, indicating good cluster stability over repeated iterations. The mean cluster consensus score was highest in cluster 2 (Figure 2A). In addition, favorable low PACs by both strict and relaxed criteria were demonstrated for 2 clusters (Figure 2B). Thus, using baseline variables at the time of transplant, the consensus clustering analysis identified 2 clusters that best represented the data pattern of our recipients with the KPS of ≤40% at kidney transplant.
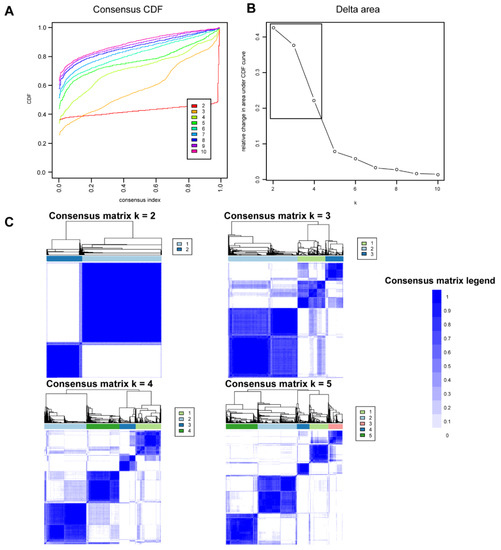
Figure 1.
(A) CDF plot displaying consensus distributions for each k. (B) Delta area plot reflecting the relative changes in the area under the CDF curve. (C) Consensus matrix heat map depicting consensus values on a white to blue color scale of each cluster.
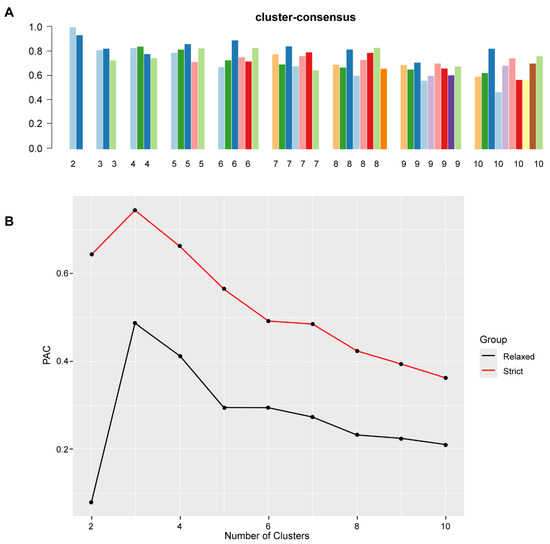
Figure 2.
(A) The bar plot represents the mean consensus score for different numbers of clusters (K ranges from two to ten). (B) The PAC values assess ambiguously clustered pairs.
3.1. Clinical Characteristics of Each Functionally Impaired Kidney Transplant Clusters
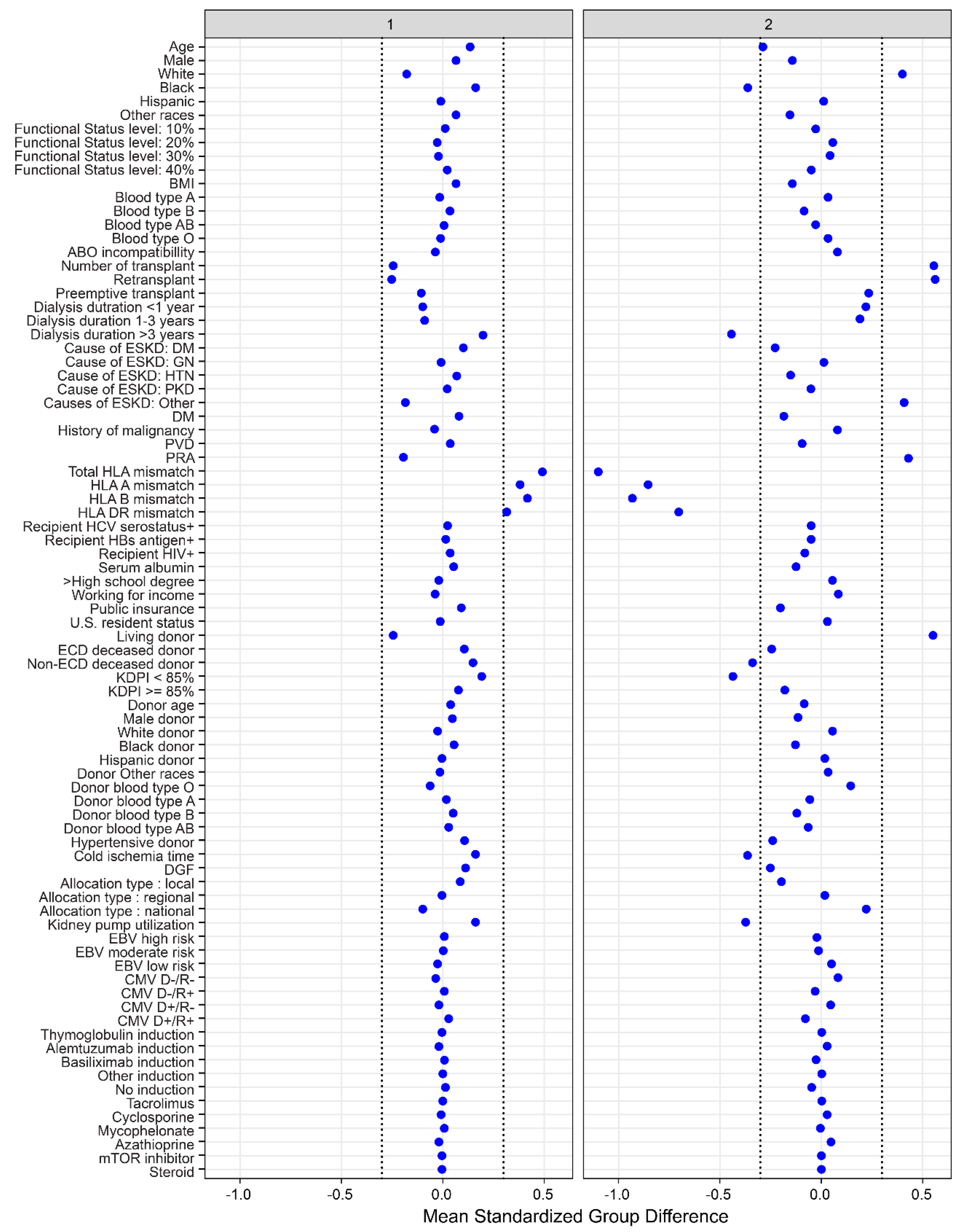
There were two distinct clinical clusters identified using consensus clustering analysis. Cluster 1 had 2216 patients (69%), whereas cluster 2 had 989 patients (31%). There were several clinical characteristics between the two clusters, as shown in Table 1 and Figure 3. Kidney transplant recipients in cluster 1 were older in age and more likely to be on dialysis longer prior to transplant and receive a locally allocated standard KDPI deceased donor kidney. In contrast, cluster 2 recipients were younger, had shorter dialysis duration, were more likely to be retransplants, and receive living donors with a lower number of HLA mismatches. Cluster 2 recipients had a higher PRA, less cold ischemia time, and lower proportion of machine-perfused kidneys.
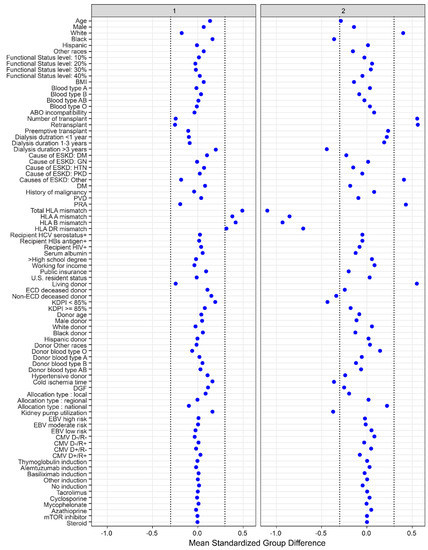
Figure 3.
The standardized differences across two clusters for each of baseline parameters. The x axis is the standardized differences value, and the y axis shows baseline parameters. The dashed vertical lines represent the standardized differences cutoffs of <−0.3 or >0.3. Abbreviations: BMI: Body mass index, CMV: Cytomegalovirus, D: Donor, DGF: Delayed graft function, DM: Diabetes mellitus, EBV: Epstein–Barr virus, ECD: Extended criteria donor, ESKD: End stage kidney disease, GN: Glomerulonephritis, HBs: Hepatitis B surface, HCV: Hepatitis C virus, HIV: Human immunodeficiency virus, HLA: Human leukocyte antigen, HTN: Hypertension, KDPI: Kidney donor profile index, mTOR: Mammalian target of rapamycin, PKD: Polycystic kidney disease, PRA: Panel reactive antibody, PVD: Peripheral vascular disease, R: Recipient.
Overall, very few recipients in clusters 1 and 2 had a working income (8%). Less than half (43% cluster 1, 47% cluster 2) had an undergraduate education or higher. Despite having a low functional status, the majority of recipients received young non-ECD standard KDPI deceased donor kidneys. Only 12% received kidney transplants from ECD donors; high KDPI kidneys were used in 5% of transplants. Thymoglobulin was the most commonly used induction agent (59%).
Supplementary Figure S10 and Table S3 showed the proportion of cluster 1 and cluster 2 based on the OPTN regions. OPTN Regions 7 (12.6%, n = 404), 2 (10.2%, n = 382), 5 (9.3%, n = 299) and 10 (9.2%, n = 296) had the highest number of cluster 1 recipients. Regions 2 (6.0%, n = 193), 2 (7.1%, n = 226), and 10 (3.7%, n = 117) had the highest number of cluster 2 recipients. Regions 7 (19.7%), 5 (13.4%), and 10 (12.9%) had the highest number of recipients from clusters 1 and 2 while regions 6 (0.4%), 1 (2.6%), and 11 (3.8%) had the overall lowest number.
3.2. Posttransplant Outcomes of Each Functionally Disabled Kidney Transplant Cluster
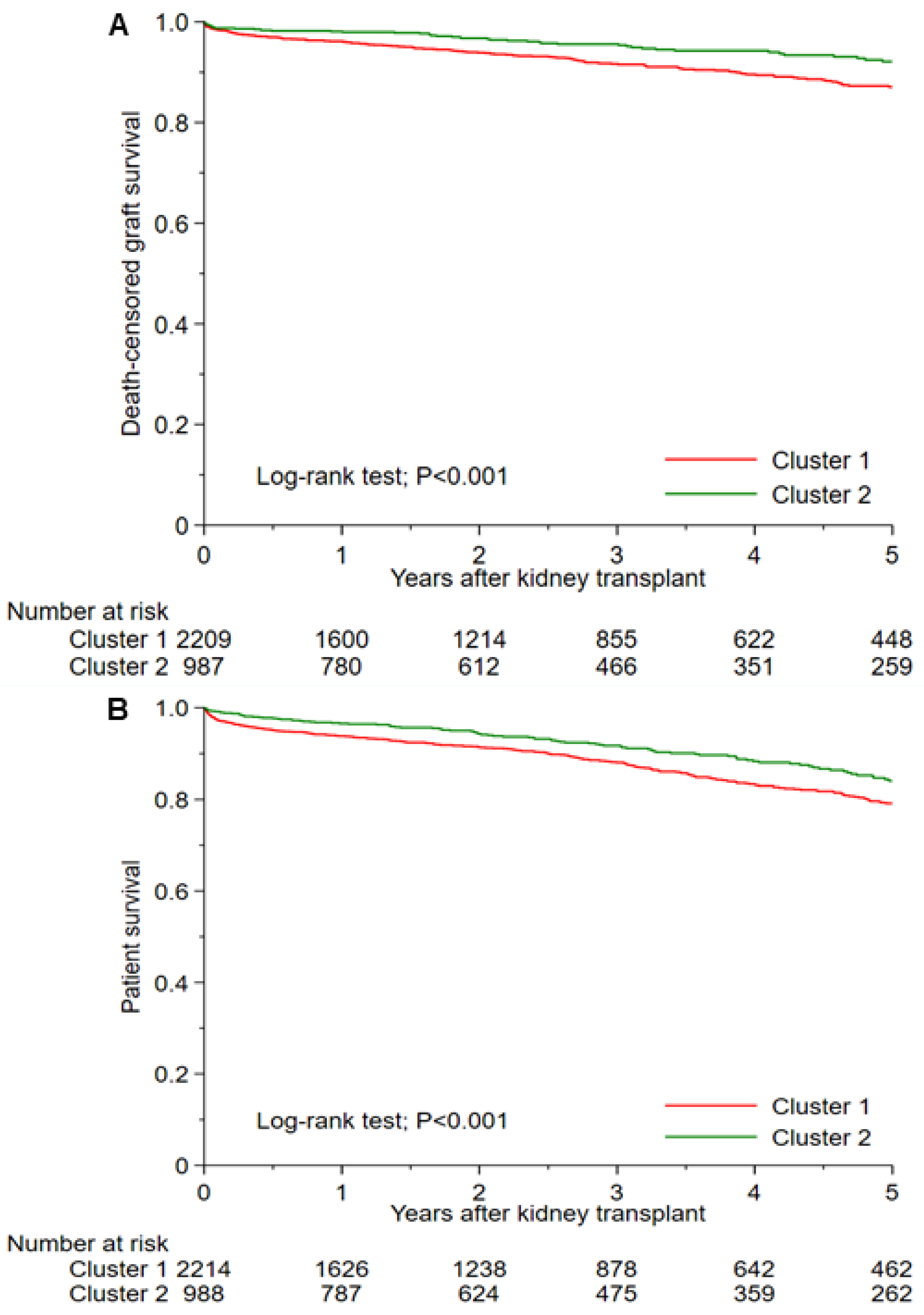
Table 2 shows cluster-based posttransplant outcomes. The 1-year and 5-year death-censored graft survival was 95.9 and 86.9% in cluster 1, and 97.9 and 91.9% in cluster 2 (p < 0.001) (Figure 4A). Cluster 1 had lower death-censored graft survival than cluster 2 with HR of 1.92 (95% CI 1.21–3.22) at 1 year and 1.75 (95% CI 1.28–2.40) at 5 years. The 1-year and 5-year patient survival was 93.7 and 79.1% in cluster 1 and 96.5 and 83.9% in cluster 2 (p < 0.001) (Figure 4B). Cluster 1 had lower survival than cluster 2 with HR of 1.82 (95% CI 1.26–2.72) at 1 year and 1.45 (95% CI 1.15–1.82) at 5 years. The incidence of 1-year acute allograft rejection was 6.7% in cluster 1, and 3.8% in cluster 2 (p = 0.001). Cluster 1 had more acute allograft rejection occurred within 1 year after kidney transplant than cluster 2 with OR of 1.80 (95% CI 1.25–2.60).

Table 2.
Post-transplant outcomes according to the clusters of functionally disabled kidney transplant recipients.
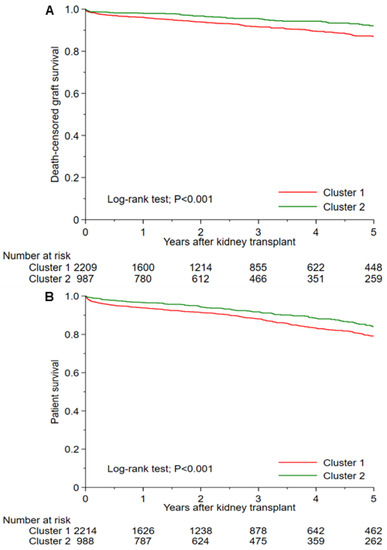
Figure 4.
(A) Death-censored graft failure and (B) patient survival after kidney transplant among two unique clusters of functionally disabled kidney transplant recipients.
4. Discussion
Studies have demonstrated poor clinical outcomes after kidney transplant among patients with impaired functional status including reduced patient and allograft survival [1,5,7,8,15,16,17]. As a result, in combination with limited transplant resources, kidney transplant surgeries are uncommonly performed for kidney transplant recipients with severely limited functional status [11]. However, not all kidney transplant recipients with low functional status, including those with KPS ≤40% at the time of transplant, have poor outcomes. Moreover, even for these high-risk recipients, their overall mortality risk remains less when compared to remaining on dialysis [1,11,15]. In this study, unsupervised ML consensus clustering was successfully used to identify two groups of kidney transplant recipients with limited functional status in the U.S. Although small in overall number, these recipients have distinct characteristics and satisfactory post-transplant outcomes and reflect a unique subgroup of kidney transplant recipients.
The majority (91% in cluster 1 vs. 89% in cluster 2) of patients had KPS of 40% at the time transplant; very few recipients had a KPS <40% (10%, n = 308). The overall average recipient age was 51 years. Very few recipients in clusters 1 and 2 had a working income (8%), and less than half (43% cluster 1, 47% cluster 2) had an undergraduate education or higher. Despite having a low functional status, the majority of recipients received young non-ECD standard KDPI deceased donor kidneys. Only 12% received kidney transplants from ECD donors; high KDPI kidneys were used in 5% of transplants. Thymoglobulin was the most commonly used induction agent for both clusters (59%).
Despite the above similarities between the two clusters, there were significant differences in baseline characteristics. Cluster 1 recipients were older compared to cluster 2 (mean 53 years vs. 47 years). Similarly, there was a striking difference in the racial mixture of these recipients; while the number of non-white recipients was low in both groups, cluster 2 had a higher number of white recipients (67 vs. 39%) and significantly lower Black recipients (13 vs. 36%). Compared to cluster 1, cluster 2 recipients had a higher proportion of living donor transplants (48 vs. 13%), less ABDR mismatches (2 vs. 5), and lower cold ischemia times (10 vs. 15 h). The higher number of HLA matches for cluster 2 likely is reflective of living-related kidney donation.
Compared to cluster 2, cluster 1 recipients had a 1.75-fold increased risk for five-year death censored graft failure and 1.45-fold higher five-year increased risk of death. Inferior outcomes in cluster 1 could potentially be explained by older age and lower rates of preemptive and living donor transplantation. While cluster 2 had higher rate of retransplantation and both clusters received comparable immunosuppression, one-year acute rejection was higher in cluster 1. This finding is possibly a reflection of higher HLA mismatches and longer cold ischemia time in cluster 1 recipients although the observed rates of rejection within both clusters were within the expected standard for kidney transplantation. Higher HLA mismatches are well-known risk factor of acute rejection [34,35,36]. In addition, longer cold ischemia time can lead to increased ischemia reperfusion injury resulting in increased endothelial damage and exposure to donor HLA antigens, and acute rejection [37,38,39,40]. It is also possible that cluster 2 recipients had access to better support and more resources as compared to cluster 1 recipients, given their clinical characteristics of shorter dialysis time and access to living donation.
To our knowledge, this is the first ML clustering approach successfully applied to kidney transplant recipients low KPS scores in the U.S. Through our use of ML clustering approach, without human intervention or assistance, we were able to identify two distinct clusters of functionally disabled kidney transplant recipients. Cluster 2 recipients do well and have excellent outcomes, which, in itself, is not commonly reported for functionally disabled kidney transplant recipients. These findings from ML clustering approach provide additional understanding towards individualized medicine and opportunities to improve care for vulnerable groups of functionally disabled kidney transplant recipients. Furthermore, there are different cluster distributions among 11 geographic OPTN regions. Regions 7 (19.7%), 5 (13.4%), and 10 (12.9%) had the highest number of recipients from clusters 1 and 2 while regions 6 (0.4%), 1 (2.6%), and 11 (3.8%) had the overall lowest number. When looking at geographic distribution by cluster regions 7 (12.6%), 2 (10.2%), 5 (9.3%), and 10 (9.2%) had the highest number of cluster 1 recipients and regions 2 (6.0%), 7 (7.1%), and 10 (3.7%) had the highest number of cluster 2 recipients.
Inherent to the source of these data, which came from the UNOS database, there are some limitations to this study. Although individuals were able to be identified as having a low functional status, KPS ≤40%, there is a lack of additional detail regarding these recipients specific to what their limitations were, criteria that centers used to determine their suitability for transplant and information regarding caregiver support. The mean recipient age was relatively low for both clusters 1 and 2 and implies that the nature of the low functional status of these individuals may differ, compared to what is observed for older kidney failure patients with low functional status. Only 39% had diabetes, and 15% had peripheral vascular disease. In addition, we lacked information on interventions and management strategies used by different centers for recipients with low functional status [4,41]. It is also unknown if cluster 2 recipients who received living donors were only offered transplantation through this option. Thus, future studies are required to assess the impacts of interventions and management strategies on changes in functional status and posttransplant outcomes among these two different clusters of functionally disabled kidney transplant recipients. While kidney transplant recipients with lower functional status had an increased mortality after kidney transplant when compared to those with higher functional status [1,11,15], the findings of our study provide further insights into the different allograft and patient outcomes among the unique phenotypic subtypes of kidney transplant recipients with lower functional status, in which those with cluster 1 subtype had the worst posttransplant outcomes in term of death-censored graft failure, death, and allograft rejection. Patients with functionally disabled kidney transplant recipients have different characteristics and should be counseled about their risk of lower posttransplant survival differently.
5. Conclusions
In summary, our ML clustering approach successfully identified two unique phenotypic clusters of kidney transplant recipients with low functional status in the U.S. Each cluster had different characteristics with distinct posttransplant outcomes consisting of allograft rejection, allograft loss, and patient mortality. These findings from ML clustering approach provide additional understanding towards individualized medicine and opportunities to improve transplant opportunities for kidney transplant recipients with low functional status. In addition, our study also showed a varying geographic distribution of these low functional status kidney transplant recipients in the different OPTN Regions in the U.S. Future studies are required to identify strategies to improve outcomes among kidney transplant recipients with lower functional status, especially those with cluster 1 subtype.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm12060859/s1, Table S1: Karnofsky Performance Score definitions. Table S2: The number and percentages of missing data. Table S3: Proportion of clusters according to the regions. Figure S1: Consensus matrix heat map (k = 2) depicting consensus values on a white to blue color scale of each cluster. Figure S2: Consensus matrix heat map (k = 3) depicting consensus values on a white to blue color scale of each cluster. Figure S3. Consensus matrix heat map (k = 4) depicting consensus values on a white to blue color scale of each cluster. Figure S4: Consensus matrix heat map (k = 5) depicting consensus values on a white to blue color scale of each cluster. Figure S5: Consensus matrix heat map (k = 6) depicting consensus values on a white to blue color scale of each cluster. Figure S6: Consensus matrix heat map (k = 7) depicting consensus values on a white to blue color scale of each cluster. Figure S7: Consensus matrix heat map (k = 8) depicting consensus values on a white to blue color scale of each cluster. Figure S8: Consensus matrix heat map (k = 9) depicting consensus values on a white to blue color scale of each cluster. Figure S9: Consensus matrix heat map (k = 10) depicting consensus values on a white to blue color scale of each cluster. Figure S10: A. Proportion of clusters according to the regions. B. OPTN regions.
Author Contributions
Conceptualization, C.T., C.C.J., W.K., P.V., S.A.M., M.A.M., N.L., F.Q. (Fawad Qureshi), P.P., F.Q. (Fahad Qureshi), P.C.A., P.N., M.C. and W.C.; data curation, C.T., N.L. and W.C.; formal analysis, C.T., W.K. and W.C.; funding acquisition, W.C.; investigation, C.T., C.C.J., W.K., P.V., S.A.M., M.A.M., N.L., F.Q. (Fawad Qureshi), P.P., P.N. and W.C.; methodology, C.T., W.K., F.Q. (Fahad Qureshi), M.C. and W.C.; project administration, W.K., F.Q. (Fahad Qureshi), P.C.A., P.N. and W.C.; resources, W.C.; software, C.T. and W.C.; supervision, C.C.J., S.A.M., F.Q. (Fawad Qureshi), P.P., M.C. and W.C.; validation, C.T., C.C.J., W.K., S.A.M., M.A.M., P.C.A. and W.C.; visualization, P.P. and W.C.; writing—original draft, C.T. and W.C.; writing—review and editing, C.T., C.C.J., W.K., P.V., S.A.M., M.A.M., N.L., F.Q. (Fawad Qureshi), P.P., F.Q. (Fahad Qureshi), P.C.A., P.N., M.C. and W.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
The Mayo Clinic Institutional Review Board approved this study (IRB number 21-007698) and waived the need for informed consent due to the use of publicly and de-identified database.
Informed Consent Statement
Patient consent was waived due to the minimal risk nature of observational chart review study.
Data Availability Statement
Data are available upon reasonable request to the corresponding author.
Acknowledgments
The authors thank the Organ Procurement and Transplantation Network for providing the data. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the OPTN or the United States government.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Reese, P.P.; Bloom, R.D.; Shults, J.; Thomasson, A.; Mussell, A.; Rosas, S.E.; Johansen, K.L.; Abt, P.; Levine, M.; Caplan, A.; et al. Functional status and survival after kidney transplantation. Transplantation 2014, 97, 189–195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kutner, N.G.; Zhang, R.; Bowles, T.; Painter, P. Pretransplant physical functioning and kidney patients’ risk for posttransplantation hospitalization/death: Evidence from a national cohort. Clin. J. Am. Soc. Nephrol. 2006, 1, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Lentine, K.L.; Alhamad, T.; Cheungpasitporn, W.; Tan, J.C.; Chang, S.H.; Cooper, M.; Dadhania, D.M.; Axelrod, D.A.; Schnitzler, M.A.; Ouseph, R.; et al. Impact of Functional Status on Outcomes of Simultaneous Pancreas-kidney Transplantation: Risks and Opportunities for Patient Benefit. Transplant. Direct 2020, 6, e599. [Google Scholar] [CrossRef] [PubMed]
- Chu, N.M.; Chen, X.; Bae, S.; Brennan, D.C.; Segev, D.L.; McAdams-DeMarco, M.A. Changes in Functional Status Among Kidney Transplant Recipients: Data From the Scientific Registry of Transplant Recipients. Transplantation 2021, 105, 2104–2111. [Google Scholar] [CrossRef]
- Garonzik-Wang, J.M.; Govindan, P.; Grinnan, J.W.; Liu, M.; Ali, H.M.; Chakraborty, A.; Jain, V.; Ros, R.L.; James, N.T.; Kucirka, L.M.; et al. Frailty and delayed graft function in kidney transplant recipients. Arch. Surg. 2012, 147, 190–193. [Google Scholar] [CrossRef]
- Kobashigawa, J.; Dadhania, D.; Bhorade, S.; Adey, D.; Berger, J.; Bhat, G.; Budev, M.; Duarte-Rojo, A.; Dunn, M.; Hall, S.; et al. Report from the American Society of Transplantation on frailty in solid organ transplantation. Am. J. Transplant. 2019, 19, 984–994. [Google Scholar] [CrossRef]
- McAdams-DeMarco, M.A.; Law, A.; King, E.; Orandi, B.; Salter, M.; Gupta, N.; Chow, E.; Alachkar, N.; Desai, N.; Varadhan, R.; et al. Frailty and mortality in kidney transplant recipients. Am. J. Transplant. 2015, 15, 149–154. [Google Scholar] [CrossRef] [Green Version]
- McAdams-DeMarco, M.A.; Law, A.; Salter, M.L.; Chow, E.; Grams, M.; Walston, J.; Segev, D.L. Frailty and early hospital readmission after kidney transplantation. Am. J. Transplant. 2013, 13, 2091–2095. [Google Scholar] [CrossRef] [Green Version]
- McAdams-DeMarco, M.A.; Law, A.; Tan, J.; Delp, C.; King, E.A.; Orandi, B.; Salter, M.; Alachkar, N.; Desai, N.; Grams, M.; et al. Frailty, mycophenolate reduction, and graft loss in kidney transplant recipients. Transplantation 2015, 99, 805–810. [Google Scholar] [CrossRef] [Green Version]
- Karnofsky, D.A. The clinical evaluation of chemotherapeutic agents in cancer. Eval. Chemother. Agents 1949, 191–205. [Google Scholar]
- Bui, K.; Kilambi, V.; Rodrigue, J.R.; Mehrotra, S. Patient Functional Status at Transplant and Its Impact on Posttransplant Survival of Adult Deceased-donor Kidney Recipients. Transplantation 2019, 103, 1051–1063. [Google Scholar] [CrossRef] [PubMed]
- McAdams-DeMarco, M.A.; Van Pilsum Rasmussen, S.E.; Chu, N.M.; Agoons, D.; Parsons, R.F.; Alhamad, T.; Johansen, K.L.; Tullius, S.G.; Lynch, R.; Harhay, M.N.; et al. Perceptions and Practices Regarding Frailty in Kidney Transplantation: Results of a National Survey. Transplantation 2020, 104, 349–356. [Google Scholar] [CrossRef] [PubMed]
- Mor, V.; Laliberte, L.; Morris, J.N.; Wiemann, M. The Karnofsky Performance Status Scale. An examination of its reliability and validity in a research setting. Cancer 1984, 53, 2002–2007. [Google Scholar] [CrossRef]
- UNOS Transplant Candidate Registration—Kidney. Available online: https://unos.org/wp-content/uploads/Adult-TCR-Kidney.pdf (accessed on 4 December 2021).
- Reese, P.P.; Shults, J.; Bloom, R.D.; Mussell, A.; Harhay, M.N.; Abt, P.; Levine, M.; Johansen, K.L.; Karlawish, J.T.; Feldman, H.I. Functional status, time to transplantation, and survival benefit of kidney transplantation among wait-listed candidates. Am. J. Kidney Dis. 2015, 66, 837–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veasey, T.M.; Fleming, J.N.; Strout, S.E.; Miller, R.; Pilch, N.A.; Meadows, H.B.; Mardis, C.R.; Mardis, B.A.; Shenvi, S.; McGillicuddy, J.; et al. Morbid obesity and functional status as predictors of surgical complication after renal transplantation. Am. J. Surg. 2018, 215, 663–668. [Google Scholar] [CrossRef]
- Bardonnaud, N.; Pillot, P.; Lillaz, J.; Delorme, G.; Chabannes, E.; Bernardini, S.; Guichard, G.; Bittard, H.; Kleinclauss, F. Outcomes of renal transplantation in obese recipients. Transplant. Proc. 2012, 44, 2787–2791. [Google Scholar] [CrossRef] [PubMed]
- Kampaktsis, P.N.; Tzani, A.; Doulamis, I.P.; Moustakidis, S.; Drosou, A.; Diakos, N.; Drakos, S.G.; Briasoulis, A. State-of-the-art machine learning algorithms for the prediction of outcomes after contemporary heart transplantation: Results from the UNOS database. Clin. Transplant. 2021, 35, e14388. [Google Scholar] [CrossRef]
- Killian, M.O.; Payrovnaziri, S.N.; Gupta, D.; Desai, D.; He, Z. Machine learning-based prediction of health outcomes in pediatric organ transplantation recipients. JAMIA Open 2021, 4, ooab008. [Google Scholar] [CrossRef]
- Ershoff, B.D.; Lee, C.K.; Wray, C.L.; Agopian, V.G.; Urban, G.; Baldi, P.; Cannesson, M. Training and Validation of Deep Neural Networks for the Prediction of 90-Day Post-Liver Transplant Mortality Using UNOS Registry Data. Transplant. Proc. 2020, 52, 246–258. [Google Scholar] [CrossRef]
- Wadhwani, S.I.; Hsu, E.K.; Shaffer, M.L.; Anand, R.; Ng, V.L.; Bucuvalas, J.C. Predicting ideal outcome after pediatric liver transplantation: An exploratory study using machine learning analyses to leverage Studies of Pediatric Liver Transplantation Data. Pediatric Transplant. 2019, 23, e13554. [Google Scholar] [CrossRef]
- Schwantes, I.R.; Axelrod, D.A. Technology-Enabled Care and Artificial Intelligence in Kidney Transplantation. Curr. Transplant. Rep. 2021, 8, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.L.; O’Sullivan, E.D.; Marson, L.P.; Wigmore, S.J.; Harrison, E.M. The Future Role of Machine Learning in Clinical Transplantation. Transplantation 2021, 105, 723–735. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Vaitla, P.; Jadlowiec, C.C.; Leeaphorn, N.; Mao, S.A.; Mao, M.A.; Pattharanitima, P.; Bruminhent, J.; Khoury, N.J.; Garovic, V.D.; et al. Use of Machine Learning Consensus Clustering to Identify Distinct Subtypes of Black Kidney Transplant Recipients and Associated Outcomes. JAMA Surg. 2022, e221286. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Mao, M.A.; Kattah, A.G.; Keddis, M.T.; Pattharanitima, P.; Erickson, S.B.; Dillon, J.J.; Garovic, V.D.; Cheungpasitporn, W. Subtyping hospitalized patients with hypokalemia by machine learning consensus clustering and associated mortality risks. Clin. Kidney J. 2022, 15, 253–261. [Google Scholar] [CrossRef]
- MacEachern, S.J.; Forkert, N.D. Machine learning for precision medicine. Genome 2021, 64, 416–425. [Google Scholar] [CrossRef]
- Alyousef, A.A.; Nihtyanova, S.; Denton, C.; Bosoni, P.; Bellazzi, R.; Tucker, A. Nearest Consensus Clustering Classification to Identify Subclasses and Predict Disease. J. Healthc. Inform. Res. 2018, 2, 402–422. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Z.; Waikar, S.S.; Schmidt, I.M.; Landis, J.R.; Hsu, C.Y.; Shafi, T.; Feldman, H.I.; Anderson, A.H.; Wilson, F.P.; Chen, J.; et al. Subtyping CKD Patients by Consensus Clustering: The Chronic Renal Insufficiency Cohort (CRIC) Study. J. Am. Soc. Nephrol. 2021, 32, 639–653. [Google Scholar] [CrossRef]
- Thongprayoon, C.; Kattah, A.G.; Mao, M.A.; Keddis, M.T.; Pattharanitima, P.; Vallabhajosyula, S.; Nissaisorakarn, V.; Erickson, S.B.; Dillon, J.J.; Garovic, V.D.; et al. Distinct Phenotypes of Hospitalized Patients with Hyperkalemia by Machine Learning Consensus Clustering and Associated Mortality Risks. QJM—Int. J. Med. 2021, hcab194. [Google Scholar] [CrossRef]
- Van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef] [Green Version]
- Monti, S.; Tamayo, P.; Mesirov, J.; Golub, T. Consensus clustering: A resampling-based method for class discovery and visualization of gene expression microarray data. Mach. Learn. 2003, 52, 91–118. [Google Scholar] [CrossRef]
- Wilkerson, M.D.; Hayes, D.N. ConsensusClusterPlus: A class discovery tool with confidence assessments and item tracking. Bioinformatics 2010, 26, 1572–1573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Șenbabaoğlu, Y.; Michailidis, G.; Li, J.Z. Critical limitations of consensus clustering in class discovery. Sci. Rep. 2014, 4, 6207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Foster, B.J.; Dahhou, M.; Zhang, X.; Platt, R.W.; Smith, J.M.; Hanley, J.A. Impact of HLA mismatch at first kidney transplant on lifetime with graft function in young recipients. Am. J. Transplant. 2014, 14, 876–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernandez, D.; Vazquez, T.; Alonso-Titos, J.; Leon, M.; Caballero, A.; Cobo, M.A.; Sola, E.; Lopez, V.; Ruiz-Esteban, P.; Cruzado, J.M.; et al. Impact of HLA Mismatching on Early Subclinical Inflammation in Low-Immunological-Risk Kidney Transplant Recipients. J. Clin. Med. 2021, 10, 1934. [Google Scholar] [CrossRef]
- Mjoen, G.; Reisaeter, A.V.; Dahle, D.O. HLA Mismatch and Allograft Survival. Transplantation 2016, 100, e52. [Google Scholar] [CrossRef]
- Kouwenhoven, E.A.; de Bruin, R.W.; Bajema, I.M.; Marquet, R.L.; Ijzermans, J.N. Cold ischemia augments allogeneic-mediated injury in rat kidney allografts. Kidney Int. 2001, 59, 1142–1148. [Google Scholar] [CrossRef] [Green Version]
- Mikhalski, D.; Wissing, K.M.; Ghisdal, L.; Broeders, N.; Touly, M.; Hoang, A.D.; Loi, P.; Mboti, F.; Donckier, V.; Vereerstraeten, P.; et al. Cold ischemia is a major determinant of acute rejection and renal graft survival in the modern era of immunosuppression. Transplantation 2008, 85, S3–S9. [Google Scholar] [CrossRef]
- Bryan, C.F.; Luger, A.M.; Martinez, J.; Muruve, N.; Nelson, P.W.; Pierce, G.E.; Ross, G.; Shield, C.F., III; Warady, B.A.; Aeder, M.I.; et al. Cold ischemia time: An independent predictor of increased HLA class I antibody production after rejection of a primary cadaveric renal allograft. Transplantation 2001, 71, 875–879. [Google Scholar] [CrossRef]
- Sert, I.; Colak, H.; Tugmen, C.; Dogan, S.M.; Karaca, C. The effect of cold ischemia time on delayed graft function and acute rejection in kidney transplantation. Saudi J. Kidney Dis. Transplant. 2014, 25, 960–966. [Google Scholar] [CrossRef]
- McAdams-DeMarco, M.A.; Isaacs, K.; Darko, L.; Salter, M.L.; Gupta, N.; King, E.A.; Walston, J.; Segev, D.L. Changes in Frailty After Kidney Transplantation. J. Am. Geriatr. Soc. 2015, 63, 2152–2157. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).