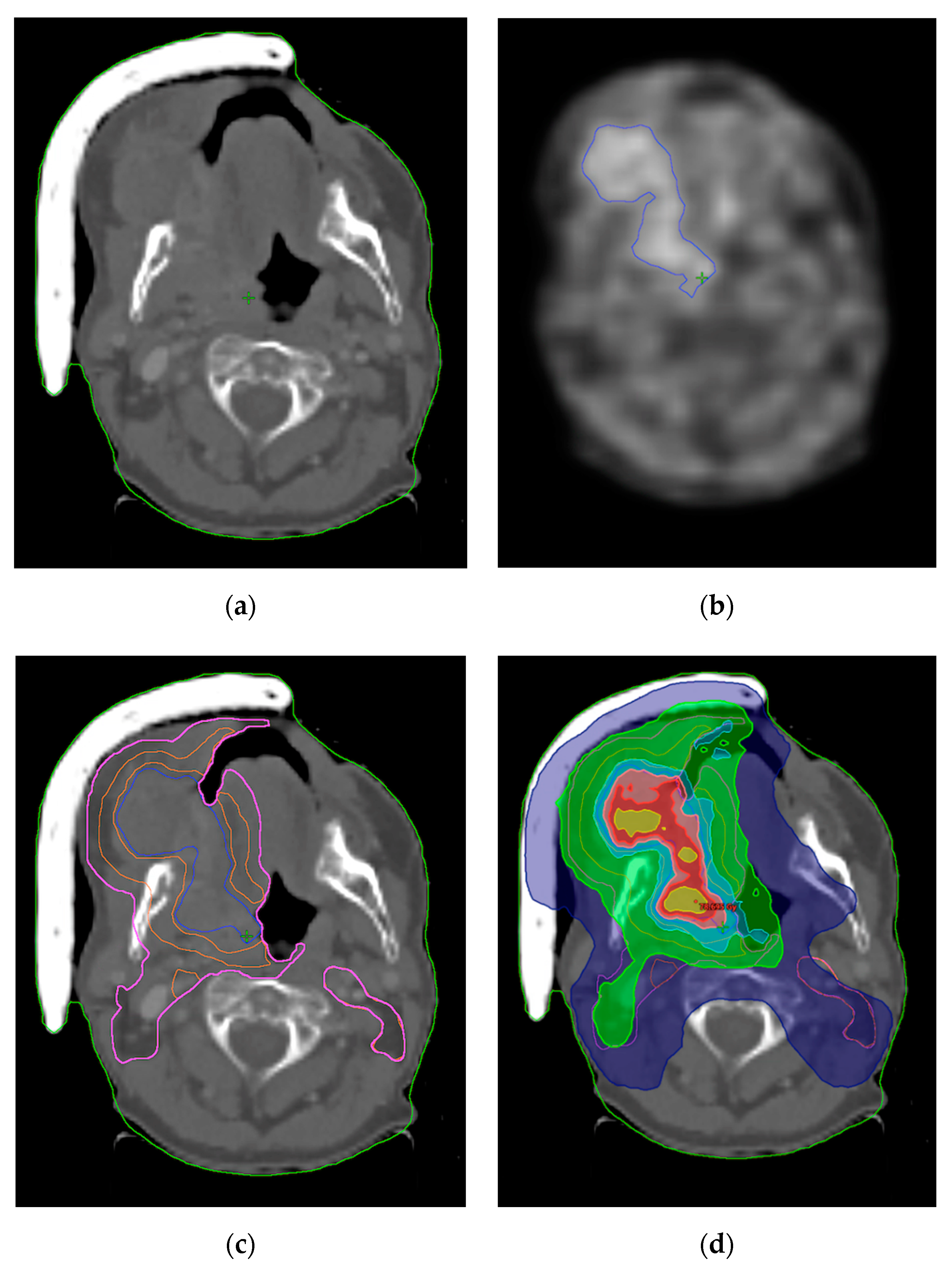
FMISO-Based Adaptive Radiotherapy in Head and Neck Cancer
Abstract
:1. Introduction
2. Hypoxia in Head and Neck Cancers
2.1. Hypoxia Evaluation Using FMISO
2.2. Locoregional Relapse
2.3. Adaptive HNC Radiotherapy
2.4. Dose-Escalated HNC Radiotherapy
2.5. FMISO-Based Adaptive Radiotherapy
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bennardo, L.; Bennardo, F.; Giudice, A.; Passante, M.; Dastoli, S.; Morrone, P.; Provenzano, E.; Patruno, C.; Nisticò, S. Local Chemotherapy as an Adjuvant Treatment in Unresectable Squamous Cell Carcinoma: What Do We Know So Far? Curr. Oncol. 2021, 28, 2317–2325. [Google Scholar] [CrossRef]
- Pentangelo, G.; Nisticò, S.; Provenzano, E.; Cisale, G.; Bennardo, L. Topical 5% Imiquimod Sequential to Surgery for HPV-Related Squamous Cell Carcinoma of the Lip. Medicina 2021, 57, 563. [Google Scholar] [CrossRef] [PubMed]
- Koukourakis, M.I.; Giatromanolaki, A.; Sivridis, E.; Pastorek, J.; Karapantzos, I.; Gatter, K.C.; Harris, A.L. Hypoxia-activated tumor pathways of angiogenesis and pH regulation independent of anemia in head-and-neck cancer. Int. J. Radiat. Oncol. Biol. Phys. 2004, 59, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Rankin, E.B.; Giaccia, A.J. The role of hypoxia-inducible factors in tumorigenesis. Cell Death Differ. 2008, 15, 678–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleming, I.N.; Manavaki, R.; Blower, P.; West, C.; Williams, K.J.; Harris, A.; Domarkas, J.; Lord, S.J.; Baldry, C.W.; Gilbert, F.J. Imaging tumour hypoxia with positron emission tomography. Br. J. Cancer 2014, 112, 238–250. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Semenza, G.L. Hydroxylation of HIF-1: Oxygen Sensing at the Molecular Level. Physiology 2004, 19, 176–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lan, M.; Huang, Y.; Chen, C.-Y.; Han, F.; Wu, S.-X.; Tian, L.; Zheng, L.; Lu, T.-X. Prognostic Value of Cervical Nodal Necrosis in Nasopharyngeal Carcinoma: Analysis of 1800 Patients with Positive Cervical Nodal Metastasis at MR Imaging. Radiology 2015, 276, 536–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, Y.; Cao, C.; Hu, Q.; Chen, X. Prognostic Value and Staging Classification of Lymph Nodal Necrosis in Nasopharyngeal Carcinoma after Intensity-Modulated Radiotherapy. Cancer Res. Treat. 2018, 51, 1222–1230. [Google Scholar] [CrossRef]
- Liang, S.-B.; Chen, L.-S.; Yang, X.-L.; Chen, D.-M.; Wang, D.-H.; Cui, C.-Y.; Xie, C.-B.; Liu, L.-Z.; Xu, X.-Y. Influence of tumor necrosis on treatment sensitivity and long-term survival in nasopharyngeal carcinoma. Radiother. Oncol. 2021, 155, 219–225. [Google Scholar] [CrossRef]
- Ou, D.; Garberis, I.; Adam, J.; Blanchard, P.; Nguyen, F.; Levy, A.; Casiraghi, O.; Gorphe, P.; Breuskin, I.; Janot, F.; et al. Prognostic value of tissue necrosis, hypoxia-related markers and correlation with HPV status in head and neck cancer patients treated with bio- or chemo-radiotherapy. Radiother. Oncol. 2018, 126, 116–124. [Google Scholar] [CrossRef]
- Zhang, X.C.; Xu, C.; Mitchell, R.M.; Zhang, B.; Zhao, D.; Li, Y.; Huang, X.; Fan, W.; Wang, H.; Lerma, L.A.; et al. Tumor Evolution and Intratumor Heterogeneity of an Oropharyngeal Squamous Cell Carcinoma Revealed by Whole-Genome Sequencing. Neoplasia 2013, 15, 1371–1378. [Google Scholar] [CrossRef] [Green Version]
- Yeung, K.T.; Yang, J. Epithelial-mesenchymal transition in tumor metastasis. Mol. Oncol. 2017, 11, 28–39. [Google Scholar] [CrossRef] [Green Version]
- Lester, R.D.; Jo, M.; Montel, V.; Takimoto, S.; Gonias, S.L. uPAR induces epithelial–mesenchymal transition in hypoxic breast cancer cells. J. Cell Biol. 2007, 178, 425–436. [Google Scholar] [CrossRef]
- Johansson, A.-C.; La Fleur, L.; Melissaridou, S.; Roberg, K. The relationship between EMT, CD44high/EGFRlow phenotype, and treatment response in head and neck cancer cell lines. J. Oral Pathol. Med. 2016, 45, 640–646. [Google Scholar] [CrossRef]
- Raleigh, J.A.; Chou, S.-C.; Arteel, G.E.; Horsman, M. Comparisons among Pimonidazole Binding, Oxygen Electrode Measurements, and Radiation Response in C3H Mouse Tumors. Radiat. Res. 1999, 151, 580–589. [Google Scholar] [CrossRef]
- Evans, S.; Joiner, B.; Jenkins, W.; Laughlin, K.; Lord, E.; Koch, C. Identification of hypoxia in cells and tissues of epigastric 9L rat glioma using EF5 [2-(2-nitro-1H-imidazol-1-yl)-N-(2,2,3,3,3-pentafluoropropyl) acetamide]. Br. J. Cancer 1995, 72, 875–882. [Google Scholar] [CrossRef] [Green Version]
- Rasey, J.S.; Koh, W.-J.; Evans, M.L.; Peterson, L.M.; Lewellen, T.K.; Graham, M.M.; Krohn, K.A. Quantifying regional hypoxia in human tumors with positron emission tomography of [18F]fluoromisonidazole: A pretherapy study of 37 patients. Int. J. Radiat. Oncol. Biol. Phys. 1996, 36, 417–428. [Google Scholar] [CrossRef]
- Piert, M.; Machulla, H.-J.; Picchio, M.; Reischl, G.; Ziegler, S.; Kumar, P.; Wester, H.-J.; Beck, R.; McEwan, A.J.B.; Wiebe, L.I.; et al. Hypoxia-specific tumor imaging with 18F-fluoroazomycin arabinoside. J. Nucl. Med. 2005, 46, 106–113. [Google Scholar]
- Urtasun, R.C.; Parliament, M.B.; McEwan, A.J.; Mercer, J.R.; Mannan, R.H.; Wiebe, L.I.; Morin, C.; Chapman, J.D. Measurement of hypoxia in human tumours by non-invasive spect imaging of iodoazomycin arabinoside. Br. J. Cancer Suppl. 1996, 27, S209–S212. [Google Scholar]
- Seddon, B.M.; Payne, G.S.; Simmons, L.; Ruddle, R.; Grimshaw, R.; Tan, S.; Turner, A.; Raynaud, F.; Halbert, G.; Leach, M.O.; et al. A phase I study of SR-4554 via intravenous administration for noninvasive investigation of tumor hypoxia by magnetic resonance spectroscopy in patients with malignancy. Clin. Cancer Res. 2003, 9, 5101–5112. [Google Scholar]
- Nordsmark, M.; Bentzen, S.M.; Rudat, V.; Brizel, D.; Lartigau, E.; Stadler, P.; Becker, A.; Adam, M.; Molls, M.; Dunst, J.; et al. Prognostic value of tumor oxygenation in 397 head and neck tumors after primary radiation therapy. An international multi-center study. Radiother. Oncol. 2005, 77, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Overgaard, J.; Hansen, H.S.; Andersen, A.; Hjelm-Hansen, M.; Jørgensen, K.; Sandberg, E.; Berthelsen, A.; Hammer, R.; Pedersen, M. Misonidazole combined with split-course radiotherapy in the treatment of invasive carcinoma of larynx and pharynx: Report from the DAHANCA 2 study. Int. J. Radiat. Oncol. Biol. Phys. 1989, 16, 1065–1068. [Google Scholar] [CrossRef]
- Overgaard, J. Hypoxic modification of radiotherapy in squamous cell carcinoma of the head and neck—A systematic review and meta-analysis. Radiother. Oncol. 2011, 100, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Grkovski, M.; Lee, N.Y.; Schöder, H.; Carlin, S.D.; Beattie, B.J.; Riaz, N.; Leeman, J.E.; O’Donoghue, J.A.; Humm, J.L. Monitoring early response to chemoradiotherapy with 18F-FMISO dynamic PET in head and neck cancer. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, 1682–1691. [Google Scholar] [CrossRef]
- Carles, M.; Fechter, T.; Grosu, A.; Sörensen, A.; Thomann, B.; Stoian, R.; Wiedenmann, N.; Rühle, A.; Zamboglou, C.; Ruf, J.; et al. 18F-FMISO-PET Hypoxia Monitoring for Head-and-Neck Cancer Patients: Radiomics Analyses Predict the Outcome of Chemo-Radiotherapy. Cancers 2021, 13, 3449. [Google Scholar] [CrossRef]
- Peeters, S.G.; Zegers, C.M.; Lieuwes, N.G.; van Elmpt, W.; Eriksson, J.; van Dongen, G.A.; Dubois, L.; Lambin, P. A Comparative Study of the Hypoxia PET Tracers [18F]HX4, [18F]FAZA, and [18F]FMISO in a Preclinical Tumor Model. Int. J. Radiat. Oncol. Biol. Phys. 2015, 91, 351–359. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; Fan, J.; Li, Y.; Fu, S.; Chen, Y.; Wu, J. Imaging of Tumor Hypoxia with Radionuclide-Labeled Tracers for PET. Front. Oncol. 2021, 11, 731503. [Google Scholar] [CrossRef]
- Lopci, E.; Grassi, I.; Chiti, A.; Nanni, C.; Cicoria, G.; Toschi, L.; Fonti, C.; Lodi, F.; Mattioli, S.; Fanti, S. PET radiopharmaceuticals for imaging of tumor hypoxia: A review of the evidence. Am. J. Nucl. Med. Mol. Imaging 2014, 4, 365–384. [Google Scholar]
- Zschaeck, S.; Löck, S.; Hofheinz, F.; Zips, D.; Mortensen, L.S.; Zöphel, K.; Troost, E.G.; Boeke, S.; Saksø, M.; Mönnich, D.; et al. Individual patient data meta-analysis of FMISO and FAZA hypoxia PET scans from head and neck cancer patients undergoing definitive radio-chemotherapy. Radiother. Oncol. 2020, 149, 189–196. [Google Scholar] [CrossRef]
- Padhani, A.R.; Krohn, K.A.; Lewis, J.S.; Alber, M. Imaging oxygenation of human tumours. Eur. Radiol. 2007, 17, 861–872. [Google Scholar] [CrossRef] [Green Version]
- Muzi, M.; Peterson, L.M.; O’Sullivan, J.N.; Fink, J.R.; Rajendran, J.G.; McLaughlin, L.J.; Muzi, J.P.; Mankoff, D.A.; Krohn, K.A. 18F-Fluoromisonidazole Quantification of Hypoxia in Human Cancer Patients Using Image-Derived Blood Surrogate Tissue Reference Regions. J. Nucl. Med. 2015, 56, 1223–1228. [Google Scholar] [CrossRef] [Green Version]
- Pignon, J.-P.; le Maître, A.; Maillard, E.; Bourhis, J.; MACH-NC Collaborative Group. Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): An update on 93 randomised trials and 17,346 patients. Radiother. Oncol. 2009, 92, 4–14. [Google Scholar] [CrossRef]
- Nishikawa, Y.; Yasuda, K.; Okamoto, S.; Ito, Y.M.; Onimaru, R.; Shiga, T.; Tsuchiya, K.; Watanabe, S.; Takeuchi, W.; Kuge, Y.; et al. Local relapse of nasopharyngeal cancer and Voxel-based analysis of FMISO uptake using PET with semiconductor detectors. Radiat. Oncol. 2017, 12, 148. [Google Scholar] [CrossRef]
- Bhandari, V.; Patel, P.; Gurjar, O.P.; Gupta, K.L. Impact of repeat computerized tomography replans in the radiation therapy of head and neck cancers. J. Med. Phys. 2014, 39, 164–168. [Google Scholar] [CrossRef]
- Bhide, S.A.; Davies, M.; Burke, K.; McNair, H.A.; Hansen, V.; Barbachano, Y.; El-Hariry, I.; Newbold, K.; Harrington, K.J.; Nutting, C.M. Weekly Volume and Dosimetric Changes during Chemoradiotherapy with Intensity-Modulated Radiation Therapy for Head and Neck Cancer: A Prospective Observational Study. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 1360–1368. [Google Scholar] [CrossRef]
- Yang, H.; Hu, W.; Wang, W.; Chen, P.; Ding, W.; Luo, W. Replanning during Intensity Modulated Radiation Therapy Improved Quality of Life in Patients with Nasopharyngeal Carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, e47–e54. [Google Scholar] [CrossRef]
- Schwartz, D.L.; Garden, A.S.; Thomas, J.; Chen, Y.; Zhang, Y.; Lewin, J.; Chambers, M.S.; Dong, L. Adaptive Radiotherapy for Head-and-Neck Cancer: Initial Clinical Outcomes from a Prospective Trial. Int. J. Radiat. Oncol. Biol. Phys. 2012, 83, 986–993. [Google Scholar] [CrossRef] [Green Version]
- Zhao, L.; Wan, Q.; Zhou, Y.; Deng, X.; Xie, C.; Wu, S. The role of replanning in fractionated intensity modulated radiotherapy for nasopharyngeal carcinoma. Radiother. Oncol. 2011, 98, 23–27. [Google Scholar] [CrossRef]
- Chen, A.M.; Daly, M.E.; Cui, J.; Mathai, M.; Benedict, S.; Purdy, J.A. Clinical outcomes among patients with head and neck cancer treated by intensity-modulated radiotherapy with and without adaptive replanning. Head Neck 2014, 36, 1541–1546. [Google Scholar] [CrossRef]
- Brown, E.; Owen, R.; Harden, F.; Mengersen, K.; Oestreich, K.; Houghton, W.; Poulsen, M.; Harris, S.; Lin, C.; Porceddu, S. Head and neck adaptive radiotherapy: Predicting the time to replan. Asia-Pac. J. Clin. Oncol. 2016, 12, 460–467. [Google Scholar] [CrossRef]
- Gensheimer, M.F.; Le, Q.-T. Adaptive radiotherapy for head and neck cancer: Are we ready to put it into routine clinical practice? Oral Oncol. 2018, 86, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Belshaw, L.; Agnew, C.E.; Irvine, D.M.; Rooney, K.P.; McGarry, C.K. Adaptive radiotherapy for head and neck cancer reduces the requirement for rescans during treatment due to spinal cord dose. Radiat. Oncol. 2019, 14, 189. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, C.L.; Steenbakkers, R.J.; Bourhis, J.; Budach, W.; Grau, C.; Grégoire, V.; van Herk, M.; Lee, A.; Maingon, P.; Nutting, C.; et al. CT-based delineation of organs at risk in the head and neck region: DAHANCA, EORTC, GORTEC, HKNPCSG, NCIC CTG, NCRI, NRG Oncology and TROG consensus guidelines. Radiother. Oncol. 2015, 117, 83–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hunter, K.U.; Fernandes, L.L.; Vineberg, K.A.; McShan, D.; Antonuk, A.E.; Cornwall, C.; Feng, M.; Schipper, M.J.; Balter, J.M.; Eisbruch, A. Parotid Glands Dose–Effect Relationships Based on Their Actually Delivered Doses: Implications for Adaptive Replanning in Radiation Therapy of Head-and-Neck Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stauch, Z.; Zoller, W.; Tedrick, K.; Walston, S.; Christ, D.; Hunzeker, A.; Lenards, N.; Culp, L.; Gamez, M.E.; Blakaj, D. An evaluation of adaptive planning by assessing the dosimetric impact of weight loss throughout the course of radiotherapy in bilateral treatment of head and neck cancer patients. Med. Dosim. 2020, 45, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Atwell, D.; Elks, J.; Cahill, K.; Hearn, N.; Vignarajah, D.; Lagopoulos, J.; Min, M. A Review of Modern Radiation Therapy Dose Escalation in Locally Advanced Head and Neck Cancer. Clin. Oncol. 2020, 32, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Lauve, A.; Morris, M.; Schmidt-Ullrich, R.; Wu, Q.; Mohan, R.; Abayomi, O.; Buck, D.; Holdford, D.; Dawson, K.; Dinardo, L.; et al. Simultaneous integrated boost intensity-modulated radiotherapy for locally advanced head-and-neck squamous cell carcinomas: II—Clinical results. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 374–387. [Google Scholar] [CrossRef]
- Kashihara, T.; Nakamura, S.; Murakami, N.; Ito, K.; Matsumoto, Y.; Kobayashi, K.; Omura, G.; Mori, T.; Honma, Y.; Kubo, Y.; et al. Initial Experience of Intentional Internal High-Dose Policy Volumetric Modulated Arc Therapy of Neck Lymph Node Metastases ≥ 2 cm in Patients with Head and Neck Squamous Cell Carcinoma. Front. Oncol. 2021, 11, 651409. [Google Scholar] [CrossRef]
- Pigorsch, S.U.; Wilkens, J.J.; Kampfer, S.; Kehl, V.; Hapfelmeier, A.; Schläger, C.; Bier, H.; Schwaiger, M.; Combs, S.E. Do selective radiation dose escalation and tumour hypoxia status impact the loco-regional tumour control after radio-chemotherapy of head & neck tumours? The ESCALOX protocol. Radiat. Oncol. 2017, 12, 45. [Google Scholar] [CrossRef] [Green Version]
- Welz, S.; Paulsen, F.; Pfannenberg, C.; Reimold, M.; Reischl, G.; Nikolaou, K.; La Fougère, C.; Alber, M.; Belka, C.; Zips, D.; et al. Dose escalation to hypoxic subvolumes in head and neck cancer: A randomized phase II study using dynamic [18F]FMISO PET/CT. Radiother. Oncol. 2022, 171, 30–36. [Google Scholar] [CrossRef]
- Meijer, G.; Steenhuijsen, J.; Bal, M.; De Jaeger, K.; Schuring, D.; Theuws, J. Dose painting by contours versus dose painting by numbers for stage II/III lung cancer: Practical implications of using a broad or sharp brush. Radiother. Oncol. 2011, 100, 396–401. [Google Scholar] [CrossRef] [PubMed]
- Strohl, M.P.; Wai, K.C.; Ha, P.K. De-intensification strategies in HPV-related oropharyngeal squamous cell carcinoma—A narrative review. Ann. Transl. Med. 2020, 8, 1601. [Google Scholar] [CrossRef] [PubMed]
| Study Number | Study Original Name | Intervention | Type | Year |
|---|---|---|---|---|
| NCT00606294 (USA) | A Study Using Fluorine-18-Labeled Fluoro-Misonidazole Positron Emission Tomography to Detect Hypoxia in Head and Neck Cancer Patients | Cohort 1 Primary tumor 70 Gy, positive nodes 70 Primary tumor 70 Gy, positive nodes 60 (HPV+/FMISO−) Cohort 2 Surgical bed 30 Gy, positive nodes 30+/− neck dissection (HPV+/FMISO−) | Prospective | 2008 |
| NCT05348486 (Czech Republic) | FARHEAD: FMISO-based Adaptive Radiotherapy for Head and Neck Cancer | Standard arm Primary tumor and positive nodes 70 Gy/33 fractions (HPV−/FMISO−) Experimental arm Primary tumor and positive nodes 75.9–79.2 Gy/33 fractions (HPV−/FMISO+) | Prospective | 2022 |
| NCT03865277 (Austria) | Individualized Radiation Dose Prescription in HNSCC Based on F-MISO-PET Hypoxia-Imaging: Multi-center, Randomized Phase-II-trial | Standard hypoxic Primary tumor and positive nodes 70/35 Gy fractions (HPV−/FMISO+) Experimental dose-escalated hypoxic Primary tumor and positive nodes 77 Gy/35 fractions (HPV−/FMISO+) Experimental dose-escalated carbon hypoxic Primary tumor and positive nodes 77 Gy/35 fractions (HPV−/FMISO+) Standard oxic Primary tumor and positive nodes 70/35 fractions Gy (HPV−/FMISO−) Standard HPV+ Primary tumor and positive nodes 70/35 fractions Gy (HPV+/FMISO+−) | Phase II | 2022 |
| NCT02352792 (Germany) | Randomized Phase II Study for Dose Escalation in Locally Advanced Head and Neck Squamous Cell Carcinomas Treated With Radiochemotherapy | Standard arm Primary tumor and positive nodes 70 Gy/33 fractions Experimental arm Standard plus 10% dose escalation to the hypoxic volume | Phase II | 2015 |
| NCT02207439 (USA) | A Phase II Trial of a Protease Inhibitor, Nelfinavir (NFV), Given With Definitive, Concurrent Chemoradiotherapy (CTRT) in Patients With Locally Advanced, Human Papilloma Virus (HPV) Negative, Squamous Cell Carcinoma of the Head and Neck | Nelfinavir for 7–14 days prior chemoradiotherapy (HPV−/FMISO+) | Phase II | 2014 |
| NCT01212354 (Germany) | Escalox—Phase III A Prospective, Randomized, Rater-blinded, Multicentre Interventional Clinical Trial. Do Selective Radiation Dose Escalation and Tumour Hypoxia Status Impact the Locoregional Tumour Control After Radiochemotherapy of Head and Neck Tumours? | Standard arm Primary tumor and positive nodes 70 Gy/33 fractions (5 × 2 Gy per week) Experimental arm Primary tumor and positive nodes 80.5 Gy/33 fractions (5 × 2.3 Gy per week) | Phase II | 2010 |
| NCT03323463 (USA) | A Prospective Single Arm Non-inferiority Trial of Major Radiation Dose De-Escalation Concurrent With Chemotherapy for Human Papilloma Virus Associated Oropharyngeal Carcinoma | Standard arm Primary tumor and positive nodes 70 Gy/33 fractions (HPV+/FMISO+) Experimental arm Primary tumor and positive nodes 30 Gy/10 fractions (HPV+/FMISO−) | Prospective | 2017 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dolezel, M.; Slavik, M.; Blazek, T.; Kazda, T.; Koranda, P.; Veverkova, L.; Burkon, P.; Cvek, J. FMISO-Based Adaptive Radiotherapy in Head and Neck Cancer. J. Pers. Med. 2022, 12, 1245. https://doi.org/10.3390/jpm12081245
Dolezel M, Slavik M, Blazek T, Kazda T, Koranda P, Veverkova L, Burkon P, Cvek J. FMISO-Based Adaptive Radiotherapy in Head and Neck Cancer. Journal of Personalized Medicine. 2022; 12(8):1245. https://doi.org/10.3390/jpm12081245
Chicago/Turabian StyleDolezel, Martin, Marek Slavik, Tomas Blazek, Tomas Kazda, Pavel Koranda, Lucia Veverkova, Petr Burkon, and Jakub Cvek. 2022. "FMISO-Based Adaptive Radiotherapy in Head and Neck Cancer" Journal of Personalized Medicine 12, no. 8: 1245. https://doi.org/10.3390/jpm12081245
APA StyleDolezel, M., Slavik, M., Blazek, T., Kazda, T., Koranda, P., Veverkova, L., Burkon, P., & Cvek, J. (2022). FMISO-Based Adaptive Radiotherapy in Head and Neck Cancer. Journal of Personalized Medicine, 12(8), 1245. https://doi.org/10.3390/jpm12081245






