Dysautonomia, but Not Cardiac Dysfunction, Is Common in a Cohort of Individuals with Long COVID
Abstract
:1. Introduction
2. Materials and Methods
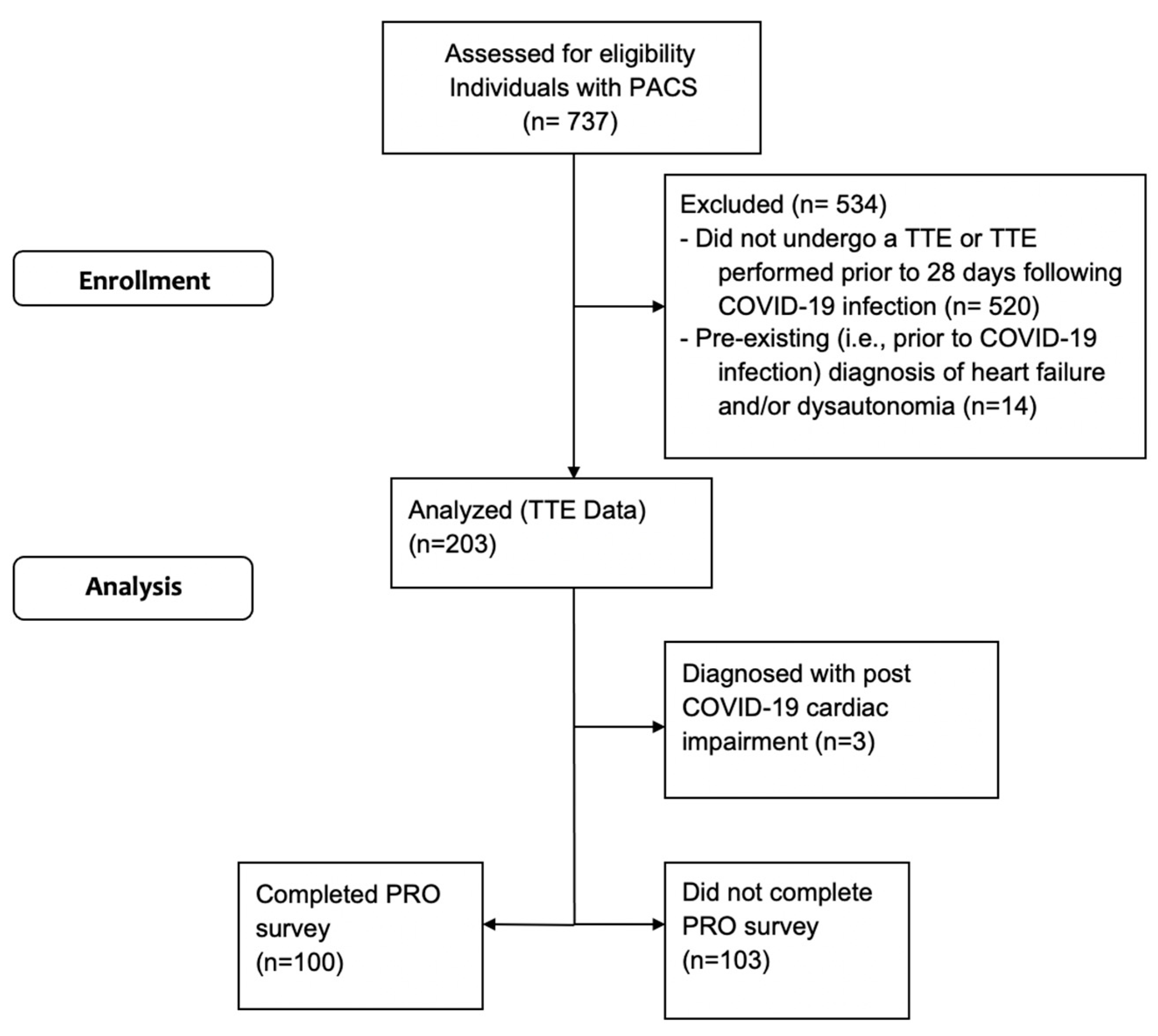
2.1. Study Design
2.2. Participants
2.3. Data Collection and Outcomes
2.4. Echocardiographic Assessment
2.5. Classification of Clinically Diagnosed Dysautonomia
2.6. Patient-Reported Outcomes
2.7. Statistical Plan
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lala, A.; Johnson, K.W.; Januzzi, J.L.; Russak, A.J.; Paranjpe, I.; Richter, F.; Zhao, S.; Somani, S.; Van Vleck, T.; Vaid, A.; et al. Prevalence and Impact of Myocardial Injury in Patients Hospitalized With COVID-19 Infection. J. Am. Coll Cardiol. 2020, 76, 533–546. [Google Scholar] [CrossRef]
- Nakatani, S.; Ohta-Ogo, K.; Nishio, M.; Amemiya, K.; Sato, S.; Sawano, H.; Hatakeyama, K.; Katano, H.; Suzuki, T.; Hirooka, K. Microthrombosis as a cause of fulminant myocarditis-like presentation with COVID-19 proven by endomyocardial biopsy. Cardiovasc. Pathol. 2022, 60, 107435. [Google Scholar] [CrossRef] [PubMed]
- Farkouh, M.E.; Stone, G.W.; Lala, A.; Bagiella, E.; Moreno, P.R.; Nadkarni, G.N.; Ben-Yehuda, O.; Granada, J.F.; Dressler, O.; Tinuoye, E.O.; et al. Anticoagulation in Patients With COVID-19: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2022, 79, 917–928. [Google Scholar] [CrossRef] [PubMed]
- Sperotto, F.; Friedman, K.G.; Son, M.B.F.; VanderPluym, C.J.; Newburger, J.W.; Dionne, A. Cardiac manifestations in SARS-CoV-2-associated multisystem inflammatory syndrome in children: A comprehensive review and proposed clinical approach. Eur. J. Pediatr. 2021, 180, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Aldeghaither, S.M.; Qutob, R.M.; Assanangkornchai, N.M.; Issa-Chergui, B.; Tam, M.C.; Larotondo, R.; Samoukovic, G.M. Clinical and Histopathologic Features of Myocarditis in Multisystem Inflammatory Syndrome (Adult)-Associated COVID-19. Crit. Care Explor. 2022, 10, e0630. [Google Scholar] [CrossRef] [PubMed]
- Ammirati, E.; Lupi, L.; Palazzini, M.; Hendren, N.S.; Grodin, J.L.; Cannistraci, C.V.; Schmidt, M.; Hekimian, G.; Peretto, G.; Bochaton, T.; et al. Prevalence, Characteristics, and Outcomes of COVID-19-Associated Acute Myocarditis. Circulation. 2022, 145, 1123–1139. [Google Scholar] [CrossRef]
- Moulson, N.; Petek, B.J.; Drezner, J.A.; Harmon, K.G.; Kliethermes, S.A.; Patel, M.R.; Baggish, A.L.; Asif, I.M.; Borchers, J.; Edenfield, K.M.; et al. SARS-CoV-2 Cardiac Involvement in Young Competitive Athletes. Circulation. 2021, 144, 256–266. [Google Scholar] [CrossRef] [PubMed]
- Daniels, C.J.; Rajpal, S.; Greenshields, J.T.; Rosenthal, G.L.; Chung, E.H.; Terrin, M.; Jeudy, J.; Mattson, S.E.; Law, I.H.; Borchers, J.; et al. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes With Recent SARS-CoV-2 Infection: Results From the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021, 6, 1078–1087. [Google Scholar] [CrossRef]
- Tabacof, L.; Tosto-Mancuso, J.; Wood, J.; Cortes, M.; Kontorovich, A.; McCarthy, D.; Rizk, D.; Rozanski, G.; Breyman, E.; Nasr, L.; et al. Post-acute COVID-19 Syndrome Negatively Impacts Physical Function, Cognitive Function, Health-Related Quality of Life, and Participation. Am. J. Phys. Med. Rehabil. 2022, 101, 48–52. [Google Scholar] [CrossRef]
- Davis, H.E.; Assaf, G.S.; McCorkell, L.; Wei, H.; Low, R.J.; Re’Em, Y.; Redfield, S.; Austin, J.P.; Akrami, A. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine 2021, 38, 101019. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Nearly One in Five American Adults Who Have Had COVID-19 Still Have “Long COVID”. Available online: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/20220622.htm# (accessed on 25 July 2022).
- Blitshteyn, S.; Whitelaw, S. Postural orthostatic tachycardia syndrome (POTS) and other autonomic disorders after COVID-19 infection: A case series of 20 patients. Immunol. Res. 2021, 69, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.; Ståhlberg, M.; Runold, M.; Nygren-Bonnier, M.; Nilsson, J.; Olshansky, B.; Bruchfeld, J.; Fedorowski, A. Long-Haul Post-COVID-19 Symptoms Presenting as a Variant of Postural Orthostatic Tachycardia Syndrome: The Swedish Experience. JACC Case Rep. 2021, 3, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Buoite Stella, A.; Furlanis, G.; Frezza, N.A.; Valentinotti, R.; Ajcevic, M.; Manganotti, P. Autonomic dysfunction in post-COVID patients with and witfhout neurological symptoms: A prospective multidomain observational study. J. Neurol. 2022, 269, 587–596. [Google Scholar] [CrossRef]
- Jamal, S.M.; Landers, D.B.; Hollenberg, S.M.; Turi, Z.G.; Glotzer, T.V.; Tancredi, J.; Parrillo, J.E. Prospective Evaluation of Autonomic Dysfunction in Post-Acute Sequela of COVID-19. J. Am. Coll. Cardiol. 2022, 79, 2325–2330. [Google Scholar] [CrossRef] [PubMed]
- Ruiz Maya, T.; Fettig, V.; Mehta, L.; Gelb, B.D.; Kontorovich, A.R. Dysautonomia in hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders is associated with exercise intolerance and cardiac atrophy. Am. J. Med. Genet. A. 2021, 185, 3754–3761. [Google Scholar] [CrossRef]
- Fu, Q.; VanGundy, T.B.; Galbreath, M.M.; Shibata, S.; Jain, M.; Hastings, J.L.; Bhella, P.S.; Levine, B.D. Cardiac origins of the postural orthostatic tachycardia syndrome. J. Am. Coll. Cardiol. 2010, 55, 2858–2868. [Google Scholar] [CrossRef]
- Novak, P.; Mukerji, S.S.; Alabsi, H.S.; Systrom, D.; Marciano, S.P.; Felsenstein, D.; Mullally, W.J.; Pilgrim, D.M. Multisystem Involvement in Post-Acute Sequelae of Coronavirus Disease 19. Ann. Neurol. 2022, 91, 367–379. [Google Scholar] [CrossRef]
- Shouman, K.; Vanichkachorn, G.; Cheshire, W.P.; Suarez, M.D.; Shelly, S.; Lamotte, G.J.; Sandroni, P.; Benarroch, E.E.; Berini, S.E.; Cutsforth-Gregory, J.K.; et al. Autonomic dysfunction following COVID-19 infection: An early experience. Clin. Auton. Res. 2021, 31, 385–394. [Google Scholar] [CrossRef]
- Monaghan, A.; Jennings, G.; Xue, F.; Byrne, L.; Duggan, E.; Romero-Ortuno, R. Orthostatic Intolerance in Adults Reporting Long COVID Symptoms Was Not Associated With Postural Orthostatic Tachycardia Syndrome. Front. Physiol. 2022, 13, 833650. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Post-COVID Conditions: Overview for Healthcare Providers. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html (accessed on 25 July 2022).
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- Goldstein, D.S. The possible association between COVID-19 and postural tachycardia syndrome. Heart Rhythm. 2021, 18, 508–509. [Google Scholar] [CrossRef]
- Bryarly, M.; Phillips, L.T.; Fu, Q.; Vernino, S.; Levine, B.D. Postural Orthostatic Tachycardia Syndrome: JACC Focus Seminar. J. Am. Coll. Cardiol. 2019, 73, 1207–1228. [Google Scholar] [CrossRef] [PubMed]
- George, S.A.; Bivens, T.B.; Howden, E.J.; Saleem, Y.; Galbreath, M.M.; Hendrickson, D.; Fu, Q.; Levine, B.D. The international POTS registry: Evaluating the efficacy of an exercise training intervention in a community setting. Heart Rhythm. 2016, 13, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Winker, R.; Barth, A.; Bidmon, D.; Ponocny, I.; Weber, M.; Mayr, O.; Robertson, D.; Diedrich, A.; Maier, R.; Pilger, A.; et al. Endurance exercise training in orthostatic intolerance: A randomized, controlled trial. Hypertension. 2005, 45, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Fu, Q.; Vangundy, T.B.; Shibata, S.; Auchus, R.J.; Williams, G.H.; Levine, B.D. Exercise training versus propranolol in the treatment of the postural orthostatic tachycardia syndrome. Hypertension 2011, 58, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Pavlik, D.; Agnew, D.; Stiles, L.; Ditoro, R. Recognizing postural orthostatic tachycardia syndrome. JAAPA 2016, 29, 17–23. [Google Scholar] [CrossRef]
- Blitshteyn, S.; Whiteson, J.H.; Abramoff, B.; Azola, A.; Bartels, M.N.; Bhavaraju-Sanka, R.; Chung, T.; Fleming, T.K.; Henning, E.; Miglis, M.G.; et al. Multi-disciplinary collaborative consensus guidance statement on the assessment and treatment of autonomic dysfunction in patients with post-acute sequelae of SARS-CoV-2 infection (PASC). PMR 2022, 14, 1270–1291. [Google Scholar]
| All Participants (n = 203) | Female (n = 135) | Male (n = 68) | Dysautonomia (n = 45) | Unclassified (n = 158) | |
|---|---|---|---|---|---|
| Female, n (%) | 135 (67%) | 135 (100) | 0 (0) | 37 (82) | 98 (62) |
| Age, y | 45 (22–80) | 46 (22–79) | 44 (23–80) | 47 (23–79) | 45 (22–80) |
| BSA | 1.9 (1.3–2.6) | 1.8 (1.3–2.5) | 2.1 (1.6–2.6) | 1.8 (1.4–2.3) | 1.9 (1.3–2.6) |
| Hospitalized for COVID-19, n (%) | 44 (22) | 29 (21) | 15 (22) | 8 (18) | 36 (23) |
| Mechanical ventilation, n (%) | 5 (2) | 5 (4) | 0 (0) | 0 (0) | 8 (18) |
| Duration of symptoms, days | 218 (34–500) | 221 (36–479) | 213 (34–500) | 212 (36–479) | 220 (34–500) |
| Parameter Reported (%) | Abnormal (%) | |
|---|---|---|
| LV systolic function | 203 (100) | 2 (1) |
| LV diastolic function | 189 (93) | 8 (4) |
| LV hypertrophy | 179 (88) | 20 (11) |
| LV dilatation | 203 (100) | 1 (0.5) |
| RV systolic function | 197 (97) | 0 (0) |
| RV size | 197 (97) | 2 (1) |
| Pulmonary hypertension | 77 (38) | 2 (3) |
| LA size | 127 (63) | 4 (3) |
| RA size | 127 (63) | 1 (1) |
| Mitral valve | 200 (99) | 1 (1) |
| Aortic valve | 200 (99) | 1 (1) |
| Tricuspid valve | 200 (99) | 0 (0) |
| Pulmonic valve | 200 (99) | 0 (0) |
| Pericardium | 113 (56) | 3 (3) |
| Aortic root dilatation | 85 (42) | 3 (4) |
| Miscellaneous | - | 3 (1) |
| All Participants (n = 200) | Dysautonomia (n = 44) | Unclassified (n = 156) | Difference | |
|---|---|---|---|---|
| LVIDd z score | −0.89 (−1.06–−0.72) | −1.16 (−1.55–−0.77) | −0.81 (−1.00–−0.62) | 0.35 (−0.06–0.72) |
| LVIDs z score a | −0.42 (−0.57–−0.28) | −0.50 (−0.82–−0.18) | −0.40 (−0.57–−0.18) | 0.10 (−0.26–0.45) |
| LVEDV a | 89.0 (85.3–92.5) | 82.5 (75.5–89.4) | 90.8 (86.6–94.9) | 8.3 (−0.3–16.9) |
| LVESV a | 39.3 (33.8–44.7) | 30.0 (25.0–35.0) | 42.2 (35.2–49.1) | 12.2 (−0.5–24.9) |
| SV a | 57.5 (54.9–60.1) | 51.6 (47.1–56.1) | 59.2 (56.2–62.3) | 7.6 (1.6–13.7) |
| LVMI | 85.2 (82.4–88.0) | 85.8 (79.3–92.3) | 85.0 (82.0–88.1) | 0.8 (−7.5–5.9) |
| Patient-Reported Outcome | All Participants (n = 99) | Dysautonomia (n = 27) | Unclassified (n = 72) | Difference (95% CI) |
|---|---|---|---|---|
| MRC breathlessness scale | 2 (1–4) | 2 (1–4) | 2 (1–4) | 0 (−1–0) |
| EQ-5D-5L domains | ||||
| Mobility | 2 (1–4) | 2 (1–4) | 2 (1–4) | 0 (−1–0) |
| Usual activities | 3 (1–5) | 3 (1–5) | 3 (1–5) | 0 (−1–1) |
| Anxiety/depression | 3 (1–4) | 3 (1–4) | 3 (1–4) | 0 (−1–1) |
| Self-care | 1 (1–3) | 1 (1–3) | 1 (1–3) | 0 (−1–0) |
| Pain/discomfort | 3 (1–4) | 3 (1–4) | 2 (1–4) | −1 (−1–0) |
| EQ-5D-5L health status VAS a,b | 59 (55–63) | 52 (43–60) | 61 (57–66) | 10 (1–19) |
| Fatigue Severity Scale, total score a,b | 49 (46–51) | 52 (48–56) | 48 (44–51) | −4 (−10–2) |
| Fatigue VAS (0 to 100) a,b | 44 (39–50) | 43 (32–55) | 45 (38–51) | 2 (−11–14) |
| Neuro-QOL, t score a,b | 41 (39–44) | 39 (34–44) | 42 (39–45) | 3 (−3–9) |
| GAD-7, total score a | 7 (6–8) | 8 (5–10) | 6 (5–8) | −1 (−4–1) |
| PHQ-2, total score a | 2 (2–2) | 2 (2–3) | 2 (2–2) | 0 (−1–0) |
| WHODAS, total score a,b | 32 (28–37) | 37 (29–45) | 30 (25–36) | −7 (−17–4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tabacof, L.; Wood, J.; Breyman, E.; Tosto-Mancuso, J.; Kelly, A.; Wilkey, K.; Zhang, C.; Putrino, D.; Kontorovich, A. Dysautonomia, but Not Cardiac Dysfunction, Is Common in a Cohort of Individuals with Long COVID. J. Pers. Med. 2023, 13, 1606. https://doi.org/10.3390/jpm13111606
Tabacof L, Wood J, Breyman E, Tosto-Mancuso J, Kelly A, Wilkey K, Zhang C, Putrino D, Kontorovich A. Dysautonomia, but Not Cardiac Dysfunction, Is Common in a Cohort of Individuals with Long COVID. Journal of Personalized Medicine. 2023; 13(11):1606. https://doi.org/10.3390/jpm13111606
Chicago/Turabian StyleTabacof, Laura, Jamie Wood, Erica Breyman, Jenna Tosto-Mancuso, Amanda Kelly, Kaitlyn Wilkey, Chi Zhang, David Putrino, and Amy Kontorovich. 2023. "Dysautonomia, but Not Cardiac Dysfunction, Is Common in a Cohort of Individuals with Long COVID" Journal of Personalized Medicine 13, no. 11: 1606. https://doi.org/10.3390/jpm13111606
APA StyleTabacof, L., Wood, J., Breyman, E., Tosto-Mancuso, J., Kelly, A., Wilkey, K., Zhang, C., Putrino, D., & Kontorovich, A. (2023). Dysautonomia, but Not Cardiac Dysfunction, Is Common in a Cohort of Individuals with Long COVID. Journal of Personalized Medicine, 13(11), 1606. https://doi.org/10.3390/jpm13111606








