Surgical Outcomes of Lensectomy-Vitrectomy with Primary Intraocular Lens Implantation in Children with Bilateral Congenital Cataracts
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
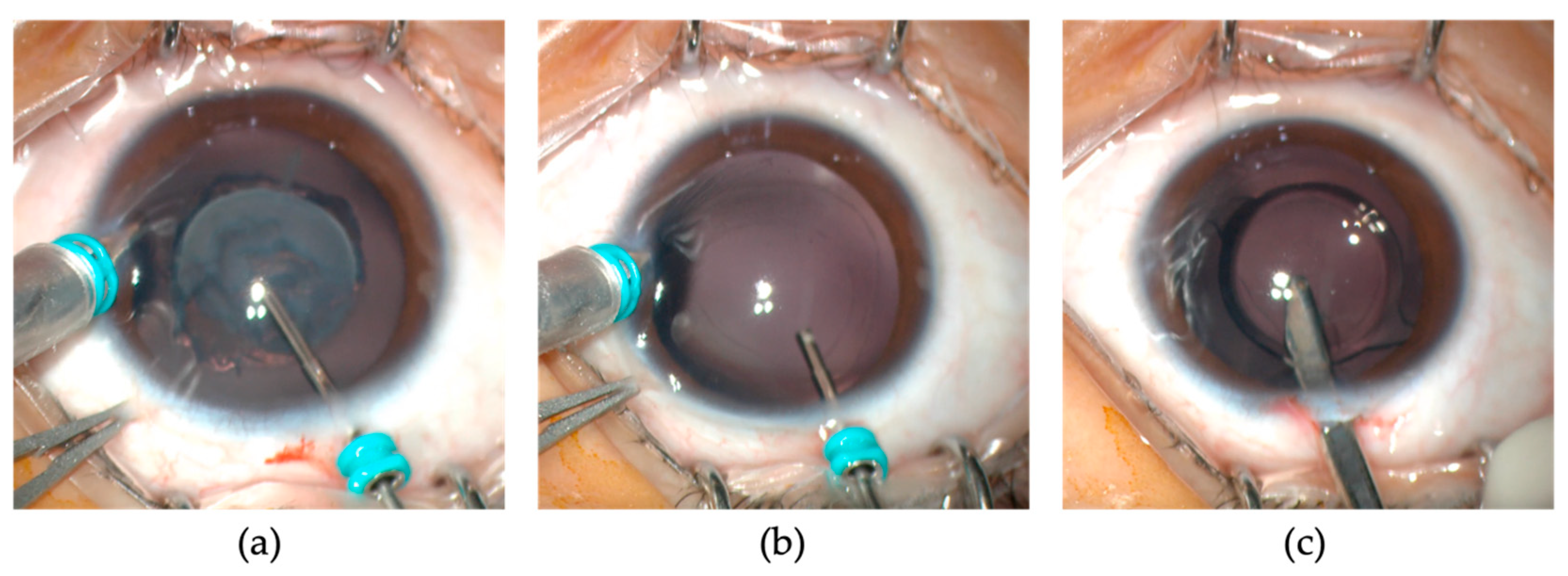
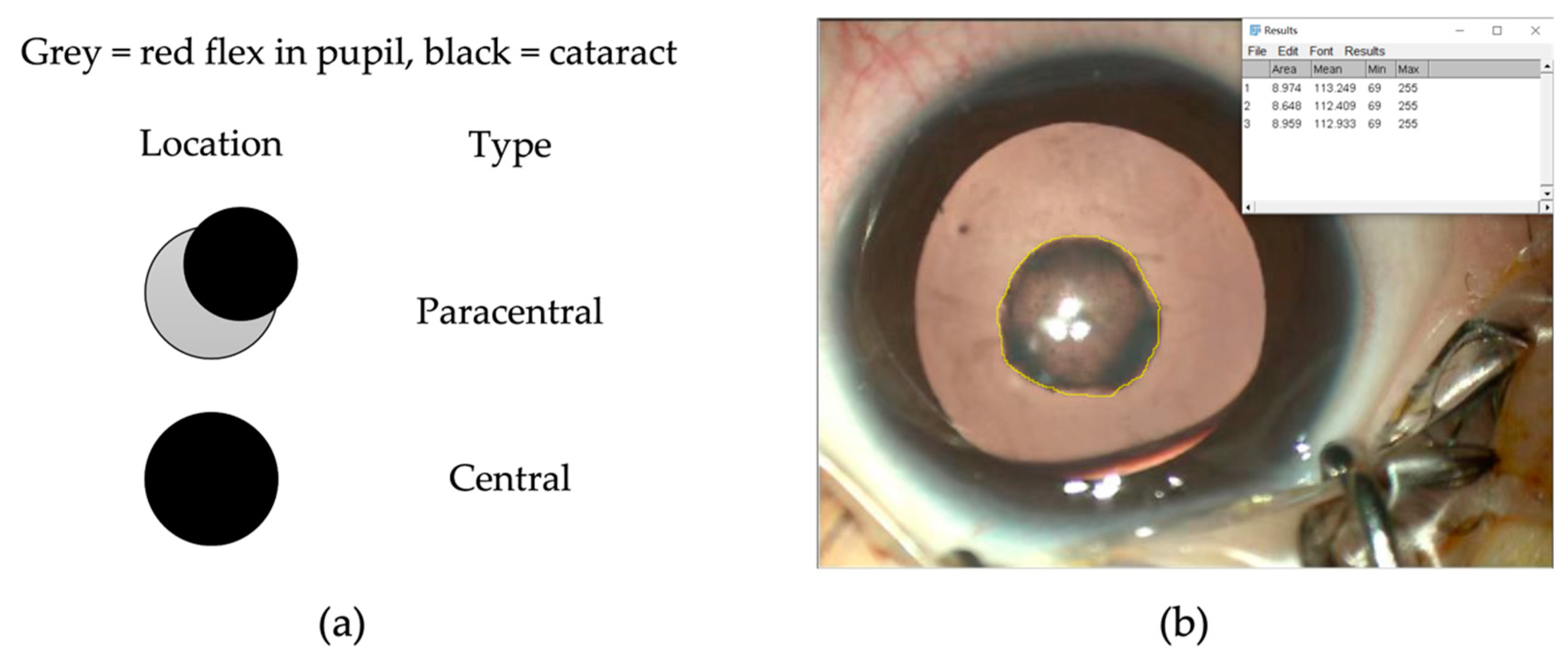
2.2. Surgical Technique
2.3. Follow-Up and Amblyopia Treatment
2.4. Ophthalmic Examinations
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Singh, R.; Barker, L.; Chen, S.I.; Shah, A.; Long, V.; Dahlmann-Noor, A. Surgical interventions for bilateral congenital cataract in children aged two years and under. Cochrane Database Syst. Rev. 2022, 9, cd003171. [Google Scholar] [CrossRef] [PubMed]
- Pichi, F.; Lembo, A.; Serafino, M.; Nucci, P. Genetics of Congenital Cataract. Dev. Ophthalmol. 2016, 57, 1–14. [Google Scholar] [CrossRef]
- Wu, X.; Long, E.; Lin, H.; Liu, Y. Prevalence and epidemiological characteristics of congenital cataract: A systematic review and meta-analysis. Sci. Rep. 2016, 6, 28564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Esposito Veneruso, P.; Ziccardi, L.; Magli, G.; Parisi, V.; Falsini, B.; Magli, A. Developmental visual deprivation: Long term effects on human cone driven retinal function. Graefes Arch. Clin. Exp. Ophthalmol. 2017, 255, 2481–2486. [Google Scholar] [CrossRef] [PubMed]
- Mansouri, B.; Stacy, R.C.; Kruger, J.; Cestari, D.M. Deprivation amblyopia and congenital hereditary cataract. Semin. Ophthalmol. 2013, 28, 321–326. [Google Scholar] [CrossRef]
- Mataftsi, A.; Haidich, A.B.; Kokkali, S.; Rabiah, P.K.; Birch, E.; Stager, D.R., Jr.; Cheong-Leen, R.; Singh, V.; Egbert, J.E.; Astle, W.F.; et al. Postoperative glaucoma following infantile cataract surgery: An individual patient data meta-analysis. JAMA Ophthalmol. 2014, 132, 1059–1067. [Google Scholar] [CrossRef]
- Solebo, A.L.; Rahi, J.S. Visual Axis Opacity after Intraocular Lens Implantation in Children in the First 2 Years of Life: Findings from the IoLunder2 Cohort Study. Ophthalmology 2020, 127, 1220–1226. [Google Scholar] [CrossRef]
- Plager, D.A.; Lynn, M.J.; Buckley, E.G.; Wilson, M.E.; Lambert, S.R. Complications in the first 5 years following cataract surgery in infants with and without intraocular lens implantation in the Infant Aphakia Treatment Study. Am. J. Ophthalmol. 2014, 158, 892–898. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.S.; Wang, J.D.; Yusufu, M.; Cao, K.; Jin, S.S.; Xiong, Y.; Li, J.; Sun, X.L.; Chen, S.Y.; Liu, Z.Y.; et al. The effect of retaining intact posterior capsule in congenital cataract surgery in children aged 4-8 years. BMC Ophthalmol. 2021, 21, 332. [Google Scholar] [CrossRef]
- Liu, X.; Zheng, T.; Zhou, X.; Lu, Y.; Zhou, P.; Fan, F.; Luo, Y. Comparison between Limbal and Pars Plana Approaches Using Microincision Vitrectomy for Removal of Congenital Cataracts with Primary Intraocular Lens Implantation. J. Ophthalmol. 2016, 2016, 8951053. [Google Scholar] [CrossRef]
- Liu, X.; Luo, Y.; Zhou, X.; Jiang, L.; Zhou, P.; Lu, Y. Combined pars plana and limbal approach for removal of congenital cataracts. J. Cataract. Refract. Surg. 2012, 38, 2066–2070. [Google Scholar] [CrossRef] [PubMed]
- Tartarella, M.B.; Fortes Filho, J.B. Twenty-five-gauge sutureless lensectomy in infants with congenital cataract. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2017, 21, 393–396. [Google Scholar] [CrossRef] [PubMed]
- Chee, K.Y.; Lam, G.C. Management of congenital cataract in children younger than 1 year using a 25-gauge vitrectomy system. J. Cataract. Refract. Surg. 2009, 35, 720–724. [Google Scholar] [CrossRef]
- Meier, P.; Sterker, I.; Tegetmeyer, H.; Wiedemann, P. 23-gauge-lentectomy for the treatment of congenital cataract. Ophthalmologe 2010, 107, 241–245. [Google Scholar] [CrossRef]
- Huang, Y.; Xie, L. Short-term outcomes of dry pars plana posterior capsulotomy and anterior vitrectomy in paediatric cataract surgery using 25-gauge instruments. Br. J. Ophthalmol. 2010, 94, 1024–1027. [Google Scholar] [CrossRef] [PubMed]
- Gogate, P.M.; Sahasrabudhe, M.; Shah, M.; Patil, S.; Kulkarni, A.N.; Trivedi, R.; Bhasa, D.; Tamboli, R.; Mane, R. Long term outcomes of bilateral congenital and developmental cataracts operated in Maharashtra, India. Miraj pediatric cataract study III. Indian J. Ophthalmol. 2014, 62, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.H.; Hossain, A.; Ferdausi, N.; Islam, M.Z.; Sen, U. Visual Outcomes of Congenital Cataract Surgery in a Tertiary Public Hospital in Bangladesh. Asia Pac. J. Ophthalmol. 2015, 4, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Khanna, R.C.; Foster, A.; Krishnaiah, S.; Mehta, M.K.; Gogate, P.M. Visual outcomes of bilateral congenital and developmental cataracts in young children in south India and causes of poor outcome. Indian J. Ophthalmol. 2013, 61, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Chak, M.; Wade, A.; Rahi, J.S. Long-term visual acuity and its predictors after surgery for congenital cataract: Findings of the British congenital cataract study. Invest. Ophthalmol. Vis. Sci. 2006, 47, 4262–4269. [Google Scholar] [CrossRef]
- You, C.; Wu, X.; Zhang, Y.; Dai, Y.; Huang, Y.; Xie, L. Visual impairment and delay in presentation for surgery in chinese pediatric patients with cataract. Ophthalmology 2011, 118, 17–23. [Google Scholar] [CrossRef]
- Forster, J.E.; Abadi, R.V.; Muldoon, M.; Lloyd, I.C. Grading infantile cataracts. Ophthalmic Physiol. Opt. 2006, 26, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Mndeme, F.G.; Mmbaga, B.T.; Msina, M.; Mwende, J.; Vaitha, S.J.; Kim, M.J.; Macleod, D.; Burton, M.J.; Gilbert, C.E.; Bowman, R. Presentation, surgery and 1-year outcomes of childhood cataract surgery in Tanzania. Br. J. Ophthalmol. 2021, 105, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Chen, H.; Lin, Z.; Lin, H.; Wang, J.; Chen, J.; Wang, Q.; Zhao, Z.; Lin, Z.; Lin, X.; et al. Visual Function in Children with Posterior Lens Opacities before and after Surgery. Am. J. Ophthalmol. 2022, 241, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Sjöstrand, J.; Magnusson, G.; Nyström, A.; Jonsson, R. Stability of visual outcome from 7 years in children treated surgically for bilateral dense congenital cataracts before 37 weeks of age. Acta Ophthalmol. 2011, 89, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Li, S.Y.; Zhang, Z.P.; Ji, S.J.; Liu, H.Y.; Si, M.Y.; Fan, K.S. Application of minimally invasive 23G vitrectomy via corneal approach for the treatment of pediatric cataract. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 2413–2418. [Google Scholar] [PubMed]
- Bowman, R.J.; Kabiru, J.; Negretti, G.; Wood, M.L. Outcomes of bilateral cataract surgery in Tanzanian children. Ophthalmology 2007, 114, 2287–2292. [Google Scholar] [CrossRef]
- Congdon, N.G.; Ruiz, S.; Suzuki, M.; Herrera, V. Determinants of pediatric cataract program outcomes and follow-up in a large series in Mexico. J. Cataract. Refract. Surg. 2007, 33, 1775–1780. [Google Scholar] [CrossRef]
- Lloyd, I.C.; Dowler, J.G.; Kriss, A.; Speedwell, L.; Thompson, D.A.; Russell-Eggitt, I.; Taylor, D. Modulation of amblyopia therapy following early surgery for unilateral congenital cataracts. Br. J. Ophthalmol. 1995, 79, 802–806. [Google Scholar] [CrossRef]
- Solebo, A.L.; Russell-Eggitt, I.; Cumberland, P.M.; Rahi, J.S. Risks and outcomes associated with primary intraocular lens implantation in children under 2 years of age: The IoLunder2 cohort study. Br. J. Ophthalmol. 2015, 99, 1471–1476. [Google Scholar] [CrossRef] [Green Version]
- Solebo, A.L.; Rahi, J.S. Glaucoma following cataract surgery in the first 2 years of life: Frequency, risk factors and outcomes from IoLunder2. Br. J. Ophthalmol. 2020, 104, 967–973. [Google Scholar] [CrossRef]
- Lambert, S.R.; Lynn, M.J.; Hartmann, E.E.; DuBois, L.; Drews-Botsch, C.; Freedman, S.F.; Plager, D.A.; Buckley, E.G.; Wilson, M.E. Comparison of contact lens and intraocular lens correction of monocular aphakia during infancy: A randomized clinical trial of HOTV optotype acuity at age 4.5 years and clinical findings at age 5 years. JAMA Ophthalmol. 2014, 132, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Freedman, S.F.; Beck, A.D.; Nizam, A.; Vanderveen, D.K.; Plager, D.A.; Morrison, D.G.; Drews-Botsch, C.D.; Lambert, S.R. Glaucoma-Related Adverse Events at 10 Years in the Infant Aphakia Treatment Study: A Secondary Analysis of a Randomized Clinical Trial. JAMA Ophthalmol. 2021, 139, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Bothun, E.D.; Cleveland, J.; Lynn, M.J.; Christiansen, S.P.; Vanderveen, D.K.; Neely, D.E.; Kruger, S.J.; Lambert, S.R. One-year strabismus outcomes in the Infant Aphakia Treatment Study. Ophthalmology 2013, 120, 1227–1231. [Google Scholar] [CrossRef] [Green Version]
- Birch, E.E.; Wang, J.; Felius, J.; Stager, D.R., Jr.; Hertle, R.W. Fixation control and eye alignment in children treated for dense congenital or developmental cataracts. J. Am. Assoc. Pediatr. Ophthalmol. 2012, 16, 156–160. [Google Scholar] [CrossRef] [Green Version]
- Rong, X.; Ji, Y.; Fang, Y.; Jiang, Y.; Lu, Y. Long-Term Visual Outcomes of Secondary Intraocular Lens Implantation in Children with Congenital Cataracts. PLoS ONE 2015, 10, e0134864. [Google Scholar] [CrossRef]
- Parks, M.M.; Johnson, D.A.; Reed, G.W. Long-term visual results and complications in children with aphakia. A function of cataract type. Ophthalmology 1993, 100, 826–840. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Chen, W.; Wu, X.H.; Lin, Z.L.; Chen, J.J.; Li, X.Y.; Chen, W.R.; Lin, H.T. Visual outcomes of surgical and conservative treatment in children with small posterior polar cataracts and posterior lenticonus. Int. J. Ophthalmol. 2021, 14, 64–71. [Google Scholar] [CrossRef]
- Crouch, E.R.; Crouch, E.R., Jr.; Pressman, S.H. Prospective analysis of pediatric pseudophakia: Myopic shift and postoperative outcomes. J. Am. Assoc. Pediatr. Ophthalmol. 2002, 6, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Yangzes, S.; Kaur, S.; Gupta, P.C.; Sharma, M.; Jinagal, J.; Singh, J.; Ram, J. Intraocular lens implantation in children with unilateral congenital cataract in the first 4 years of life. Eur. J. Ophthalmol. 2019, 29, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Magli, A.; Forte, R.; Rombetto, L. Long-term outcome of primary versus secondary intraocular lens implantation after simultaneous removal of bilateral congenital cataract. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 309–314. [Google Scholar] [CrossRef]
- Solebo, A.L.; Cumberland, P.; Rahi, J.S. 5-year outcomes after primary intraocular lens implantation in children aged 2 years or younger with congenital or infantile cataract: Findings from the IoLunder2 prospective inception cohort study. Lancet Child. Adolesc. Health 2018, 2, 863–871. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bothun, E.D.; Wilson, M.E.; Vanderveen, D.K.; Plager, D.A.; Freedman, S.F.; Trivedi, R.H.; Traboulsi, E.I.; Anderson, J.S.; Loh, A.R.; Yen, K.G.; et al. Outcomes of Bilateral Cataracts Removed in Infants 1 to 7 Months of Age Using the Toddler Aphakia and Pseudophakia Treatment Study Registry. Ophthalmology 2020, 127, 501–510. [Google Scholar] [CrossRef] [PubMed]
| Age at IOL Implantation (Years) | Target Hyperopia Diopter (D) |
|---|---|
| 1 ~ 2 | +5 ~ +6 |
| 2 ~ 3 | +4 ~ +5 |
| 3 ~ 4 | +3 ~ +4 |
| 4 ~ 5 | +2 ~ +3 |
| 5 ~ 6 | +1 ~ +2 |
| Characteristics | Mean ± SD or N (%) |
|---|---|
| Patients/eyes | 74/148 |
| Male/female | 44/30 |
| Cataract morphology | |
| Total | 50 (33.8) |
| Nuclear | 32 (21.6) |
| Lamellar | 38 (25.7) |
| Posterior polar | 10 (6.7) |
| Other types | 18 (12.2) |
| Preexisting comorbidity | |
| strabismus | 26 (17.6) |
| nystagmus | 20 (13.5) |
| Preoperative AL (mm) | 21.55 ± 1.45 (19.14–26.70) |
| Surgery age (months) | 44.04 ± 14.60 (19–71) |
| Follow-up (months) | 46.66 ± 14.34 (12–72) |
| Age at last follow-up (years) | 7.56 ± 0.75 (6.4–9.4) |
| Characteristics | All (n = 148) | Younger Children (≤2 Years Old) (n = 14) | Elder Group (>2 Years Old) (n = 124) | p Value |
|---|---|---|---|---|
| BCVA (logMAR) | 0.24 ± 0.32 | 0.26 ± 0.30 | 0.24 ± 0.32 | 0.834 |
| Low vision, n (%) | 22 (14.9) | 3 (27.2) | 19 (15.8) | 0.439 |
| Refractive error at last follow-up (ASE, D) | 2.07 ± 1.78 | 2.60 ± 2.06 | 2.01 ± 1.74 | 0.047 * |
| Postoperative complications requiring surgeries, n (%) | 8 (5.4) | 3 (21.4) | 5 (4.0) | 0.029 * |
| Early postoperative complications | ||||
| IOL pupillary capture | 2 (1.3) | 0 (0.0) | 2 (1.4) | 0.819 |
| Iris incarceration in incision | 1 (0.7) | 0 (0.0) | 1 (0.8) | 0.905 |
| Late postoperative complications | ||||
| VAO | 4 (2.7) | 3 (21.4) | 1 (0.8) | 0.003 * |
| Glaucoma | 1 (0.7) | 0 (0.0) | 1 (0.8) | 0.905 |
| Characteristics | Low Vision Group (n = 22) | Non-Low Vision Group (2 = 126) | p Value |
|---|---|---|---|
| Gender (male: female) | 12:10 | 76:50 | 0.389 |
| Cataract density (grade ≤7: grade >7) | 1:21 | 43:83 | 0.003 * |
| Cataract location (central: paracentral) | 7:15 | 53:73 | 0.254 |
| cataract size (mm2) | 15.38 ± 6.73 | 11.68 ± 6.08 | 0.038 * |
| Preoperative comorbidity (yes: no) | 14:8 | 22:104 | <0.001 * |
| Preoperative AL (mm) | 22.00 ± 1.53 | 21.47 ± 1.42 | 0.114 |
| Surgery age (months) | 45.55 ± 14.17 | 43.78 ± 14.72 | 0.241 |
| Follow-up period (months) | 45.16 ± 12.37 | 46.92 ± 14.68 | 0.136 |
| Refractive error (ASE, D) | 2.78 ± 1.63 | 1.94 ± 1.78 | 0.035 * |
| postoperative complications (yes: no) | 3:19 | 5:121 | 0.097 |
| Characteristics | OR | 95% CI | p Value |
|---|---|---|---|
| Cataract density | |||
| grade ≤ 7 | - | - | - |
| grade > 7 | 9.303 | 1.171–73.903 | 0.035 * |
| cataract size (mm2) | 1.033 | 0.978–1.092 | 0.247 |
| Preexisting comorbidity | |||
| no | - | - | - |
| yes | 4.712 | 1.656–13.410 | 0.004 * |
| Refractive error (ASE, D) | 1.154 | 0.891–1.494 | 0.277 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, H.; Lin, X.; Liu, X.; Zhou, X.; Yang, T.; Fan, F.; Luo, Y. Surgical Outcomes of Lensectomy-Vitrectomy with Primary Intraocular Lens Implantation in Children with Bilateral Congenital Cataracts. J. Pers. Med. 2023, 13, 189. https://doi.org/10.3390/jpm13020189
Li H, Lin X, Liu X, Zhou X, Yang T, Fan F, Luo Y. Surgical Outcomes of Lensectomy-Vitrectomy with Primary Intraocular Lens Implantation in Children with Bilateral Congenital Cataracts. Journal of Personalized Medicine. 2023; 13(2):189. https://doi.org/10.3390/jpm13020189
Chicago/Turabian StyleLi, Hongzhe, Xiaolei Lin, Xin Liu, Xiyue Zhou, Tianke Yang, Fan Fan, and Yi Luo. 2023. "Surgical Outcomes of Lensectomy-Vitrectomy with Primary Intraocular Lens Implantation in Children with Bilateral Congenital Cataracts" Journal of Personalized Medicine 13, no. 2: 189. https://doi.org/10.3390/jpm13020189





