Comparison of the Accuracy of 2D and 3D Templating for Revision Total Hip Replacement
Abstract
:1. Introduction
2. Materials and Methods
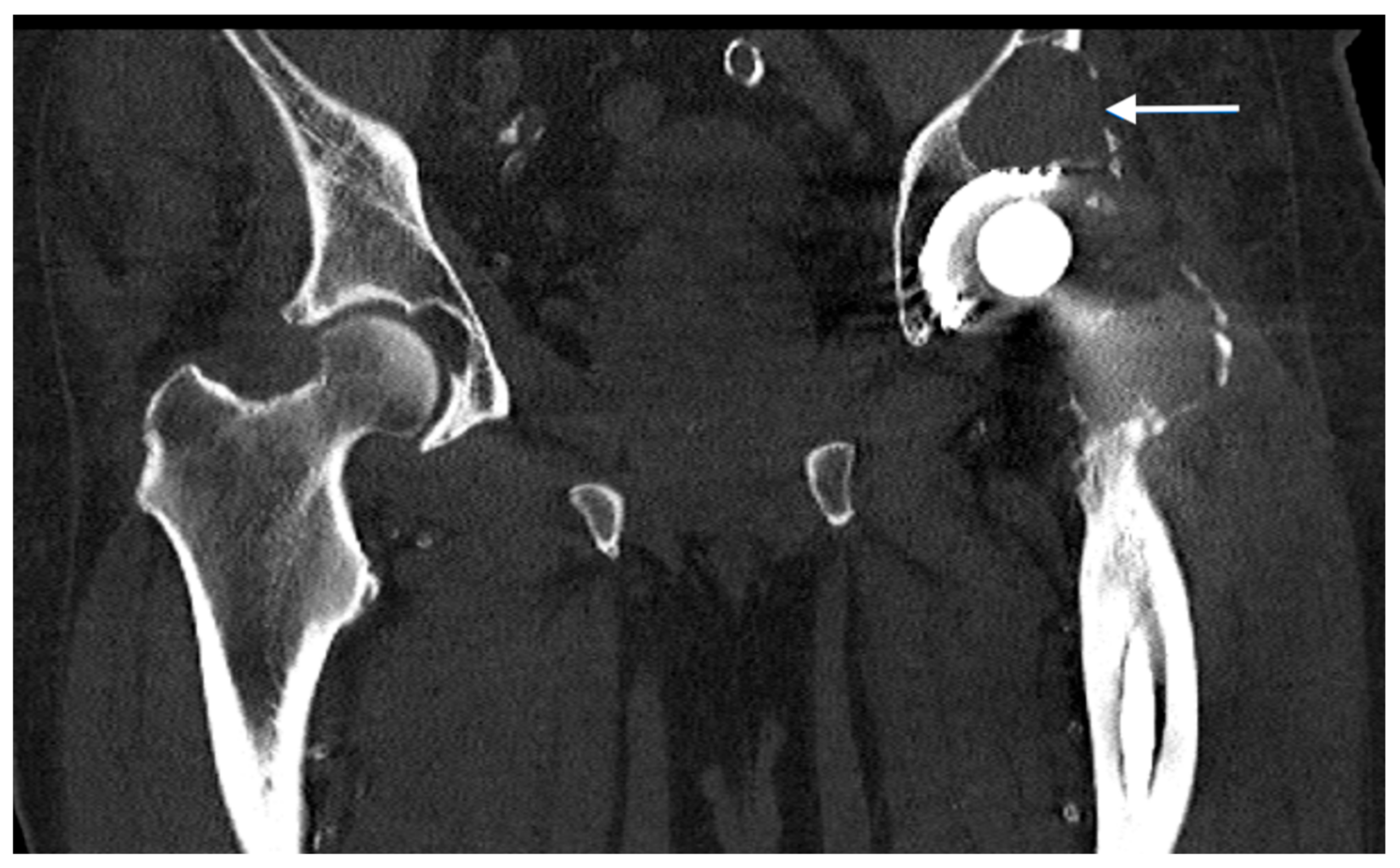
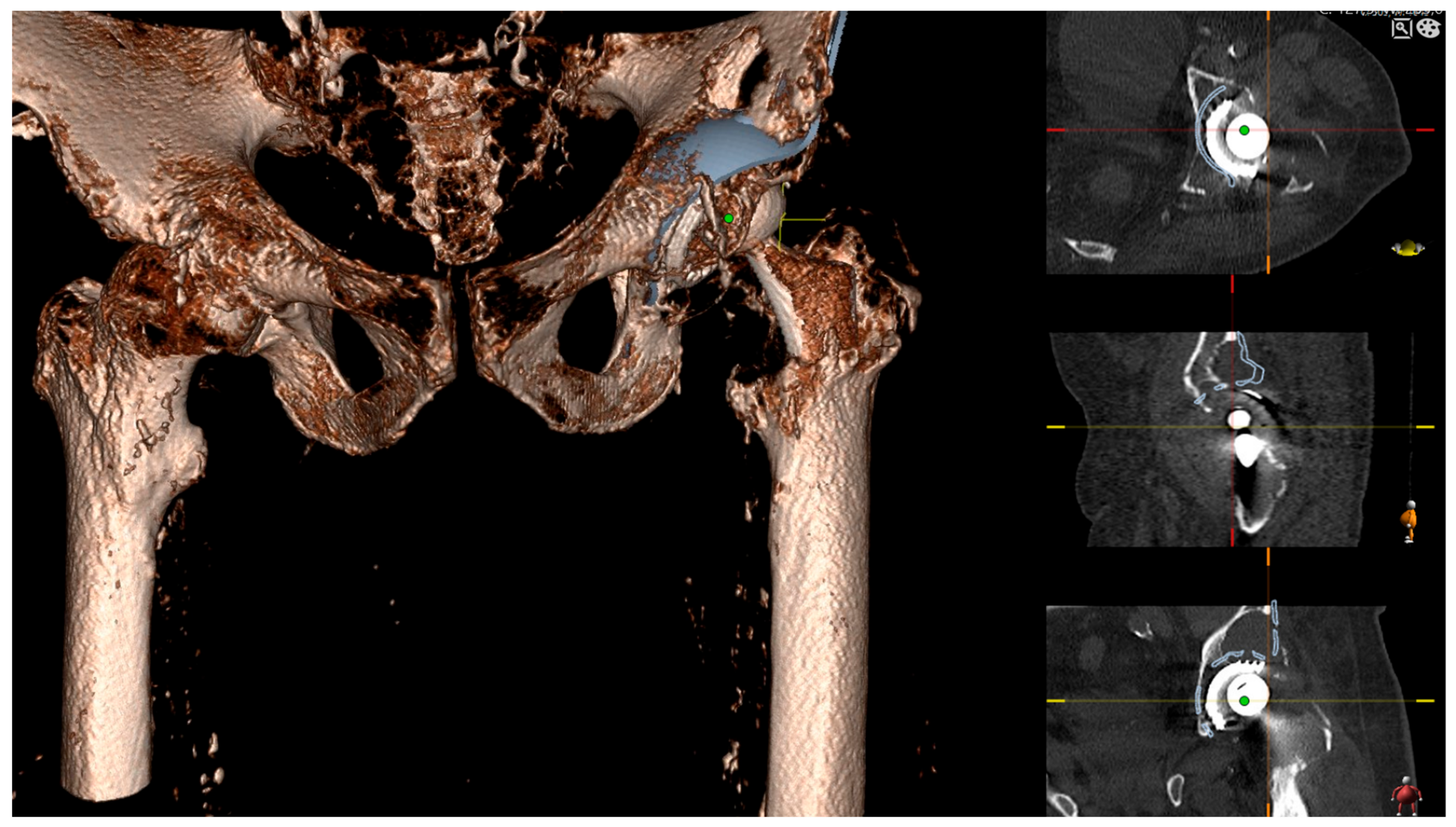
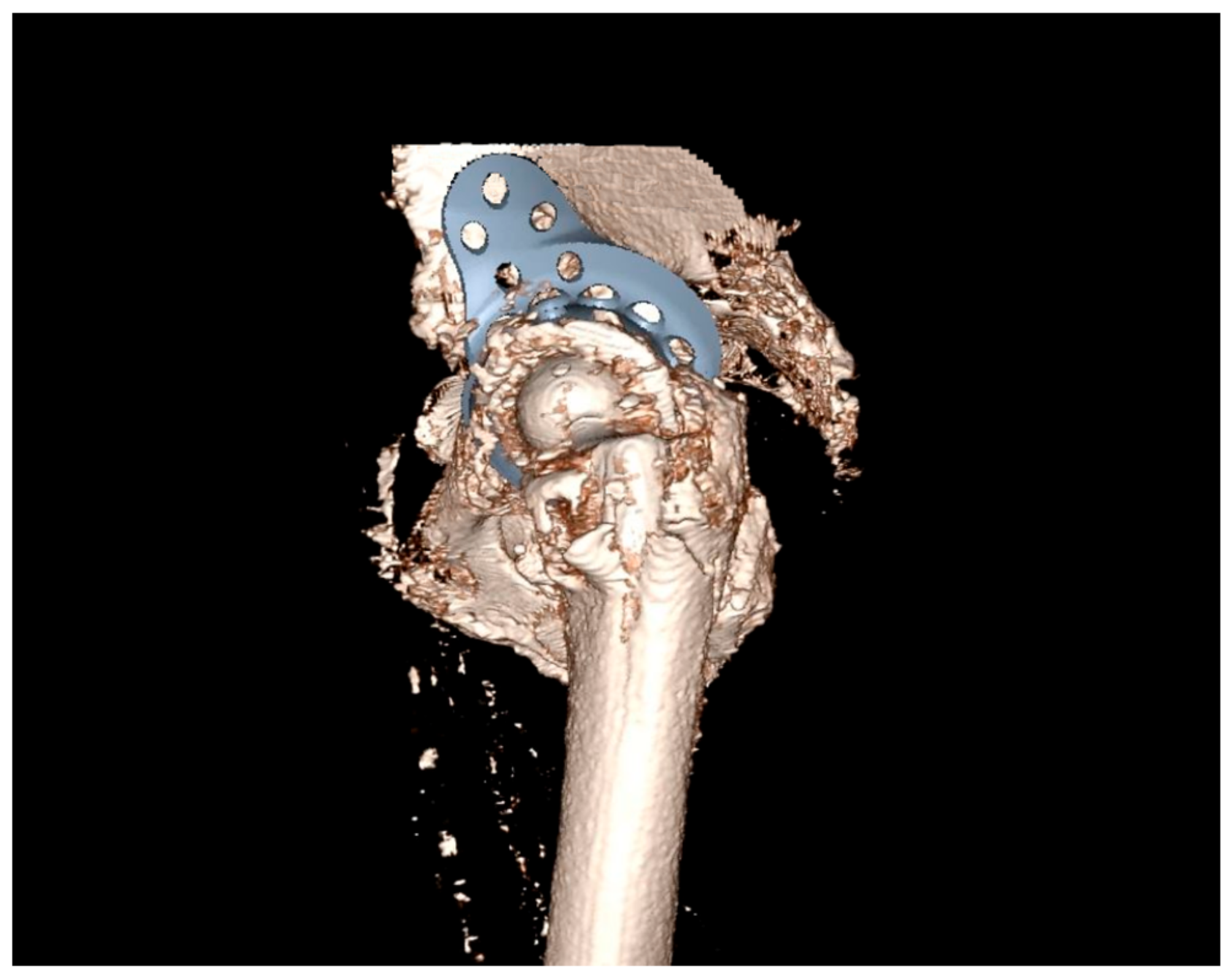
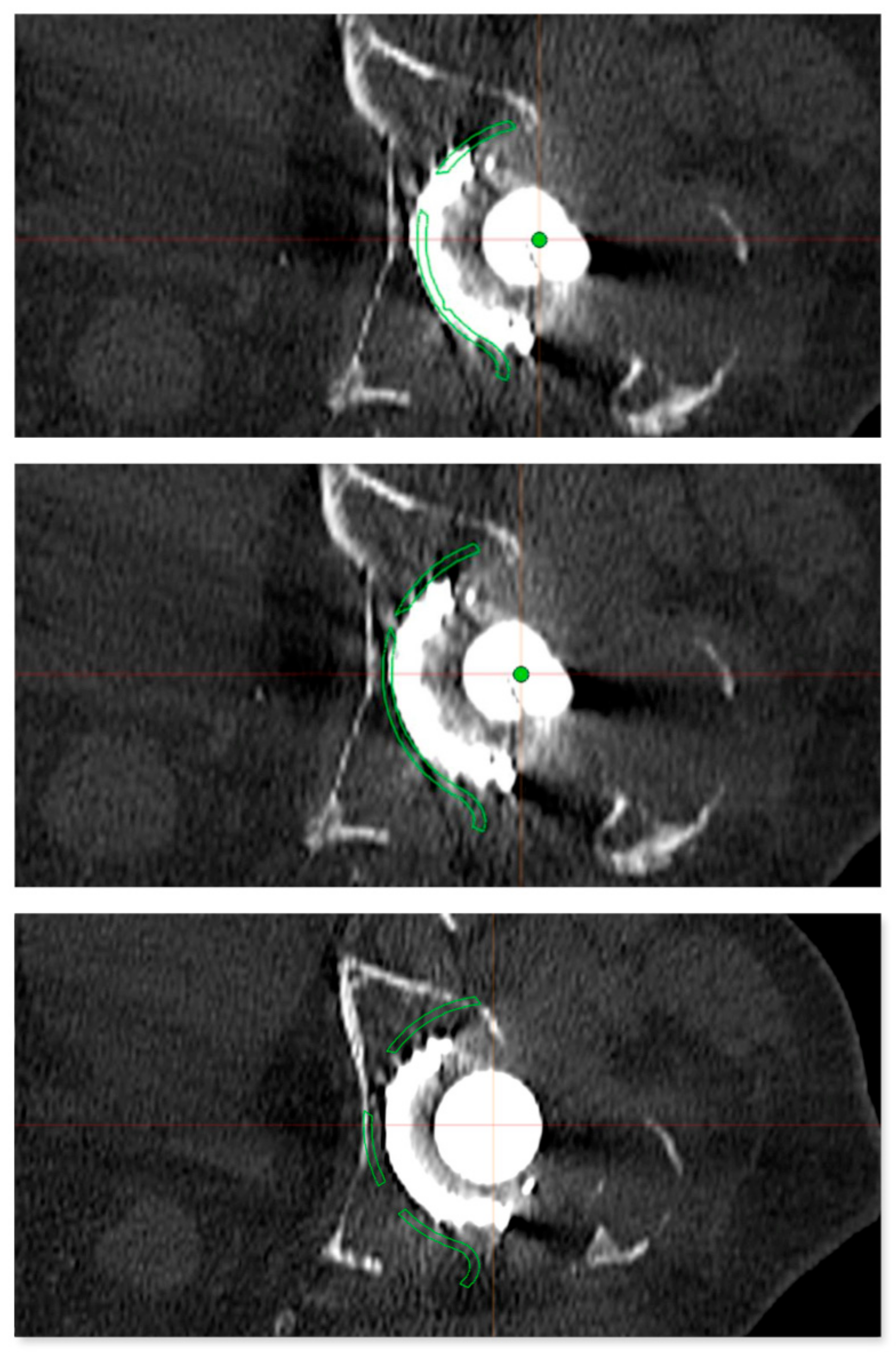
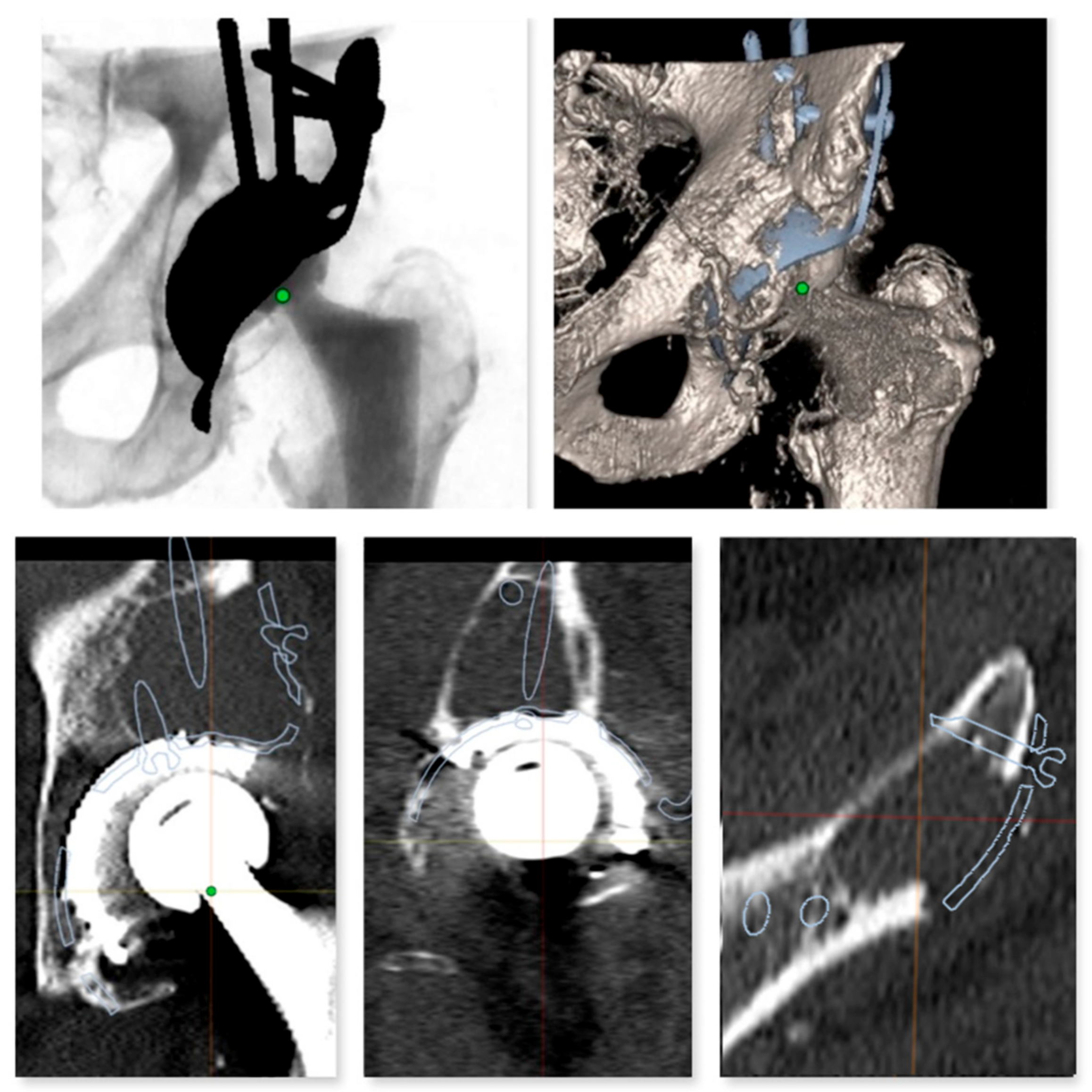
2.1. Preoperative Imaging
2.2. Digital Templating
2.3. Surgical Procedure
2.4. Statistical Analysis
3. Results
3.1. Gender and Planning Accuracy
3.2. BMI and Planning Accuracy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 2D Templating | Final Implant | 3D Templating | ||
|---|---|---|---|---|
| Patient number | 1 | 62 mm | 56 mm | 56 mm |
| 2 | 56 mm | 56 mm | 56 mm | |
| 3 | 56 mm | 56 mm | 56 mm | |
| 4 | 56 mm | 56 mm | 56 mm | |
| 5 | 50 mm | 50 mm | 50 mm | |
| 6 | 56 mm | 56 mm | 56 mm | |
| 7 | 56 mm | 56 mm | 56 mm | |
| 8 | 44 mm | 50 mm | 50 mm | |
| 9 | 50 mm | 56 mm | 56 mm | |
| 10 | 50 mm | 56 mm | 56 mm | |
| 11 | 50 mm | 50 mm | 50 mm | |
| 12 | 56 mm | 56 mm | 56 mm | |
| 13 | 62 mm | 62 mm | 62 mm | |
| 14 | 62 mm | 56 mm | 56 mm | |
| 15 | 50 mm | 56 mm | 56 mm | |
| 16 | 56 mm | 56 mm | 56 mm | |
| 17 | 50 mm | 62 mm | 62 mm | |
| 18 | 50 mm | 50 mm | 50 mm | |
| 19 | 56 mm | 62 mm | 62 mm | |
| 20 | 50 mm | 56 mm | 56 mm | |
| 21 | 56 mm | 56 mm | 50 mm | |
| 22 | 56 mm | 56 mm | 56 mm | |
| 23 | 56 mm | 62 mm | 62 mm | |
| 24 | 62 mm | 62 mm | 62 mm | |
| 25 | 56 mm | 62 mm | 62 mm | |
| 26 | 62 mm | 56 mm | 56 mm | |
| 27 | 50 mm | 50 mm | 50 mm | |
| 54.6 mm | 56.2 mm | 56.0 mm | ||
References
- Kurtz, S.M.; Ong, K.L.; Schmier, J.; Mowat, F.; Saleh, K.; Dybvik, E.; Kärrholm, J.; Garellick, G.; Havelin, L.I.; Furnes, O.; et al. Future Clinical and Economic Impact of Revision Total Hip and Knee Arthroplasty. J. Bone Joint Surg. Am. 2007, 89 (Suppl. S3), 144–151. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, S.D.; Seyler, T.M.; Bennett, D.; Delanois, R.E.; Saleh, K.J.; Thongtrangan, I.; Kuskowski, M.; Cheng, E.Y.; Sharkey, P.F.; Parvizi, J.; et al. Total Hip Arthroplasties: What Are the Reasons for Revision? Int. Orthop. 2008, 32, 597–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelmer, G.; Stone, A.H.; Turcotte, J.; King, P.J. Reasons for Revision: Primary Total Hip Arthroplasty Mechanisms of Failure. J. Am. Acad. Orthop. Surg. 2021, 29, 78–87. [Google Scholar] [CrossRef] [PubMed]
- Barrack, R.L. Preoperative Planning for Revision Total Hip Arthroplasty. Clin. Orthop. 2004, 87, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Haddad, F.S.; Masri, B.A.; Garbuz, D.S.; Duncan, C.P. The Prevention of Periprosthetic Fractures in Total Hip and Knee Arthroplasty. Orthop. Clin. North Am. 1999, 30, 191–207. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Kim, V.E. Uncemented Porous-Coated Anatomic Total Hip Replacement. Results at Six Years in a Consecutive Series. J. Bone Joint Surg. Br. 1993, 75, 6–13. [Google Scholar] [CrossRef] [Green Version]
- Della Valle, A.G.; Padgett, D.E.; Salvati, E.A. Preoperative Planning for Primary Total Hip Arthroplasty. J. Am. Acad. Orthop. Surg. 2005, 13, 455–462. [Google Scholar] [CrossRef]
- Kosashvili, Y.; Shasha, N.; Olschewski, E.; Safir, O.; White, L.; Gross, A.; Backstein, D. Digital versus Conventional Templating Techniques in Preoperative Planning for Total Hip Arthroplasty. Can. J. Surg. 2009, 52, 6–11. [Google Scholar]
- White, S.P.; Shardlow, D.L. Effect of Introduction of Digital Radiographic Techniques on Pre-Operative Templating in Orthopaedic Practice. Ann. R. Coll. Surg. Engl. 2005, 87, 53–54. [Google Scholar] [CrossRef] [Green Version]
- Sinclair, V.F.; Wilson, J.; Jain, N.P.M.; Knowles, D. Assessment of Accuracy of Marker Ball Placement in Pre-Operative Templating for Total Hip Arthroplasty. J. Arthroplast. 2014, 29, 1658–1660. [Google Scholar] [CrossRef]
- Franken, M.; Grimm, B.; Heyligers, I. A Comparison of Four Systems for Calibration When Templating for Total Hip Replacement with Digital Radiography. J. Bone Joint Surg. Br. 2010, 92, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Sariali, E.; Mauprivez, R.; Khiami, F.; Pascal-Mousselard, H.; Catonné, Y. Accuracy of the Preoperative Planning for Cementless Total Hip Arthroplasty. A Randomised Comparison between Three-Dimensional Computerised Planning and Conventional Templating. Orthop. Traumatol. Surg. Res. OTSR 2012, 98, 151–158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bishi, H.; Smith, J.B.V.; Asopa, V.; Field, R.E.; Wang, C.; Sochart, D.H. Comparison of the Accuracy of 2D and 3D Templating Methods for Planning Primary Total Hip Replacement: A Systematic Review and Meta-Analysis. EFORT Open Rev. 2022, 7, 70–83. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [CrossRef] [Green Version]
- Paprosky, W.G.; Perona, P.G.; Lawrence, J.M. Acetabular Defect Classification and Surgical Reconstruction in Revision Arthroplasty. A 6-Year Follow-up Evaluation. J. Arthroplast. 1994, 9, 33–44. [Google Scholar] [CrossRef]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 January 2023).
- Maryada, V.R.; Mulpur, P.; Eachempati, K.K.; Annapareddy, A.; Badri Narayana Prasad, V.; Gurava Reddy, A.V. Pre-Operative Planning and Templating with 3-D Printed Models for Complex Primary and Revision Total Hip Arthroplasty. J. Orthop. 2022, 34, 240–245. [Google Scholar] [CrossRef]
- Chiarlone, F.; Zanirato, A.; Cavagnaro, L.; Alessio-Mazzola, M.; Felli, L.; Burastero, G. Acetabular Custom-Made Implants for Severe Acetabular Bone Defect in Revision Total Hip Arthroplasty: A Systematic Review of the Literature. Arch. Orthop. Trauma Surg. 2020, 140, 415–424. [Google Scholar] [CrossRef]
- Berend, M.E.; Berend, K.R.; Lombardi, A.V.; Cates, H.; Faris, P. The Patient-Specific Triflange Acetabular Implant for Revision Total Hip Arthroplasty in Patients with Severe Acetabular Defects: Planning, Implantation, and Results. Bone Jt. J. 2018, 100, 50–54. [Google Scholar] [CrossRef]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. Do Custom 3D-Printed Revision Acetabular Implants Provide Enough Value to Justify the Additional Costs? The Health-Economic Comparison of a New Porous 3D-Printed Hip Implant for Revision Arthroplasty of Paprosky Type 3B Acetabular Defects and Its Closest Alternative. Orthop. Traumatol. Surg. Res. OTSR 2021, 107, 102600. [Google Scholar] [CrossRef]
- Ballard, D.H.; Mills, P.; Duszak, R.; Weisman, J.A.; Rybicki, F.J.; Woodard, P.K. Medical 3D Printing Cost-Savings in Orthopedic and Maxillofacial Surgery: Cost Analysis of Operating Room Time Saved with 3D Printed Anatomic Models and Surgical Guides. Acad. Radiol. 2020, 27, 1103–1113. [Google Scholar] [CrossRef]
- Martelli, N.; Serrano, C.; van den Brink, H.; Pineau, J.; Prognon, P.; Borget, I.; El Batti, S. Advantages and Disadvantages of 3-Dimensional Printing in Surgery: A Systematic Review. Surgery 2016, 159, 1485–1500. [Google Scholar] [CrossRef]
- Huppertz, A.; Radmer, S.; Asbach, P.; Juran, R.; Schwenke, C.; Diederichs, G.; Hamm, B.; Sparmann, M. Computed Tomography for Preoperative Planning in Minimal-Invasive Total Hip Arthroplasty: Radiation Exposure and Cost Analysis. Eur. J. Radiol. 2011, 78, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Alexander, C.; Loeb, A.E.; Fotouhi, J.; Navab, N.; Armand, M.; Khanuja, H.S. Augmented Reality for Acetabular Component Placement in Direct Anterior Total Hip Arthroplasty. J. Arthroplast. 2020, 35, 1636–1641. [Google Scholar] [CrossRef] [PubMed]
- Logishetty, K.; Western, L.; Morgan, R.; Iranpour, F.; Cobb, J.P.; Auvinet, E. Can an Augmented Reality Headset Improve Accuracy of Acetabular Cup Orientation in Simulated THA? A Randomized Trial. Clin. Orthop. 2019, 477, 1190–1199. [Google Scholar] [CrossRef] [PubMed]
- Tanzer, M.; Laverdière, C.; Barimani, B.; Hart, A. Augmented Reality in Arthroplasty: An Overview of Clinical Applications, Benefits, and Limitations. J. Am. Acad. Orthop. Surg. 2022, 30, e760–e768. [Google Scholar] [CrossRef]
- Holzer, L.A.; Scholler, G.; Wagner, S.; Friesenbichler, J.; Maurer-Ertl, W.; Leithner, A. The Accuracy of Digital Templating in Uncemented Total Hip Arthroplasty. Arch. Orthop. Trauma Surg. 2019, 139, 263–268. [Google Scholar] [CrossRef] [Green Version]
- Heep, H.; Xu, J.; Löchteken, C.; Wedemeyer, C. A Simple and Convenient Method Guide to Determine the Magnification of Digital X-Rays for Preoperative Planning in Total Hip Arthroplasty. Orthop. Rev. 2012, 4, e12. [Google Scholar] [CrossRef] [Green Version]
- Shaarani, S.R.; McHugh, G.; Collins, D.A. Accuracy of Digital Preoperative Templating in 100 Consecutive Uncemented Total Hip Arthroplasties: A Single Surgeon Series. J. Arthroplast. 2013, 28, 331–337. [Google Scholar] [CrossRef]
- Archibeck, M.J.; Cummins, T.; Tripuraneni, K.R.; Carothers, J.T.; Murray-Krezan, C.; Hattab, M.; White, R.E. Inaccuracies in the Use of Magnification Markers in Digital Hip Radiographs. Clin. Orthop. 2016, 474, 1812–1817. [Google Scholar] [CrossRef] [Green Version]

| Age (mean ± SD) | 72.3 ± 11.9 |
| Female | 15 |
| Male | 12 |
| BMI (WHO classification in kg/m2) | |
| underweight (<18.5) | 1 |
| normal weight (18.5–24.9) | 5 |
| overweight (≥25.0) | 11 |
| obese (≥30.0) | 10 |
| Paprosky classification of acetabular bone loss | |
| Paprosky type 2A | 6 |
| Paprosky type 2B | 11 |
| Paprosky type 2C | 5 |
| Paprosky type 3A | 2 |
| Paprosky type 3B | 3 |
| 2D Templating | Total | ||||||
|---|---|---|---|---|---|---|---|
| 44 mm | 50 mm | 56 mm | 62 mm | ||||
| Intraoperative size | 50 mm | 1 | 4 | 0 | 0 | 5 | |
| 56 mm | 0 | 4 | 9 | 3 | 16 | ||
| 62 mm | 0 | 1 | 3 | 2 | 6 | ||
| Total | 1 | 9 | 12 | 5 | 27 | ||
| 3D Templating | Total | |||||
|---|---|---|---|---|---|---|
| 50 mm | 56 mm | 62 mm | ||||
| Intraoperative size | 50 mm | 5 | 0 | 0 | 5 | |
| 56 mm | 1 | 15 | 0 | 16 | ||
| 62 mm | 0 | 0 | 6 | 6 | ||
| Total | 6 | 15 | 6 | 27 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Winter, P.; Fritsch, E.; König, J.; Wolf, M.; Landgraeber, S.; Orth, P. Comparison of the Accuracy of 2D and 3D Templating for Revision Total Hip Replacement. J. Pers. Med. 2023, 13, 510. https://doi.org/10.3390/jpm13030510
Winter P, Fritsch E, König J, Wolf M, Landgraeber S, Orth P. Comparison of the Accuracy of 2D and 3D Templating for Revision Total Hip Replacement. Journal of Personalized Medicine. 2023; 13(3):510. https://doi.org/10.3390/jpm13030510
Chicago/Turabian StyleWinter, Philipp, Ekkehard Fritsch, Jochem König, Milan Wolf, Stefan Landgraeber, and Patrick Orth. 2023. "Comparison of the Accuracy of 2D and 3D Templating for Revision Total Hip Replacement" Journal of Personalized Medicine 13, no. 3: 510. https://doi.org/10.3390/jpm13030510
APA StyleWinter, P., Fritsch, E., König, J., Wolf, M., Landgraeber, S., & Orth, P. (2023). Comparison of the Accuracy of 2D and 3D Templating for Revision Total Hip Replacement. Journal of Personalized Medicine, 13(3), 510. https://doi.org/10.3390/jpm13030510






