Biomechanical Comparison of Conventional Plate and the C-Nail® System for the Treatment of Displaced Intra-Articular Calcaneal Fractures: A Finite Element Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Geometry Reconstruction
- from the midpoint of the anterior facet to the medial calcaneal tuberosity;
- a vertical cut near the angle of Gissane extending from the lateral cortex to the first cut;
- a vertical cut separating the posterior tuberosity from the posterior facet.
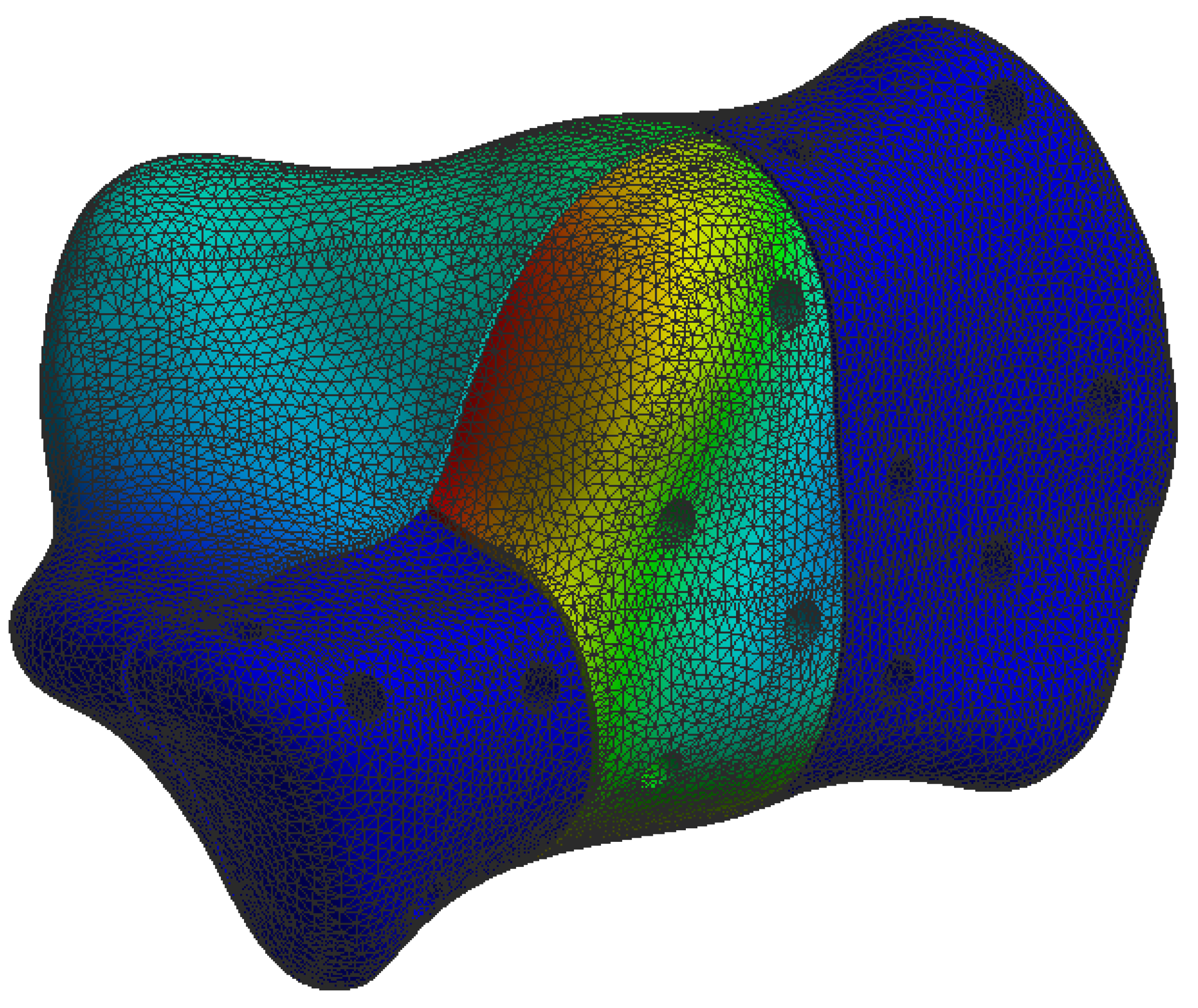
2.2. Material Properties and Mesh Creation
2.3. Boundary and Loading Conditions
3. Results
3.1. Stresses on Calcaneal C-Nail® Implant
3.2. Stresses on Calcaneal Plate Implant
3.3. Stresses on Calcaneal Bone
3.4. Displacement on Calcaneal Bone
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Cianni, L.; Vitiello, R.; Greco, T.; Sirgiovanni, M.; Ragonesi, G.; Maccauro, G.; Perisano, C. Predictive Factors of Poor Outcome in Sanders Type III and IV Calcaneal Fractures Treated with an Open Reduction and Internal Fixation with Plate: A Medium-Term Follow-Up. J. Clin. Med. 2022, 11, 5660. [Google Scholar] [CrossRef]
- Coughlin, M.; Saltzman, C.; Anderson, R. Mann’s Surgery of the Foot and Ankle, 9th ed.; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Volpin, G.; Cohen, Z.; Kirshner, G.; Shtarker, H. Displaced intra-articular calcaneal fractures: Current concepts and modern management. J. Foot Ankle Surg. 2014, 1, 24–31. [Google Scholar] [CrossRef]
- Wei, N.; Yuwen, P.; Liu, W.; Zhu, Y.; Chang, W.; Feng, C.; Chen, W. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: A meta-analysis of current evidence base. Medicine 2017, 96, e9027. [Google Scholar] [CrossRef] [PubMed]
- Rammelt, S.; Sangeorzan, B.J.; Swords, M.P. Calcaneal Fractures—Should We or Should We not Operate? Indian J. Orthop. 2018, 52, 220–230. [Google Scholar] [CrossRef]
- Rammelt, S.; Zwipp, H. Fractures of the calcaneus: Current treatment strategies. Acta Chir. Orthop. Traumatol. Cech. 2014, 81, 177–196. [Google Scholar] [PubMed]
- Razik, A.; Harris, M.; Trompeter, A. Calcaneal fractures: Where are we now? Strat. Traum Limb Recon 2018, 13, 1–11. [Google Scholar] [CrossRef]
- Luo, X.; Li, Q.; He, S.; He, S. Operative Versus Nonoperative Treatment for Displaced Intra-Articular Calcaneal Fractures: A Meta-Analysis of Randomized Controlled Trials. J. Foot Ankle Surg. 2016, 55, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Backes, M.; Schepers, T.; Beerekamp, M.S.H.; Luitse, J.S.; Goslings, J.C.; Schep, N.W. Wound infections following open reduction and internal fixation of calcaneal fractures with an extended lateral approach. Int. Orthop. 2014, 38, 767–773. [Google Scholar] [CrossRef]
- Schepers, T.; Den Hartog, D.; Vogels, L.M.; Van Lieshout, E.M. Extended lateral approach for intra-articular calcaneal fractures: An inverse relationship between surgeon experience and wound complications. J. Foot Ankle Surg. 2013, 52, 167–171. [Google Scholar] [CrossRef]
- Caravelli, S.; Gardini, G.; Pungetti, C.; Gentile, P.; Perisano, C.; Greco, T.; Rinaldi, V.G.; Marcheggiani Muccioli, G.M.; Tigani, D.; Mosca, M. Intra-Articular Calcaneal Fractures: Comparison between Mini-Invasive Approach and Kirschner Wires vs. Extensive Approach and Dedicated Plate—A Retrospective Evaluation at Long-Term Follow-Up. J. Clin. Med. 2023, 12, 20. [Google Scholar] [CrossRef]
- Wu, J.; Zhou, F.; Yang, L.; Tan, J. Percutaneous reduction and fixation with Kirschner wires versus open reduction internal fixation for the management of calcaneal fractures: A meta-analysis. Sci. Rep. 2016, 6, 30480. [Google Scholar] [CrossRef] [PubMed]
- Tantavisut, S.; Phisitkul, P.; Westerlind, B.O.; Gao, Y.; Karam, M.D.; Marsh, J.L. Percutaneous Reduction and Screw Fixation of Displaced Intra-articular Fractures of the Calcaneus. Foot Ankle Int. 2017, 38, 367–374. [Google Scholar] [CrossRef]
- Pan, M.; Chai, L.; Xue, F.; Ding, L.; Tang, G.; Lv, B. Comparisons of external fixator combined with limited internal fixation and open reduction and internal fixation for Sanders type 2 calcaneal fractures: Finite element analysis and clinical outcome. Bone Jt. Res. 2017, 6, 433–438. [Google Scholar] [CrossRef]
- Yeo, J.H.; Cho, H.J.; Lee, K.B. Comparison of two surgical approaches for displaced intra-articular calcaneal fractures: Sinus tarsi versus extensile lateral approach. BMC Musculoskelet Disord. 2015, 16, 63. [Google Scholar] [CrossRef] [PubMed]
- Park, C.H.; Lee, D.Y. Surgical treatment of Sanders type 2 calcaneal fractures using a sinus tarsi approach. Indian J. Orthop. 2017, 51, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Pastides, P.S.; Milnes, L.; Rosenfeld, P.F. Percutaneous arthroscopic calcaneal osteosynthesis: A minimally invasive technique for displaced intraarticular calcaneal fractures. J. Foot Ankle Surg. 2015, 54, 798–804. [Google Scholar] [CrossRef]
- Park, C.H.; Yoon, D.H. Role of subtalar arthroscopy in operative treatment of Sanders type 2 calcaneal fractures using a sinus tarsi approach. Foot Ankle Int. 2018, 39, 443–449. [Google Scholar] [CrossRef]
- Zwipp, H.; Paša, L.; Žilka, L.; Amlang, M.; Rammelt, S.; Pompach, M. Introduction of a New Locking Nail for Treatment of Intraarticular Calcaneal Fractures. J. Orthop. Trauma 2016, 30, e88–e92. [Google Scholar] [CrossRef]
- Goldzak, M.; Mittlmeier, T.; Simon, P. Locked nailing for the treatment of displaced articular fractures of the calcaneus: Description of a new procedure with calcanail. Eur. J. Orthop. Surg. Traumatol. 2012, 22, 345–349. [Google Scholar] [CrossRef]
- Bernasconi, A.; Iorio, P.; Ghani, Y.; Argyropoulos, M.; Patel, S.; Barg, A.; Smeraglia, F.; Balato, G.; Welck, M. Use of intramedullary locking nail for displaced intraarticular fractures of the calcaneus: What is the evidence? Arch. Orthop. Trauma Surg. 2022, 142, 1911–1922. [Google Scholar] [CrossRef]
- Blake, M.H.; Owen, J.R.; Sanford, T.S.; Wayne, J.S.; Adelaar, R.S. Biomechanical evaluation of a locking and nonlocking reconstruction plate in an osteoporotic calcaneal fracture model. Foot Ankle Int. 2011, 32, 432–436. [Google Scholar] [CrossRef] [PubMed]
- Allegra, P.R.; Rivera, S.; Desai, S.S.; Aiyer, A.; Kaplan, J.; Gross, C.E. Intra-articular calcaneus fractures: Current concepts review. Foot Ankle Orthop. 2020, 5, 2473011420927334. [Google Scholar] [CrossRef] [PubMed]
- Veliceasa, B.; Filip, A.; Pinzaru, R.; Pertea, M.; Ciuntu, B.; Alexa, O. Treatment of Displaced Intra-articular Calcaneal Fractures With an Interlocking Nail (C-Nail). J. Orthop. Trauma 2020, 34, e414–e419. [Google Scholar] [CrossRef] [PubMed]
- Fascione, F.; Di Mauro, M.; Guelfi, M.; Malagelada, F.; Pantalone, A.; Salini, V. Surgical treatment of displaced intraarticular calcaneal fractures by a minimally invasive technique using a locking nail: A preliminary study. Foot Ankle Surg. 2019, 25, 679–683. [Google Scholar] [CrossRef]
- Nosewicz, T.L.; Dingemans, S.A.; Backes, M.; Luitse, J.S.K.; Goslings, J.C.; Schepers, T. A systematic review and meta-analysis of the sinus tarsi and extended lateral approach in the operative treatment of displaced intra-articular calcaneal fractures. Foot Ankle Surg. 2019, 25, 580–588. [Google Scholar] [CrossRef]
- Pompach, M.; Carda, M.; Amlang, M.; Zwipp, H. Treatment of calcaneal fractures with a locking nail (C-Nail). Oper Orthop. Traumatol. 2016, 28, 218–230. [Google Scholar] [CrossRef]
- Sejda, F.; Frydrýšek, K.; Pleva, L.; Pompach, M.; Hlinka, J.; Sadílek, M.; Murčinková, Z.; Krpec, P.; Havlíček, M.; Madeja, R.; et al. Numerical Analysis of the Calcaneal Nail C-NAIL. Appl. Sci. 2022, 12, 5265. [Google Scholar] [CrossRef]
- Reinhardt, S.; Martin, H.; Ulmar, B.; Döbele, S.; Zwipp, H.; Rammelt, S.; Richter, M.; Pompach, M.; Mittlmeier, T. Interlocking Nailing Versus Interlocking Plating in Intra-articular Calcaneal Fractures: A Biomechanical Study. Foot Ankle Int. 2016, 37, 891–897. [Google Scholar] [CrossRef]
- Ni, M.; Wong, D.W.; Niu, W.; Wang, Y.; Mei, J.; Zhang, M. Biomechanical comparison of modified Calcanail system with plating fixation in intra-articular calcaneal fracture: A finite element analysis. Med. Eng. Phys. 2019, 70, 55–61. [Google Scholar] [CrossRef]
- Yu, B.; Chen, W.C.; Lee, P.Y.; Lin, K.P.; Lin, K.J.; Tsai, C.L.; Wei, H.W. Biomechanical comparison of conventional and anatomical calcaneal plates for the treatment of intraarticular calcaneal fractures—A finite element study. Comput. Methods Biomech. Biomed. Eng. 2016, 19, 1363–1370. [Google Scholar] [CrossRef]
- Ouyang, H.; Deng, Y.; Xie, P.; Yang, Y.; Jiang, B.; Zeng, C.; Huang, W. Biomechanical comparison of conventional and optimized locking plates for the fixation of intraarticular calcaneal fractures: A finite element analysis. Comput. Methods Biomech. Biomed. Eng. 2017, 20, 1339–1349. [Google Scholar] [CrossRef] [PubMed]














| Material | Young’s Modulus (MPa) 1 | Poisson’s Ratio 2 |
|---|---|---|
| Calcaneal bone | 1.89 | |
| Steel (implants) | 2 |
| Max von Mises Stress (MPa) | Max Displacement (mm) | |
|---|---|---|
| C-Nail® System | ||
| Single-standing stance (700 N) | 110 | |
| Full-standing stance (350 N) | 56 | |
| Calcaneal Plate | ||
| Single-standing stance (700 N) | 360 | |
| Full-standing stance (350 N) | 185 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pînzaru, R.M.; Pavăl, S.D.; Perțea, M.; Alexa, O.; Sîrbu, P.D.; Filip, A.; Carp, A.C.; Savin, L.; Forna, N.; Veliceasa, B. Biomechanical Comparison of Conventional Plate and the C-Nail® System for the Treatment of Displaced Intra-Articular Calcaneal Fractures: A Finite Element Analysis. J. Pers. Med. 2023, 13, 587. https://doi.org/10.3390/jpm13040587
Pînzaru RM, Pavăl SD, Perțea M, Alexa O, Sîrbu PD, Filip A, Carp AC, Savin L, Forna N, Veliceasa B. Biomechanical Comparison of Conventional Plate and the C-Nail® System for the Treatment of Displaced Intra-Articular Calcaneal Fractures: A Finite Element Analysis. Journal of Personalized Medicine. 2023; 13(4):587. https://doi.org/10.3390/jpm13040587
Chicago/Turabian StylePînzaru, Roxana Maria, Silviu Dumitru Pavăl, Mihaela Perțea, Ovidiu Alexa, Paul Dan Sîrbu, Alexandru Filip, Adrian Claudiu Carp, Liliana Savin, Norin Forna, and Bogdan Veliceasa. 2023. "Biomechanical Comparison of Conventional Plate and the C-Nail® System for the Treatment of Displaced Intra-Articular Calcaneal Fractures: A Finite Element Analysis" Journal of Personalized Medicine 13, no. 4: 587. https://doi.org/10.3390/jpm13040587
APA StylePînzaru, R. M., Pavăl, S. D., Perțea, M., Alexa, O., Sîrbu, P. D., Filip, A., Carp, A. C., Savin, L., Forna, N., & Veliceasa, B. (2023). Biomechanical Comparison of Conventional Plate and the C-Nail® System for the Treatment of Displaced Intra-Articular Calcaneal Fractures: A Finite Element Analysis. Journal of Personalized Medicine, 13(4), 587. https://doi.org/10.3390/jpm13040587







