Clinical Application of Personalized Digital Surgical Planning and Precise Execution for Severe and Complex Adult Spinal Deformity Correction Utilizing 3D Printing Techniques
Abstract
1. Introduction
2. Materials and Methods
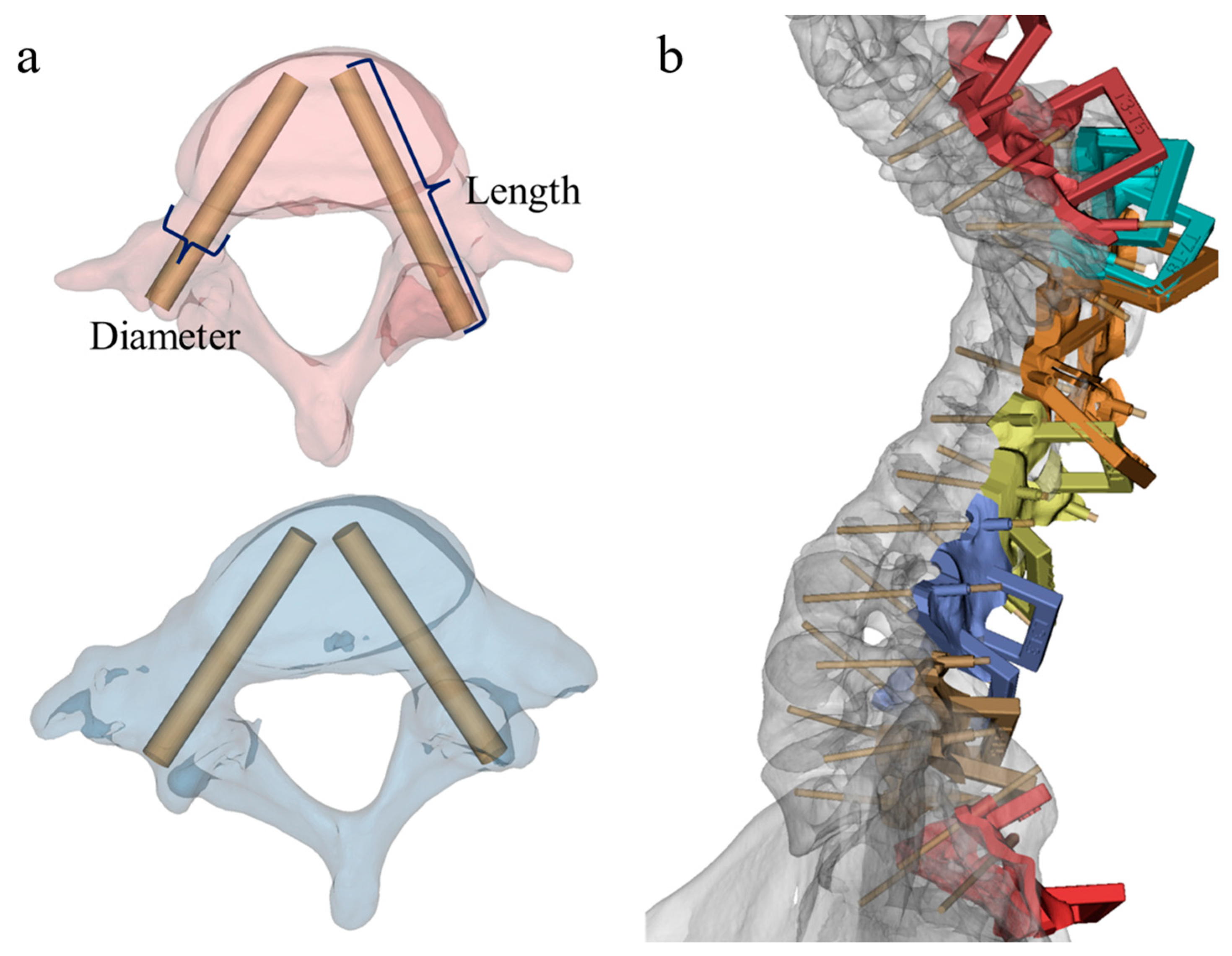
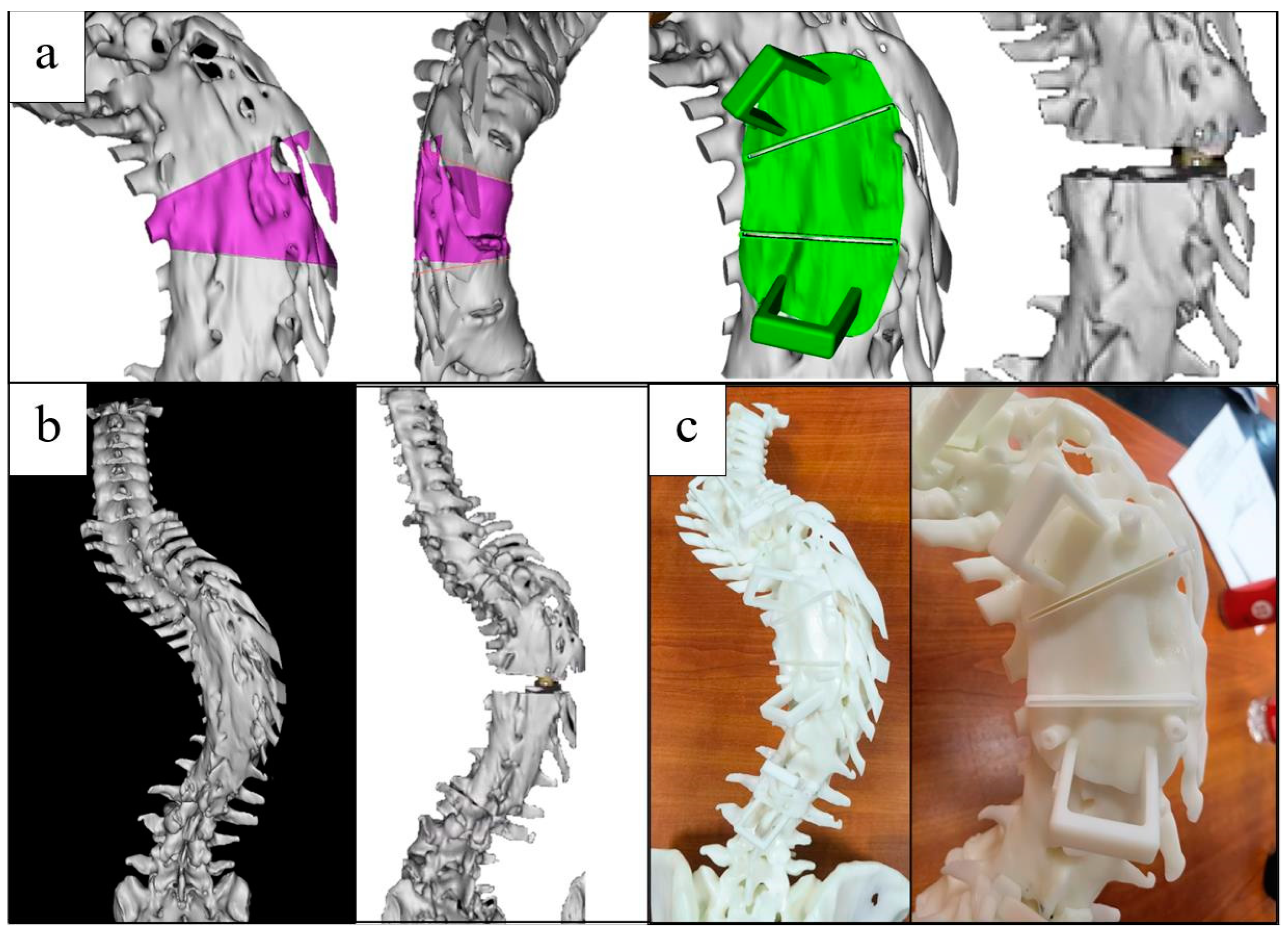
2.1. Construction of Pedicle Screw Insertion Guide Template
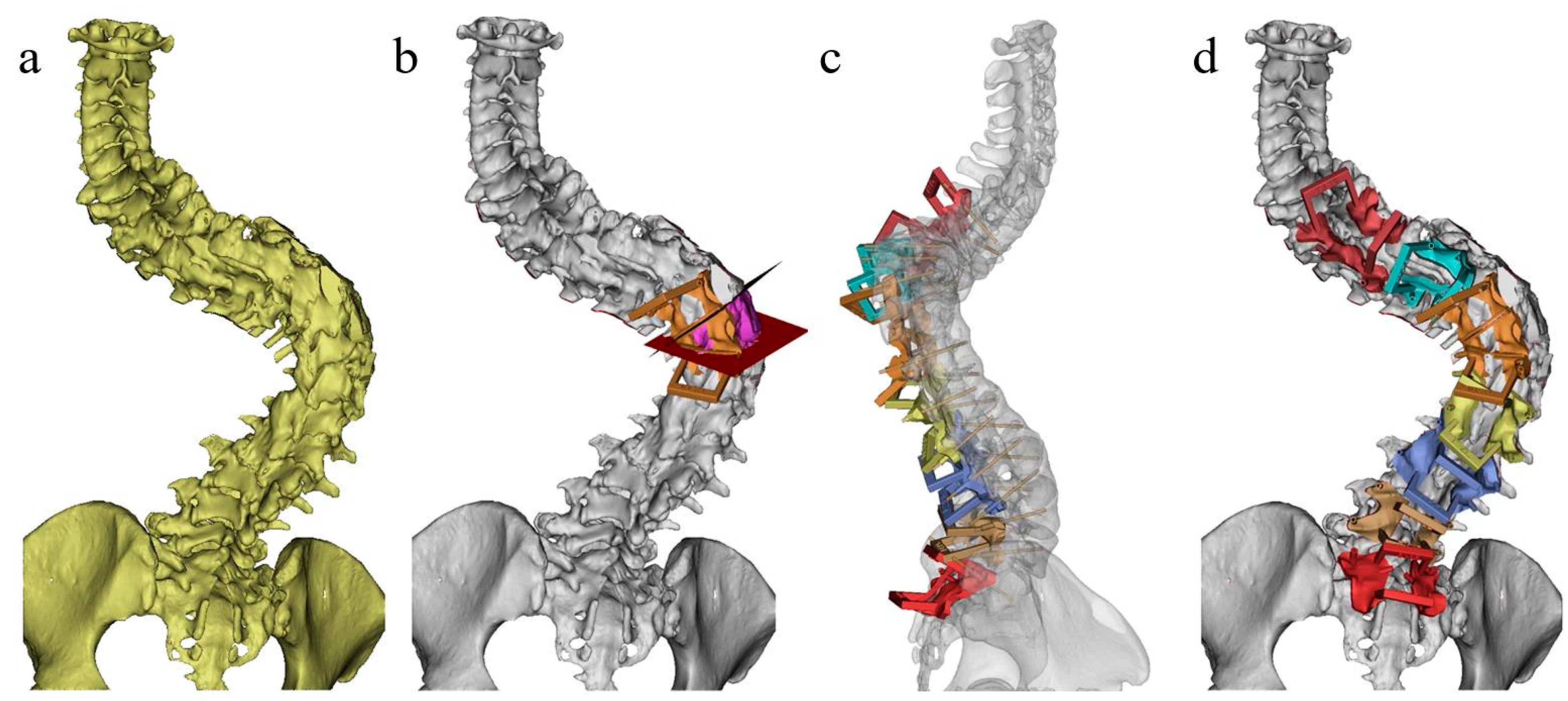
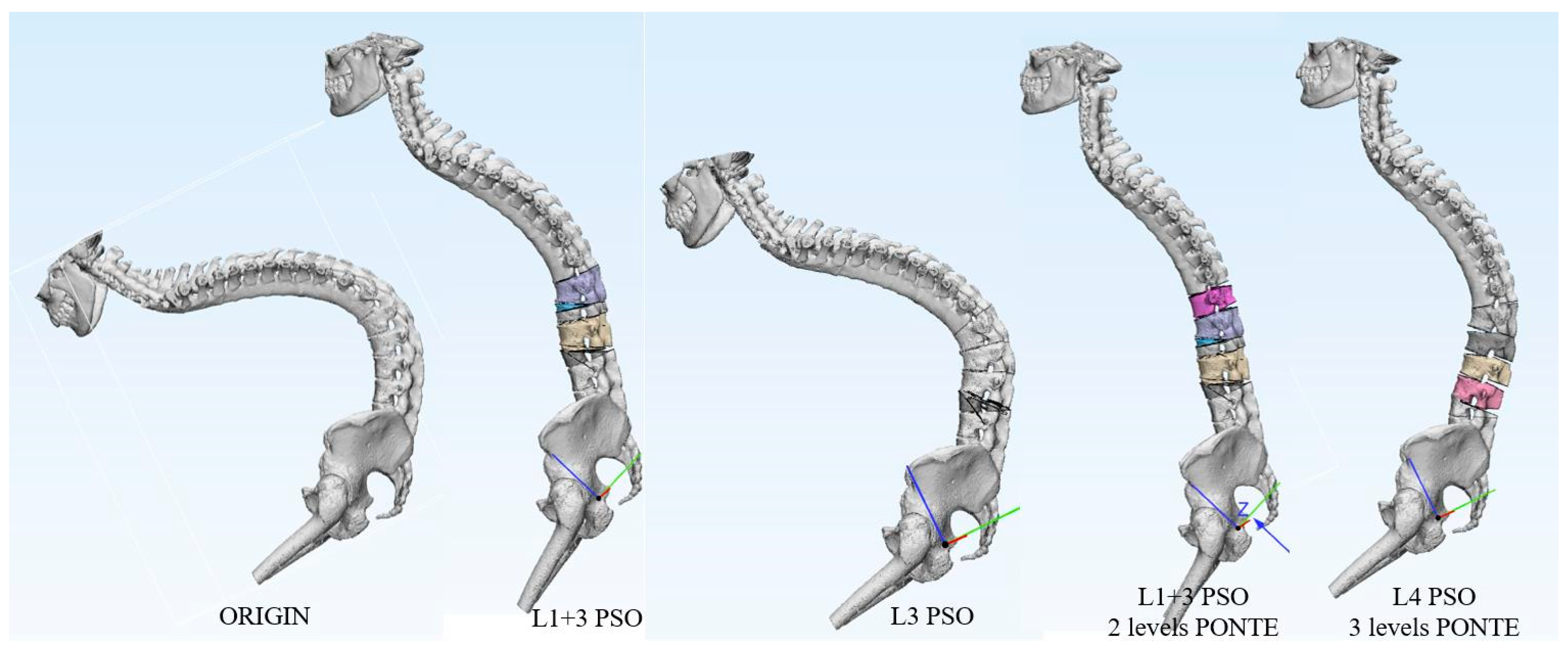
2.2. Construction of Osteotomy Guide Template
2.3. Model and Template Printing
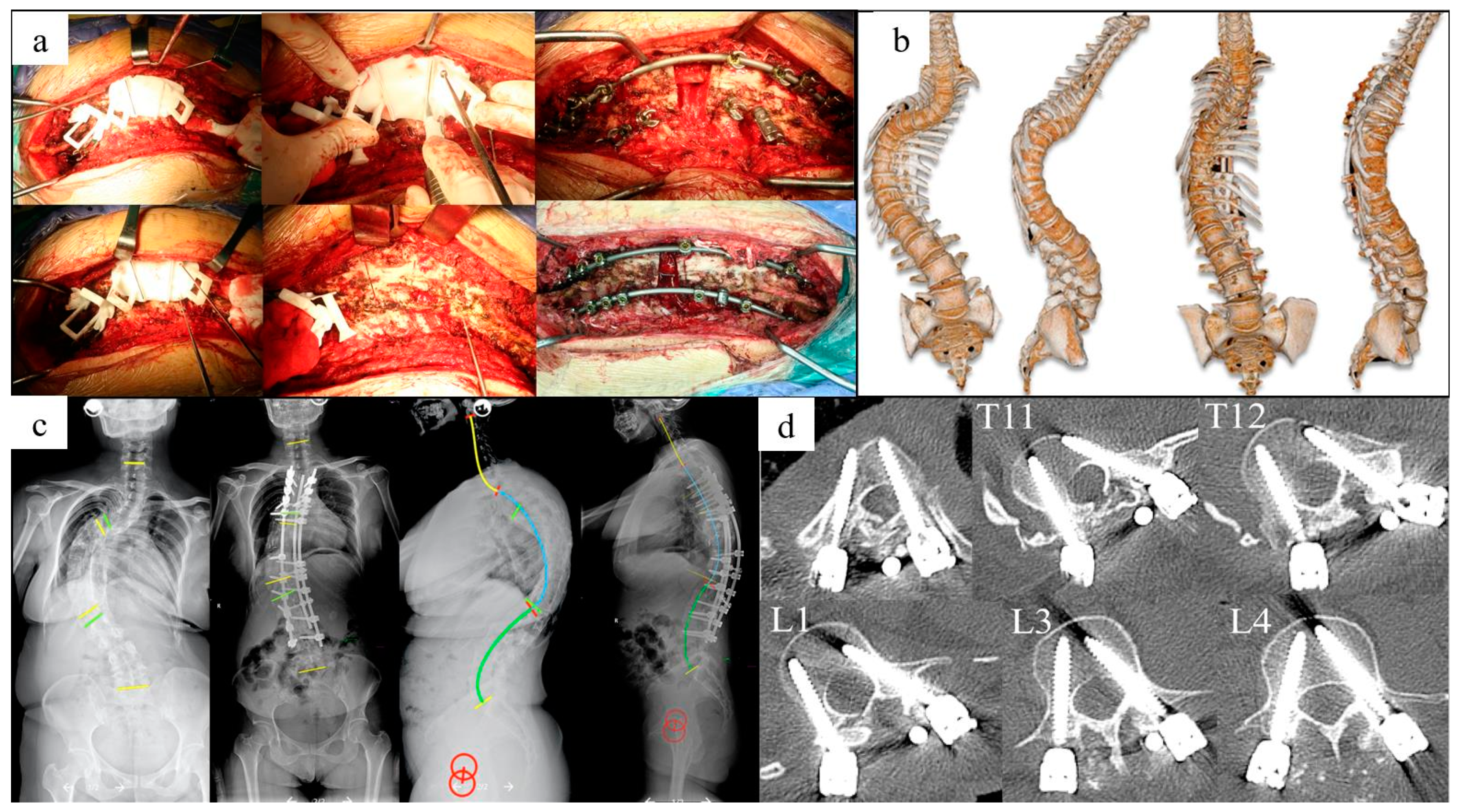
2.4. Surgical Procedure
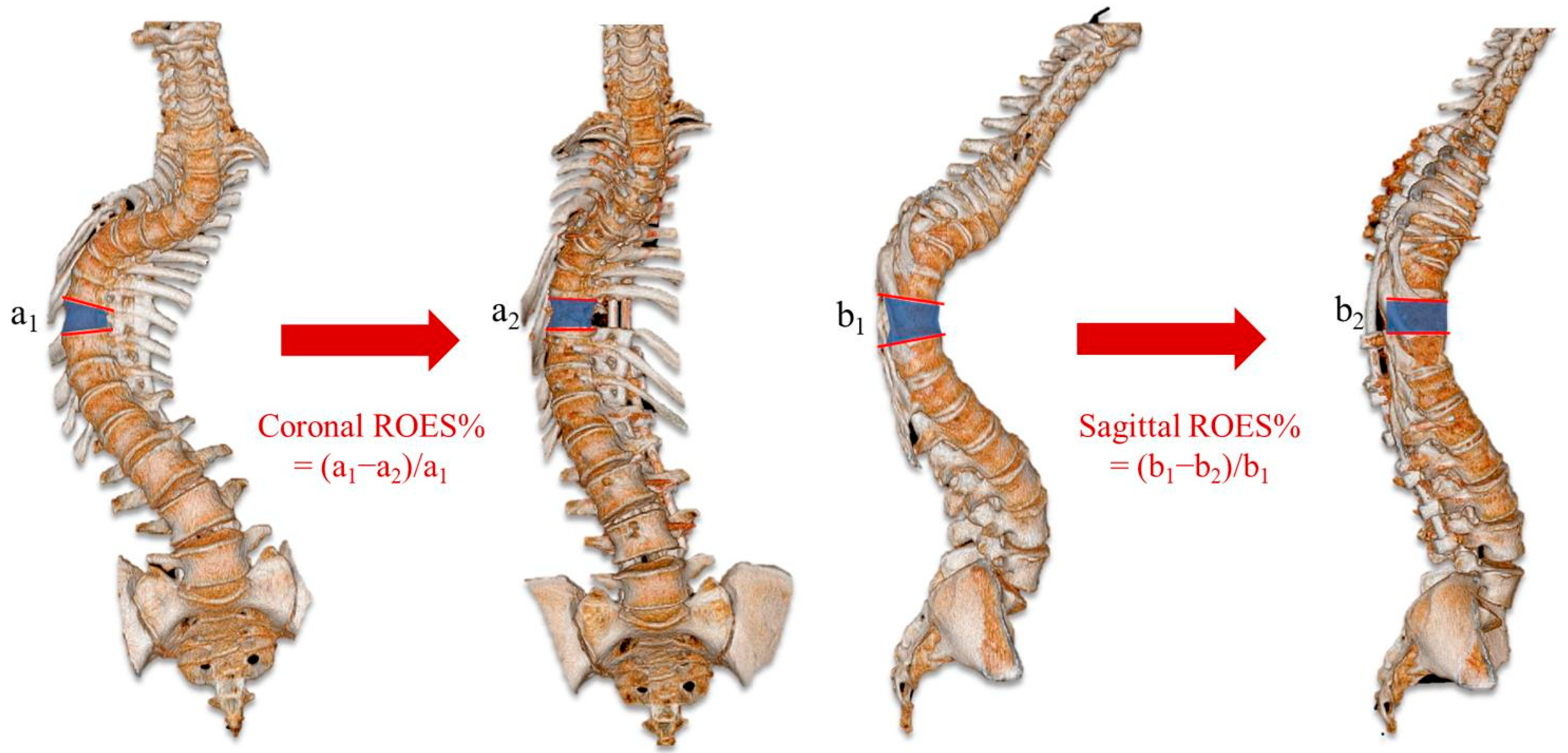
2.5. Data Collection
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lenke, L.G.; O’Leary, P.T.; Bridwell, K.H.; Sides, B.A.; Koester, L.A.; Blanke, K.M. Posterior vertebral column resection for severe pediatric deformity: Minimum two-year follow-up of thirty-five consecutive patients. Spine Phila Pa 1976 2009, 34, 2213–2221. [Google Scholar] [CrossRef]
- Kelly, M.P.; Lenke, L.G.; Shaffrey, C.I.; Ames, C.P.; Carreon, L.Y.; Lafage, V.; Smith, J.S.; Shimer, A.L. Evaluation of complications and neurological deficits with three-column spine reconstructions for complex spinal deformity: A retrospective Scoli-RISK-1 study. Neurosurg. Focus 2014, 36, E17. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.L.; Huang, Z.F.; Yin, J.Q.; Deng, Y.L.; Xie, X.B.; Li, F.B.; Yang, J.F. A proposed classification system for guiding surgical strategy in cases of severe spinal deformity based on spinal cord function. Eur. Spine J. 2016, 25, 1821–1829. [Google Scholar] [CrossRef] [PubMed]
- Fehlings, M.G.; Kato, S.; Lenke, L.G.; Nakashima, H.; Nagoshi, N.; Shaffrey, C.I.; Cheung, K.M.C.; Carreon, L.; Dekutoski, M.B.; Schwab, F.J.; et al. Incidence and risk factors of postoperative neurologic decline after complex adult spinal deformity surgery: Results of the Scoli-RISK-1 study. Spine J. Off. J. N. Am. Spine Soc. 2018, 18, 1733–1740. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.B.; Lenke, L.G.; Thuet, E.; Blanke, K.; Koester, L.A.; Roth, M. Deformity Angular Ratio Describes the Severity of Spinal Deformity and Predicts the Risk of Neurologic Deficit in Posterior Vertebral Column Resection Surgery. Spine Phila Pa 1976 2016, 41, 1447–1455. [Google Scholar] [CrossRef]
- Chen, J.; Shao, X.X.; Sui, W.Y.; Yang, J.F.; Deng, Y.L.; Xu, J.; Huang, Z.F.; Yang, J.L. Risk factors for neurological complications in severe and rigid spinal deformity correction of 177 cases. BMC Neurol. 2020, 20, 433. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hai, Y.; Liu, Y.; Zhang, X.; Zhang, Y.; Han, C.; Liu, J.; Zhou, L. The Reliability of Computer-Assisted Three-Dimensional Surgical Simulation of Posterior Osteotomies in Thoracolumbar Kyphosis Secondary to Ankylosing Spondylitis Patients. Mediat. Inflamm. 2022, 2022, 8134242. [Google Scholar] [CrossRef]
- Yang, M.; Li, C.; Li, Y.; Zhao, Y.; Wei, X.; Zhang, G.; Fan, J.; Ni, H.; Chen, Z.; Bai, Y.; et al. Application of 3D rapid prototyping technology in posterior corrective surgery for Lenke 1 adolescent idiopathic scoliosis patients. Medicine 2015, 94, e582. [Google Scholar] [CrossRef]
- Sheha, E.D.; Gandhi, S.D.; Colman, M.W. 3D printing in spine surgery. Ann. Transl. Med. 2019, 7, S164. [Google Scholar] [CrossRef]
- Zamborsky, R.; Kilian, M.; Jacko, P.; Bernadic, M.; Hudak, R. Perspectives of 3D printing technology in orthopaedic surgery. Bratisl. Lek. Listy 2019, 120, 498–504. [Google Scholar] [CrossRef]
- Izatt, M.T.; Thorpe, P.L.; Thompson, R.G.; D’Urso, P.S.; Adam, C.J.; Earwaker, J.W.; Labrom, R.D.; Askin, G.N. The use of physical biomodelling in complex spinal surgery. Eur. Spine J. 2007, 16, 1507–1518. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Wang, W.; Yang, N.; Xia, L. Does Three-dimensional Printing Plus Pedicle Guider Technology in Severe Congenital Scoliosis Facilitate Accurate and Efficient Pedicle Screw Placement? Clin. Orthop. Relat. Res. 2019, 477, 1904–1912. [Google Scholar] [CrossRef]
- Pan, A.; Ding, H.; Hai, Y.; Liu, Y.; Hai, J.J.; Yin, P.; Han, B. The Value of Three-Dimensional Printing Spine Model in Severe Spine Deformity Correction Surgery. Glob. Spine J. 2023, 13, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Garg, B.; Gupta, M.; Singh, M.; Kalyanasundaram, D. Outcome and safety analysis of 3D-printed patient-specific pedicle screw jigs for complex spinal deformities: A comparative study. Spine J. Off. J. N. Am. Spine Soc. 2019, 19, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Xin, X.; Wang, F.; Liu, X. A 3D-Printed Personalized, Combined, Modular Pedicle Subtraction Osteotomy Guide Plate System: An Experimental Study. Spine Phila Pa 1976 2021, 47, 931–937. [Google Scholar] [CrossRef]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of pedicular screw placement in vivo. Spine Phila Pa 1976 1990, 15, 11–14. [Google Scholar] [CrossRef]
- Raynor, B.L.; Bright, J.D.; Lenke, L.G.; Rahman, R.K.; Bridwell, K.H.; Riew, K.D.; Buchowski, J.M.; Luhmann, S.J.; Padberg, A.M. Significant change or loss of intraoperative monitoring data: A 25-year experience in 12,375 spinal surgeries. Spine Phila Pa 1976 2013, 38, E101–E108. [Google Scholar] [CrossRef]
- Coe, J.D.; Arlet, V.; Donaldson, W.; Berven, S.; Hanson, D.S.; Mudiyam, R.; Perra, J.H.; Shaffrey, C.I. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine Phila Pa 1976 2006, 31, 345–349. [Google Scholar] [CrossRef]
- Kim, S.S.; Cho, B.C.; Kim, J.H.; Lim, D.J.; Park, J.Y.; Lee, B.J.; Suk, S.I. Complications of posterior vertebral resection for spinal deformity. Asian Spine J. 2012, 6, 257–265. [Google Scholar] [CrossRef]
- Lenke, L.G.; Newton, P.O.; Sucato, D.J.; Shufflebarger, H.L.; Emans, J.B.; Sponseller, P.D.; Shah, S.A.; Sides, B.A.; Blanke, K.M. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: A multicenter analysis. Spine Phila Pa 1976 2013, 38, 119–132. [Google Scholar] [CrossRef]
- Bundoc, R.C.; Delgado, G.G.; Grozman, S.A. A Novel Patient-Specific Drill Guide Template for Pedicle Screw Insertion into the Subaxial Cervical Spine Utilizing Stereolithographic Modelling: An In Vitro Study. Asian Spine J. 2017, 11, 4–14. [Google Scholar] [CrossRef]
- Lopez, C.D.; Boddapati, V.; Lee, N.J.; Dyrszka, M.D.; Sardar, Z.M.; Lehman, R.A.; Lenke, L.G. Three-Dimensional Printing for Preoperative Planning and Pedicle Screw Placement in Adult Spinal Deformity: A Systematic Review. Glob. Spine J. 2021, 11, 936–949. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Guo, K.; Yang, H.; Wu, D.; Yuan, F. Thoracic Pedicle Screw Placement Guide Plate Produced by Three-Dimensional (3-D) Laser Printing. Med. Sci. Monit. 2016, 22, 1682–1686. [Google Scholar] [CrossRef]
- Takemoto, M.; Fujibayashi, S.; Ota, E.; Otsuki, B.; Kimura, H.; Sakamoto, T.; Kawai, T.; Futami, T.; Sasaki, K.; Matsushita, T.; et al. Additive-manufactured patient-specific titanium templates for thoracic pedicle screw placement: Novel design with reduced contact area. Eur. Spine J. 2016, 25, 1698–1705. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, Q.; Li, X.; Zhao, C.; Quan, X.; Zhao, R.; Chen, Z.; Li, Y. Preliminary application of a multi-level 3D printing drill guide template for pedicle screw placement in severe and rigid scoliosis. Eur. Spine J. 2017, 26, 1684–1689. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, T.; Higashiyama, N.; Kaneyama, S.; Takabatake, M.; Watanabe, N.; Uchida, F.; Sumi, M.; Mizoi, K. Multistep pedicle screw insertion procedure with patient-specific lamina fit-and-lock templates for the thoracic spine: Clinical article. J. Neurosurg. Spine 2013, 19, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Pijpker, P.A.J.; Kuijlen, J.M.A.; Kraeima, J.; Faber, C. Three-Dimensional Planning and Use of Individualized Osteotomy-Guiding Templates for Surgical Correction of Kyphoscoliosis: A Technical Case Report. World Neurosurg. 2018, 119, 113–117. [Google Scholar] [CrossRef]
- Tu, Q.; Ding, H.W.; Chen, H.; Miao, Q.J.; Yang, X.; Li, K.; Zhang, K.; Wu, Z.H.; Tang, Y.; Xia, H.; et al. Three-Dimensional-Printed Individualized Guiding Templates for Surgical Correction of Severe Kyphoscoliosis Secondary to Ankylosing Spondylitis: Outcomes of 9 Cases. World Neurosurg. 2019, 130, e961–e970. [Google Scholar] [CrossRef]
- Suk, S.I.; Kim, J.H.; Kim, W.J.; Lee, S.M.; Chung, E.R.; Nah, K.H. Posterior vertebral column resection for severe spinal deformities. Spine Phila Pa 1976 2002, 27, 2374–2382. [Google Scholar] [CrossRef]
- Xin, X.; Liu, X.; Zhu, Y.; Li, J.; Yue, C.; Hao, D. 3D-Printed Guide Plate System-Assisted Thoracolumbar Kyphosis Osteotomy: A Technical Case Series. World Neurosurg. 2023, 173, 28–33. [Google Scholar] [CrossRef]



| No. | Gender | Age (yrs.) | Diagnosis | Deformity Type | Instrumented Segments | Osteotomy Type | Osteotomy Position | Duration (min) | EBL (mL) | Blood Transfusion (mL) | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 39 | ADIS/revision | Kyphoscoliosis | T3-L4 | VCR | T10 | 400 | 700 | 480 | N |
| 2 | F | 33 | ADIS/revision | Kyphoscoliosis | T3-L4 | VCR | T10 | 420 | 800 | 800 | N |
| 3 | M | 43 | CS | Kyphoscoliosis | T10-L4 | PSO | L1 | 265 | 500 | 200 | N |
| 4 | M | 22 | CS | Kyphoscoliosis | T4-L4 | VCRs | T12/L1 | 455 | 1000 | 850 | N |
| 5 | M | 38 | TB | Kyphosis | T4-L2 | VCRs | T8/T9/T10 | 370 | 700 | 300 | N |
| 6 | F | 34 | CS | Scoliosis | T1-T12 | PSO | T5 | 380 | 1500 | 1300 | N |
| 7 | M | 33 | AS | Kyphosis | T8-L5 | PSOs | L1/L3 | 300 | 400 | 200 | N |
| 8 | F | 28 | CS | Kyphoscoliosis | T4-L5 | VCRs | T10/T11/T12 | 300 | 800 | 1575 | N |
| No. | Pre-Operation | Post-Operation | Designed Osteotomy Angle (°) | Achieved Osteotomy Angle (°) | Achieved Correction Angle (°) | ROES (%) | Pedicle Accuracy | Modified Macnab Criteria | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scoliosis (°) | Kyphosis (°) | Trunk Shift (mm) | SVA (mm) | Scoliosis (°) | Kyphosis (°) | Trunk Shift (mm) | SVA (mm) | Coronal | Sagittal | Coronal | Sagittal | Coronal | Sagittal | Coronal | Sagittal | |||
| 1 | 88 | 112 | 15 | 29 | 27 | 54 | 26 | 35 | 43 | 30 | 41 | 33 | 61 | 58 | 95.35 | 110.0 | 20/21 (95.24%) | Excellent |
| 2 | 118 | 96 | 36 | 22 | 60 | 34 | 14 | 5 | 48 | 25 | 45 | 23 | 58 | 62 | 93.75 | 92.0 | 21/23 (91.30%) | Excellent |
| 3 | 85 | 92 | 10 | 13 | 21 | 8 | 0 | 7 | 35 | 35 | 37 | 33 | 64 | 74 | 105.71 | 94.29 | 11/12 (91.67%) | Excellent |
| 4 | 107 | 118 | 19 | 59 | 31 | 45 | 7 | 34 | 60 | 45 | 57 | 47 | 76 | 73 | 95.0 | 104.44 | 20/22 (90.91%) | Good |
| 5 | - | 99 | 0 | 0 | - | 34 | 0 | 14 | - | 50 | - | 46 | - | 65 | - | 92.0 | 16/16 (100%) | Excellent |
| 6 | 87 | - | 32 | 2 | 30 | - | 3 | 2 | 35 | - | 36 | - | 57 | - | 102.86 | - | 17/19 (89.47%) | Excellent |
| 7 | - | 115 | - | 620 | - | 74 | - | 330 | - | 30 | - | 26 | - | 41 | - | 86.67 | 16/16 (100%) | Good |
| 8 | 111 | 138 | 16 | 35 | 36 | 45 | 28 | 23 | 57 | 55 | 55 | 51 | 75 | 93 | 96.49 | 92.73 | 18/21 (85.71%) | Excellent |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ding, H.; Hai, Y.; Zhou, L.; Liu, Y.; Zhang, Y.; Han, C.; Zhang, Y. Clinical Application of Personalized Digital Surgical Planning and Precise Execution for Severe and Complex Adult Spinal Deformity Correction Utilizing 3D Printing Techniques. J. Pers. Med. 2023, 13, 602. https://doi.org/10.3390/jpm13040602
Ding H, Hai Y, Zhou L, Liu Y, Zhang Y, Han C, Zhang Y. Clinical Application of Personalized Digital Surgical Planning and Precise Execution for Severe and Complex Adult Spinal Deformity Correction Utilizing 3D Printing Techniques. Journal of Personalized Medicine. 2023; 13(4):602. https://doi.org/10.3390/jpm13040602
Chicago/Turabian StyleDing, Hongtao, Yong Hai, Lijin Zhou, Yuzeng Liu, Yiqi Zhang, Chaofan Han, and Yangpu Zhang. 2023. "Clinical Application of Personalized Digital Surgical Planning and Precise Execution for Severe and Complex Adult Spinal Deformity Correction Utilizing 3D Printing Techniques" Journal of Personalized Medicine 13, no. 4: 602. https://doi.org/10.3390/jpm13040602
APA StyleDing, H., Hai, Y., Zhou, L., Liu, Y., Zhang, Y., Han, C., & Zhang, Y. (2023). Clinical Application of Personalized Digital Surgical Planning and Precise Execution for Severe and Complex Adult Spinal Deformity Correction Utilizing 3D Printing Techniques. Journal of Personalized Medicine, 13(4), 602. https://doi.org/10.3390/jpm13040602







