The Deep-MCL Line: A Reliable Anatomical Landmark to Optimize the Tibial Cut in UKA
Abstract
:1. Introduction
2. Materials and Methods
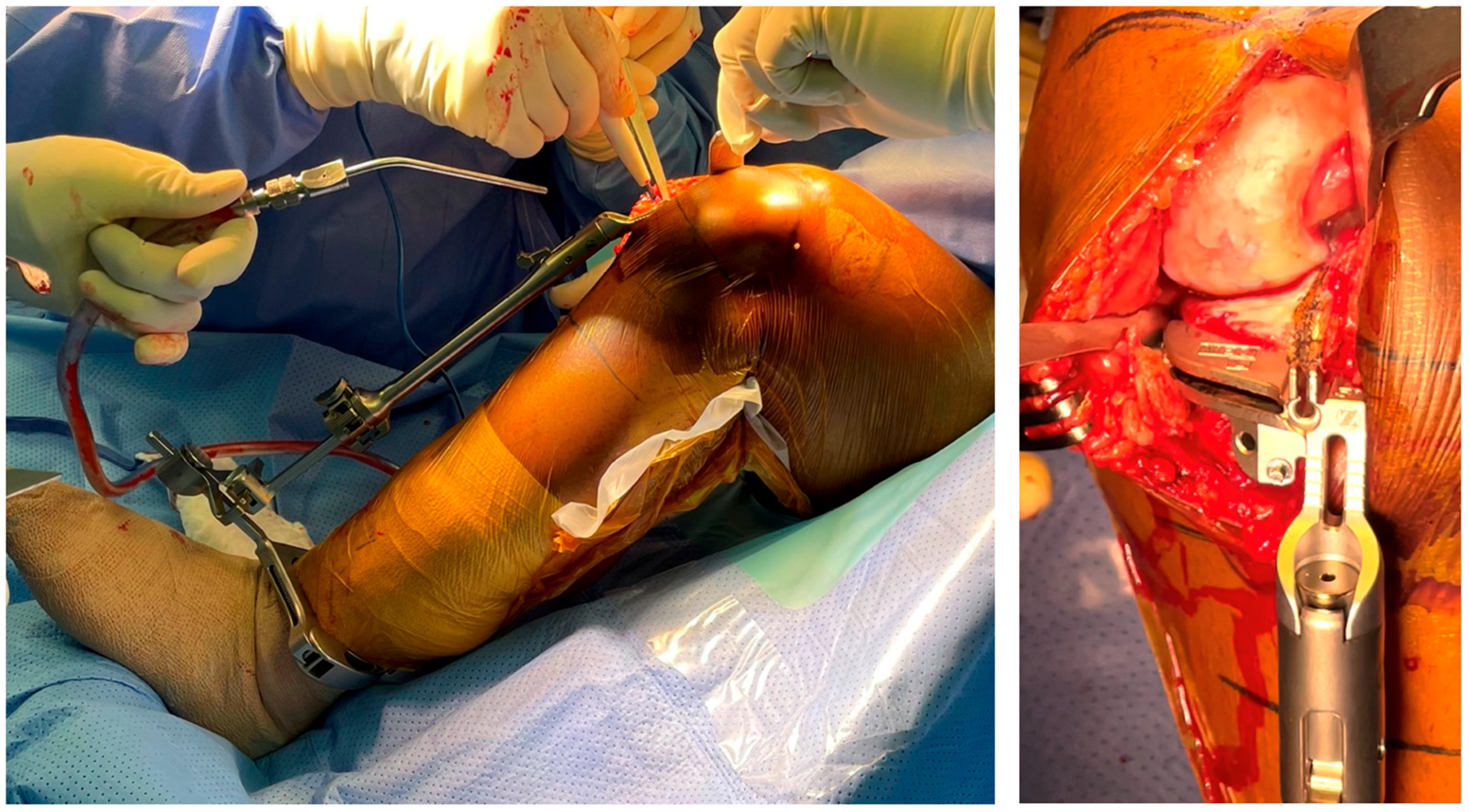
2.1. Surgical Technique
2.2. Patients
2.3. Data Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barbadoro, P.; Ensini, A.; Leardini, A.; d’Amato, M.; Feliciangeli, A.; Timoncini, A.; Amadei, F.; Belvedere, C.; Giannini, S. Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: A radiographic and radiostereometric study. Knee Surg. Sport. Traumatol. Arthrosc. 2014, 22, 3157–3162. [Google Scholar] [CrossRef]
- Epinette, J.A.; Brunschweiler, B.; Mertl, P.; Mole, D.; Cazenave, A.; The French Society for the Hip and Knee. Unicompartmental knee arthroplasty modes of failure: Wear is not the main reason for failure: A multicentre study of 418 failed knees. Orthop. Traumatol. Surg. Res. 2012, 98, S124–S130. [Google Scholar] [CrossRef]
- Ko, Y.B.; Gujarathi, M.R.; Oh, K.J. Outcome of Unicompartmental Knee Arthroplasty: A Systematic Review of Comparative Studies between Fixed and Mobile Bearings Focusing on Complications. Knee Surg. Relat. Res. 2015, 27, 141–148. [Google Scholar] [CrossRef]
- Bell, S.W.; Anthony, I.; Jones, B.; MacLean, A.; Rowe, P.; Blyth, M. Improved Accuracy of Component Positioning with Robotic-Assisted Unicompartmental Knee Arthroplasty: Data from a Prospective, Randomized Controlled Study. J. Bone Jt. Surg. Am. Vol. 2016, 98, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Ponzio, D.Y.; Lonner, J.H. Robotic Technology Produces More Conservative Tibial Resection Than Conventional Techniques in UKA. Am. J. Orthop. 2016, 45, E465–E468. [Google Scholar]
- Batailler, C.; White, N.; Ranaldi, F.M.; Neyret, P.; Servien, E.; Lustig, S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 27, 1232–1240. [Google Scholar] [CrossRef]
- Herry, Y.; Batailler, C.; Lording, T.; Servien, E.; Neyret, P.; Lustig, S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int. Orthop. 2017, 41, 2265–2271. [Google Scholar] [CrossRef]
- Thilak, J.; Thadi, M.; Mane, P.P.; Sharma, A.; Mohan, V.; Babu, B.C. Accuracy of tibial component positioning in the robotic arm assisted versus conventional unicompartmental knee arthroplasty. J. Orthop. 2020, 22, 367–371. [Google Scholar] [CrossRef]
- Gaudiani, M.A.; Nwachukwu, B.U.; Baviskar, J.V.; Sharma, M.; Ranawat, A.S. Optimization of sagittal and coronal planes with robotic-assisted unicompartmental knee arthroplasty. Knee 2017, 24, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Savov, P.; Tuecking, L.R.; Windhagen, H.; Calliess, T.; Ettinger, M. Robotics improves alignment accuracy and reduces early revision rates for UKA in the hands of low-volume UKA surgeons. Arch. Orthop. Trauma. Surg. 2021, 141, 2139–2146. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.G.; Clement, N.D.; Hamilton, D.; Blyth, M.J.G.; Haddad, F.S.; Patton, J.T. A systematic review of robotic-assisted unicompartmental knee arthroplasty: Prosthesis design and type should be reported. Bone Jt. J. 2019, 101, 838–847. [Google Scholar] [CrossRef]
- Kayani, B.; Haddad, F.S. Robotic unicompartmental knee arthroplasty: Current challenges and future perspectives. Bone Jt. Res. 2019, 8, 228–231. [Google Scholar] [CrossRef]
- Zambianchi, F.; Daffara, V.; Franceschi, G.; Banchelli, F.; Marcovigi, A.; Catani, F. Robotic arm-assisted unicompartmental knee arthroplasty: High survivorship and good patient-related outcomes at a minimum five years of follow-up. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 29, 3316–3322. [Google Scholar] [CrossRef] [PubMed]
- Gilmour, A.; MacLean, A.D.; Rowe, P.J.; Banger, M.S.; Donnelly, I.; Jones, B.G.; Blyth, M.J.G. Robotic-Arm-Assisted vs. Conventional Unicompartmental Knee Arthroplasty. The 2-Year Clinical Outcomes of a Randomized Controlled Trial. J. Arthroplast. 2018, 33, S109–S115. [Google Scholar] [CrossRef] [PubMed]
- Kawahara, S.; Matsuda, S.; Okazaki, K.; Tashiro, Y.; Iwamoto, Y. Is the medial wall of the intercondylar notch useful for tibial rotational reference in unicompartmental knee arthroplasty? Clin. Orthop. Relat. Res. 2012, 470, 1177–1184. [Google Scholar] [CrossRef]
- Lee, S.Y.; Chay, S.; Lim, H.C.; Bae, J.H. Tibial component rotation during the unicompartmental knee arthroplasty: Is the anterior superior iliac spine an appropriate landmark? Knee Surg. Sport. Traumatol. Arthrosc. 2017, 25, 3723–3732. [Google Scholar] [CrossRef]
- Makhdom, A.M.; Kerr, G.J.; Wu, E.; Lonner, J.H. Rotational alignment errors can occur in unicompartmental knee arthroplasty if anatomical landmarks are misused: A preoperative CT scan analysis. Knee 2020, 27, 242–248. [Google Scholar] [CrossRef]
- Parratte, S.; Sah, A.; Batailler, C. Safe and reliable clinical outcomes at 2 years of a fixed-bearing partial knee arthroplasty with a morphometric tibial tray in a large worldwide population. Knee Surg. Sport. Traumatol. Arthrosc. 2023, 31, 814–821. [Google Scholar] [CrossRef]
- National Joint Registry for England and Wales: 17th Annual Report. 2020. Available online: https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2017th%20Annual%20Report%202020.pdf (accessed on 14 May 2023).
- Weber, P.; Schroder, C.; Laubender, R.P.; Baur-Melnyk, A.; von Schulze Pellengahr, C.; Jansson, V.; Muller, P.E. Joint line reconstruction in medial unicompartmental knee arthroplasty: Development and validation of a measurement method. Knee Surg. Sport. Traumatol. Arthrosc. Off. J. ESSKA 2013, 21, 2468–2473. [Google Scholar] [CrossRef]
- Negrin, R.; Duboy, J.; Reyes, N.O.; Barahona, M.; Iniguez, M.; Infante, C.; Cordero, J.A.; Sepulveda, V.; Ferrer, G. Robotic-assisted Unicompartmental knee Arthroplasty optimizes joint line restitution better than conventional surgery. J. Exp. Orthop. 2020, 7, 94. [Google Scholar] [CrossRef] [PubMed]
- Regier, D.A.; Narrow, W.E.; Clarke, D.E.; Kraemer, H.C.; Kuramoto, S.J.; Kuhl, E.A.; Kupfer, D.J. DSM-5 field trials in the United States and Canada, Part II: Test-retest reliability of selected categorical diagnoses. Am. J. Psychiatry 2013, 170, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Riviere, C.; Sivaloganathan, S.; Villet, L.; Cartier, P.; Lustig, S.; Vendittoli, P.A.; Cobb, J. Kinematic alignment of medial UKA is safe: A systematic review. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 30, 1082–1094. [Google Scholar] [CrossRef] [PubMed]
- Walker, T.; Heinemann, P.; Bruckner, T.; Streit, M.R.; Kinkel, S.; Gotterbarm, T. The influence of different sets of surgical instrumentation in Oxford UKA on bearing size and component position. Arch. Orthop. Trauma. Surg. 2017, 137, 895–902. [Google Scholar] [CrossRef] [PubMed]
- Bonnin, M.; Chambat, P. Current status of valgus angle, tibial head closing wedge osteotomy in media gonarthrosis. Orthopade 2004, 33, 135–142. [Google Scholar] [CrossRef]
- Deschamps, G.; Chol, C. Fixed-bearing unicompartmental knee arthroplasty. Patients’ selection and operative technique. Orthop. Traumatol. Surg. Res. OTSR 2011, 97, 648–661. [Google Scholar] [CrossRef]
- Small, S.R.; Berend, M.E.; Rogge, R.D.; Archer, D.B.; Kingman, A.L.; Ritter, M.A. Tibial loading after UKA: Evaluation of tibial slope, resection depth, medial shift and component rotation. J. Arthroplast. 2013, 28, 179–183. [Google Scholar] [CrossRef]
- Kwon, O.R.; Kang, K.T.; Son, J.; Suh, D.S.; Baek, C.; Koh, Y.G. Importance of joint line preservation in unicompartmental knee arthroplasty: Finite element analysis. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2017, 35, 347–352. [Google Scholar] [CrossRef]
- Simpson, D.J.; Price, A.J.; Gulati, A.; Murray, D.W.; Gill, H.S. Elevated proximal tibial strains following unicompartmental knee replacement--a possible cause of pain. Med. Eng. Phys. 2009, 31, 752–757. [Google Scholar] [CrossRef]
- Collier, M.B.; Eickmann, T.H.; Sukezaki, F.; McAuley, J.P.; Engh, G.A. Patient, implant, and alignment factors associated with revision of medial compartment unicondylar arthroplasty. J. Arthroplast. 2006, 21, 108–115. [Google Scholar] [CrossRef]





| Intra Observer ICC | Inter Observer ICC | Agreement | |
|---|---|---|---|
| HKA angle | 0.98 | 0.98 | Excellent |
| mMDFA | 0.95 | 0.92 | Excellent |
| MPTA | 0.90 | 0.83 | Excellent |
| Tibial slope | 0.82 | 0.83 | Excellent |
| Cartier angle | 0.85 | 0.69 | Very good |
| Joint line height | 0.85 | 0.72 | Very good |
| Tibial cut height | 0.80 | 0.75 | Very good |
| Tibial cut Coronal Axis | 0.87 | 0.78 | Very good |
| Preoperative Data N = 50 | Postoperative Data N = 50 | |
|---|---|---|
| HKA (°) | 173.5 ± 3.6 | 176.5 ± 3.1 |
| (mean ± SD) [Min; Max] | [164.6; 180] | [170; 185] |
| mMDFA (°) | 91.2 ± 2.2 | 92.2 ± 2.3 |
| (mean ± SD) [Min; Max] | [87; 96] | [88; 96] |
| MPTA (°) | 86.4 ± 1.5 | 86.8 ± 1.5 |
| (mean ± SD) [Min; Max] | [83; 89] | [84; 90] |
| OUTLIERS MPTA < 85° | 6 (12%) | 1 (2%) |
| Slope (°) | 80.9 ± 3.2 | 82.6 ± 2.3 |
| (mean ± SD) [Min; Max] | [74; 87] | [78; 87] |
| OUTLIERS Slope < 78° | 7 (14%) | 0 |
| Cartier angle (°) | 2.6 ± 2.8 | - |
| (mean ± SD) [Min; Max] | [−3; 7] | - |
| Joint line height (femoral cortex) (mm) | - | 0.9 ± 1.1 |
| (mean ± SD) [Min; Max] | [−1.7; 4.5] | |
| Joint line height (femoral diaphysis) (mm) | - | 0.8 ± 1.1 |
| (mean ± SD) [Min; Max] | [−1.7; 4.5] | |
| OUTLIERS Joint line height > 2 mm | - | 3 (6%) |
| Tibial resection height (mm) | - | 6.0 ± 1.7 |
| (mean ± SD) [Min; Max] | [1; 9.5] | |
| Tibial cut axis (°) | - | 87.7 ± 1.6 |
| (mean ± SD) [Min; Max] | [84; 92] | |
| OUTLIERS Tibial cut axis < 85° | - | 1 (2%) |
| OUTLIERS Tibial cut axis > 90° | - | 2 (4%) |
| Difference between tibial cut and Cartier angle (°) | - | 0.57 ± 1.1 |
| (mean in absolute value ± SD) [Min; Max] | [−5; 4] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parratte, S.; Daxhelet, J.; Argenson, J.-N.; Batailler, C. The Deep-MCL Line: A Reliable Anatomical Landmark to Optimize the Tibial Cut in UKA. J. Pers. Med. 2023, 13, 855. https://doi.org/10.3390/jpm13050855
Parratte S, Daxhelet J, Argenson J-N, Batailler C. The Deep-MCL Line: A Reliable Anatomical Landmark to Optimize the Tibial Cut in UKA. Journal of Personalized Medicine. 2023; 13(5):855. https://doi.org/10.3390/jpm13050855
Chicago/Turabian StyleParratte, Sébastien, Jeremy Daxhelet, Jean-Noel Argenson, and Cécile Batailler. 2023. "The Deep-MCL Line: A Reliable Anatomical Landmark to Optimize the Tibial Cut in UKA" Journal of Personalized Medicine 13, no. 5: 855. https://doi.org/10.3390/jpm13050855
APA StyleParratte, S., Daxhelet, J., Argenson, J.-N., & Batailler, C. (2023). The Deep-MCL Line: A Reliable Anatomical Landmark to Optimize the Tibial Cut in UKA. Journal of Personalized Medicine, 13(5), 855. https://doi.org/10.3390/jpm13050855






