MicroRNAs Associated with the Pathophysiological Mechanisms of Gestational Diabetes Mellitus: A Systematic Review for Building a Panel of miRNAs
Abstract
1. Introduction
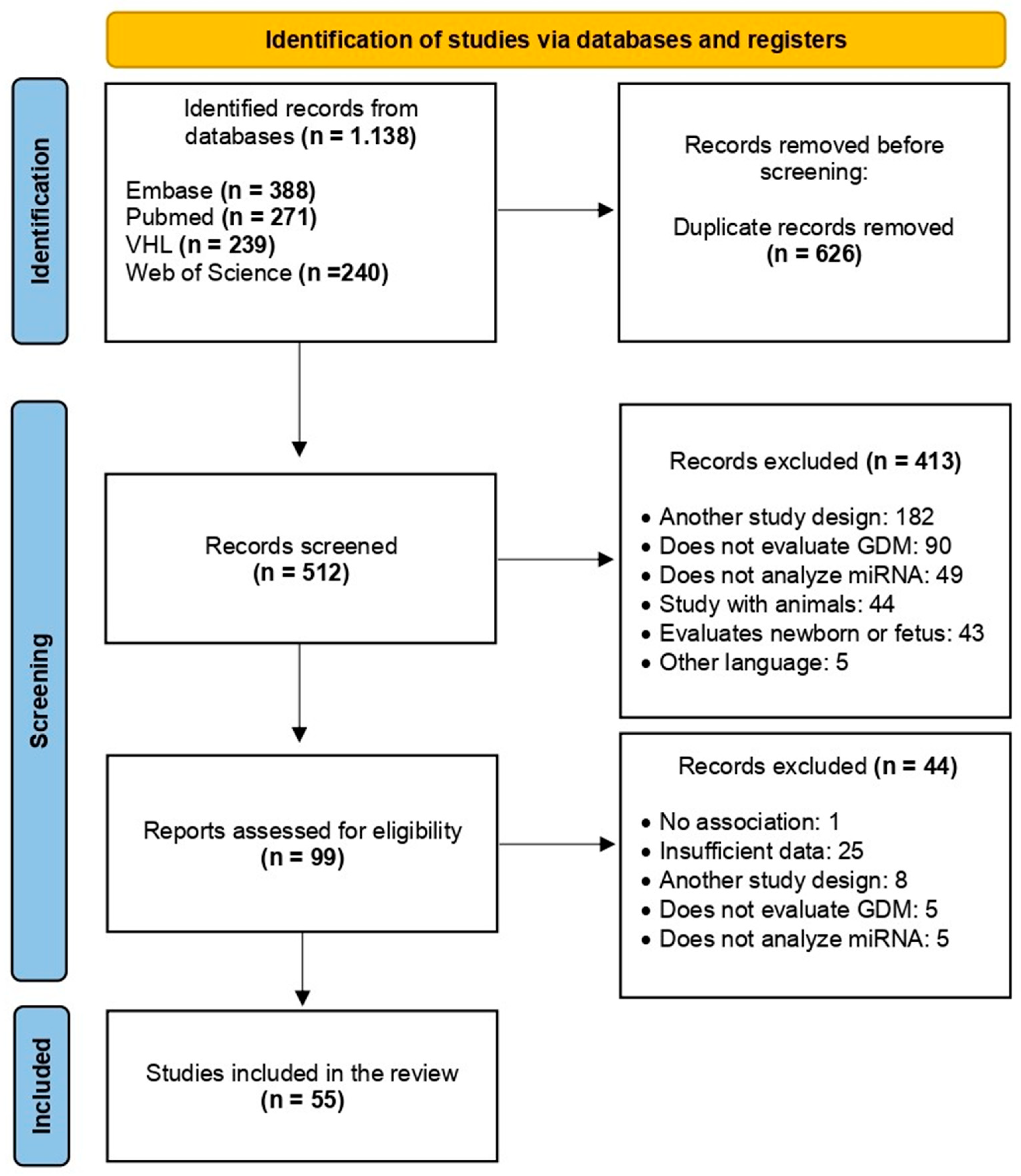
2. Materials and Methods
2.1. Registration, Data Source, and Search Strategy
2.2. Selection of Studies
2.3. Risk of Bias Assessment
2.4. Data Extraction and Synthesis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Caughey, A.B.; Turrentine, M. ACOG practice bulletin No. 190 Summary: Gestational diabetes mellitus. Obs. Gynecol. 2018, 131, 406–408. [Google Scholar]
- Durnwald, C. Gestational Diabetes Mellitus: Screening, Diagnosis, and Prevention; Nathan, D.M., Werner, E.F., Eds.; UpToDate: Wellesley, MA, USA, 2022. [Google Scholar]
- Carracher, A.M.; Marathe, P.H.; Close, K.L. International Diabetes Federation 2017. J. Diabetes 2018, 10, 353–356. [Google Scholar] [CrossRef]
- McIntyre, H.D.; Catalano, P.; Zhang, C.; Desoye, G.; Mathiesen, E.R.; Damm, P. Gestational diabetes mellitus. Nat. Rev. Dis. Prim. 2019, 5, 48. [Google Scholar] [CrossRef]
- Yang, X.; Wu, N. MicroRNAs and Exosomal microRNAs May Be Possible Targets to Investigate in Gestational Diabetes Mellitus. Diabetes Metab. Syndr. Obes. 2022, 15, 321–330. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Diagnostic criteria and classification of hyperglycemia first detected in pregnancy: A World Health Organization guideline. Diabetes Res. Clin. Pract. 2014, 103, 341–363. [Google Scholar] [CrossRef]
- Liu, Z.-N.; Jiang, Y.; Liu, X.-Q.; Yang, M.M.; Chen, C.; Zhao, B.-H.; Huang, H.-F.; Luo, Q. MiRNAs in Gestational Diabetes Mellitus: Potential Mechanisms and Clinical Applications. J. Diabetes Res. 2021, 2021, 4632745. [Google Scholar] [CrossRef]
- Metzger, B.E.; Coustan, D.R.; Trimble, E.R. Hyperglycemia and adverse pregnancy outcomes. Clin. Chem. 2019, 65, 937–938. [Google Scholar] [CrossRef]
- Guarino, E.; Poggi, C.D.; Grieco, G.E.; Cenci, V.; Ceccarelli, E.; Crisci, I.; Sebastiani, G.; Dotta, F. Circulating MicroRNAs as Biomarkers of Gestational Diabetes Mellitus: Updates and perspectives. Int. J. Endocrinol. 2018, 2018, 6380463. [Google Scholar] [CrossRef]
- Cuffe, J.S.M.; Holland, O.; Salomon, C.; Rice, G.E.; Perkins, A.V. Review: Placental derived biomarkers of pregnancy disorders. Placenta 2017, 54, 104–110. [Google Scholar] [CrossRef]
- Jonas, S.; Izaurralde, E. Towards a molecular understanding of microRNA-mediated gene silencing. Nat. Rev. Genet. 2015, 16, 421–433. [Google Scholar] [CrossRef]
- Sun, B.K.; Tsao, H. Small RNAs in development and disease. J. Am. Acad. Derm. 2008, 59, 725–737. [Google Scholar] [CrossRef] [PubMed]
- Morales-Prieto, D.M.; Ospina-Prieto, S.; Schmidt, A.; Chaiwangyen, W.; Markert, U.R. Elsevier Trophoblast Research Award Lecture: Origin, evolution and future of placenta miRNAs. Placenta 2014, 35, S39–S45. [Google Scholar] [CrossRef]
- Cai, M.; Kolluru, G.K.; Ahmed, A. Small molecule, big prospects: Microrna in pregnancy and its complications. J. Pregnancy 2017, 2017, 6972732. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, S.; Bohl, M.; Gregersen, S.; Hermansen, K.; O’Driscoll, L. Blood-based biomarkers for metabolic syndrome. Trends Endocrinol. Metab. 2016, 27, 363–374. [Google Scholar] [CrossRef]
- Iljas, J.D.; Guanzon, D.; Elfeky, O.; Rice, G.E.; Salomon, C. Review: Bio-compartmentalization of microRNAs in exosomes during gestational diabetes mellitus. Placenta 2017, 54, 76–82. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Institute TJB. JBI Reviewer’s Manual. Joanna Briggs Inst. 32. The Joanna Briggs Institute 2022. Available online: https://reviewersmanual.joannabriggs.org/ (accessed on 30 September 2022).
- Ke, W.; Chen, Y.; Zheng, L.; Zhang, Y.; Wu, Y.; Li, L. miR-134-5p promotes inflammation and apoptosis of trophoblast cells via regulating FOXP2 transcription in gestational diabetes mellitus. Bioengineered 2022, 13, 319–330. [Google Scholar] [CrossRef]
- Wang, P.; Ma, Z.; Wang, Z.; Wang, X.; Zhao, G.; Wang, Z. MiR-6869-5p Induces M2 Polarization by Regulating PTPRO in Gestational Diabetes Mellitus. Mediat. Inflamm. 2021, 2021, 6696636. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, J.; Liu, Y. MicroRNA-1323 serves as a biomarker in gestational diabetes mellitus and aggravates high glucose-induced inhibition of trophoblast cell viability by suppressing TP53INP1. Exp. Ther. Med. 2021, 21, 230. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, T.; Sun, D.; Cheng, G.; Ren, H.; Hong, H.; Chen, L.; Jiao, X.; Du, Y.; Zou, Y.; et al. Diagnostic value of dysregulated microribonucleic acids in the placenta and circulating exosomes in gestational diabetes mellitus. J. Diabetes Investig. 2021, 12, 1490–1500. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhuang, J. miR-345-3p serves a protective role during gestational diabetes mellitus by targeting BAK1. Exp. Ther. Med. 2021, 21, 2. [Google Scholar] [CrossRef] [PubMed]
- Guan, C.-Y.; Tian, S.; Cao, J.-L.; Wang, X.-Q.; Ma, X.; Xia, H.-F. Down-Regulated miR-21 in Gestational Diabetes Mellitus Placenta Induces PPAR-α to Inhibit Cell Proliferation and Infiltration. Diabetes Metab. Syndr. Obes. 2020, 13, 3009–3034. [Google Scholar] [CrossRef] [PubMed]
- Deng, L.; Huang, Y.; Li, L.; Chen, H.; Su, J. Serum miR-29a/b expression. in gestational diabetes mellitus and its influence on prognosis evaluation. J. Int. Med. Res. 2020, 48, 300060520954763. [Google Scholar] [CrossRef]
- Zhao, C.; Zhao, C.; Zhao, H. Defective insulin receptor signaling in patients with gestational diabetes is related to dysregulated miR-140 which can be improved by naringenin. Int. J. Biochem. Cell Biol. 2020, 128, 105824. [Google Scholar] [CrossRef]
- Xiao, Y.; Ding, J.; Shi, Y.; Lin, L.; Huang, W.; Shen, D.; Wang, W. MiR-330-3p contributes to INS-1 cell dysfunction by targeting glucokinase in gestational diabetes mellitus. J. Obs. Gynaecol. Res. 2020, 46, 864–875. [Google Scholar] [CrossRef]
- Tang, L.; Li, P.; Li, L. Whole transcriptome expression profiles in placenta samples from women with gestational diabetes mellitus. J. Diabetes Investig. 2020, 11, 1307–1317. [Google Scholar] [CrossRef]
- Hocaoglu, M.; Demirer, S.; Senturk, H.; Turgut, A.; Komurcu-Bayrak, E. Differential expression of candidate circulating microRNAs in maternal blood leukocytes of the patients with preeclampsia and gestational diabetes mellitus. Pregnancy Hypertens. 2019, 17, 5–11. [Google Scholar] [CrossRef]
- Stirm, L.; Huypens, P.; Sass, S.; Batra, R.; Fritsche, L.; Brucker, S.; Abele, H.; Hennige, A.M.; Theis, F.; Beckers, J.; et al. Maternal whole blood cell miRNA-340 is elevated in gestational diabetes and inversely regulated by glucose and insulin. Sci. Rep. 2018, 8, 1366. [Google Scholar] [CrossRef]
- Wander, P.L.; Boyko, E.J.; Hevner, K.; Parikh, V.J.; Tadesse, M.G.; Sorensen, T.K.; Williams, M.A.; Enquobahrie, D.A. Circulating early- and mid-pregnancy microRNAs and risk of gestational diabetes. Diabetes Res. Clin. Pract. 2017, 132, 1–9. [Google Scholar] [CrossRef]
- Hocaoglu, M.; Demirer, S.; Karaalp, I.L.; Kaynak, E.; Attar, E.; Turgut, A.; Karateke, A.; Komurcu-Bayrak, E. Identification of miR-16-5p and miR-155-5p microRNAs differentially expressed in circulating leukocytes of pregnant women with polycystic ovary syndrome and gestational diabetes. Gynecol. Endocrinol. 2020, 37, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Hua, Z.; Li, D.; Wu, A.; Cao, T.; Luo, S. miR-377 inhibition enhances the survival of trophoblast cells via upregulation of FNDC5 in gestational diabetes mellitus. Open Med. 2021, 16, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Shen, H.; Sun, J.; Liu, J.; Wang, L.; Dong, L. miR-181d promotes pancreatic beta cell dysfunction by targeting IRS2 in gestational diabetes mellitus. Ginekol. Pol. 2021, 92, 563–570. [Google Scholar] [CrossRef]
- Balci, S.; Gorur, A.; Yildirim, D.D.; Cayan, F.; Tamer, L. Expression level of miRNAS in patients with gestational diabetes. Turk. J. Biochem. 2020, 45, 825–831. [Google Scholar] [CrossRef]
- Ji, Y.; Zhang, W.; Yang, J.; Li, C. MiR-193b inhibits autophagy and apoptosis by targeting IGFBP5 in high glucose-induced trophoblasts. Placenta 2020, 101, 185–193. [Google Scholar] [CrossRef]
- Tu, C.; Wang, L.; Tao, H.; Gu, L.; Zhu, S.; Chen, X. Expression of miR-409-5p in gestational diabetes mellitus and its relationship with insulin resistance. Exp. Med. 2020, 20, 3324–3329. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, S.; Sánchez-Lechuga, B.; Donovan, P.; Halang, L.; Prehn, J.H.M.; Campos-Caro, A.; Byrne, M.M.; López-Tinoco, C. Circulating miR-330-3p in Late Pregnancy is Associated with Pregnancy Outcomes Among Lean Women with GDM. Sci. Rep. 2020, 10, 908. [Google Scholar] [CrossRef]
- Zhu, Y.; Tian, F.; Li, H.; Zhou, Y.; Lu, J.; Ge, Q. Profiling maternal plasma microRNA expression in early pregnancy to predict gestational diabetes mellitus. Int. J. Gynaecol. Obstet. 2015, 130, 49–53. [Google Scholar] [CrossRef]
- Zhao, C.; Dong, J.; Jiang, T.; Shi, Z.; Yu, B.; Zhu, Y.; Chen, D.; Xu, J.; Huo, R.; Dai, J.; et al. Early Second-Trimester Serum MiRNA Profiling Predicts Gestational Diabetes Mellitus. PLoS ONE 2011, 6, e23925. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, X.; Zhou, H. Role of cell free microRNA-19a and microRNA-19b in gestational diabetes mellitus patients. 3 Biotech 2019, 9, 406. [Google Scholar] [CrossRef]
- Gillet, V.; Ouellet, A.; Stepanov, Y.; Rodosthenous, R.S.; Croft, E.K.; Brennan, K.; Abdelouahab, N.; Baccarelli, A.; Takser, L. miRNA Profiles in Extracellular Vesicles from Serum Early in Pregnancies Complicated by Gestational Diabetes Mellitus. J. Clin. Endocrinol. Metab. 2019, 104, 5157–5169. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Wang, H.; Li, C.; Zhang, X.; Xiu, X.; Teng, P.; Wang, Z. Dysregulation of microRNA-657 influences inflammatory response via targeting interleukin-37 in gestational diabetes mellitus. J. Cell. Physiol. 2019, 234, 7141–7148. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Wang, Z.; Liu, G.; Jin, C.; Zhang, Q.; Man, S.; Wang, Z. miR-657 Promotes Macrophage Polarization toward M1 by Targeting FAM46C in Gestational Diabetes Mellitus. Mediat. Inflamm. 2019, 2019, 4851214. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Song, L.; Zhou, L.; Wu, J.; Sheng, C.; Chen, H.; Liu, Y.; Gao, S.; Huang, W. A MicroRNA Signature in Gestational Diabetes Mellitus Associated with Risk of Macrosomia. Cell. Physiol. Biochem. 2015, 37, 243–252. [Google Scholar] [CrossRef]
- Sørensen, A.E.; van Poppel, M.N.M.; Desoye, G.; Damm, P.; Simmons, D.; Jensen, D.M.; Dalgaard, L.T.; DALI Core Investigator Group. The Predictive Value of miR-16, -29a and -134 for Early Identification of Gestational Diabetes: A Nested Analysis of the DALI Cohort. Cells 2021, 10, 170. [Google Scholar] [CrossRef]
- Xu, K.; Bian, D.; Hao, L.; Huang, F.; Xu, M.; Qin, J.; Liu, Y. microRNA-503 contribute to pancreatic β cell dysfunction by targeting the mTOR pathway in gestational diabetes mellitus. EXCLI J. 2017, 16, 1177–1187. [Google Scholar]
- He, Y.; Bai, J.; Liu, P.; Dong, J.; Tang, Y.; Zhou, J.; Han, P.; Xing, J.; Chen, Y.; Yu, X. miR-494 protects pancreatic β-cell function by targeting PTEN in gestational diabetes mellitus. EXCLI J. 2017, 16, 1297–1307. [Google Scholar]
- Sebastiani, G.; Guarino, E.; Grieco, G.E.; Formichi, C.; Poggi, C.D.; Ceccarelli, E.; Dotta, F. Circulating microRNA (miRNA) expression Profiling in Plasma of Patients with gestational Diabetes Mellitus reveals Upregulation of miRNA mir-330-3p. Front. Endocrinol. 2017, 8, 345. [Google Scholar] [CrossRef]
- Filardi, T.; Catanzaro, G.; Grieco, G.E.; Splendiani, E.; Trocchianesi, S.; Santangelo, C.; Brunelli, R.; Guarino, E.; Sebastiani, G.; Dotta, F.; et al. Identification and Validation of miR-222-3p and miR-409-3p as Plasma Biomarkers in Gestational Diabetes Mellitus Sharing Validated Target Genes Involved in Metabolic Homeostasis. Int. J. Mol. Sci. 2022, 23, 4276. [Google Scholar] [CrossRef]
- Yu, X.; Liu, Z.; Fang, J.; Qi, H. miR-96-5p: A potential diagnostic marker for gestational diabetes mellitus. Medicine 2021, 100, e25808. [Google Scholar] [CrossRef]
- Zhou, X.; Xiang, C.; Zheng, X. miR-132 serves as a diagnostic biomarker in gestational diabetes mellitus and its regulatory effect on trophoblast cell viability. Diagn. Pathol. 2019, 14, 119. [Google Scholar] [CrossRef]
- Abdeltawab, A.; Zaki, M.E.; Abdeldayem, Y.; Mohamed, A.A.; Zaied, S.M. Circulating Micro RNA-223 and Angiopoietin-Like Protein 8 as Biomarkers of Gestational Diabetes mellitus. Br. J. Biomed. Sci. 2020, 78, 12–17. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Zhao, C.; Guo, X.; Ding, H.; Cui, Y.; Shen, R.; Liu, J. Differential Expression of MicroRNAs in Omental Adipose Tissue from Gestational Diabetes Mellitus Subjects Reveals miR-222 as a Regulator of ER Expression in Estrogen-Induced Insulin Resistance. Endocrinology 2014, 155, 1982–1990. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Jiang, Y.; Li, L.-F.; Liu, X. Upregulation of YWHAZ in placental tissues, blood, and amniotic fluid from patients with gestational diabetes mellitus related to downregulation of microRNA-214. Int. J. Clin. Exp. Med. 2019, 12, 9961–9968. [Google Scholar]
- Sun, D.-G.; Tian, S.; Zhang, L.; Hu, Y.; Guan, C.-Y.; Ma, X.; Xia, H.-F. The miRNA-29b Is Downregulated in Placenta During Gestational Diabetes Mellitus and May Alter Placenta Development by Regulating Trophoblast Migration and Invasion Through a HIF3A-Dependent Mechanism. Front. Endocrinol. 2020, 11, 169. [Google Scholar] [CrossRef] [PubMed]
- Yoffe, L.; Polsky, A.; Gilam, A.; Raff, C.; Mecacci, F.; Ognibene, A.; Crispi, F.; Gratacós, E.; Kanety, H.; Mazaki-Tovi, S.; et al. Early diagnosis of gestational diabetes mellitus using circulating microRNAs. Eur. J. Endocrinol. 2019, 181, 565–577. [Google Scholar] [CrossRef]
- Zhang, Y.-L.; Chen, X.-Q. Dysregulation of microRNA-770-5p influences pancreatic-β-cell function by targeting TP53 regulated inhibitor of apoptosis 1 in gestational diabetes mellitus. Eur. Rev. Med. Pharm. Sci. 2020, 24, 793–801. [Google Scholar]
- Wen, J.; Bai, X. miR-520h Inhibits cell survival by targeting mTOR in gestational diabetes mellitus. Acta Biochim. Pol. 2021, 68, 65–70. [Google Scholar] [CrossRef]
- Zhang, M.; Zhu, X. miR-9-5p plays an important role in gestational diabetes mellitus (GDM) progression by targeting HK-2. Int. J. Clin. Exp. Med. 2018, 11, 6694–6701. [Google Scholar]
- Pheiffer, C.; Dias, S.; Rheeder, P.; Adam, S. Decreased Expression of Circulating miR-20a-5p in South African Women with Gestational Diabetes Mellitus. Mol. Diagn. Ther. 2018, 22, 345–352. [Google Scholar] [CrossRef]
- Feng, Y.; Qu, X.; Chen, Y.; Feng, Q.; Zhang, Y.; Hu, J.; Li, X. MicroRNA-33a-5p sponges to inhibit pancreatic β-cell function in gestational diabetes mellitus LncRNA DANCR. Reprod. Biol. Endocrinol. 2020, 18, 61. [Google Scholar] [CrossRef]
- Zhang, C.; Wang, L.; Chen, J.; Song, F.; Guo, Y. Differential Expression of miR-136 in Gestational Diabetes Mellitus Mediates the High-Glucose-Induced Trophoblast Cell Injury through Targeting E2F1. Int. J. Genom. 2020, 2020, 3645371. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, K.; Tian, S.; Wang, X.-Q.; Li, J.-H.; Dong, Y.-C.; Xia, H.-F.; Ma, X. Down-regulation of microRNA-30d-5p is associated with gestational diabetes mellitus by targeting RAB8A. J. Diabetes Complicat. 2021, 35, 107959. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Pan, Y.; Dai, F.; Wang, F.; Qiu, H.; Huang, X. Serum miR-195-5p is upregulated in gestational diabetes mellitus. J. Clin. Lab. Anal. 2020, 34, e23325. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.-L.; Zhang, L.; Li, J.; Tian, S.; Lv, X.-D.; Wang, X.-Q.; Su, X.; Li, Y.; Hu, Y.; Ma, X.; et al. Up-regulation of miR-98 and unraveling regulatory mechanisms in gestational diabetes mellitus. Sci. Rep. 2016, 6, 32268. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.-L.; Jia, Y.-J.; Xing, B.; Shi, D.; Dong, X. Plasma microRNA-16-5p, -17-5p and -20a-5p: Novel diagnostic biomarkers for gestational diabetes mellitus. J. Obs. Gynaecol. Res. 2017, 43, 974–981. [Google Scholar] [CrossRef]
- Wang, F.; Li, Z.; Zhao, M.; Ye, W.; Wu, H.; Liao, Q.; Bu, S.; Zhang, Y. Circulating miRNAs miR-574-5p and miR-3135b are potential metabolic regulators for serum lipids and blood glucose in gestational diabetes mellitus. Gynecol. Endocrinol. 2021, 37, 665–671. [Google Scholar] [CrossRef]
- Van Oostdam, A.S.H.; Toro-Ortíz, J.C.; López, J.A.; Noyola, D.E.; Garcia-López, D.A.; Durán-Figueroa, N.V.; Martínez-Martínez, E.; Portales-Pérez, D.P.; Salgado-Bustamante, M.; López-Hernández, Y. Placental exosomes isolated from urine of patients with gestational diabetes exhibit a differential profile expression of microRNAs across gestation. Int. J. Mol. Med. 2020, 46, 546–560. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.-Y.; Li, H.-P.; Li, M.-Q. High glucose induces dysfunction of human umbilical vein endothelial cells by upregulating miR-137 in gestational diabetes mellitus. Microvasc. Res. 2018, 118, 90–100. [Google Scholar] [CrossRef]
- Tagoma, A.; Alnek, K.; Kirss, A.; Uibo, R.; Haller-Kikkatalo, K. MicroRNA profiling of second trimester maternal plasma shows upregulation of miR-195-5p in patients with gestational diabetes. Gene 2018, 672, 137–142. [Google Scholar] [CrossRef]
- Monfared, Y.K.; Ghadimi, F.; Foroughi, F.; Honardoost, M.; Hashemipour, S.; Sefidi, F.; Sarookhani, M.R. Determination and comparison miR135a in the serum between women with GDM, non-pregnant type 2 diabetes, healthy pregnant and control group. Middle East J. Fam. Med. 2018, 16, 193–197. [Google Scholar] [CrossRef]
- Wang, S.; Wei, D.; Sun, X.; Li, Y.; Li, D.; Chen, B. MiR-190b impedes pancreatic β cell proliferation and insulin secretion by targeting NKX6-1 and may associate to gestational diabetes mellitus. J. Recept. Signal Transduct. Res. 2021, 41, 349–356. [Google Scholar] [CrossRef]
- Gao, X.; Zhao, S. miRNA-16-5p inhibits the apoptosis of high glucose-induced pancreatic β cells via targeting of CXCL10: Potential biomarkers in type 1 diabetes mellitus. Endokrynol. Pol. 2020, 71, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Kwon, D.N.; Chang, B.S.; Kim, J.H. MicroRNA dysregulation in liver and pancreas of CMP-Neu5Ac hydroxylase null mice disrupts insulin/PI3K-AKT signaling. Biomed. Res. Int. 2014, 2014, 236385. [Google Scholar] [CrossRef] [PubMed]
- Geng, Y.; Ju, Y.; Ren, F.; Qiu, Y.; Tomita, Y.; Tomoeda, M.; Kishida, M.; Wang, Y.; Jin, L.; Su, F.; et al. Insulin receptor substrate 1/2 (IRS1/2) regulates Wnt/β-catenin signaling through blocking autophagic degradation of dishevelled2. J. Biol. Chem. 2014, 289, 11230–11241. [Google Scholar] [CrossRef]
- Li, H.-P.; Chen, X.; Li, M.-Q. Gestational diabetes induces chronic hypoxia stress and excessive inflammatory response in murine placenta. Int. J. Clin. Exp. Pathol. 2013, 6, 650–659. [Google Scholar]
- Li, Y.; Xiao, R.; Li, C.-P.; Huangfu, J.; Mao, J.-F. Increased plasma levels of FABP4 and PTEN is associated with more severe insulin resistance in women with gestational diabetes mellitus. Med. Sci. Monit. 2015, 21, 426–431. [Google Scholar]
- Magee, T.R.; Ross, M.G.; Wedekind, L.; Desai, M.; Kjos, S.; Belkacemi, L. Gestational diabetes mellitus alters apoptotic and inflammatory gene expression of trophobasts from human term placenta. J. Diabetes Complicat. 2014, 28, 448–459. [Google Scholar] [CrossRef]
- Nishiyama, A.; Yoshizumi, M.; Rahman, M.; Kobori, H.; Seth, D.M.; Miyatake, A.; Zhang, G.-X.; Yao, L.; Hitomi, H.; Shokoji, T.; et al. Effects of AT1 receptor blockade on renal injury and mitogen-activated protein activity in Dahl salt-sensitive rats. Kidney Int. 2004, 65, 972–981. [Google Scholar] [CrossRef]
- Perucci, L.O.; Gomes, K.B.; Freitas, L.G.; Godoi, L.C.; Alpoim, P.N.; Pinheiro, M.B.; Miranda, A.S.; Teixeira, A.L.; Dusse, L.M.; Sousa, L.P. Soluble endoglin, transforming growth factor-Beta 1 and soluble tumor necrosis factor alpha receptors in different clinical manifestations of preeclampsia. PLoS ONE 2014, 9, e97632. [Google Scholar] [CrossRef]
- Kumar, A.; Lawrence Jr, J.C.; Jung, D.Y.; Ko, H.J.; Keller, S.R.; Kim, J.K.; Magnuson, M.A.; Harris, T.E. Fat cell-specific ablation of rictor in mice impairs insulin-regulated fat cell and whole-body glucose and lipid metabolism. Diabetes 2010, 59, 1397–1406. [Google Scholar] [CrossRef] [PubMed]
- Qian, K.; Hu, L.; Chen, H.; Li, H.; Liu, N.; Li, Y.; Ai, J.; Zhu, G.; Tang, Z.; Zhang, H. Hsa-miR-222 is involved in differentiation of endometrial stromal cells in vitro. Endocrinology 2009, 150, 4734–4743. [Google Scholar] [CrossRef]
- Margaritis, K.; Margioula-Siarkou, G.; Giza, S.; Kotanidou, E.P.; Tsinopoulou, V.R.; Christoforidis, A.; Galli-Tsinopoulou, A. Micro-RNA implications in type-1 diabetes mellitus: A review of literature. Int. J. Mol. Sci. 2021, 22, 12165. [Google Scholar] [CrossRef] [PubMed]
- Poirier, C.; Desgagné, V.; Guérin, R.; Bouchard, L. MicroRNAs in pregnancy and gestational diabetes mellitus: Emerging role in maternal metabolic regulation. Curr. Diab. Rep. 2017, 17, 1–10. [Google Scholar] [CrossRef]
- Long, H.; Cundy, T. Establishing consensus in the diagnosis of gestational diabetes following HAPO: Where do we stand? Curr. Diabetes Rep. 2013, 13, 43–50. [Google Scholar] [CrossRef]
- Yang, Y.; Li, Q.; Wang, Q.; Ma, X. Thyroid antibodies and gestational diabetes mellitus: A meta-analysis. Fertil. Steril. 2015, 104, 665–671. [Google Scholar] [CrossRef] [PubMed]

| Database | Search Strategy |
|---|---|
| PubMed/Medline | ((“Diabetes, Gestational” OR “Diabetes Gestacional” OR “Diabetes Mellitus, Gestational” OR “Diabetes, Pregnancy Induced” OR “Diabetes, Pregnancy-Induced” OR “Gestational Diabetes” OR “Gestational Diabetes Mellitus” OR “Pregnancy-Induced Diabetes”) AND (“MicroRNAs” OR “Micro RNA” OR “MicroRNA” OR “MicroRNA, Primary” OR “miRNA” OR “miRNA, Primary” OR “miRNAs” OR “pre miRNA” OR “pre-miRNA” OR “pri miRNA” OR “pri-miRNA” OR “Primary MicroRNA” OR “Primary miRNA” OR “RNA, Micro” OR “Small Temporal RNA” OR “stRNA” OR “MicroARNs” OR “miARN” OR “miARNs” OR “Micro ARN” OR “Micro ARNs” OR “MicroARN” OR “stARN” OR “Circulating MicroRNA” OR “Cell Free MicroRNA” OR “Cell-Free MicroRNA” OR “MicroRNA, Cell-Free” OR “MicroRNA, Circulating”)) |
| Virtual Health Library | (“microrna”) AND (“gestational diabetes”) AND (mj:(“Diabetes Gestacional” OR “MicroRNAs”)) |
| Web of Science | ((“Diabetes, Gestational” OR “Diabetes Mellitus, Gestational” OR “Diabetes, Pregnancy Induced” OR “Diabetes, Pregnancy-Induced” OR “Gestational Diabetes” OR “Gestational Diabetes Mellitus” OR “Pregnancy-Induced Diabetes”) AND (“MicroRNAs” OR “Micro RNA” OR “MicroRNA” OR “MicroRNA, Primary” OR “miRNA” OR “miRNA, Primary” OR “miRNAs” OR “pre miRNA” OR “pre-miRNA” OR “pri miRNA” OR “pri-miRNA” OR “Primary MicroRNA” OR “Primary miRNA” OR “RNA, Micro” OR “RNA, Small Temporal” OR “Small Temporal RNA” OR “sirna” OR “stRNA” OR “Temporal RNA, Small” OR “MicroARNs”)) |
| EMBASE | (‘diabetes, gestational’/exp OR ‘diabetes, gestational’ OR ‘diabetes gestacional’ OR ‘diabetes, pregnancy induced’ OR ‘diabetes, pregnancy-induced’ OR ‘gestational diabetes’/exp OR ‘gestational diabetes’ OR ‘gestational diabetes mellitus’/exp OR ‘gestational diabetes mellitus’ OR ‘pregnancy-induced diabetes’) AND (‘micrornas’/exp OR ‘micrornas’ OR ‘micro rna’/exp OR ‘micro rna’ OR ‘microrna’/exp OR ‘microrna’ OR ‘microrna, primary’ OR ‘mirna’/exp OR ‘mirna’ OR ‘mirna, primary’ OR ‘mirnas’/exp OR ‘mirnas’ OR ‘pre mirna’ OR ‘pre-mirna’ OR ‘pri mirna’ OR ‘pri-mirna’ OR ‘primary microrna’/exp OR ‘primary microrna’ OR ‘primary mirna’ OR ‘rna, micro’ OR ‘rna, small temporal’ OR ‘small temporal rna’ OR ‘strna’ OR ‘temporal rna, small’ OR ‘microarns’ OR ‘arn pequeño temporal’ OR ‘arn temporal pequeño’ OR ‘miarn’ OR ‘miarns’ OR ‘micro arn’ OR ‘micro arns’ OR ‘microarn’ OR ‘microarn primario’ OR ‘microrna primario’ OR ‘starn’ OR ‘rna pequeno temporário’ OR ‘rna temporário pequeno’ OR ‘circulating microrna’/exp OR ‘circulating microrna’ OR ‘cell free microrna’/exp OR ‘cell free microrna’ OR ‘cell-free microrna’/exp OR ‘cell-free microrna’ OR ‘microrna, cell-free’ OR ‘microrna, circulating’ OR ‘microarn circulante’ OR ‘microrna circulante’ OR ‘microrna fora da célula’ OR ‘microrna livre’) AND (‘biological marker’/dd OR ‘circular ribonucleic acid’/dd OR ‘glucose’/dd OR ‘insulin’/dd OR ‘microrna’/dd OR ‘microrna 122’/dd OR ‘microrna 143’/dd OR ‘microrna 146a’/dd OR ‘microrna 16’/dd OR ‘microrna 21’/dd OR ‘microrna 210’/dd OR ‘microrna 222’/dd OR ‘rna’/dd OR ‘small interfering rna’/dd OR ‘transcription factor’/dd) AND (‘congenital heart disease’/dm OR ‘diabetes mellitus’/dm OR ‘diabetic complication’/dm OR ‘intrauterine growth retardation’/dm OR ‘macrosomia’/dm OR ‘maternal diabetes mellitus’/dm OR ‘pregnancy diabetes mellitus’/dm) |
| Authors And Year of Publication | Study Design | Country or Continent | Sample Size | Mean Age | Gestational Time | Sample Type | miRNA Identification Technique | miRNA | Regulation | p-Value |
|---|---|---|---|---|---|---|---|---|---|---|
| [20] | Case-control | China | Case: 70 Control: 70 | Case: 30.33 ± 2.25 Control: 30.04 ± 2.25 | Case: 39.12 ± 1.15 Control: 38.76 ± 1.06 (weeks) | Blood | qRT-PCR | miR-134-5p | Up-regulation | <0.001 |
| [21] | Case-control | China | Case: 26 Control: 23 | Case: 30.6 ± 4.4 Control: 29.2 ± 3.5 | Case: 38.1 ± 1.2 Control: 39.4 ± 1.2 (weeks) | Placenta | RT-PCR | miR-6869-5p | Down-regulation | <0.001 |
| [22] | Case-control | China | Case: 110 Control: 78 | Case: 33,118 ± 3402 Control: 32,385 ± 3579 | Case: 25.591 ± 1.757 Control: 25.218 ± 2.196 | Blood | qRT-PCR | miR-1323 | Up-regulation | <0.05 |
| [23] | Cross-sectional | China | Case: 36 Control: 37 | 20–40 Years | 37–41 Weeks | Placenta | qRT-PCR | miR-125b; miR-144; miR-543 | Up-regulation | <0.001 |
| [24] | Case-control | China | Case: 30 Control: 30 | Case: 24–39 Control: 24–39 | 24–28 Weeks | Plasma and Placenta | qRT-PCR | miR-345-3p | Down-regulation | <0.01 |
| [25] | Case-control | Gana | Case: 137 Control: 158 | Case: 30.94 ± 3.45 Control: 29.67 ± 3.64 | Case: 272.22 ± 6.40 Control: 274.41 ± 8.02 (Days) | Placenta | qRT-PCR | miR-21 | Down-regulation | <0.01 |
| [26] | Case-control | China | Case: 68 Control: 55 | Case:32.65 ± 4.63 Control: 31.27 ± 4.01 | Case: 39.09 ± 1.11 Control: 38.98 ± 1.05 (weeks) | Plasma | qRT-PCR | miR-29a; miR-29b | Down-regulation | <0.001 |
| [27] | Case-control | China | Case: 33 Control: 20 | ND | Case: 24–26 weeks Control: 37–41 weeks | Placenta | qRT-PCR | miR-140-3p | Up-regulation | <0.05 |
| [28] | Case-control | China | Case: 30 Control: 10 | ND | ND | Blood | qRT-PCR | miR-330-3p | Up-regulation | <0.001 |
| [29] | Case-control | China | Case: 20 Control: 20 | Case: 29.4 ± 1.2 Control: 29.6 ± 0.4 | Case: 38.7 ± 0.6 Control: 39.0 ± 1.0 | Placenta | qRT-PCR | miR-17; miR-195; miR-257 | Down-regulation; Up-regulation; Up-regulation | <0.01 |
| [30] | Case-control | Turkey | Case: 19 Control: 28 | Case: 30.4 ± 4.6 Control: 28.1 ± 5.8 | Case: 33.5 ± 3.6 Control: 33 ± 4.1 | Blood | qRT-PCR | miR-21-3p | Down-regulation | 0.008 |
| [31] | Case-control | Germany | Case: 30 Control: 30 | Case: 31 ± 4 Control: 32 ± 4 | Case: 27.0 ± 2.3 Control:27.6 ± 2.37 | Blood | qRT-PCR | miRNA-340 | Up-regulation | 0.02 |
| [32] | Cohort | United States | Case: 36 Control: 80 | Case: 34.3 ± 3.6 Control: 32.9 ± 4.4 | Case: 15.1 ± 2.9 Control: 16.5 ± 2.3 | Blood | qRT-PCR | miR-21-3p; miR-155-5p | ND | 0.005; 0.028 |
| [33] | Case-control | Turkey | Case: 14 Control: 27 | Case: 30.4 ± 4.4 Control: 27.9 ± 5.5 | Case: 33.5 ± 3.5 Control: 33.1 ± 4.1 | Blood | qPCR | miR-155-5p | Down-regulation | 0.04 |
| [34] | Case-control | China | Case: 30 Control: 38 | Case: 30.27 ± 6.38 Control: 33.21 ± 8.17 | Case: 38.12 ± 1.65 Control: 37.54 ± 1.31 | Blood | qRT-PCR | miR-377-3p | Up-regulation | <0.01 |
| [35] | Case-control | China | Case: 25 Control: 30 | ND | ND | Blood | qRT-PCR | miR-181d | Up-regulation | <0.01 |
| [36] | Case-control | Turkey | Case: 30 Control: 30 | Case: 32.3 Control: 29.9 | Case: 26.9 Control: 27.4 | Plasma | qRT-PCR | miR-7-5p | Up-regulation | 0.02 |
| [37] | Case-control | China | Case: 20 Control: 20 | Case: 35.30 ± 4.37 Control: 32.30 ± 3.40 | Case: 74.38 ± 8.58 Control: 71.50 ± 11.72 | Blood | qRT-PCR | miR-193b | Down-regulation | <0.001 |
| [38] | Case-control | China | Case: 76 Control: 73 | 27.02 ± 3.17 | ND | Blood | qRT-PCR | miR-409-5p | Up-regulation | <0.05 |
| [39] | Cohort | Spain | Case: 31 Control: 29 | Case: 31.9 ± 1.8 Control: 31.0 ± 3.6 | Case: 39.1 ± 1.3 Control: 39.2 ± 1.2 | Blood | qRT-PCR | miR-330-3p | Up-regulation | 0.003 |
| [40] | Case-control | China | Case: 10 Control: 10 | Case: 30.03 ± 3.56 Control: 26.67 ± 4.59 | Case: 17.66 ± 0.85 Control: 18.17 ± 0.93 | Blood | qRT-PCR | miR-16-5p; miR-17-5p; miR-19a-3p; miR-19b-3p; miR-20a-5p | Up-regulation | 5.36 × 10−11; 1.10 × 10−10; 6.57 × 10−43; 1.73 × 10−74; 5.27 × 10−37 |
| [41] | Case-control | China | Case: 24 Control: 24 | Case: 28.79 ± 2.21 Control: 29.46 ± 1.89 | Case: 17.40 ± 0.70 Control: 17.16 ± 0.79 | Plasma | qRT-PCR/ chip TLDA | miR-132; miR-29a; miR-222 | Down-regulation | 0.042; 0.032; 0.041 |
| [42] | Case-control | China | Case: 100 Control: 100 | ND | ND | Blood | qRT-PCR | miRNA-19a; miRNA-19b | Up-regulation | ND |
| [43] | Cohort | Canada | Case: 23 Control: 46 | Case: 29.8 ± 5.3 Control: 27.9 ± 4.4 | Case: 10.5 ± 2.5 Control: 10.6 ± 2.4 | Blood | qRT-PCR | miR-122-5p; miR-132-3p; miR-1323; miR-136-5p; miR-182-3p; miR-210-3p; miR-29a-3p; miR-29b-3p; miR-342-3p; miR-520h | Up-regulation | 0.01; 0.03; 0.03; 0.03; 0.01; 0.02; 0.03; 0.04; 0.008; 0.03 |
| [44] | Case-control | China | Case: 48 Control: 46 | Case: 29.86 ± 0.94 Control: 30.02 ± 0.89 | ND | Placenta | qRT-PCR | miR-657 | Up-regulation | <0.001 |
| [45] | Case-control | China | Case: 30 Control: 29 | Case: 28–40 Control: 29–38 | Case: 37.9 ± 1.1 Control: 39.2 ± 1.1 | Placenta | qRT-PCR | miR-657 | Up-regulation | <0.01 |
| [46] | Case-control | China | Case: 10 Control: 10 | 21–37 Years | ND | Placenta | qRT-PCR | miR-508-3p; miR-27a; miR-9; miR-137; miR-92a; miR-33a; miR-30d; miR-362-5p; miR-502-5p | Up-regulation; down-regulation; down-regulation; down-regulation; down-regulation; down-regulation; down-regulation; down-regulation; down-regulation | <0.01; <0.05; <0.05; <0.05; <0.05; <0.05; <0.05; <0.05; <0.05 |
| [47] | Case-control | Europe | Case: 41 Control: 41 | Case: 32.7 ± 4 Control: 33.2 ± 3.8 | Case: 40 ± 39.3 Control: 40.1 ± 1.1 | Blood | qRT-PCR | miR-16-5p; miR-29a-3p; miR-134-5p | Up-regulation | 0.008; 0.004; 0.046 |
| [48] | Case-control | China | Case: 25 Control: 25 | ND | ND | Blood | qRT-PCR | miR-503 | Up-regulation | <0.01 |
| [49] | Case-control | China | Case: 20 Control: 20 | ND | ND | Blood | qRT-PCR | miR-494 | Down-regulation | <0.01 |
| [50] | Cohort | Italy | Case: 21 Control: 10 | Case: 35.57 ± 5.63 Control: 32.80 ± 5.16 | ND | Blood | qRT-PCR | miR-330-3p | Up-regulation | 0.01 |
| [51] | Cohort | Italy | Case: 12 Control: 12 | Case: 36.4 ± 4.6 Control: 34.9 ± 5.1 | ND | Plasma | qRT-PCR | miR-222-3p; miR-409-3p | Up-regulation | 0.05; 0.01 |
| [52] | Case-control | China | Case: 123 Control: 123 | Case: 31.23 ± 2.31 Control: 30.84 ± 2.95 | Case: 39.35 ± 3.81 Control: 39.52 ± 2.47 | Plasma | qRT-PCR | miR-96-5p | Down-regulation | 0.01 |
| [53] | Case-control | China | Case: 108 Control: 50 | Case: 30.89 ± 3.45 Control: 30.10 ± 2.79 | Case: 25.20 ± 1.23 Control: 25.32 ± 1.45 | Blood and placenta | qRT-PCR | miR-132 | Down-regulation | <0.001 |
| [54] | Case-control | Egypt | Case: 109 Control: 103 | Case: 29.9 ± 6.28 Control: 29.7 ± 5.85 | ND | Blood | qRT-PCR | miR-223 | Up-regulation | <0.001 |
| [55] | Case-control | China | Case: 13 Control: 13 | Case: 27.62 ± 3.10 Control: 27.85 ± 3.36 | ND | Adipose tissue | qRT-PCR | miR-222 | Up-regulation | <0.01 |
| [56] | Case-control | China | Case: 30 Control: 26 | Case: 27.6 Control: 26.9 | ND | Blood | qRT-PCR | miR-214 | Down-regulation | <0.05 |
| [57] | Case-control | China | Case: 204 Control: 202 | Case: 30.91 ± 0.38 Control: 29.68 ± 0.53 | Case: 271.68 ± 11.47 Control: 274.37 ± 8.10 (days) | Placenta | qRT-PCR | miR-29b | Down-regulation | <0.05 |
| [58] | Case-control | Spain and Italy | Case: 23 Control: 20 | Case: 34.0 (32.5–37.5) Control: 34.5 (32.0–37.2) | Case: 40.3 (38.4–40.7) Control: 39.9 (39.4–40.7) | Plasma | qRT-PCR | miR-223; miR-23a | Up-regulation | 1.4 × 10−7; 0.019 |
| [59] | Case-control | China | Case: 30 Control: 30 | ND | ND | Blood | qRT-PCR | miR-770-5p | Up-regulation | <0.01 |
| [60] | Case-control | China | Case: 32 Control: 48 | Case: 32.71 ± 5.26 Control: 29.13 ± 4.22 | Case: 28.33 ± 2.81 Control: 29.10 ± 2.32 | Blood | qRT-PCR | miR-520h | Up-regulation | <0.001 |
| [61] | Case-control | China | Case: 5 Control: 5 | ND | ND | Placenta | qRT-PCR | miR-9-5p | Down-regulation | <0.01 |
| [62] | Case-control | South Africa | Case: 28 Control: 53 | Case: 29.5 ± 6.2 Control: 28.6 ± 6.4 | ND | Blood | qRT-PCR | miR-20a-5p; miR-222-3p | Down-regulation | 0.038; 0.027 |
| [63] | Case-control | China | Case: 12 Control: 12 | ND | ND | Blood | qRT-PCR | miR-33a-5p | Up-regulation | <0.01 |
| [64] | Case-control | China | Case: 112 Control: 58 | Case: 31.59 ± 3.93 Control: 31.14 ± 3.94 | Case: 24.85 ± 1.69 Control: 24.47 ± 2.15 | Blood and placenta | qRT-PCR | miR-136 | Up-regulation | <0.001 |
| [65] | Case-control | China | Case: 166 Control: 196 | Case: 31.03 ± 3.63 Control: 29.70 ± 3.83 | ND | Placenta | qRT-PCR | miR-30d-5p | Down-regulation | <0.01 |
| [66] | Case-control | China | Case: 102 Control:102 | Case: 29.8 ± 3.2 Control: 29.5 ± 2.8 | Case: 27.0 ± 1.6 Control: 26.8 ± 1.1 | Blood | qRT-PCR | miR-195-5p | Up-regulation | <0.01 |
| [67] | Case-control | China | Case: 193 Control: 202 | Case: 30.93 ± 3.45 Control: 29.68 ± 3.66 | Case: 272.22 ± 6.39 Control: 274.41 ± 8.03 (days) | Placenta | qRT-PCR | miR-98 | Up-regulation | <0.05 |
| [68] | Case-control | China | Case: 85 Control: 72 | Case: 26.8 ± 3.5 Control: 26.4 ± 3.6 | Case: 25.8 ± 2.5 Control: 26.1 ± 1.2 | Blood | qRT-PCR | miR-16-5p; miR-17-5p; miR-20a-5p | Up-regulation | <0.01 |
| [69] | Case-control | China | Case: 53 Control: 46 | Case: 29.8 ± 0.4 Control: 29.2 ± 0.6 | Case: 39.9 ± 0.1 Control: 39.0 ± 0.2 | Blood | qRT-PCR | miR-574-5p; miR-3135b | Down-regulation | <0.0001; 0.002 |
| [70] | Case-control | Mexico | Case: 27 Control: 34 | Case: 29.93 ± 6.03 Control: 26.06 ± 5.28 | ND | Urine (urinary exosome) | qRT-PCR | miR-516-5p; miR-517-3p; miR-518-5p; miR-222-3p; miR-16-5p | Down-regulation; down-regulation; down-regulation; down-regulation; up-regulation | <0.05; <0.05; <0.01; <0.01; <0.01 |
| [71] | Case-control | China | Case: 11 Control: 12 | Case: 29.91 ± 1.385 Control: 29.08 ± 1.305 | ND | Blood | qRT-PCR | miR-137 | Up-regulation | 0.0073 |
| [72] | Case-control | Estonia | Case: 13 Control: 9 | Case: 31.1 ± 4.2 Control: 28.1 ± 4.5 | 23–31 weeks | Blood | qRT-PCR | let-7e-5p; let-7g-5p; miR-100-5p; miR-101-3p; miR-146a-5p; miR-195-5p; miR-222-3p; miR-23b-3p; miR-30b-5p; miR-30c-5p; miR-30d-5p; miR-342-3p; miR-423-5p | Up-regulation | 0.03; 0.01; 0.04; 0.03; 0.03; 0.03; 0.03; 0.02; 0.04; 0.02; 0.03; 0.04; 0.02 |
| [73] | Case-control | Iran | Case: 30 Control: 30 | ND | ND | Plasma | qRT-PCR | miR-135a | Down-regulation | 0.001 |
| [74] | Case-control | China | Case: 5 Control: 5 | ND | ND | Placenta | qRT-PCR | miR-190b | Up-regulation | <0.001 |
| Reference | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| [20] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [21] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [22] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [23] 3 | Y | Y | Y | Y | N | NA | Y | Y | NA | NA | NA |
| [24] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [25] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [26] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [27] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [28] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [29] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [30] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [31] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [32] 2 | Y | Y | Y | N | NA | Y | Y | Y | Y | Y | Y |
| [33] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [34] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [35] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [36] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [37] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [38] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [39] 2 | Y | Y | Y | N | NA | Y | Y | Y | Y | Y | Y |
| [40] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [41] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [42] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [43] 2 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| [44] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [45] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [46] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [47] 2 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| [48] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [49] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [50] 2 | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| [51] 2 | Y | Y | Y | N | NA | Y | Y | Y | Y | Y | Y |
| [52] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [53] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [54] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [55] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [56] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [57] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [58] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [59] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [60] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [61] 1 | Y | N | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [62] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [63] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [64] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [65] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [66] 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | NA |
| [67] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [68] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [69] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [70] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [71] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [72] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [73] 1 | Y | N | Y | Y | Y | N | NA | Y | Y | Y | NA |
| [74] 1 | Y | Y | Y | Y | Y | N | NA | Y | Y | Y | NA |
| miRNA | Role/Biological Function | Regulation | Reference |
|---|---|---|---|
| let-7e-5p | Osteoblast differentiation and bone formation | ↑ | [72] |
| let-7g-5p | Inhibit mammary cell proliferation | ↑ | [72] |
| miR-7-5p | Regulates insulin sensitivity | ↑ | [36] |
| miR-9 | Mammalian neuronal development and function | ↓ | [46] |
| miR-9-5p | Regulation of aerobic glycolysis and mitochondrial complex expression | ↓ | [61] |
| miR-16-5p | It targets insulin receptor substrate (IRS) proteins 1 and 2 and mediates insulin-like growth factor-I (IGF-I), which is closely related to insulin resistance | ↑ | [40,47,68,70] |
| miR-17 | Anti-diabetic activity by the anti-inflammation effect on macrophage | ↓ | [29] |
| miR-17-5p | Improves insulin and blood glucose metabolic imbalances | ↑ | [40,68] |
| miR-19a | Promotes cell proliferation and angiogenesis by regulating the PI3K/AKT pathway, known as insulin signaling pathway | ↑ | [42] |
| miR-19a-3p | Regulates insulin secretion while it suppresses the apoptosis of pancreatic β cells | ↑ | [40] |
| miR-19b | Regulates cells apoptosis | ↑ | [42] |
| miR-19b-3p | Regulates the immune and nervous system | ↑ | [40] |
| miR-20a-5p | Improves glucose uptake and relieves diabetic cardiac hypertrophy, fibrosis, inflammation, and apoptosis | ↑ | [40,68] |
| ↓ | [62] | ||
| miR-21 | Keeps glucose levels down in patients with diabetic complications | ↓ | [25] |
| miR-21-3p | Regulates the healing process of diabetic lesions | ↓ | [30] |
| ND | [32] | ||
| miR-23a | Regulates the inflammatory response | ↑ | [58] |
| miR-23b-3p | Promotes high glucose-induced cellular metabolic memory in diabetic retinopathy | ↑ | [72] |
| miR-27a | Promotes insulin resistance | ↓ | [46] |
| miR-29a | Acts as an important regulator of insulin-stimulated glucose metabolism | ↓ | [26,41] |
| miR-29a-3p | Regulator of insulin-like growth factor 1 receptor | ↑ | [43,47] |
| miR-29b | Regulates aortic remodeling and stiffening in diabetes | ↓ | [26,57] |
| miR-29b-3p | Promotes cell proliferation, apoptosis, fibrosis, and inflammation | ↑ | [43] |
| miR-30b-5p | Induces abnormal angiogenesis | ↑ | [72] |
| miR-30c-5p | Induces macrophage-mediated inflammation and pro-atherosclerosis signal pathways | ↑ | [72] |
| miR-30d | Induces insulin production | ↓ | [46] |
| miR-30d-5p | Regulates human chorionic trophoblast cell proliferation, migration, and glucose uptake capacity | ↑ | [72] |
| ↓ | [65] | ||
| miR-33a | Regulates the insulin signaling pathway and glucose metabolism | ↓ | [46] |
| miR-33a-5p | Related to decreased cell growth (β cell) and insulin production | ↑ | [63] |
| miR-92a | Modulation of vascular homeostasis | ↓ | [46] |
| miR-96-5p | Relieves the antiproliferative effects induced by high glucose conditions on trophoblasts | ↓ | [52] |
| miR-98 | Protects nucleus pulposus cells against apoptosis | ↑ | [67] |
| miR-100-5p | Promotes angiogenesis during the implantation process | ↑ | [72] |
| miR-101-3p | Associated with insulin production, survival, and death of pancreatic β cells | ↑ | [72] |
| miR-122-5p | Suppresses insulin resistance | ↑ | [43] |
| miR-125b | Modulates insulin secretion | ↑ | [23] |
| miR-132 | Promote the trophoblast cell proliferation | ↓ | [41,53] |
| miR-132-3p | Related to insulin resistance and β cell function | ↑ | [43] |
| miR-134-5p | Regulate trophoblast cell behaviors in preeclampsia, such as apoptosis, migration, and invasion | ↑ | [20,47] |
| miR-135a | Related to the proliferation and migration of cells | ↓ | [73] |
| miR-136 | Relieves inhibited cell viability induced by high glucose treatment | ↑ | [64] |
| miR-136-5p | Related to cellular proliferation, migration, and invasion | ↑ | [43] |
| miR-137 | Participates in the interaction between endothelial cells and monocytes | ↑ | [71] |
| ↓ | [46] | ||
| miR-140-3p | Important regulator of osteoblastogenesis | ↑ | [27] |
| miR-144 | Regulates proliferation and apoptosis | ↑ | [23] |
| miR-146a-5p | Inhibit the inflammatory response and apoptosis | ↑ | [72] |
| miR-155-5p | Promotes fibrosis of proximal tubule cells | ↓ | [33] |
| ND | [32] | ||
| miR-181d | Modulates the process of insulin signaling, cell viability, and apoptosis in pancreatic β cells | ↑ | [35] |
| miR-182-3p | Related to vascular smooth muscle cells proliferation and migration | ↑ | [43] |
| miR-190b | Inhibits pancreatic β cell proliferation and insulin secretion | ↑ | [74] |
| miR-193b | Suppresses apoptosis and autophagy | ↓ | [37] |
| miR-195 | Increases epithelial-mesenchymal transition and cell permeability | ↑ | [29] |
| miR-195-5p | Relates to cell viability and proliferation, and apoptosis | ↑ | [66,72] |
| miR-210-3p | Reduces cell viability and promotes apoptosis of pancreatic β cells | ↑ | [43] |
| miR-214 | Involved in cellular immune response, regulating cell activation, proliferation, and differentiation | ↓ | [56] |
| miR-222 | Regulates estrogen receptor (ER) and glucose transporter 4 (GLUT4) | ↑ | [55] |
| ↓ | [41] | ||
| miR-222-3p | Relates to glucose metabolism in pregnancy | ↑ | [51,72] |
| ↓ | [62,70] | ||
| miR-223 | Modulator of human myeloid differentiation | ↑ | [54,58] |
| miR-257 | ND | ↑ | [29] |
| miR-330-3p | Involved in insulin secretion and β cell growth and proliferation, activating proteins involved in cell cycle and cell growth | ↑ | [28,39,50] |
| miR-340 | Associated with induced hyperinsulinemia | ↑ | [31] |
| miR-342-3p | Induction of vascular dysfunction | ↑ | [43,72] |
| miR-345-3p | Regulates cell growth, apoptosis, migration, and invasion | ↓ | [24] |
| miR-362-5p | Promotes cell proliferation and inhibition of apoptosis | ↓ | [46] |
| miR-377-3p | Regulates VEGF expression | ↑ | [34] |
| miR-409-3p | Relates to immune dysregulation in autoimmune diabetes | ↑ | [51] |
| miR-409-5p | Correlated with insulin resistance | ↑ | [38] |
| miR-423-5p | Relieves high glucose-mediated podocyte injuries | ↑ | [72] |
| miR-494 | Decreased insulin secretion and cell proliferation, and increased apoptosis | ↓ | [49] |
| miR-502-5p | Mediates insulin resistance | ↓ | [46] |
| miR-503 | Impairs restorative angiogenesis | ↑ | [48] |
| miR-508-3p | Promotes cell proliferation and inhibits apoptosis | ↑ | [46] |
| miR-516-5p | Inhibits cell proliferation | ↓ | [70] |
| miR-517-3p | Promotes trophoblast dysfunction | ↓ | [70] |
| miR-518-5p | Increases hypoxia-induced vascular endothelial cell damage | ↓ | [70] |
| miR-520h | Inhibit cell viability and promote cell apoptosis | ↑ | [43,60] |
| miR-543 | Regulates high glucose-induced fibrosis and autophagy | ↑ | [23] |
| miR-574-5p | Metabolic regulator for serum lipids and blood glucose | ↓ | [69] |
| miR-657 | Promotes macrophage polarization | ↑ | [44,45] |
| miR-770-5p | Inhibits cell proliferation and promotes apoptosis | ↑ | [59] |
| miR-1323 | Promotes the trophoblast cell viability under high glucose conditions | ↑ | [22,43] |
| miR-3135b | Metabolic regulator for serum lipids and blood glucose | ↓ | [69] |
| miR-6869-5p | Involved in maintaining the microenvironmental balance of the placenta | ↓ | [21] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, P.H.C.M.; Santos, K.d.F.; da Silva, L.; da Costa, C.C.P.; Santos, R.d.S.; Reis, A.A.d.S. MicroRNAs Associated with the Pathophysiological Mechanisms of Gestational Diabetes Mellitus: A Systematic Review for Building a Panel of miRNAs. J. Pers. Med. 2023, 13, 1126. https://doi.org/10.3390/jpm13071126
da Silva PHCM, Santos KdF, da Silva L, da Costa CCP, Santos RdS, Reis AAdS. MicroRNAs Associated with the Pathophysiological Mechanisms of Gestational Diabetes Mellitus: A Systematic Review for Building a Panel of miRNAs. Journal of Personalized Medicine. 2023; 13(7):1126. https://doi.org/10.3390/jpm13071126
Chicago/Turabian Styleda Silva, Pedro Henrique Costa Matos, Kamilla de Faria Santos, Laura da Silva, Caroline Christine Pincela da Costa, Rodrigo da Silva Santos, and Angela Adamski da Silva Reis. 2023. "MicroRNAs Associated with the Pathophysiological Mechanisms of Gestational Diabetes Mellitus: A Systematic Review for Building a Panel of miRNAs" Journal of Personalized Medicine 13, no. 7: 1126. https://doi.org/10.3390/jpm13071126
APA Styleda Silva, P. H. C. M., Santos, K. d. F., da Silva, L., da Costa, C. C. P., Santos, R. d. S., & Reis, A. A. d. S. (2023). MicroRNAs Associated with the Pathophysiological Mechanisms of Gestational Diabetes Mellitus: A Systematic Review for Building a Panel of miRNAs. Journal of Personalized Medicine, 13(7), 1126. https://doi.org/10.3390/jpm13071126






