Predictive Performance of Scoring Systems for Mortality Risk in Patients with Cryptococcemia: An Observational Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection and Definition
2.2. Scoring Systems
2.3. Statistical Analysis
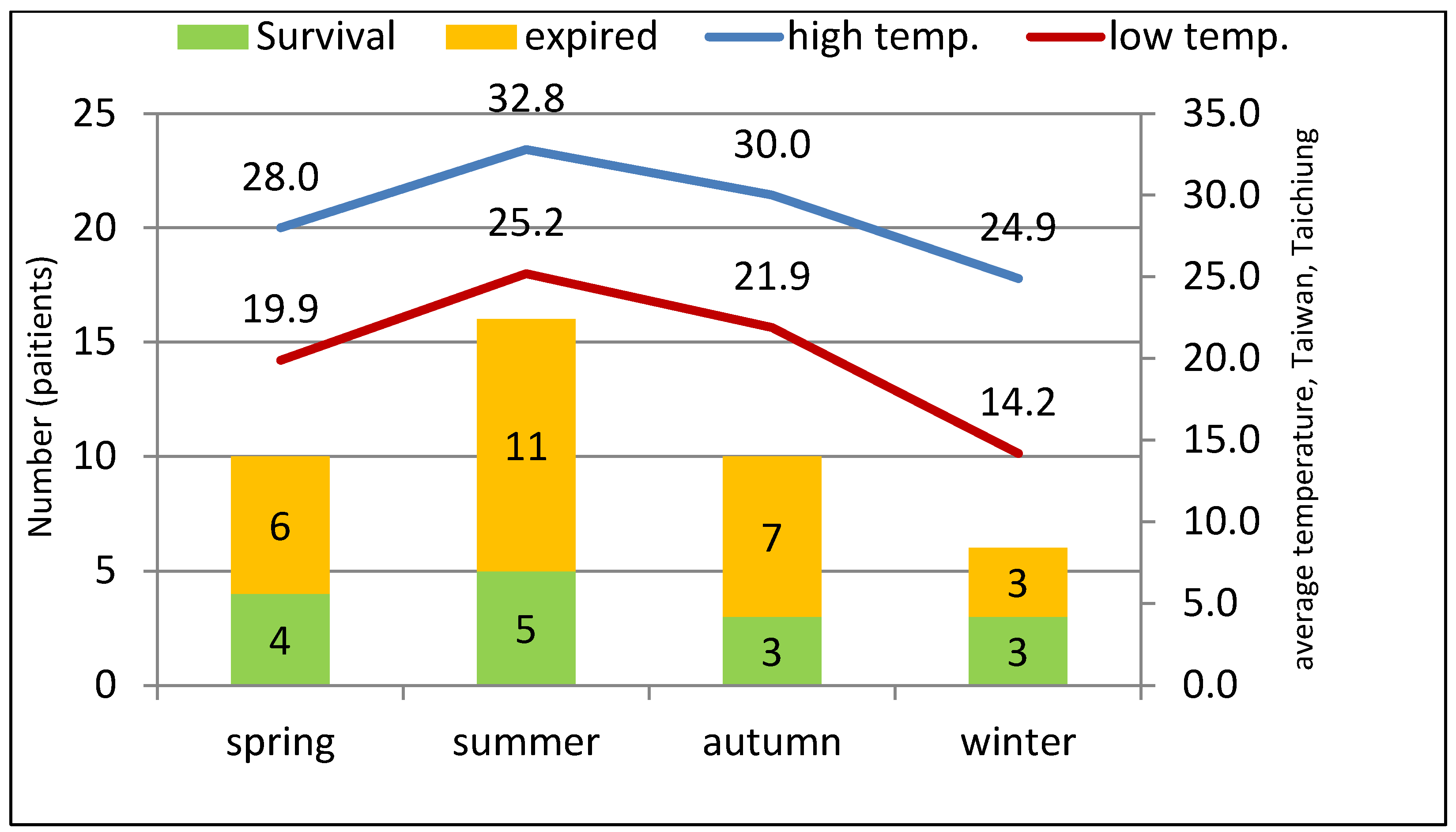
3. Results
3.1. Demographics and Clinical Characteristics
3.2. Laboratory Data and Scoring Systems
3.3. Microbiology
3.4. Clinical Outcomes and Co-Infections Related to Other Pathogens
3.5. Univariate and Multivariate Analysis of Risk Factors
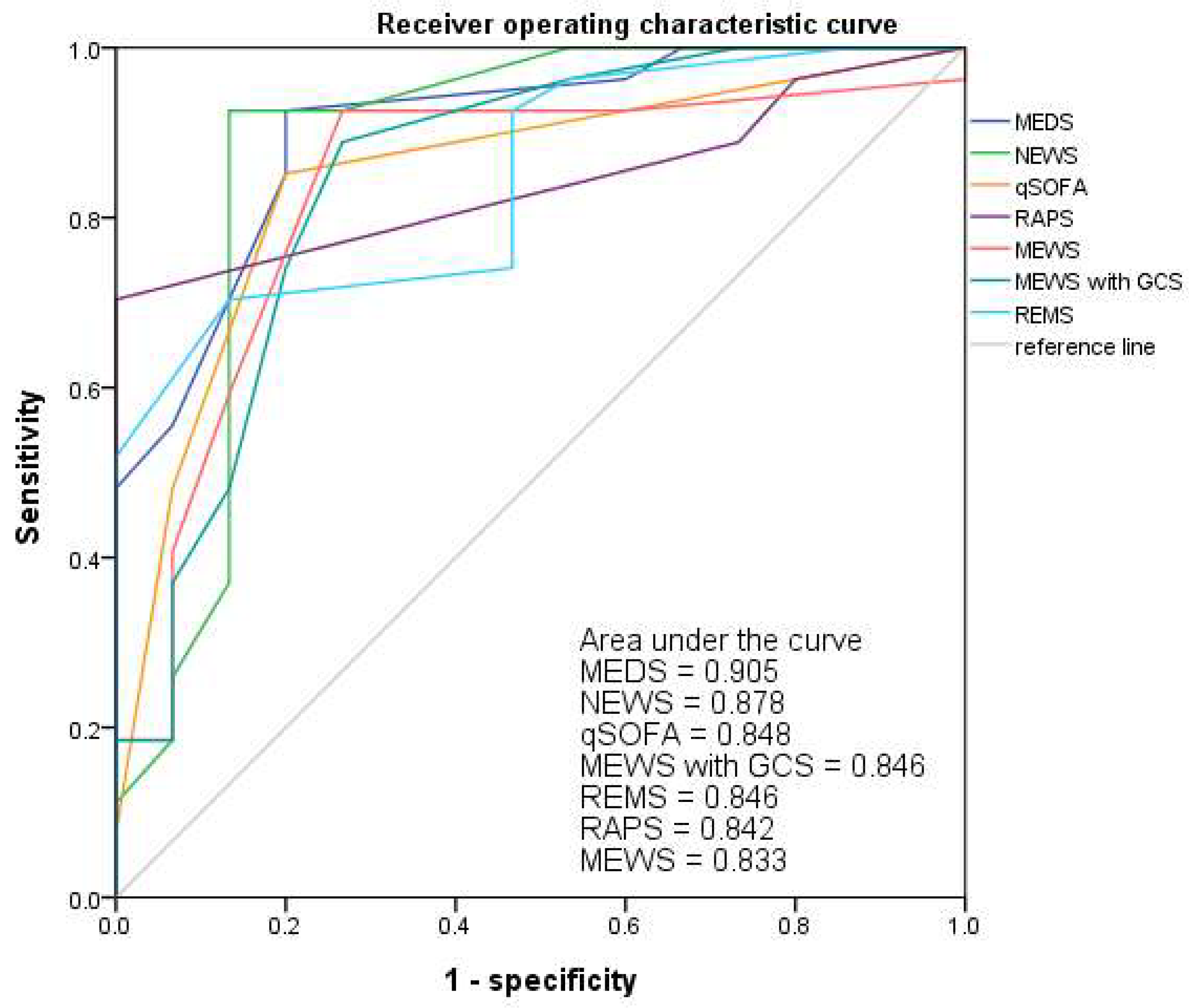
3.6. Receiver Operating Characteristic Curve (ROC)
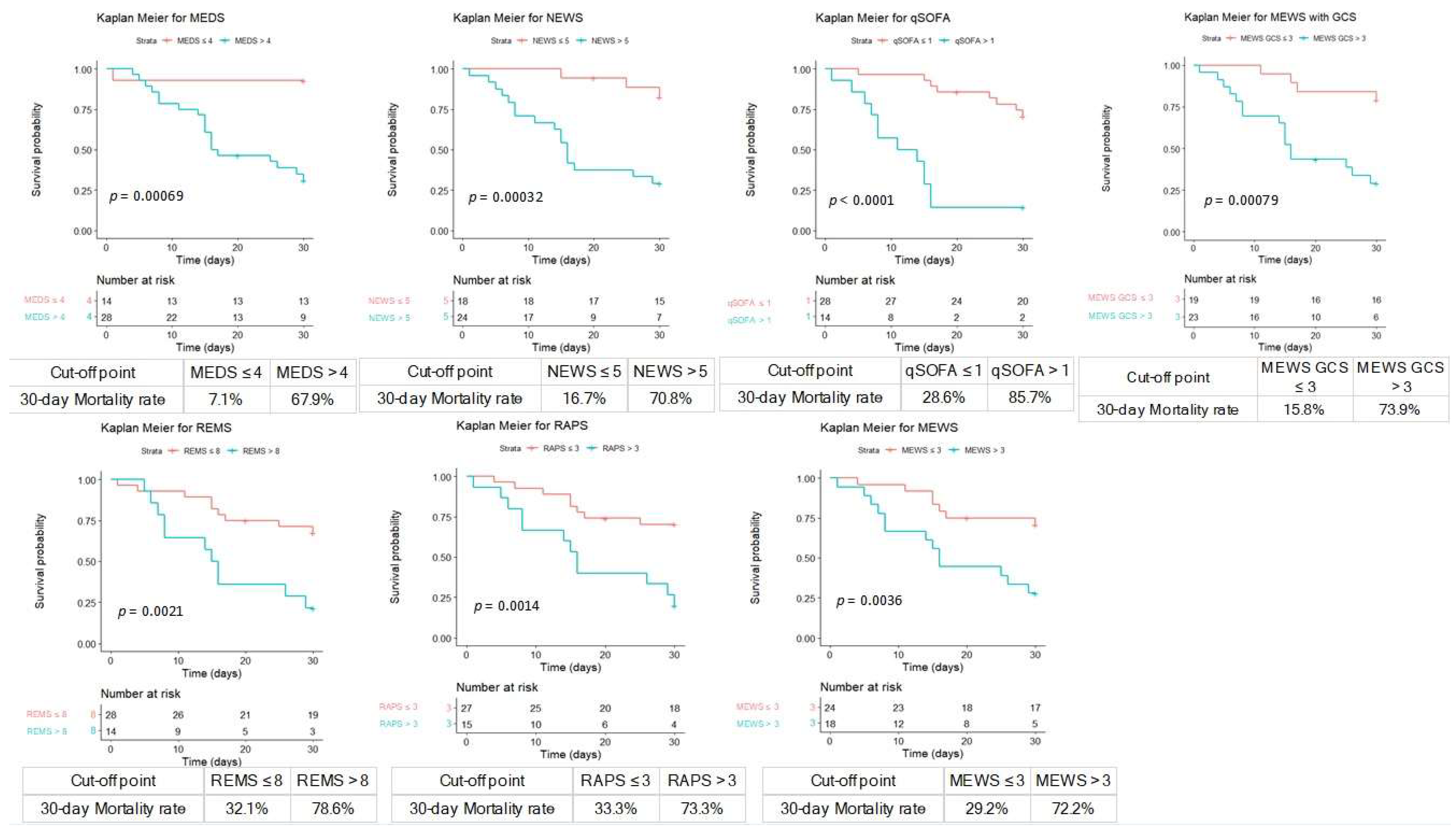
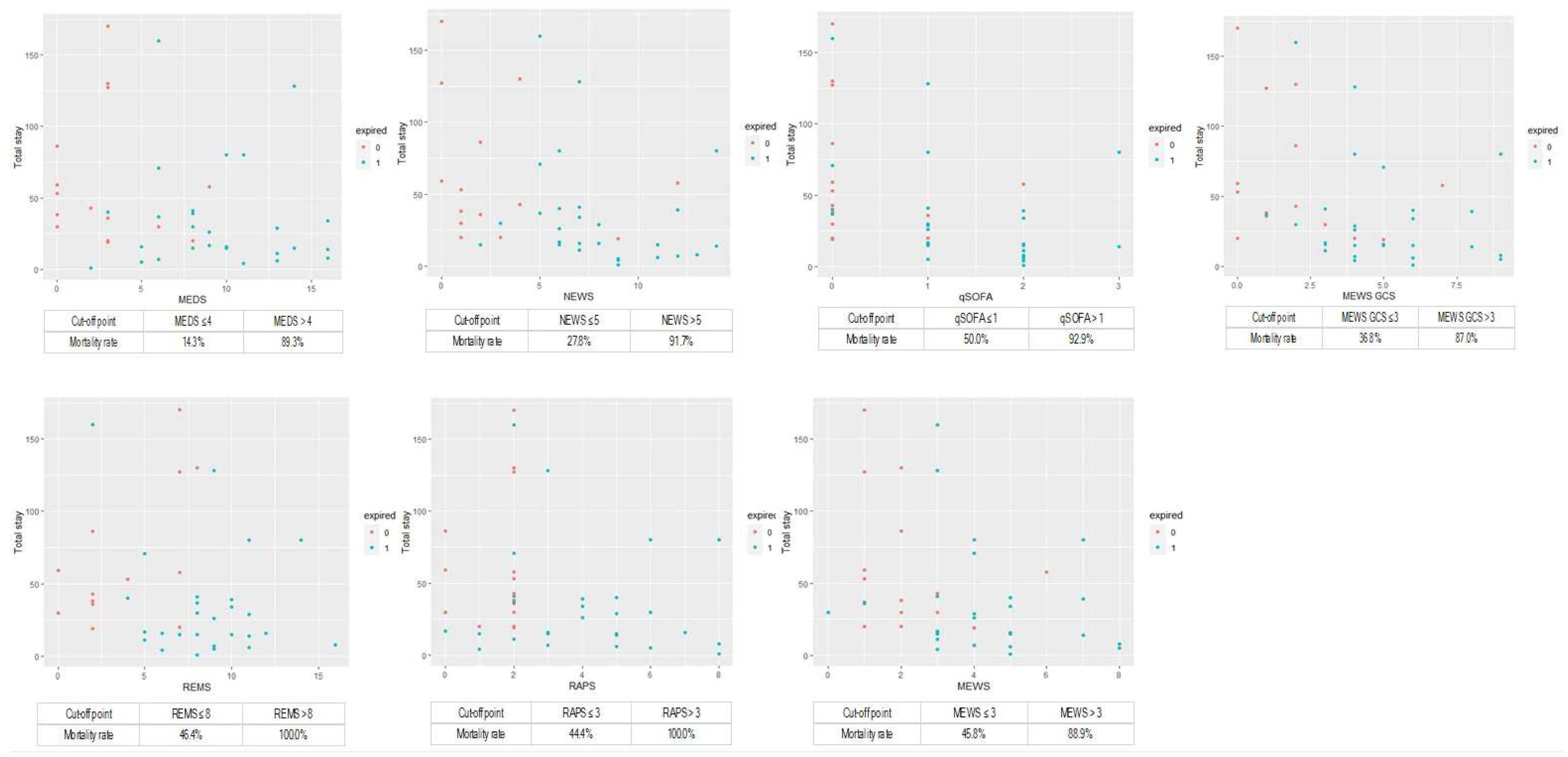
3.7. Cumulative Survival Rates Using Kaplan–Meier and Discrimination Plots
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maziarz, E.K.; Perfect, J.R. Cryptococcosis. Infect. Dis. Clin. N. Am. 2016, 30, 179–206. [Google Scholar] [CrossRef]
- Bicanic, T.; Harrison, T.S. Cryptococcal meningitis. Br. Med. Bull. 2005, 72, 99–118. [Google Scholar] [CrossRef]
- Kidd, S.E.; Hagen, F.; Tscharke, R.L.; Huynh, M.; Bartlett, K.H.; Fyfe, M.; Macdougall, L.; Boekhout, T.; Kwon-Chung, K.J.; Meyer, W. A rare genotype of Cryptococcus gattii caused the cryptococcosis outbreak on Vancouver Island (British Columbia, Canada). Proc. Natl. Acad. Sci. USA 2004, 101, 17258–17263. [Google Scholar] [CrossRef]
- Williamson, P.R.; Jarvis, J.N.; Panackal, A.A.; Fisher, M.C.; Molloy, S.F.; Loyse, A.; Harrison, T.S. Cryptococcal meningitis: Epidemiology, immunology, diagnosis and therapy. Nat. Rev. Neurol. 2017, 13, 13–24. [Google Scholar] [CrossRef]
- Rajasingham, R.; Smith, R.M.; Park, B.J.; Jarvis, J.N.; Govender, N.P.; Chiller, T.M.; Denning, D.W.; Loyse, A.; Boulware, D.R. Global burden of disease of HIV-associated cryptococcal meningitis: An updated analysis. Lancet Infect. Dis. 2017, 17, 873–881. [Google Scholar] [CrossRef]
- Chang, C.C.; Sorrell, T.C.; Chen, S.C. Pulmonary Cryptococcosis. Semin. Respir. Crit. Care Med. 2015, 36, 681–691. [Google Scholar] [CrossRef]
- Setianingrum, F.; Rautemaa-Richardson, R.; Denning, D.W. Pulmonary cryptococcosis: A review of pathobiology and clinical aspects. Med. Mycol. 2019, 57, 133–150. [Google Scholar] [CrossRef]
- Sobel, J.D.; Vazquez, J.A. Fungal infections of the urinary tract. World J. Urol. 1999, 17, 410–414. [Google Scholar] [CrossRef]
- Noguchi, H.; Matsumoto, T.; Kimura, U.; Hiruma, M.; Kusuhara, M.; Ihn, H. Cutaneous Cryptococcosis. Med. Mycol. J. 2019, 60, 101–107. [Google Scholar] [CrossRef]
- Dumenigo, A.; Sen, M. Cryptococcal Osteomyelitis in an Immunocompetent Patient. Cureus 2022, 14, e21074. [Google Scholar] [CrossRef]
- Zainal, A.I.; Wong, S.L.; Pan, K.L.; Wong, O.L.; Tzar, M.N. Cryptococcal osteomyelitis of the femur: A case report and review of literature. Trop. Biomed. 2011, 28, 444–449. [Google Scholar] [PubMed]
- Amphornphruet, A.; Silpa-Archa, S.; Preble, J.M.; Foster, C.S. Endogenous Cryptococcal Endophthalmitis in Immunocompetent Host: Case Report and Review of Multimodal Imaging Findings and Treatment. Ocul. Immunol. Inflamm. 2018, 26, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Sheu, S.J.; Chen, Y.C.; Kuo, N.W.; Wang, J.H.; Chen, C.J. Endogenous cryptococcal endophthalmitis. Ophthalmology 1998, 105, 377–381. [Google Scholar]
- Jean, S.S.; Wang, J.L.; Wang, J.T.; Fang, C.T.; Chen, Y.C.; Chang, S.C. Cryptococcus neoformans peritonitis in two patients with liver cirrhosis. J. Formos. Med. Assoc. 2005, 104, 39–42. [Google Scholar]
- Gushiken, A.C.; Saharia, K.K.; Baddley, J.W. Cryptococcosis. Infect. Dis. Clin. N. Am. 2021, 35, 493–514. [Google Scholar] [CrossRef]
- Chen, Y.C.; Chang, S.C.; Shih, C.C.; Hung, C.C.; Luhbd, K.T.; Pan, Y.S.; Hsieh, W.C. Clinical features and in vitro susceptibilities of two varieties of Cryptococcus neoformans in Taiwan. Diagn. Microbiol. Infect. Dis. 2000, 36, 175–183. [Google Scholar] [CrossRef]
- Archibald, L.K.; McDonald, L.C.; Rheanpumikankit, S.; Tansuphaswadikul, S.; Chaovanich, A.; Eampokalap, B.; Banerjee, S.N.; Reller, L.B.; Jarvis, W.R. Fever and human immunodeficiency virus infection as sentinels for emerging mycobacterial and fungal bloodstream infections in hospitalized patients >/=15 years old, Bangkok. J. Infect. Dis. 1999, 180, 87–92. [Google Scholar] [CrossRef]
- Jean, S.S.; Fang, C.T.; Shau, W.Y.; Chen, Y.C.; Chang, S.C.; Hsueh, P.R.; Hung, C.C.; Luh, K.T. Cryptococcaemia: Clinical features and prognostic factors. QJM 2002, 95, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Pasqualotto, A.C.; BittencourtSevero, C.; de Mattos Oliveira, F.; Severo, L.C. Cryptococcemia. An analysis of 28 cases with emphasis on the clinical outcome and its etiologic agent. Rev. Iberoam. Micol. 2004, 21, 143–146. [Google Scholar] [PubMed]
- Fu, Y.; Xu, M.; Zhou, H.; Yao, Y.; Zhou, J.; Pan, Z. Microbiological and clinical characteristics of cryptococcemia: A retrospective analysis of 85 cases in a Chinese hospital. Med. Mycol. 2020, 58, 478–484. [Google Scholar] [CrossRef]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Raith, E.P.; Udy, A.A.; Bailey, M.; McGloughlin, S.; MacIsaac, C.; Bellomo, R.; Pilcher, D.V.; Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality Among Adults With Suspected Infection Admitted to the Intensive Care Unit. JAMA 2017, 317, 290–300. [Google Scholar] [CrossRef]
- Rhee, K.J.; Fisher, C.J., Jr.; Willitis, N.H. The rapid acute physiology score. Am. J. Emerg. Med. 1987, 5, 278–282. [Google Scholar] [CrossRef] [PubMed]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM 2001, 94, 521–526. [Google Scholar] [CrossRef]
- Smith, G.B.; Prytherch, D.R.; Meredith, P.; Schmidt, P.E.; Featherstone, P.I. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013, 84, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Olsson, T.; Terent, A.; Lind, L. Rapid Emergency Medicine score: A new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J. Intern. Med. 2004, 255, 579–587. [Google Scholar] [CrossRef]
- Hsieh, C.C.; Yang, C.Y.; Lee, C.H.; Chi, C.H.; Lee, C.C. Validation of MEDS score in predicting short-term mortality of adults with community-onset bacteremia. Am. J. Emerg. Med. 2020, 38, 282–287. [Google Scholar] [CrossRef]
- Huang, S.H.; Hsieh, M.S.; Hu, S.Y.; Huang, S.C.; Tsai, C.A.; Hsu, C.Y.; Lin, T.C.; Lee, Y.C.; Liao, S.H. Performance of Scoring Systems in Predicting Clinical Outcomes in Patients with Bacteremia of Listeria monocytogenes: A 9-Year Hospital-Based Study. Biology 2021, 10, 1073. [Google Scholar] [CrossRef]
- Doering, T.L. A unique α-1,3 mannosyltransferase of the pathogenic fungus Cryptococcus neoformans. J. Bacteriol. 1999, 181, 5482–5488. [Google Scholar] [CrossRef] [PubMed]
- Pettit, R.K.; Repp, K.K.; Hazen, K.C. Temperature affects the susceptibility of Cryptococcus neoformans biofilms to antifungal agents. Med. Mycol. 2010, 48, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Serna-Espinosa, B.N.; Guzmán-Sanabria, D.; Forero-Castro, M.; Escandón, P.; Sánchez-Quitian, Z.A. Environmental status of Cryptococcus neoformans and Cryptococcus gattii in Colombia. J. Fungi 2021, 7, 410. [Google Scholar] [CrossRef] [PubMed]
- Perfect, J.R.; Dismukes, W.E.; Dromer, F.; Goldman, D.L.; Graybill, J.R.; Hamill, R.J.; Harrison, T.S.; Larsen, R.A.; Lortholary, O.; Nguyen, M.H.; et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2010, 50, 291–322. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Zhang, K.; Zheng, X.; Cui, W.; Hong, Y.; Zhang, Z. Performance of the MEDS score in predicting mortality among emergency department patients with a suspected infection: A meta-analysis. Emerg. Med. J. 2020, 37, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, N.I.; Wolfe, R.E.; Moore, R.B.; Smith, E.; Burdick, E.; Bates, D.W. Mortality in Emergency Department Sepsis (MEDS) score: A prospectively derived and validated clinical prediction rule. Crit. Care Med. 2003, 31, 670–675. [Google Scholar] [CrossRef]
| General Data | Patients (n = 42) | Survivors (n = 15) | Non-Survivors (n = 27) | p-Value |
|---|---|---|---|---|
| Age (years) | 63.0 ± 19.7 | 52.5 ± 19.7 | 68.9 ± 17.4 | 0.014 * |
| Male (%) | 28 (66.7%) | 12 (80%) | 16 (59.3%) | 0.172 |
| Hospital stays (days) | 44.4 ± 42.9 | 61.3 ± 46.5 | 35.0 ± 38.5 | 0.008 ** |
| Focus of cryptococcosis | ||||
| CNS f | 22 (52.4%) | 11 (73.3%) | 11 (40.7%) | 0.009 ** |
| Respiratory tract f | 4 (9.5%) | 2 (13.3%) | 2 (7.4%) | 0.608 |
| Clinical conditions | ||||
| Septic shock f | 7 (16.7%) | 0 (0.0%) | 7 (25.9%) | 0.038 * |
| IICP f | 18 (42.9%) | 8 (53.3%) | 10 (37.0%) | 0.007 ** |
| Concomitant infections | ||||
| Pneumonia | 16 (38.1%) | 5 (33.3%) | 11 (40.7%) | 0.746 |
| Urinary tract f | 8 (19.1%) | 2 (13.3%) | 6 (22.2%) | 0.689 |
| Bacteremia | 21 (50.0%) | 7 (46.7%) | 14 (51.9%) | 1 |
| Comorbidities | ||||
| HIV f | 8 (19.1%) | 6 (40.0%) | 2 (7.4%) | 0.016 * |
| Liver cirrhosis f | 6 (14.3%) | 1 (6.7%) | 5 (18.5%) | 0.395 |
| ESRD f | 5 (11.9%) | 0 (0.0%) | 5 (18.5%) | 0.142 |
| DM f | 6 (14.3%) | 1 (6.7%) | 5 (18.5%) | 0.395 |
| Immunosuppressant use | 16 (38.1%) | 5 (33.3%) | 11 (40.7%) | 0.746 |
| Under chemotherapy f | 4 (9.5%) | 1 (6.7%) | 3 (11.1%) | 1 |
| Vital signs | ||||
| SBP (mmHg) | 134.6 ± 26.8 | 136.8 ± 20.1 | 133.4 ± 30.2 | 0.763 |
| DBP (mmHg) | 80.6 ± 19.4 | 79.9 ± 12.6 | 81.0 ± 22.5 | 0.937 |
| MAP (mmHg) | 98.6 ± 20.5 | 98.8 ± 13.5 | 98.4 ± 23.7 | 1 |
| HR (bpm) | 97.4 ± 25.5 | 96.2 ± 18.5 | 98.0 ± 29.0 | 0.636 |
| RR (bpm) | 20.1 ± 3.7 | 18.5 ± 1.6 | 20.9 ± 4.3 | 0.022 * |
| BT (°C) | 37.7 ± 0.9 | 37.7 ± 1.2 | 37.7 ± 0.8 | 0.590 |
| SpO2 (%) | 95.6 ± 5.4 | 96.1 ± 2.6 | 95.3 ± 6.5 | 0.355 |
| O2 use | 26 (61.9%) | 3 (20.0%) | 23 (85.2%) | <0.001 ** |
| GCS | 11.6 ± 4.2 | 14.6 ± 1.1 | 10.0 ± 4.4 | <0.001 ** |
| Laboratory data | ||||
| WBC (counts/uL) | 9312.9 ± 6707.0 | 7026.0 ± 5071.7 | 10,583.3 ± 7238.2 | 0.125 |
| Hb (g/dL) | 10.1 ± 2.4 | 11.0 ± 1.6 | 9.5 ± 2.6 | 0.021 * |
| PLT (×103 counts/uL) | 170.2 ± 119.0 | 244.7 ± 124.5 | 128.7 ± 94.9 | 0.002 ** |
| Crea (mg/dL) | 1.97 ± 2.17 | 0.96 ± 0.42 | 2.56 ± 2.54 | 0.003 ** |
| Lactate (mg/dL) | 22.1 ± 28.6 | 11.6 ± 4.6 | 25.6 ± 32.3 | 0.104 |
| pH | 7.40 ± 0.07 | 7.42 ± 0.04 | 7.39 ± 0.07 | 0.427 |
| Scoring systems | ||||
| qSOFA | 1.0 ± 0.9 | 0.3 ± 0.6 | 1.4 ± 0.8 | <0.001 ** |
| RAPS | 3.2 ± 2.2 | 1.5 ± 0.8 | 4.1 ± 2.3 | <0.001 ** |
| MEWS | 3.5 ± 2.0 | 2.1 ± 1.4 | 4.3 ± 1.9 | <0.001 ** |
| MEWS with GCS | 3.9 ± 2.6 | 2.0 ± 2.0 | 4.9 ± 2.2 | <0.001 ** |
| REMS | 7.1 ± 3.7 | 4.3 ± 3.0 | 8.6 ± 3.1 | <0.001 ** |
| NEWS | 6.1 ± 4.1 | 2.9 ± 3.4 | 8.0 ± 3.2 | <0.001 ** |
| MEDS | 7.1 ± 4.8 | 2.9 ± 2.9 | 9.5 ± 4.0 | <0.001 ** |
| General Data | Patients (n = 30) | Survivors (n = 15) | Non-Survivors (n = 15) | p-Value |
|---|---|---|---|---|
| Age (years) | 57.5 ± 19.5 | 52.5 ± 19.7 | 62.6 ± 18.7 | 0.106 |
| Male (%) | 23 (76.7%) | 12 (80.0%) | 11 (73.3%) | 1 |
| Hospital stays (days) | 53.5 ± 45.9 | 61.3 ± 46.5 | 45.7 ± 45.5 | 0.116 |
| Focus of cryptococcosis | ||||
| CNS | 22 (73.3%) | 11 (73.3%) | 11 (73.3%) | 1 |
| Respiratory tract | 4 (13.3%) | 2 (13.3%) | 2 (13.3%) | 1 |
| Clinical conditions | ||||
| Septic shock | 2 (6.7%) | 0 (0.0%) | 2 (13.3%) | 0.483 |
| IICP | 18 (60.0%) | 8 (53.3%) | 10 (66.7%) | 0.709 |
| Concomitant infections | ||||
| Pneumonia | 13 (38.1%) | 5 (33.3%) | 8 (53.3%) | 0.461 |
| Urinary tract | 5 (16.7%) | 2 (13.3%) | 3 (20.0%) | 1 |
| Bacteremia | 16 (53.3%) | 7 (46.7%) | 9 (60.0%) | 0.714 |
| Comorbidities | ||||
| HIV | 8 (26.7%) | 6 (40.0%) | 2 (13.3%) | 0.215 |
| Liver cirrhosis | 4 (13.3%) | 1 (6.7%) | 3 (20.0%) | 0.598 |
| ESRD | 2 (6.7%) | 0 (0.0%) | 2 (13.3%) | 0.483 |
| DM | 4 (13.3%) | 1 (6.7%) | 3 (20.0%) | 0.598 |
| Immunosuppressant use | 12 (40.0%) | 5 (33.3%) | 7 (46.7%) | 0.709 |
| Under chemotherapy | 2 (6.6%) | 1 (6.7%) | 1 (6.7%) | 1 |
| Vital signs | ||||
| SBP (mmHg) | 139.2 ± 21.8 | 136.8 ± 20.1 | 141.5 ± 23.9 | 0.567 |
| DBP (mmHg) | 84.4 ± 17.9 | 79.9 ± 12.6 | 88.87 ± 21.4 | 0.217 |
| MAP (mmHg) | 102.6 ± 17.6 | 98.8 ± 13.5 | 106.4 ± 20.6 | 0.267 |
| HR (bpm) | 93.9 ± 24.3 | 96.2 ± 18.5 | 91.5 ± 29.5 | 0.744 |
| RR (bpm) | 19.0 ± 2.6 | 18.5 ± 1.6 | 19.4 ± 3.3 | 0.187 |
| BT (°C) | 37.7 ± 1.1 | 37.7 ± 1.2 | 37.8 ± 1.0 | 0.870 |
| SpO2 (%) | 96.2 ± 2.8 | 96.1 ± 2.6 | 96.3 ± 3.0 | 0.838 |
| O2 use | 14 (46.7%) | 3 (20.0%) | 11 (73.3%) | <0.001 ** |
| GCS | 12.6 ± 4.0 | 14.6 ± 1.1 | 10.5 ± 4.7 | 0.019 * |
| Laboratory data | ||||
| WBC (counts/uL) | 7574.0 ± 4616.7 | 7026.0 ± 5071.7 | 8122.0 ± 4217.2 | 0.412 |
| Hb (g/dL) | 10.4 ± 2.5 | 11.0 ± 1.6 | 9.7 ± 3.0 | 0.098 |
| PLT (×103 counts/uL) | 181.3 ± 124.3 | 244.7 ± 124.5 | 117.9 ± 88.8 | 0.002 |
| Crea (mg/dL) | 1.63 ± 2.10 | 0.96 ± 0.42 | 2.34 ± 2.87 | 0.026 * |
| Lactate (mg/dL) | 14.1 ± 8.8 | 11.6 ± 4.6 | 15.6 ± 10.5 | 0.313 |
| pH | 7.42 ± 0.04 | 7.42 ± 0.04 | 7.41 ± 0.05 | 0.681 |
| Scoring systems | ||||
| qSOFA | 0.6 ± 0.8 | 0.3 ± 0.6 | 1.0 ± 0.8 | 0.011 * |
| RAPS | 2.7 ± 2.1 | 1.5 ± 0.8 | 3.9 ± 2.3 | 0.002 ** |
| MEWS | 2.8 ± 1.6 | 2.1 ± 1.4 | 3.4 ± 1.5 | 0.013 * |
| MEWS GCS | 3.0 ± 2.1 | 2.0 ± 2.0 | 4.1 ± 1.6 | 0.004 ** |
| REMS | 6.0 ± 3.3 | 4.3 ± 3.0 | 7.6 ± 2.8 | 0.005 ** |
| NEWS | 4.4 ± 3.1 | 2.9 ± 3.4 | 5.9 ± 1.8 | 0.001 ** |
| MEDS | 5.5 ± 4.3 | 2.9 ± 2.9 | 8.2 ± 3.8 | <0.001 ** |
| Characteristics | Hazard Ratios | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Age (years) | 1.03 | (1.00–1.06) | 0.023 * |
| Female | 2.45 | (1.11–5.42) | 0.027 * |
| Focus of cryptococcosis | |||
| CNS | 0.36 | (0.16–0.85) | 0.013 * |
| Concomitant infection | |||
| LRTI | 2.59 | (1.15–5.81) | 0.021 * |
| Vital signs | |||
| RR (bpm) | 1.18 | (1.06–1.32) | 0.002 ** |
| GCS | 0.92 | (0.84–0.97) | 0.008 ** |
| Laboratory data | |||
| WBC (counts/uL) | 1.00 | (1.00–1.00) | 0.028 * |
| PLT (×103 counts/uL) | 1.00 | (0.99–1.00) | 0.026 * |
| Crea (mg/dL) | 1.17 | (1.03–1.32) | 0.016 * |
| Lactate (mg/dL) | 1.03 | (1.00–1.05) | 0.004 ** |
| Clinical management | |||
| O2 use | 4.74 | (1.64–13.73) | 0.004 ** |
| Scoring systems | |||
| REMS | 1.18 | (1.06–1.32) | 0.003 ** |
| RAPS | 1.30 | (1.11–1.53) | 0.001 ** |
| MEWS | 1.37 | (1.14–1.66) | 0.001 ** |
| MEWS with GCS | 1.29 | (1.12–1.48) | <0.001 ** |
| MEDS | 1.18 | (1.08–1.28) | <0.001 ** |
| NEWS | 1.19 | (1.09–1.30) | <0.001 ** |
| qSOFA | 2.11 | (1.47–3.02) | <0.001 ** |
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| Variables | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| MEDS | 1.18 | (1.08–1.28) | <0.001 ** | 1.20 | (1.03–1.40) | 0.018 * |
| NEWS | 1.19 | (1.09–1.30) | <0.001 ** | 1.03 | (0.77–1.39) | 0.813 |
| MEWS with GCS | 1.29 | (1.12–1.48) | <0.001 ** | 1.09 | (0.59–2.04) | 0.766 |
| MEWS | 1.37 | (1.14–1.66) | 0.001 ** | 0.84 | (0.40–1.75) | 0.647 |
| RAPS | 1.30 | (1.11–1.53) | 0.001 ** | 1.24 | (0.88–1.74) | 0.211 |
| REMS | 1.18 | (1.06–1.32) | 0.003 ** | 0.84 | (0.65–1.09) | 0.196 |
| qSOFA | 2.11 | (1.47–3.02) | <0.001 ** | 1.73 | (0.61–4.88) | 0.298 |
| Scores | AUC | COP | Sensitivity | Specificity | PPV | NPV | Accuracy | SE | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| MEDS | 0.905 | 4 | 93% | 80% | 89% | 86% | 88% | 0.047 | <0.001 ** |
| NEWS | 0.878 | 5 | 93% | 87% | 93% | 87% | 91% | 0.069 | <0.001 ** |
| qSOFA | 0.848 | 1 | 85% | 80% | 89% | 75% | 83% | 0.064 | <0.001 ** |
| MEWS with GCS | 0.846 | 3 | 89% | 73% | 86% | 79% | 83% | 0.069 | <0.001 ** |
| REMS | 0.846 | 8 | 70% | 87% | 91% | 62% | 76% | 0.059 | <0.001 ** |
| RAPS | 0.842 | 3 | 70% | 100% | 100% | 65% | 81% | 0.061 | <0.001 ** |
| MEWS | 0.833 | 3 | 93% | 73% | 86% | 85% | 86% | 0.071 | <0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, W.-K.; Hsieh, M.-S.; Hu, S.-Y.; Huang, S.-C.; Tsai, C.-A.; Chang, Y.-Z.; Tsai, Y.-C. Predictive Performance of Scoring Systems for Mortality Risk in Patients with Cryptococcemia: An Observational Study. J. Pers. Med. 2023, 13, 1358. https://doi.org/10.3390/jpm13091358
Liao W-K, Hsieh M-S, Hu S-Y, Huang S-C, Tsai C-A, Chang Y-Z, Tsai Y-C. Predictive Performance of Scoring Systems for Mortality Risk in Patients with Cryptococcemia: An Observational Study. Journal of Personalized Medicine. 2023; 13(9):1358. https://doi.org/10.3390/jpm13091358
Chicago/Turabian StyleLiao, Wei-Kai, Ming-Shun Hsieh, Sung-Yuan Hu, Shih-Che Huang, Che-An Tsai, Yan-Zin Chang, and Yi-Chun Tsai. 2023. "Predictive Performance of Scoring Systems for Mortality Risk in Patients with Cryptococcemia: An Observational Study" Journal of Personalized Medicine 13, no. 9: 1358. https://doi.org/10.3390/jpm13091358
APA StyleLiao, W.-K., Hsieh, M.-S., Hu, S.-Y., Huang, S.-C., Tsai, C.-A., Chang, Y.-Z., & Tsai, Y.-C. (2023). Predictive Performance of Scoring Systems for Mortality Risk in Patients with Cryptococcemia: An Observational Study. Journal of Personalized Medicine, 13(9), 1358. https://doi.org/10.3390/jpm13091358





