Smartphone-Based versus Non-Invasive Automatic Oscillometric Brachial Cuff Blood Pressure Measurements: A Prospective Method Comparison Volunteer Study
Abstract
:1. Introduction
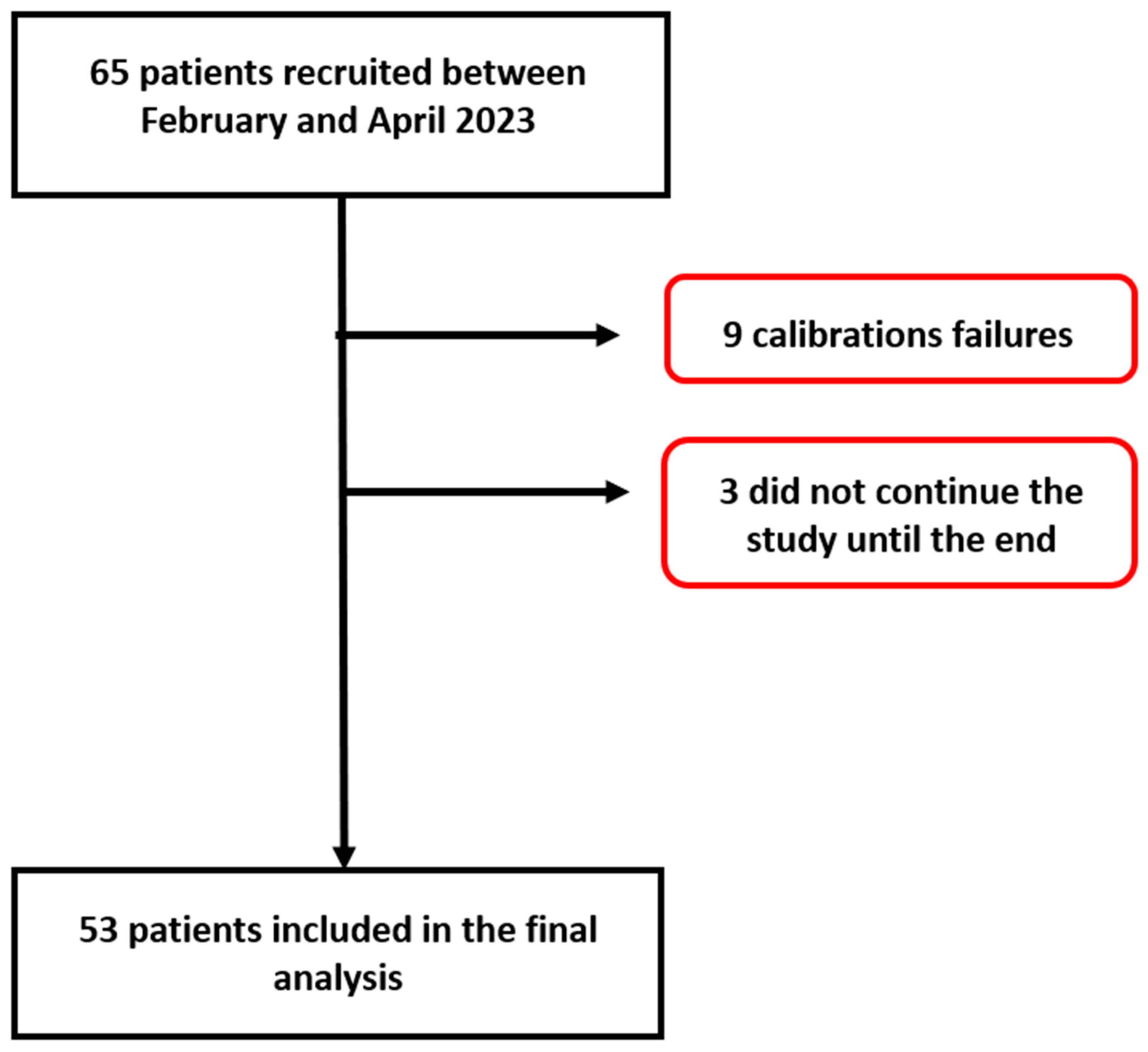
2. Materials and Methods
2.1. Test Method (OptiBPTM)
2.2. Reference Method (Non-Invasive Automatic Brachial Cuff Oscillometry)
2.3. Study Protocol
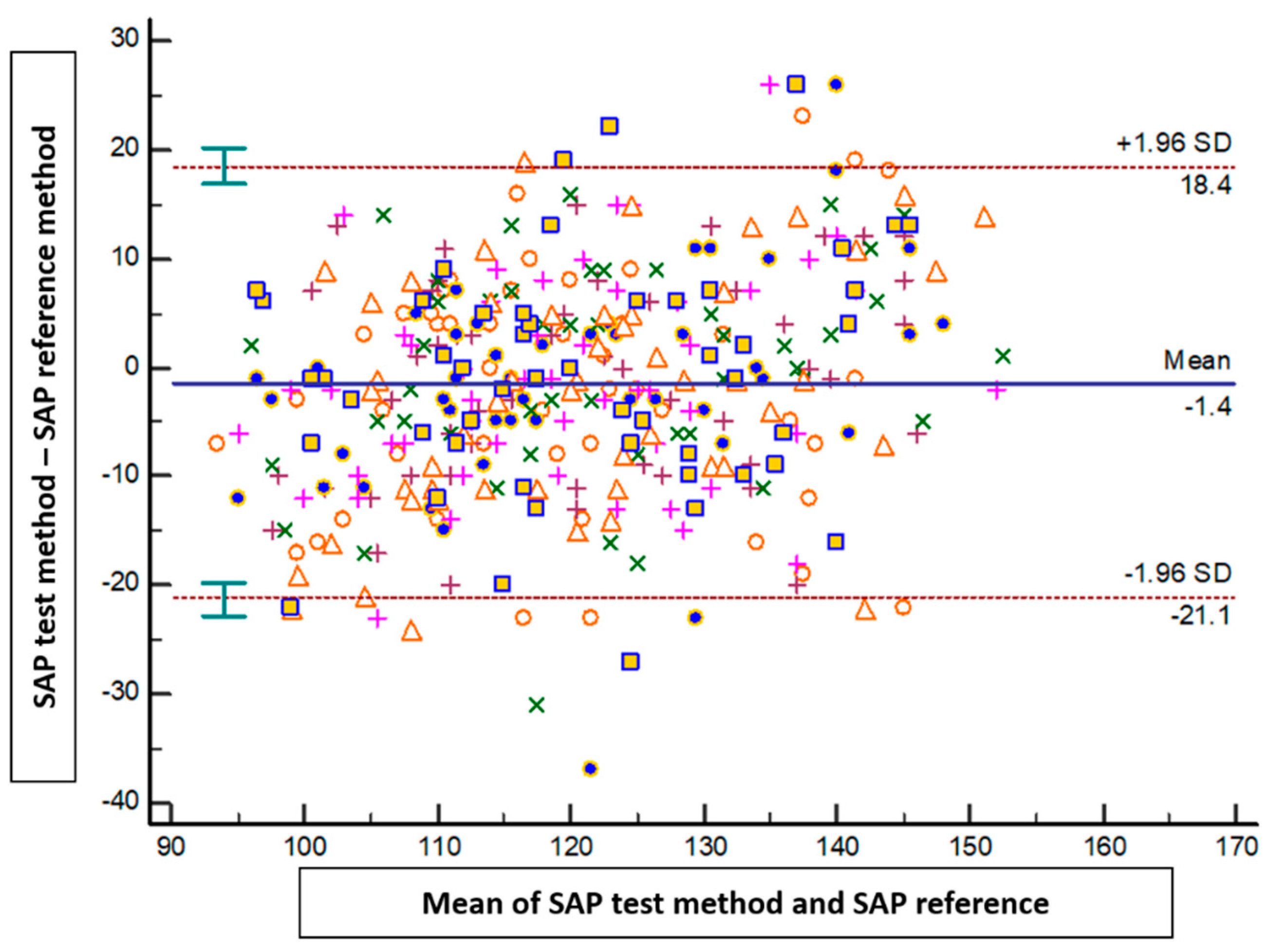
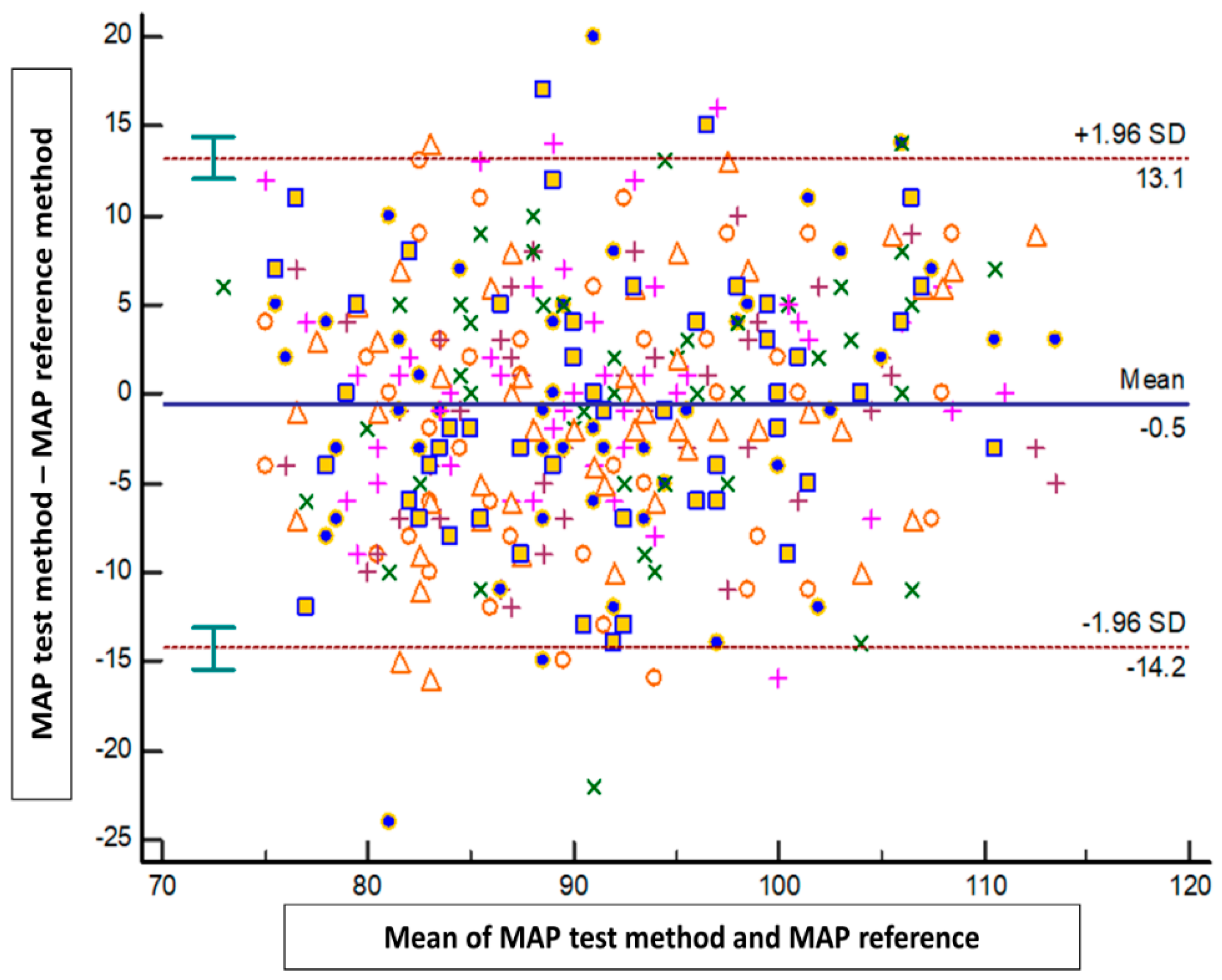
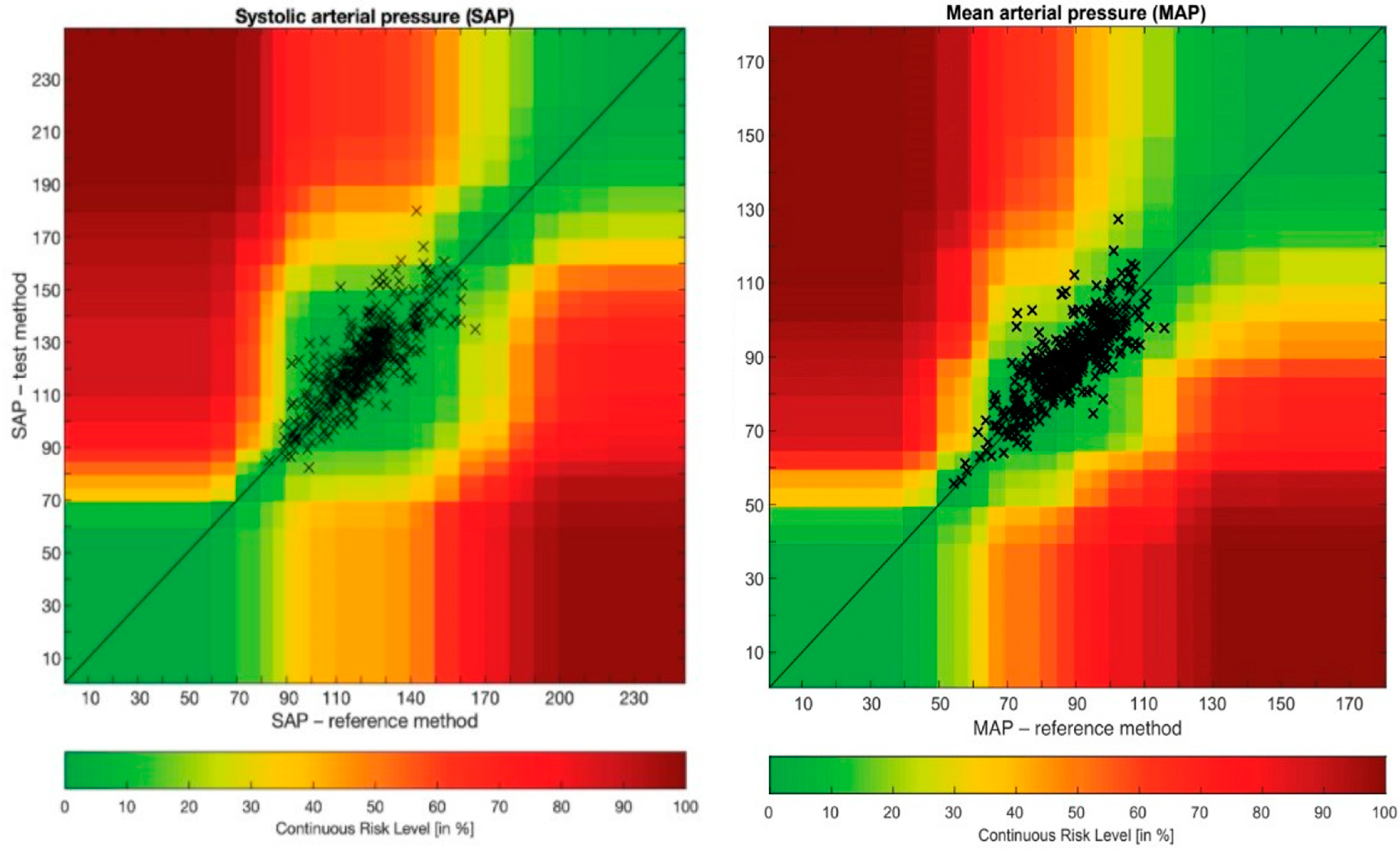
2.4. Statistical Analysis
3. Results
4. Discussion
Future Prospects
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Boateng, E.B.; Ampofo, A.G. A glimpse into the future: Modelling global prevalence of hypertension. BMC Public Health 2023, 23, 1906. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef] [PubMed]
- Schutte, A.E.; Kollias, A.; Stergiou, G.S. Blood pressure and its variability: Classic and novel measurement techniques. Nat. Rev. Cardiol. 2022, 19, 643–654. [Google Scholar] [CrossRef] [PubMed]
- Pioli, M.R.; Ritter, A.M.; de Faria, A.P.; Modolo, R. White coat syndrome and its variations: Differences and clinical impact. Integr. Blood Press. Control 2018, 11, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, K.; Bowling, C.B.; Sim, J.J.; Sridharan, L.; Harrison, T.N.; Shimbo, D. The Utility of Ambulatory Blood Pressure Monitoring for Diagnosing White Coat Hypertension in Older Adults. Curr. Hypertens. Rep. 2015, 17, 86. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, D.Y.; Li, Y.; Wang, J.G. The Role of Out-of-Clinic Blood Pressure Measurements in Preventing Hypertension. Curr. Hypertens. Rep. 2018, 20, 85. [Google Scholar] [CrossRef]
- Ventola, C.L. Mobile devices and apps for health care professionals: Uses and benefits. Pharm. Ther. 2014, 39, 356–364. [Google Scholar]
- Holopainen, A. Mobile technology and health applications, what are they? Duodecim 2015, 131, 1285–1290. [Google Scholar]
- Joosten, A.; Boudart, C.; Vincent, J.L.; Vanden Eynden, F.; Barvais, L.; Van Obbergh, L.; Rinehart, J.; Desebbe, O. Ability of a New Smartphone Pulse Pressure Variation and Cardiac Output Application to Predict Fluid Responsiveness in Patients Undergoing Cardiac Surgery. Anesth. Analg. 2019, 128, 1145–1151. [Google Scholar] [CrossRef] [PubMed]
- Joosten, A.; Jacobs, A.; Desebbe, O.; Vincent, J.L.; Sarah, S.; Rinehart, J.; Van Obbergh, L.; Hapfelmeier, A.; Saugel, B. Monitoring of pulse pressure variation using a new smartphone application (Capstesia) versus stroke volume variation using an uncalibrated pulse wave analysis monitor: A clinical decision making study during major abdominal surgery. J. Clin. Monit. Comput. 2019, 33, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Pluta, M.P.; Dziech, M.; Zachura, M.N.; Szczepańska, A.J.; Czempik, P.F.; Liberski, P.S.; Krzych, Ł.J. Hemodynamic Monitoring by Smartphone-Preliminary Report from a Comparative Prospective Observational Study. J. Pers. Med. 2022, 12, 200. [Google Scholar] [CrossRef] [PubMed]
- Bacariza, J.; Gonzalez, F.A.; Varudo, R.; Leote, J.; Martins, C.; Fernandes, A.; Michard, F. Smartphone-based automatic assessment of left ventricular ejection fraction with a silicon chip ultrasound probe: A prospective comparison study in critically ill patients. Br. J. Anaesth. 2023, 130, e485–e487. [Google Scholar] [CrossRef] [PubMed]
- Bastawrous, A.; Armstrong, M.J. Mobile health use in low- and high-income countries: An overview of the peer-reviewed literature. J. R. Soc. Med. 2013, 106, 130–142. [Google Scholar] [CrossRef] [PubMed]
- McCool, J.; Dobson, R.; Whittaker, R.; Paton, C. Mobile Health (mHealth) in Low- and Middle-Income Countries. Annu. Rev. Public Health 2022, 43, 525–539. [Google Scholar] [CrossRef]
- Dol, J.; Richardson, B.; Tomblin Murphy, G.; Aston, M.; McMillan, D.; Campbell-Yeo, M. Impact of mobile health (mHealth) interventions during the perinatal period for mothers in low- and middle-income countries: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2019, 17, 1634–1667. [Google Scholar] [CrossRef]
- Ogedegbe, G.; Pickering, T. Principles and techniques of blood pressure measurement. Cardiol. Clin. 2010, 28, 571–586. [Google Scholar] [CrossRef]
- Sharman, J.E.; Tan, I.; Stergiou, G.S.; Lombardi, C.; Saladini, F.; Butlin, M.; Padwal, R.; Asayama, K.; Avolio, A.; Brady, T.M.; et al. Automated ‘oscillometric’ blood pressure measuring devices: How they work and what they measure. J. Hum. Hypertens. 2023, 37, 93–100. [Google Scholar] [CrossRef]
- Alpert, B.S.; Quinn, D.; Gallick, D. Oscillometric blood pressure: A review for clinicians. J. Am. Soc. Hypertens. 2014, 8, 930–938. [Google Scholar] [CrossRef]
- Matsumura, K.; Rolfe, P.; Toda, S.; Yamakoshi, T. Cuffless blood pressure estimation using only a smartphone. Sci. Rep. 2018, 8, 7298. [Google Scholar] [CrossRef] [PubMed]
- Frey, L.; Menon, C.; Elgendi, M. Blood pressure measurement using only a smartphone. NPJ Digit. Med. 2022, 5, 86. [Google Scholar] [CrossRef] [PubMed]
- Bard, D.M.; Joseph, J.I.; van Helmond, N. Cuff-Less Methods for Blood Pressure Telemonitoring. Front. Cardiovasc. Med. 2019, 6, 40. [Google Scholar] [CrossRef] [PubMed]
- Boulos, M.N.; Wheeler, S.; Tavares, C.; Jones, R. How smartphones are changing the face of mobile and participatory healthcare: An overview, with example from eCAALYX. Biomed. Eng. Online 2011, 10, 24. [Google Scholar] [CrossRef] [PubMed]
- Caillat, M.; Degott, J.; Wuerzner, A.; Proençain, M.; Bonnier, G.; Knebel, J.F.; Stoll, C.; Christen, U.; Durgnat, V.; Hofmann, G.; et al. Accuracy of blood pressure measurement across BMI categories using the OptiBP™ mobile application. Blood Press. 2022, 31, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Degiorgis, Y.; Proença, M.; Ghamri, Y.; Hofmann, G.; Lemay, M.; Schoettker, P. Photoplethysmography-Based Blood Pressure Monitoring Could Improve Patient Outcome during Anesthesia Induction. J. Pers. Med. 2022, 12, 1571. [Google Scholar] [CrossRef]
- Desebbe, O.; Anas, C.; Alexander, B.; Kouz, K.; Knebel, J.F.; Schoettker, P.; Creteur, J.; Vincent, J.L.; Joosten, A. Evaluation of a novel optical smartphone blood pressure application: A method comparison study against invasive arterial blood pressure monitoring in intensive care unit patients. BMC Anesthesiol. 2022, 22, 259. [Google Scholar] [CrossRef]
- Hofmann, G.; Proença, M.; Degott, J.; Bonnier, G.; Lemkaddem, A.; Lemay, M.; Schorer, R.; Christen, U.; Knebel, J.F.; Schoettker, P. A novel smartphone app for blood pressure measurement: A proof-of-concept study against an arterial catheter. J. Clin. Monit. Comput. 2023, 37, 249–259. [Google Scholar] [CrossRef]
- Desebbe, O.; El Hilali, M.; Kouz, K.; Alexander, B.; Karam, L.; Chirnoaga, D.; Knebel, J.F.; Degott, J.; Schoettker, P.; Michard, F.; et al. Evaluation of a new smartphone optical blood pressure application (OptiBP™) in the post-anesthesia care unit: A method comparison study against the non-invasive automatic oscillometric brachial cuff as the reference method. J. Clin. Monit. Comput. 2022, 36, 1525–1533. [Google Scholar] [CrossRef]
- Desebbe, O.; Tighenifi, A.; Jacobs, A.; Toubal, L.; Zekhini, Y.; Chirnoaga, D.; Collange, V.; Alexander, B.; Knebel, J.F.; Schoettker, P.; et al. Evaluation of a novel mobile phone application for blood pressure monitoring: A proof of concept study. J. Clin. Monit. Comput. 2022, 36, 1147–1153. [Google Scholar] [CrossRef]
- Degott, J.; Ghajarzadeh-Wurzner, A.; Hofmann, G.; Proença, M.; Bonnier, G.; Lemkaddem, A.; Lemay, M.; Christen, U.; Knebel, J.F.; Durgnat, V.; et al. Smartphone based blood pressure measurement: Accuracy of the OptiBP mobile application according to the AAMI/ESH/ISO universal validation protocol. Blood Press. Monit. 2021, 26, 441–448. [Google Scholar] [CrossRef] [PubMed]
- Schoettker, P.; Degott, J.; Hofmann, G.; Proença, M.; Bonnier, G.; Lemkaddem, A.; Lemay, M.; Schorer, R.; Christen, U.; Knebel, J.F.; et al. Blood pressure measurements with the OptiBP smartphone app validated against reference auscultatory measurements. Sci. Rep. 2020, 10, 17827. [Google Scholar] [CrossRef] [PubMed]
- Michard, F. Hemodynamic Monitoring: Would a Pulse Oximeter Do the Job? Crit. Care Med. 2021, 49, 383–386. [Google Scholar] [CrossRef] [PubMed]
- Michard, F.; Shelley, K.; L’Her, E. COVID-19: Pulse oximeters in the spotlight. J. Clin. Monit. Comput. 2021, 35, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Demiris, G.; Afrin, L.B.; Speedie, S.; Courtney, K.L.; Sondhi, M.; Vimarlund, V.; Lovis, C.; Goossen, W.; Lynch, C. Patient-centered applications: Use of information technology to promote disease management and wellness. A white paper by the AMIA knowledge in motion working group. J. Am. Med. Inform. Assoc. 2008, 15, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.iso.org/obp/ui/en/#iso:std:iso:81060:-2:ed-3:v1:en (accessed on 20 October 2023).
- Saugel, B.; Grothe, O.; Nicklas, J.Y. Error Grid Analysis for Arterial Pressure Method Comparison Studies. Anesth. Analg. 2018, 126, 1177–1185. [Google Scholar] [CrossRef]
- Grothe, O.; Kaplan, A.; Kouz, K.; Saugel, B. Computer Program for Error Grid Analysis in Arterial Blood Pressure Method Comparison Studies. Anesth. Analg. 2020, 130, e71–e74. [Google Scholar] [CrossRef]
- Juri, T.; Suehiro, K.; Kanematsu, R.; Takahashi, K.; Fujimoto, Y.; Tanaka, K.; Mori, T. Validation of Continuous Noninvasive Blood Pressure Monitoring Using Error Grid Analysis. Anesth. Analg. 2022, 134, 773–780. [Google Scholar] [CrossRef]
- Juri, T.; Suehiro, K.; Uchimoto, A.; Go, H.; Fujimoto, Y.; Mori, T.; Nishikawa, K. Error grid analysis for risk management in the difference between invasive and noninvasive blood pressure measurements. J. Anesth. 2021, 35, 189–196. [Google Scholar] [CrossRef]
- Kho, E.; van der Ster, B.J.P.; van der Ven, W.H.; Vlaar, A.P.J.; Immink, R.V.; Veelo, D.P. Clinical agreement of a novel algorithm to estimate radial artery blood pressure from the non-invasive finger blood pressure. J. Clin. Anesth. 2022, 83, 110976. [Google Scholar] [CrossRef]
- Eley, V.; Christensen, R.; Guy, L.; Wyssusek, K.; Pelecanos, A.; Dodd, B.; Stowasser, M.; van Zundert, A. ClearSight™ finger cuff versus invasive arterial pressure measurement in patients with body mass index above 45 kg/m2. BMC Anesthesiol. 2021, 21, 152. [Google Scholar] [CrossRef] [PubMed]
- Festo, C.; Vannevel, V.; Ali, H.; Tamrat, T.; Mollel, G.J.; Hlongwane, T.; Fahmida, K.A.; Alland, K.; Barreix, M.; Mehrtash, H.; et al. Accuracy of a smartphone application for blood pressure estimation in Bangladesh, South Africa, and Tanzania. NPJ Digit. Med. 2023, 6, 69. [Google Scholar] [CrossRef] [PubMed]
- Michard, F.; Barrachina, B.; Schoettker, P. Is your smartphone the future of physiologic monitoring? Intensive Care Med. 2019, 45, 869–871. [Google Scholar] [CrossRef] [PubMed]
- Michard, F. Toward Smart Monitoring with Phones, Watches, and Wearable Sensors. Anesthesiol. Clin. 2021, 39, 555–564. [Google Scholar] [CrossRef] [PubMed]
- Michard, F. Smartphones and e-tablets in perioperative medicine. Korean J. Anesthesiol. 2017, 70, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Michard, F.; Gan, T.J.; Kehlet, H. Digital innovations and emerging technologies for enhanced recovery programmes. Br. J. Anaesth. 2017, 119, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Michard, F. A sneak peek into digital innovations and wearable sensors for cardiac monitoring. J. Clin. Monit. Comput. 2017, 31, 253–259. [Google Scholar] [CrossRef]
- O’Loughlin, K.; Neary, M.; Adkins, E.C.; Schueller, S.M. Reviewing the data security and privacy policies of mobile apps for depression. Internet Interv. 2019, 15, 110–115. [Google Scholar] [CrossRef]
- Xiang, D.; Cai, W. Privacy Protection and Secondary Use of Health Data: Strategies and Methods. Biomed. Res. Int. 2021, 2021, 6967166. [Google Scholar] [CrossRef]
- Huckvale, K.; Torous, J.; Larsen, M.E. Assessment of the Data Sharing and Privacy Practices of Smartphone Apps for Depression and Smoking Cessation. JAMA Netw. Open 2019, 2, e192542. [Google Scholar] [CrossRef]

| Variables | N = 53 |
|---|---|
| Age (years) | 47 ± 16 |
| Sex, Male (N, %) | 16 (30%) |
| Height (cm) | 169 ± 9 |
| Body weight (kg) | 73 ± 14 |
| Body mass index (kg/m2) | 26 ± 5 |
Ethnicity (N, %)
| 32 (60%) 8 (15%) 10 (19%) 3 (6%) |
| Chronic hypertension (N, %) | 9 (17%) |
| Untreated hypertensive patients (N, %) | 2 (4%) |
| Hypertensive patients with a treatment (N, %) | 7 (13%) |
| Author | Year | Place of Investigation and Reference Method | Population | No. of Subjects | Duration of the Study | ISO Standards | Error Grid |
|---|---|---|---|---|---|---|---|
| Schoettker et al. [32] | 2020 | Hypertension clinic and auscultatory method | Hypertensive or non-hypertensive patients | 40 | 7 × 1 min | SAP: −0.7 ± 7.7 mmHg DAP: −0.4 ± 4.5 mmHg MAP: −0.6 ± 5.2 mmHg | Not realized |
| Degott et al. [31] | 2021 | Hypertension clinic and auscultatory method | Patients with hypertension | 91 | 9 × 1 min | SAP: 0.5 ± 7.7 mmHg DAP: 0.4 ± 4.6 mmHg | Not realized |
| Desebbe et al. [30] | 2022 | Emergency department and automatic brachial cuff | General population | 110 | 3 × 1 min | SAP: −0.1 ± 11.5 mmHg DAP: −0.1 ± 6.5 mmHg MAP: −0.3 ± 8.9 mmHg | SAP: A: 89.3, B: 10.7, C-E: 0 MAP: A: 86.9, B: 13.1, C-E: 0 |
| Desebbe et al. [29] | 2022 | Recovery room and automatic brachial cuff | Post abdominal surgery | 120 (101) | Each 15 min for 2 consecutive hours | SAP: 1.95 ± 11.0 mmHg DAP: 1.27 ± 8.0 mmHg MAP: 1.3 ± 7.0 mmHg | SAP: A: 89.9, B: 9.1, C: 1.0, D-E: 0 MAP: A: 90.3, B: 9.7, C-E: 0 |
| Desebbe et al. [27] | 2022 | ICU and radial arterial catheter | Intensive care patients | 22 | Each hour for 5 consecutive hours during 2 consecutive days | SAP: 0.2 ± 13.75 mmHg DAP: 1.1 ± 5.97 mmHg MAP: 0.9 ± 7.27 mmHg | SAP: A: 88.4, B: 8.6, C: 3.0, D-E: 0 MAP: A: 88.8, B: 10.0, C: 1.0, D-E: 0 |
| Hofmann et al. [28] | 2023 | Operating theatre and arterial catheter | Elective surgery | 119 | 10 × 1 min | SAP: 0.0 ± 7.5 mmHg DAP: 0.1 ± 2.9 mmHg MAP: 0.1 ± 4.2 mmHg | SAP: A: 89.8, B: 9.0, C: 1.2, D-E: 0 MAP: A: 89.9, B: 9.8, C: 0.2, D-E: 0 |
| Festo et al. [43] | 2023 | General population and auscultatory method | General and pregnant population | 100 60 | 4 × 30 s | In South Africa SAP: 0.5 ± 5.8 mm Hg DAP: 0.1 ± 3.9 mmHg In Tanzania SAP: 0.8 ± 7.0 mmHg DAP: −4.0 ± 4.0 mmHg In Bangladesh SAP: 3.3 ± 7.4 mmHg DAP: −0.4 ± 4.3 mmHg | Not realized |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delmotte, L.; Desebbe, O.; Alexander, B.; Kouz, K.; Coeckelenbergh, S.; Schoettker, P.; Turgay, T.; Joosten, A. Smartphone-Based versus Non-Invasive Automatic Oscillometric Brachial Cuff Blood Pressure Measurements: A Prospective Method Comparison Volunteer Study. J. Pers. Med. 2024, 14, 15. https://doi.org/10.3390/jpm14010015
Delmotte L, Desebbe O, Alexander B, Kouz K, Coeckelenbergh S, Schoettker P, Turgay T, Joosten A. Smartphone-Based versus Non-Invasive Automatic Oscillometric Brachial Cuff Blood Pressure Measurements: A Prospective Method Comparison Volunteer Study. Journal of Personalized Medicine. 2024; 14(1):15. https://doi.org/10.3390/jpm14010015
Chicago/Turabian StyleDelmotte, Lila, Olivier Desebbe, Brenton Alexander, Karim Kouz, Sean Coeckelenbergh, Patrick Schoettker, Tuna Turgay, and Alexandre Joosten. 2024. "Smartphone-Based versus Non-Invasive Automatic Oscillometric Brachial Cuff Blood Pressure Measurements: A Prospective Method Comparison Volunteer Study" Journal of Personalized Medicine 14, no. 1: 15. https://doi.org/10.3390/jpm14010015
APA StyleDelmotte, L., Desebbe, O., Alexander, B., Kouz, K., Coeckelenbergh, S., Schoettker, P., Turgay, T., & Joosten, A. (2024). Smartphone-Based versus Non-Invasive Automatic Oscillometric Brachial Cuff Blood Pressure Measurements: A Prospective Method Comparison Volunteer Study. Journal of Personalized Medicine, 14(1), 15. https://doi.org/10.3390/jpm14010015






