The Influence of Physical Activity during Pregnancy on Maternal Pain and Discomfort: A Meta-Analysis
Abstract
:1. Introduction
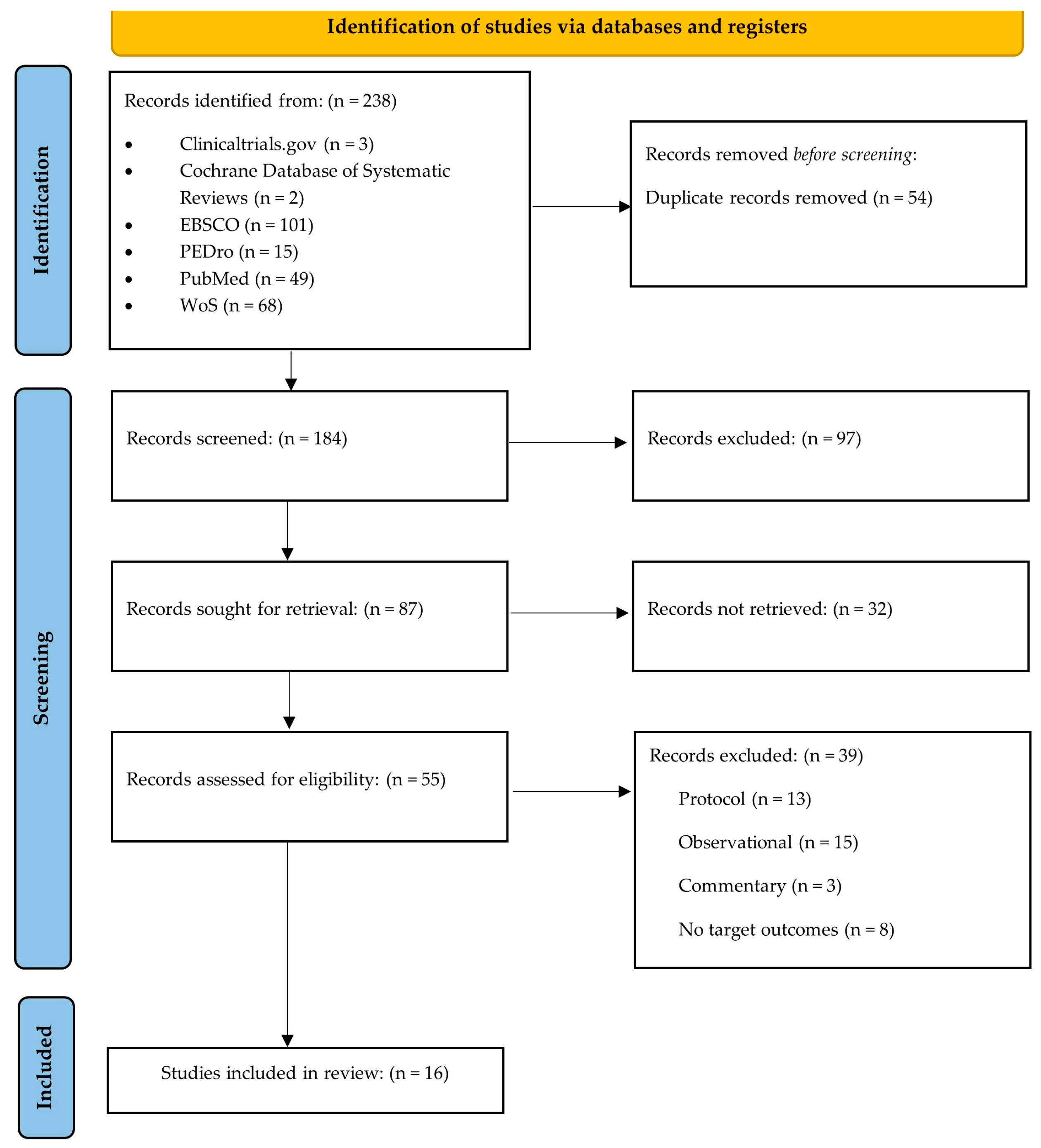
2. Materials and Methods
2.1. Population
2.2. Intervention
2.3. Comparison
2.4. Outcomes
2.5. Study Selection Process, Data Sources, and Data Extraction
- English: physical activity OR exercise OR fitness OR physical exercise OR sport OR walking OR cycling OR physical intervention AND pregnancy OR pregnant OR prenatal OR maternal OR antenatal OR perinatal AND randomized clinical trial OR randomized controlled trial OR RCT AND pain OR pain management OR pain relief OR pain control OR pain reduction OR discomfort OR low back pain OR lumbar pain OR lumbar spine pain OR nonspecific low back pain OR chronic low back pain OR pelvic girdle pain OR PGP OR pelvic pain OR pelvic dysfunction.
- Spanish: actividad física O ejercicio O fitness O ejercicio físico O deporte O caminar O bicicleta O intervención Y embarazo O embarazada O prenatal O maternal O antenatal O perinatal Y ensayo clínico aleatorizado O ensayo controlado aleatorizado O ECA Y dolor O gestion del dolor O Alivio del dolor O control del dolor O reducción del dolor O malestar O lumbalgia O dolor lumbar O dolor de columna O dolor lumbar no específico O lumbalgia crónica O dolor de cintura pélvica O dolor pélvico O disfunción pélvica.
2.6. Risk of Bias and Quality of Evidence
2.7. Statistical Analysis
3. Results
3.1. Risk of Bias and Quality of Evidence Assessments
3.2. Article Characteristics
3.3. Effect of Physical Activity on Pain, Pain Intensity, and ODI Score
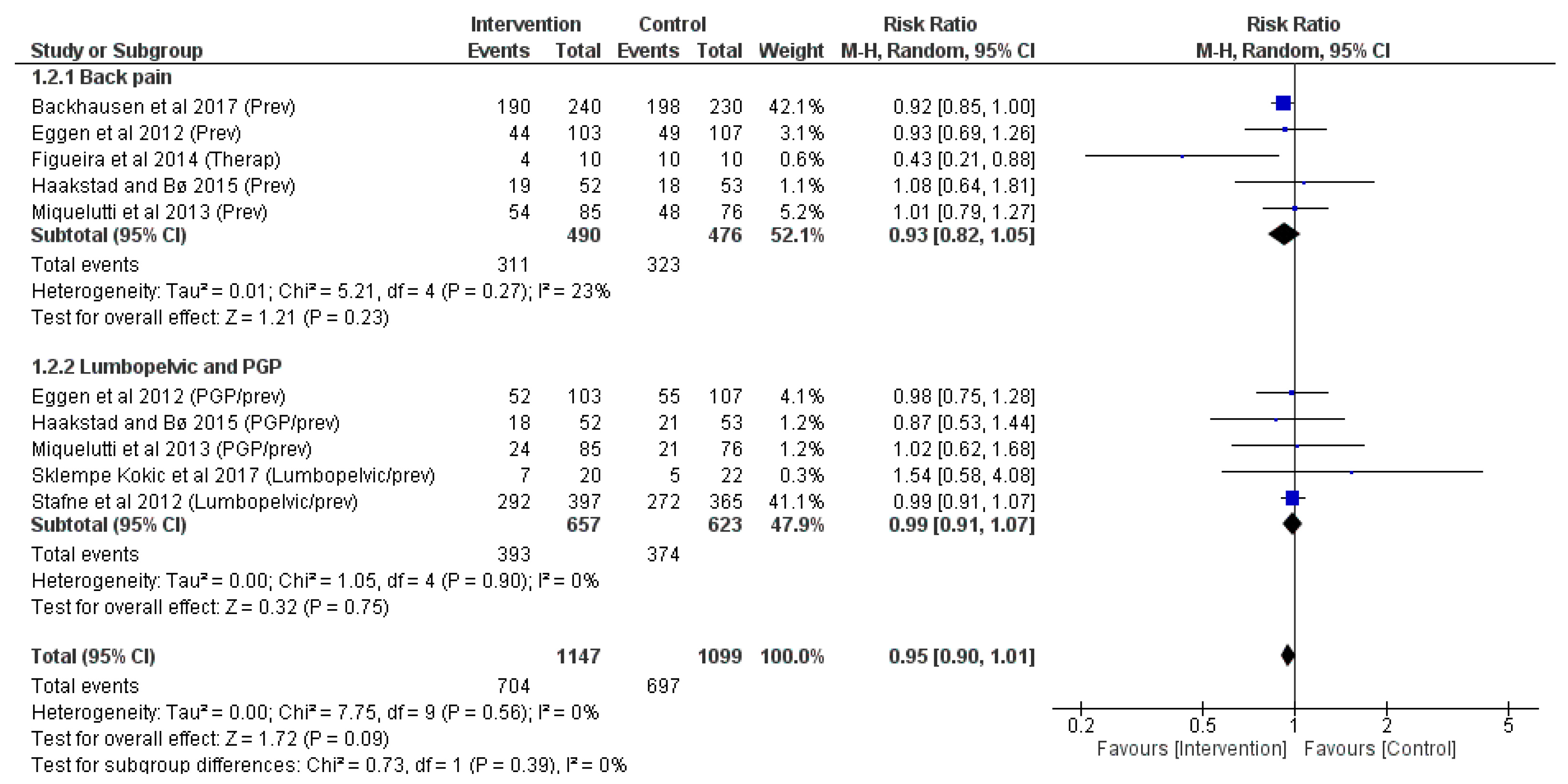
3.4. Physical Activity Effects on Events of Back Pain and Pelvic Girdle Pain at the End of Pregnancy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quintero Rodriguez, C.; Troynikov, O. The Effect of Maternity Support Garments on Alleviation of Pains and Discomforts during Pregnancy: A Systematic Review. J. Pregnancy 2019, 2019, 2163790. [Google Scholar] [CrossRef] [PubMed]
- Verstraete, E.H.; Vanderstraeten, G.; Parewijck, W. Pelvic Girdle Pain during or after Pregnancy: A review of recent evidence and a clinical care path proposal. Facts Views Vis. Obgyn. 2013, 5, 33–43. [Google Scholar] [PubMed]
- Bryndal, A.; Majchrzycki, M.; Grochulska, A.; Glowinski, S.; Seremak-Mrozikiewicz, A. Risk factors associated with low back pain among A group of 1510 pregnant women. J. Pers. Med. 2020, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Wuytack, F.; Begley, C.; Daly, D. Risk factors for pregnancy-related pelvic girdle pain: A scoping review. BMC Pregnancy Childbirth 2020, 20, 739. [Google Scholar] [CrossRef] [PubMed]
- Conder, R.; Zamani, R.; Akrami, M. The biomechanics of pregnancy: A systematic review. J. Funct. Morphol. Kinesiol. 2019, 4, 72. [Google Scholar] [CrossRef] [PubMed]
- Yousefabadi, S.R.; Sarani, A.; Arbabshastan, M.E.; Adineh, H.A.; Shahnavazi, M. The effect of exercise on back pain and lordosis in the second trimester of pregnancy. Drug Invent. Today 2019, 11, 2169–2175. [Google Scholar]
- Feldthusen, C.; Fagevik Olsen, M.; Ejnell, H.; Elden, H. Effects of a New Mattress and Pillow and Standard Treatment for Nightly Pelvic Girdle Pain in Pregnant Women: A Randomised Controlled Study. Int. J. Womens Health 2021, 13, 1251–1260. [Google Scholar] [CrossRef]
- Ribeiro, M.M.; Andrade, A.; Nunes, I. Physical exercise in pregnancy: Benefits, risks and prescription. J. Perinat. Med. 2021, 50, 4–17. [Google Scholar] [CrossRef]
- Davenport, M.H.; Marchand, A.; Mottola, M.F.; Poitras, V.J.; Gray, C.E.; Garcia, A.J.; Barrowman, N.; Sobierajski, F.; James, M.; Meah, V.L.; et al. Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 90–98. [Google Scholar] [CrossRef]
- Kandru, M.; Zallipalli, S.N.; Dendukuri, N.K.; Linga, S.; Jeewa, L.; Jeewa, A.; Sunar, S.B. Effects of Conventional Exercises on Lower Back Pain and/or Pelvic Girdle Pain in Pregnancy: A Systematic Review and Meta-Analysis. Cureus 2023, 15, e42010. [Google Scholar] [CrossRef]
- Ferraz, V.S.; Peixoto, C.; Ferreira Resstel, A.P.; Cerqueira de Paula, Y.T.; Gomes de Souza Pegorare, A.B. Effect of the pilates method on pain and quality of life in pregnancy: A systematic review and meta-analysis. J. Bodyw. Mov. Ther. 2023, 35, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. Surg. J. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Mottola, M.F.; Davenport, M.H.; Ruchat, S.M.; Davies, G.A.; Poitras, V.J.; Gray, C.E.; Garcia, A.J.; Barrowman, N.; Adamo, K.B.; Duggan, M.; et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br. J. Sports Med. 2018, 52, 1339–1346. [Google Scholar] [CrossRef] [PubMed]
- Barakat, R.; Díaz-Blanco, A.; Franco, E.; Rollán-Malmierca, A.; Brik, M.; Vargas, M.; Silva, C.; Sánchez-Polan, M.; Gil, J.; Perales, M.; et al. Guías clínicas para el ejercicio físico durante el embarazo. Prog. Obstet. Ginecol. 2019, 62, 464–471. [Google Scholar]
- Higgins, J.P.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A. Assessing risk of bias in a randomized trial. Cochrane Handb. Syst. Rev. Interv. 2019, 6, 205–228. [Google Scholar]
- GRADEpro. Guideline Development Tool. McMaster University and Evidence Prime. 2022. Available online: https://www.gradepro.org/ (accessed on 10 September 2023).
- Guyatt, G.H.; Oxman, A.; Vist, G.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE an Emerging Consensus on Rating Quality of Evidence and Strength of Recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Chu, H. Quantifying publication bias in meta-analysis. Biometrics 2018, 74, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Backhausen, M.G.; Tabor, A.; Albert, H.; Rosthøj, S.; Damm, P.; Hegaard, H.K. The effects of an unsupervised water exercise program on low back pain and sick leave among healthy pregnant women—A randomised controlled trial. PLoS ONE 2017, 12, e0182114. [Google Scholar] [CrossRef]
- Bolanthakodi, C.; Raghunandan, C.; Saili, A.; Mondal, S.; Saxena, P. Prenatal Yoga: Effects on Alleviation of Labor Pain and Birth Outcomes. J. Altern. Complement. Med. 2018, 24, 1181–1188. [Google Scholar] [CrossRef]
- Eggen, M.H.; Stuge, B.; Mowinckel, P.; Jensen, K.S.; Hagen, K.B. Can supervised group exercises including ergonomic advice reduce the prevalence and severity of low back pain and pelvic girdle pain in pregnancy? A randomized controlled trial. Phys. Ther. 2012, 92, 781–790. [Google Scholar] [CrossRef]
- Field, T.; Diego, M.; Hernandez-Reif, M.; Medina, L.; Delgado, J.; Hernandez, A. Yoga and massage therapy reduce prenatal depression and prematurity. J. Bodyw. Mov. Ther. 2012, 16, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Field, T.; Diego, M.; Delgado, J.; Medina, L. Yoga and social support reduce prenatal depression, anxiety and cortisol. J. Bodyw. Mov. Ther. 2013, 17, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Figueira, H.A.; de Souza Vale, R.G.; Rodrigues, W.F.G.; Figueira, A.A.; Figueira, J.A.; Dantas, E.H.M. Pregnancy-related low back pain relief after maximum static flexibility program. Health 2014, 6, 2966. [Google Scholar] [CrossRef]
- Haakstad, L.A.; Bø, K. Effect of a regular exercise programme on pelvic girdle and low back pain in previously inactive pregnant women: A randomized controlled trial. J. Rehabil. Med. 2015, 47, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Kordi, R.; Abolhasani, M.; Rostami, M.; Hantoushzadeh, S.; Mansournia, M.A.; Vasheghani-Farahani, F. Comparison between the effect of lumbopelvic belt and home based pelvic stabilizing exercise on pregnant women with pelvic girdle pain; a randomized controlled trial. J. Back Musculoskelet. Rehabil. 2013, 26, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Mamipour, H.; Farazmehr, S.; Negahban, H.; Nazary-Moghadam, S.; Dehghan-Manshadi, F.; Nezhad, M.N.; Jafari, S.; Sharifzadeh, M. Effect of Core Stabilization Exercises on Pain, Functional Disability, and Quality of Life in Pregnant Women With Lumbar and Pelvic Girdle Pain: A Randomized Controlled Trial. J. Manip. Physiol. Ther. 2023, 46, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Mazzarino, M.; Kerr, D.; Morris, M.E. Feasibility of pilates for pregnant women: A randomised trial. J. Bodyw. Mov. Ther. 2022, 32, 207–212. [Google Scholar] [CrossRef]
- Miquelutti, M.A.; Cecatti, J.G.; Makuch, M.Y. Evaluation of a birth preparation program on lumbopelvic pain, urinary incontinence, anxiety and exercise: A randomized controlled trial. BMC Pregnancy Childbirth 2013, 13, 154. [Google Scholar] [CrossRef]
- Mohyadin, E.; Ghorashi, Z.; Molamomanaei, Z. The effect of practicing yoga during pregnancy on labor stages length, anxiety and pain: A randomized controlled trial. J. Complement. Integr. Med. 2020, 18, 413–417. [Google Scholar] [CrossRef]
- Ozdemir, S.; Bebis, H.; Ortabag, T.; Acikel, C. Evaluation of the efficacy of an exercise program for pregnant women with low back and pelvic pain: A prospective randomized controlled trial. J. Adv. Nurs. 2015, 71, 1926–1939. [Google Scholar] [CrossRef]
- Sklempe Kokic, I.; Ivanisevic, M.; Uremovic, M.; Kokic, T.; Pisot, R.; Simunic, B. Effect of therapeutic exercises on pregnancy-related low back pain and pelvic girdle pain: Secondary analysis of a randomized controlled trial. J. Rehabil. Med. 2017, 49, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Sonmezer, E.; Özköslü, M.A.; Yosmaoğlu, H.B. The effects of clinical pilates exercises on functional disability, pain, quality of life and lumbopelvic stabilization in pregnant women with low back pain: A randomized controlled study. J. Back Musculoskelet. Rehabil. 2021, 34, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Stafne, S.N.; Salvesen, K.Å.; Romundstad, P.R.; Stuge, B.; Mørkved, S. Does regular exercise during pregnancy influence lumbopelvic pain? A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2012, 91, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Boutib, A.; Chergaoui, S.; Marfak, A.; Hilali, A.; Youlyouz-Marfak, I. Quality of Life During Pregnancy from 2011 to 2021: Systematic Review. Int. J. Womens Health 2022, 14, 975–1005. [Google Scholar] [CrossRef] [PubMed]
- Sward, L.; Manning, N.; Murchison, A.B.; Ghahremani, T.; McCaulley, J.A.; Magann, E.F. Pelvic Girdle Pain in Pregnancy: A Review. Obstet. Gynecol. Surv. 2023, 78, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Diez-Buil, H.; Hernandez-Lucas, P.; Leirós-Rodríguez, R.; Echeverría-García, O. Effects of the combination of exercise and education in the treatment of low back and/or pelvic pain in pregnant women: Systematic review and meta-analysis. Int. J. Gynaecol. Obstet. 2023, 00, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, F.M.; Garcia, E.; Royuela, A.; González, L.; Abraira, V. Spanish Back Pain Research Network. Prevalence and factors associated with low back pain and pelvic girdle pain during pregnancy: A multicenter study conducted in the Spanish National Health Service. Spine 2012, 37, 1516–1533. [Google Scholar] [CrossRef] [PubMed]
- Bagwell, J.J.; Reynolds, N.; Smith, J.A.; Walaszek, M.; Runez, H.; Lam, K.; Peterson, J.; Katsavelis, D. An exploratory analysis of gait biomechanics and muscle activation in pregnant females with high and low scores for low back or pelvic girdle pain during and after pregnancy. Clin. Biomech. 2022, 97, 105705. [Google Scholar] [CrossRef]
- Stuge, B.; Laerum, E.; Kirkesola, G.; Vøllestad, N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy: A randomized controlled trial. Spine 2004, 29, 351–359. [Google Scholar] [CrossRef]
- Pennick, V.; Liddle, S.D. Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database Syst. Rev. 2013, 8, CD001139. [Google Scholar] [CrossRef]
- Chang, H.Y.; Jensen, M.P.; Lai, Y.H. How do pregnant women manage lumbopelvic pain? Pain manage-ment and their perceived effectiveness. J. Clin. Nurs. 2015, 24, 1338–1346. [Google Scholar] [CrossRef] [PubMed]
- Fiat, F.; Merghes, P.E.; Scurtu, A.D.; Almajan Guta, B.; Dehelean, C.A.; Varan, N.; Bernad, E. The main changes in pregnancy—Therapeutic approach to musculoskeletal pain. Medicina 2022, 58, 1115. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.S.; Yu, W.W.; Lao, T.T.; Chow, D.H.; Chung, J.W.; Li, Y. Effectiveness of maternity support belts in reducing low back pain during pregnancy: A review. J. Clin. Nurs. 2009, 18, 1523–1532. [Google Scholar] [CrossRef] [PubMed]
- Maryati, S.; Karwati, K.; Yanti, D. Pain Reduction Techniques to Overcome Back Pain Complaints in Third Trimester of Pregnancy. Health Notions 2022, 6, 432–435. [Google Scholar]
- Bakker, E.C.; van Nimwegen-Matzinger, C.W.; Ekkel-van der Voorden, W.; Nijkamp, M.D.; Völlink, T. Psychological determinants of pregnancy-related lumbopelvic pain: A prospective cohort study. Acta Obstet. Gynecol. Scand. 2013, 92, 797–803. [Google Scholar] [CrossRef] [PubMed]
- McDonald, H.M.; Sherman, K.A.; Kasparian, N.A. Factors associated with psychological distress among Australian women during pregnancy. Pers. Individ. Differ. 2021, 172, 110577. [Google Scholar] [CrossRef]
- Nodine, P.M.; Matthews, E.E. Common sleep disorders: Management strategies and pregnancy outcomes. J. Midwifery Womens Health 2013, 58, 368–377. [Google Scholar] [CrossRef]
- Poudevigne, M.S.; O’Connor, P.J. A review of physical activity patterns in pregnant women and their relationship to psychological health. Sports Med. 2006, 36, 19–38. [Google Scholar] [CrossRef]
- Tan, L.; Zou, J.; Zhang, Y.; Yang, Q.; Shi, H. A Longitudinal Study of Physical Activity to Improve Sleep Quality During Pregnancy. Nat. Sci. Sleep 2020, 12, 431–442. [Google Scholar] [CrossRef]
- Aparicio, V.A.; Marín-Jiménez, N.; Flor-Alemany, M.; Acosta-Manzano, P.; Coll-Risco, I.; Baena-García, L. Effects of a concurrent exercise training program on low back and sciatic pain and pain disability in late pregnancy. Scand. J. Med. Sci. Sports 2023, 33, 1201–1210. [Google Scholar] [CrossRef]
- Aldabe, D.; Lawrenson, P.; Sullivan, J.; Hyland, G.; Bussey, M.D.; Hammer, N.; Bryant, K.; Woodley, S.J. Management of women with pregnancy-related pelvic girdle pain: An international Delphi study. Physiotherapy 2022, 115, 66–84. [Google Scholar] [CrossRef] [PubMed]


| Ref. | Country | N | IG | CG | Intervention | Main Outcomes | Secondary Outcomes | Co-Intervention | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Freq | Inten | Time | Type | Super | Dur | Adh | |||||||||
| Backhausen et al., 2017 [19] | Denmark | 516 | 258 | 258 | 2 | Low-Mod | 12 | Swimming, aerobic, and strengthening exercises in water | Unsup | 45 min. | ND | Intensity of low back pain | Self-reported days spent on sick leave | - | |
| Bolanthakodi et al., 2018 [20] | India | 150 | 75 | 75 | 3 | Mod | 9 | Yoga | Unsup | 30 min. | ND | Labour pain intensity, type, and duration of delivery | Birth weight and preterm delivery | - | |
| Eggen et al., 2012 [21] | Norway | 257 | 129 | 128 | 1 | ND | 16–20 | Aerobic, joint mobility, strengthening, and pelvic floor exercises | Sup | 60 min. | ND with mean | Events of low back pain and pelvic girdle pain | Pain and disability | Home exercises | |
| Field et al., 2012 [22] | United States | 84 | 28 | 28 | 28 | 2 | Mod | 12 | Yoga | Sup | 20 min. | ND | Anxiety and depression during pregnancy | Back and legs pain | - |
| Field et al., 2013 [23] | United States | 79 | 40 | 39 | 1 | Mod | 12 | Yoga | Unsup | 20 min. | ND | Anxiety and depression during and after pregnancy | Hormone levels and back and legs pain | - | |
| Figueira et al., 2014 [24] | Brazil | 40 | 20 | 20 | 2 | Mod | 11 | Warm up (dancing smooth), flexibility, and relaxation | Sup | 45 min. | ND | Pain intensity | Anthropometric variables | - | |
| Haakstad and Bø, 2015 [25] | Norway | 105 | 52 | 53 | 2 | Mod | 12 | Aerobic, endurance, strengthening, and pelvic floor exercises | Sup | 60 min. | 40.4% | Low back pain and pelvic girdle pain during and after pregnancy | Pain severity | - | |
| Kordi et al., 2013 [26] | Iran | 105 | 35 | 35 | 35 | 3 | Mod | ND | Aerobic, stretching, and strengthening of pelvic girdle muscles | Unsup | ND | ND | Disability due to the pain and pain intensity | Maternal characteristics and quality of life | - |
| Mamipour et al., 2023 [27] | Iran | 35 | 18 | 17 | 1 | ND | 10 | Warm-up, core stability, and cool-down exercises | Sup | 60 min. | ND | Pain intensity and disability | Quality of life | - | |
| 2 | Unsup | 30 min. | |||||||||||||
| Mazzarino et al., 2022 [28] | Australia | 21 | 11 | 10 | 1 | ND | 6 | Pilates | Sup | 60 min. | 72.7% | Feasibility of Pilates classes | Quality of life, pain, and mobility | Instructions and performance of daily floor work exercises at home | |
| Miquelutti et al., 2013 [29] | Brazil | 197 | 97 | 100 | 2 | ND | 16–22 | Nonaerobic exercises and pelvic floor muscle training | Sup | 50 min. | ND | Lumbopelvic pain, anxiety, and urinary incontinence | Perinatal outcomes | - | |
| Mohyadin et al., 2020 [30] | Iran | 84 | 42 | 42 | 1 every 2 | ND | 11 | Yoga | Sup | 60 min. | 100% | Anxiety, labour pain, and length of labour stages | Neonatal Apgar score and mode of delivery | Booklet and training DVD to teach principles of yoga | |
| 3 | Unsup | 20 min. | |||||||||||||
| Ozdemir et al., 2015 [31] | Turkey | 96 | 48 | 48 | 3 | ND | 4 | Stretching, tightening, and loosening movements | Sup | 30 min. | ND | Change in pain intensity | Disability due to pain and frequency of low back and pelvic pain | Individualised health counselling to relieve low back and pelvic pain | |
| Walking exercises | |||||||||||||||
| Sklempe Kokic et al., 2017 [32] | Croatia | 42 | 22 | 20 | 2 | Mod | 6 | Aerobic, resistance, pelvic floor, stretching, and relaxation exercises | Sup | 50–55 min. | 70% | Outcomes of gestational diabetes mellitus | Disability due to the pain, and pelvic girdle | - | |
| Sonmezer et al., 2021 [33] | Turkey | 40 | 20 | 20 | 2 | ND | 8 | Pilates | Sup | 60–70 min. | ND | Low back disability and pain intensity | Health-related quality of life and lumbopelvic stabilisation | - | |
| Stafne et al., 2012 [34] | Norway | 762 | 397 | 365 | 1 | Mod | 12 | Aerobic (or endurance), strengthening, balance, stretching, and pelvic floor exercises | Sup | 55–70 min. | 55% | Prevalence and sick due to lumbopelvic pain | Disability due to the pain and pain intensity | - | |
| 2 | Unsup | 45 min. | |||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Polán, M.; Nagpal, T.S.; Zhang, D.; Silva-Jose, C.; Montejo, R.; Barakat, R. The Influence of Physical Activity during Pregnancy on Maternal Pain and Discomfort: A Meta-Analysis. J. Pers. Med. 2024, 14, 44. https://doi.org/10.3390/jpm14010044
Sánchez-Polán M, Nagpal TS, Zhang D, Silva-Jose C, Montejo R, Barakat R. The Influence of Physical Activity during Pregnancy on Maternal Pain and Discomfort: A Meta-Analysis. Journal of Personalized Medicine. 2024; 14(1):44. https://doi.org/10.3390/jpm14010044
Chicago/Turabian StyleSánchez-Polán, Miguel, Taniya S. Nagpal, Dingfeng Zhang, Cristina Silva-Jose, Rocío Montejo, and Rubén Barakat. 2024. "The Influence of Physical Activity during Pregnancy on Maternal Pain and Discomfort: A Meta-Analysis" Journal of Personalized Medicine 14, no. 1: 44. https://doi.org/10.3390/jpm14010044






