Reliability, Concurrent Validity, and Clinical Performances of the Shorter Version of the Roland Morris Disability Questionnaire in a Sample of Italian People with Non-Specific Low Back Pain
Abstract
1. Introduction
2. Materials and Methods
Statistics
3. Results
4. Discussion
- (i)
- does support the concrete possibility to adopt the shorter version when compared with the longer form: both PROMs were significant determinants of pain intensity, and hence, rehab professionals can safely also use the RM-18 during their clinical practice;
- (ii)
- confirms the clockwise circularity of the FAM [14]: this finding should suggest that disability has to be considered as the primary reference point to personalize when people with non-specific LBP are addressed.
- (i)
- it is of importance to plan an adequate evaluation phase for the correct definition of individualized objectives for personal care [22,23]. It is known that each individual presents different characteristics from other people by pursuing short-, medium-, and long-term goals: by means of a correct evaluation, it is possible to precisely identify which objectives to work on [24,25].
- (ii)
- people who feel accurately assessed and are helped to identify their own objectives will also be more compliant with the treatment with a notable saving of resources and time.
- (iii)
- there will be the possibility of adapting the treatment to the person and not vice versa. For example, when an individual with non-specific LBP answers “yes” to question nos. 2 (I walk more slowly than usual because of my back), 8 (I get dressed more slowly than usual because of my back), 13 (I find it difficult to turn over in bed because of my back), or 16 (I avoid heavy jobs around the house because of my back) of the RM-18, the physiotherapist can gradually introduce and shape exercises within the rehab program, with the aim of training people during every session; videos on the management of specific ADLs should also be taken into account. Answering “no” to some issues should be regarded also as a resource that the person already has, by enhancing positive moods and self-efficacy and giving only brief hints while focusing more on the other troubling items.
4.1. Future Research and Prospective
4.2. Possible Rehabilitative and Clinical Applications
4.3. Limits
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 10137. [Google Scholar] [CrossRef] [PubMed]
- Gabel, C.P.; Mokhtarinia, H.R.; Melloh, M.; Mateo, S. Slacklining as therapy to address non-specific low back pain in the presence of multifidus arthrogenic muscle inhibition. World J. Orthop. 2021, 12, 178–196. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.W.; Binkley, J.M. Measurement Properties of the RM-18: A Modified Version of the Roland-Morris Disability Scale. Spine 1997, 22, 2416–2421. [Google Scholar] [CrossRef] [PubMed]
- Roland, M.; Fairbank, J. The Roland–Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef] [PubMed]
- Stratford, P.W.; Riddle, D.L. A Roland Morris Disability Questionnaire Target Value to Distinguish between Functional and Dysfunctional States in People with Low Back Pain. Physiother. Can. 2016, 68, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, M.; Barten, D.; Pisters, M.; Verheij, R. Current use of PROMs and factors associated with their use in patients with nonspecific low back pain. Learn. Health Syst. 2019, 3, e10194. [Google Scholar] [CrossRef] [PubMed]
- Stokes, O.M.; Cole, A.A.; Breakwell, L.M.; Lloyd, A.J.; Leonard, C.M.; Grevitt, M. Do we have the right PROMs for measuring outcomes in lumbar spinal surgery? Eur. Spine J. 2017, 26, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Östhols, S.; Boström, C.; Rasmussen-Barr, E. Clinical assessment and patient-reported outcome measures in low-back pain—A survey among primary health care physiotherapists. Disabil. Rehabil. 2019, 41, 2459–2467. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen-Barr, E.; Lindqvist, C.; Östhols, S.; Boström, C. Are patient reported outcome measures (PROMs) useful in low back pain? Experiences of physiotherapists in primary health care in Sweden. Musculoskelet. Sci. Pract. 2021, 55, 102414. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Elfering, A.; Fekete, T.F.; Harding, I.J.; Monticone, M.; Obid, P.; Niemeyer, T.; Liljenqvist, U.; Boss, A.; Zimmermann, L.; et al. Shorter and sweeter: The 16-item version of the SRS questionnaire shows better structural validity than the 20-item version in young patients with spinal deformity. Spine Deform. 2022, 10, 1055–1062. [Google Scholar] [CrossRef] [PubMed]
- Damman, O.C.; Jani, A.; de Jong, B.A.; Becker, A.; Metz, M.J.; de Bruijne, M.C.; Timmermans, D.R.; Cornel, M.C.; Ubbink, D.T.; van der Steen, M.; et al. The use of PROMs and shared decision-making in medical encounters with patients: An opportunity to deliver value-based health care to patients. J. Eval. Clin. Pract. 2020, 26, 524–540. [Google Scholar] [CrossRef]
- Field, J.; Holmes, M.M.; Newell, D. PROMs data: Can it be used to make decisions for individual patients? A narrative review. Patient Relat. Outcome Meas. 2019, 10, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Ambrosini, E.; Rocca, B.; Cazzaniga, D.; Liquori, V.; Foti, C. Group-based task-oriented exercises aimed at managing kinesiophobia improved disability in chronic low back pain. Eur. J. Pain. 2016, 20, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Vlaeyen, J.W.S.; Kole-Snijders, A.M.J.; Boeren, R.G.B.; van Eek, H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain 1995, 62, 363–372. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. Declaration of Helsinki. Law Med. Health Care 1991, 19, 264–265. [Google Scholar] [CrossRef]
- Padua, R.; Padua, L.; Ceccarelli, E.; Romanini, E.; Zanoli, G.; Bondì, R.; Campi, A. Italian version of the Roland Disability Questionnaire, specific for low back pain: Cross-cultural adaptation and validation. Eur. Spine J. 2002, 11, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Monticone, M.; Baiardi, P.; Ferrari, S.; Foti, C.; Mugnai, R.; Pillastrini, P.; Vanti, C.; Zanoli, G. Development of the Italian Version of the Oswestry Disability Index (ODI-I): A Cross-Cultural Adaptation, Reliability, and Validity Study. Spine 2009, 34, 2090–2095. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain. 2004, 8, 283–291. [Google Scholar] [CrossRef]
- Monticone, M.; Galeoto, G.; Berardi, A.; Tofani, M. Psychometric properties of assessment tools. In Measuring Spinal Cord Injury: A Practical Guide of Outcome Measures; Springer: Cham, Switzerland, 2021; pp. 7–15. [Google Scholar]
- De Vet, H.C.; Terwee, C.B.; Mokkink, L.B.; Knol, D.L. Measurement in Medicine: A Practical Guide; Cambridge University Press: Cambridge, UK, 2011. [Google Scholar]
- Serdar, C.C.; Cihan, M.; Yücel, D.; Serdar, M.A. Sample size, power and effect size revisited: Simplified and practical approaches in pre-clinical, clinical and laboratory studies. Biochem. Med. 2021, 31, 27–53. [Google Scholar] [CrossRef]
- Massé-Alarie, H.; Angarita-Fonseca, A.; Lacasse, A.; Pagé, M.G.; Tétreault, P.; Fortin, M.; on behalf of the Quebec. Low back pain definitions: Effect on patient inclusion and clinical profiles. Pain Rep. 2022, 7, e997. [Google Scholar] [CrossRef] [PubMed]
- Iles, R.A.; Taylor, N.F.; Davidson, M.; O’Halloran, P.D. Patient recovery expectations in non-chronic non-specific low back pain: A qualitative investigation. J. Rehabil. Med. 2012, 44, 781–787. [Google Scholar] [CrossRef]
- Paolucci, T.; Zangrando, F.; Iosa, M.; De Angelis, S.; Marzoli, C.; Piccinini, G.; Saraceni, V.M. Improved interoceptive awareness in chronic low back pain: A comparison of Back school versus Feldenkrais method. Disabil. Rehabil. 2017, 39, 994–1001. [Google Scholar] [CrossRef] [PubMed]
- Bailly, F.; Trouvin, A.-P.; Bercier, S.; Dadoun, S.; Deneuville, J.-P.; Faguer, R.; Fassier, J.-B.; Koleck, M.; Lassalle, L.; Vraux, T.L.; et al. Clinical guidelines and care pathway for management of low back pain with or without radicular pain. Jt. Bone Spine 2021, 88, 105227. [Google Scholar] [CrossRef]
- Nicholas, M.K. The pain self-efficacy questionnaire: Taking pain into account. Eur. J. Pain. 2007, 11, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Robinson, M.E.; Riley, J.L.; Myers, C.D.; Sadler, I.J.; Kvaal, S.A.; Geisser, M.E.; Keefe, F.J. The Coping Strategies Questionnaire: A Large Sample Item Level Factor Analysis. Clin. J. Pain. 1997, 13, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item Short-Form Health Survey (SF-36). Med. Care 1992, 30, 437–483. [Google Scholar] [CrossRef]
| Age (years), mean ± SD | 53.03 ± 15.25 | |
| Gender (n) | Male | 22 (29.7%) |
| Female | 52 (70.3%) | |
| Marital status (n) | Married | 47 (63.5%) |
| Single | 17 (23%) | |
| Divorced | 5 (6.8%) | |
| Widowed | 5 (6.8%) | |
| Employment (n) | Students | 4 (5.4%) |
| Employed | 43 (58.1%) | |
| Self-employed | 6 (8.1%) | |
| Domestic works | 3 (4.1%) | |
| Retired | 17 (23%) | |
| Missing | 1 (1.4%) | |
| Education level (n) | Primary school | 5 (6.8%) |
| Middle school | 7 (9.5%) | |
| High school | 32 (43.2%) | |
| University | 30 (40.5%) | |
| Smokers (n) | Yes | 19 (25.7%) |
| No | 55 (74.3%) | |
| Alcohol (n) | Yes | 20 (27%) |
| No | 54 (73%) | |
| Physical activity (n) | Yes | 40 (54.1%) |
| No | 34 (45.9%) | |
| Comorbidities (n) | None | 53 (71.6%) |
| Cardiac | 8 (10.8%) | |
| Respiratory | 4 (5.4%) | |
| Gastrointestinal | 4 (5.4%) | |
| Renal | 1 (1.4%) | |
| Headache | 4 (5.4%) | |
| Body Mass Index (kg/m2), mean ± SD | 25.14 ± 3.86 | |
| Mean | SD | 25th% | 50th% | 75th% | Floor Effect [%] | Ceiling Effect [%] | |
|---|---|---|---|---|---|---|---|
| RM-18 (0–18) | 7.31 | 5.64 | 2 | 6 | 13 | 0 | 0 |
| RMQ (0–24) | 8.47 | 6.53 | 3 | 7 | 14.25 | 0 | 0 |
| ODI (0–50) | 12.14 | 9.41 | 4.75 | 9 | 17 | 0 | 0 |
| NRS (0–10) | 4.59 | 2.36 | 3 | 5 | 6.25 | 0 | 0 |
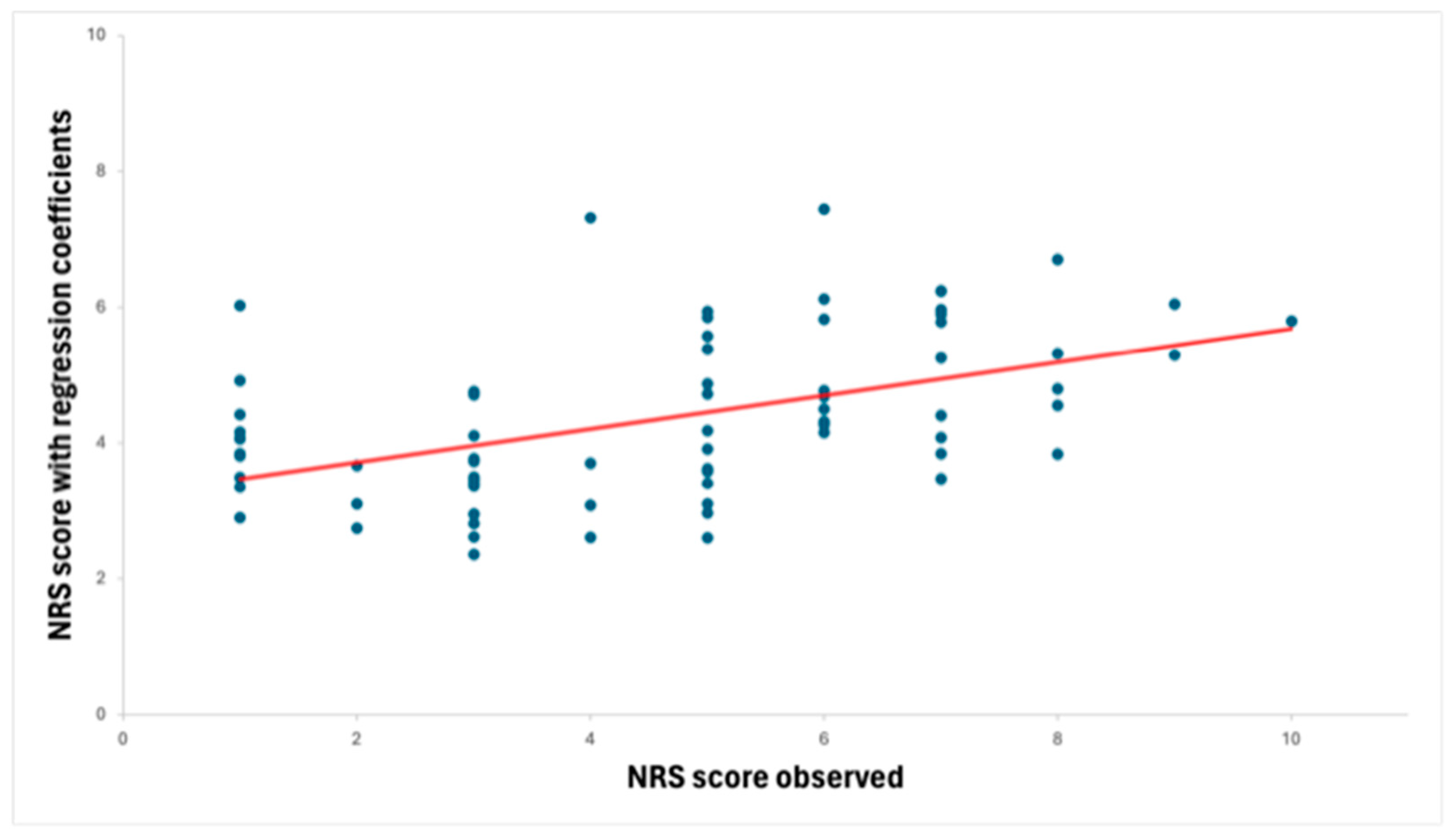
| Outcome | Determinants | Coefficient | 95% CI | t | p Value |
|---|---|---|---|---|---|
| NRS | RM-18 | 0.162 | 0.061–0.263 | 3.209 | 0.002 |
| Age | 0.045 | 0.010–0.081 | 2.524 | 0.014 | |
| Pain Duration | −0.001 | −0.005–0.003 | −0.397 | 0.692 | |
| Constant | 1.091 | −0.624–2.806 | −0.269 | 0.209 |
| Outcome | Determinants | Coefficient | 95% CI | t | p Value |
|---|---|---|---|---|---|
| NRS | RMQ | 0.139 | 0.050–0.228 | 3.125 | 0.003 |
| Age | 0.047 | 0.011–0.083 | 2.620 | 0.011 | |
| Pain Duration | −0.001 | −0.006–0.003 | 2.620 | 0.596 | |
| Constant | 1.043 | −0.676–2.762 | 1.210 | 0.230 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paolucci, T.; Pezzi, L.; Coraci, D.; Tognolo, L.; Pantalone, A.; Attanasi, C.; Graziani, G.; Dalla Costa, D.; Arippa, F.; Cichelli, A.; et al. Reliability, Concurrent Validity, and Clinical Performances of the Shorter Version of the Roland Morris Disability Questionnaire in a Sample of Italian People with Non-Specific Low Back Pain. J. Pers. Med. 2024, 14, 740. https://doi.org/10.3390/jpm14070740
Paolucci T, Pezzi L, Coraci D, Tognolo L, Pantalone A, Attanasi C, Graziani G, Dalla Costa D, Arippa F, Cichelli A, et al. Reliability, Concurrent Validity, and Clinical Performances of the Shorter Version of the Roland Morris Disability Questionnaire in a Sample of Italian People with Non-Specific Low Back Pain. Journal of Personalized Medicine. 2024; 14(7):740. https://doi.org/10.3390/jpm14070740
Chicago/Turabian StylePaolucci, Teresa, Letizia Pezzi, Daniele Coraci, Lucrezia Tognolo, Andrea Pantalone, Carmine Attanasi, Giancarlo Graziani, Davide Dalla Costa, Federico Arippa, Alice Cichelli, and et al. 2024. "Reliability, Concurrent Validity, and Clinical Performances of the Shorter Version of the Roland Morris Disability Questionnaire in a Sample of Italian People with Non-Specific Low Back Pain" Journal of Personalized Medicine 14, no. 7: 740. https://doi.org/10.3390/jpm14070740
APA StylePaolucci, T., Pezzi, L., Coraci, D., Tognolo, L., Pantalone, A., Attanasi, C., Graziani, G., Dalla Costa, D., Arippa, F., Cichelli, A., & Monticone, M. (2024). Reliability, Concurrent Validity, and Clinical Performances of the Shorter Version of the Roland Morris Disability Questionnaire in a Sample of Italian People with Non-Specific Low Back Pain. Journal of Personalized Medicine, 14(7), 740. https://doi.org/10.3390/jpm14070740










