Association between Cardiovascular Risk Assessment by SCORE2 and Diverticulosis: A Cross-Sectional Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Patient Assessment for Risk Factors
2.3. Assessment of Cardiovascular Risk
2.4. Assessment of Diverticulosis
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Timmis, A.; Vardas, P.; Townsend, N.; Torbica, A.; Katus, H.; De Smedt, D.; Gale, C.P.; Maggioni, A.P.; Petersen, S.E.; Huculeci, R.; et al. European Society of Cardiology: Cardiovascular disease statistics 2021. Eur. Heart J. 2022, 43, 716–799. [Google Scholar] [CrossRef]
- Schultz, J.K.; Azhar, N.; Binda, G.A.; Barbara, G.; Biondo, S.; Boermeester, M.A.; Chabok, A.; Consten, E.C.J.; van Dijk, S.T.; Johanssen, A.; et al. European Society of Coloproctology: Guidelines for the management of diverticular disease of the colon. Color. Dis. 2020, 22 (Suppl. 2), 5–28. [Google Scholar] [CrossRef] [PubMed]
- Tursi, A.; Scarpignato, C.; Strate, L.L.; Lanas, A.; Kruis, W.; Lahat, A.; Danese, S. Colonic diverticular disease. Nat. Rev. Dis. Primers 2020, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Munie, S.T.; Nalamati, S.P.M. Epidemiology and Pathophysiology of Diverticular Disease. Clin. Colon. Rectal Surg. 2018, 31, 209–213. [Google Scholar]
- Etzioni, D.A.; Mack, T.M.; Beart, R.W., Jr.; Kaiser, A.M. Diverticulitis in the United States: 1998–2005: Changing Patterns of Disease and Treatment. Ann. Surg. 2009, 249, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Schafmayer, C.; Harrison, J.W.; Buch, S.; Lange, C.; Reichert, M.C.; Hofer, P.; Cossais, F.; Kupcinskas, J.; von Schönfels, W.; Schniewind, B.; et al. Genome-wide association analysis of diverticular disease points towards neuromuscular, connective tissue and epithelial pathomechanisms. Gut 2019, 68, 854–865. [Google Scholar] [CrossRef]
- Peery, A.F.; Keku, T.O.; Martin, C.F.; Eluri, S.; Runge, T.; Galanko, J.A.; Sandler, R.S. Distribution and Characteristics of Colonic Diverticula in a United States Screening Population. Clin. Gastroenterol. Hepatol. 2016, 14, 980–985.e1. [Google Scholar] [CrossRef] [PubMed]
- Tursi, A.; Violi, A.; Cambie’, G.; Franceschi, M.; Baldassarre, G.; Rodriguez, K.I.; Miraglia, C.; Brandimarte, G.; Elisei, W.; Picchio, M.; et al. Risk factors for endoscopic severity of diverticular disease of the colon and its outcome: A real-life case-control study. Eur. J. Gastroenterol. Hepatol. 2020, 32, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.P.; Ahn, Y.W.; Lee, O.Y.; Lee, K.N. The relationship between colonic diverticulosis and abdominal visceral and subcutaneous fat accumulation measured by abdominal C.T. scan. Turk. J. Gastroenterol. 2014, 25, 192–197. [Google Scholar]
- Bae, H.J.; Kim, S.T.; Hong, S.G.; Lee, H.; Choi, H.S.; Cho, Y.-K.; Kim, T.H.; Chung, S.H. Risk Factors for Asymptomatic Colon Diverticulosis. Korean J. Gastroenterol. 2019, 74, 142–148. [Google Scholar] [CrossRef]
- Kempiński, R.; Łukawska, A.; Krzyżanowski, F.; Ślósarz, D.; Poniewierka, E. Clinical outcomes of non-alcoholic fatty liver disease: Polish-case control study. Adv. Clin. Exp. Med. 2019, 28, 1615–1620. [Google Scholar] [CrossRef]
- Wlodarczyk, J.R.; Yoon, D.; Owens, J.; Ershadi, S.; Lee, S.W.; Cologne, K.G.; Koller, S.E. Prevalence of and Risk Factors for Incidental Colonic Diverticulosis. J. Surg. Res. 2022, 280, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Peery, A.F. Colonic Diverticula and Diverticular Disease: 10 Facts Clinicians Should Know. N. C. Med. J. 2016, 77, 220–222. [Google Scholar] [CrossRef] [PubMed]
- Rustom, L.B.O.; Sharara, A.I. The Natural History of Colonic Diverticulosis: Much Ado about Nothing? Inflamm. Intest. Dis. 2018, 3, 69–74. [Google Scholar] [CrossRef]
- Peery, A.F.; Keku, T.O.; Addamo, C.; McCoy, A.N.; Martin, C.F.; Galanko, J.A.; Sandler, R.S. Colonic Diverticula Are Not Associated with Mucosal Inflammation or Chronic Gastrointestinal Symptoms. Clin. Gastroenterol. Hepatol. 2018, 16, 884–891.e1. [Google Scholar] [CrossRef]
- Violi, A.; Cambiè, G.; Miraglia, C.; Barchi, A.; Nouvenne, A.; Capasso, M.; Leandro, G.; Meschi, T.; De’ Angelis, G.L.; Di Mario, F. Epidemiology and risk factors for diverticular disease. Acta Biomed. 2018, 89 (Suppl. 9), 107–112. [Google Scholar] [PubMed]
- Peery, A.F.; Shaukat, A.; Strate, L.L. AGA Clinical Practice Update on Medical Management of Colonic Diverticulitis: Expert Review. Gastroenterology 2021, 160, 906–911.e1. [Google Scholar] [CrossRef]
- Shahedi, K.; Fuller, G.; Bolus, R.; Cohen, E.; Vu, M.; Shah, R.; Agarwal, N.; Kaneshiro, M.; Atia, M.; Sheen, V.; et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin. Gastroenterol. Hepatol. 2013, 11, 1609–1613. [Google Scholar] [CrossRef]
- Stollman, N.; Smalley, W.; Hirano, I. AGA Institute Clinical Guidelines Committee. American Gastroenterological Association Institute Guideline on the Management of Acute Diverticulitis. Gastroenterology 2015, 149, 1944–1949. [Google Scholar] [CrossRef]
- Strate, L.L. Lifestyle factors and the course of diverticular disease. Dig. Dis. 2012, 30, 35–45. [Google Scholar] [CrossRef]
- Peery, A.F.; Crockett, S.D.; Murphy, C.C.; Jensen, E.T.; Kim, H.P.; Egberg, M.D.; Lund, J.L.; Moon, A.M.; Pate, V.; Barnes, E.L.; et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2021. Gastroenterology 2022, 162, 621–644. [Google Scholar] [CrossRef] [PubMed]
- Wernly, S.; Semmler, G.; Völkerer, A.; Rezar, R.; Datz, L.; Radzikowski, K.; Stickel, F.; Aigner, E.; Niederseer, D.; Wernly, B.; et al. Cardiovascular Risk Assessment by SCORE2 Predicts Risk for Colorectal Neoplasia and Tumor-Related Mortality. J. Pers. Med. 2022, 12, 848. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar]
- SCORE2 working group and ESC Cardiovascular risk collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef] [PubMed]
- Bisschops, R.; Areia, M.; Coron, E.; Dobru, D.; Kaskas, B.; Kuvaev, R.; Pech, O.; Ragunath, K.; Weusten, B.; Familiari, P.; et al. Performance measures for upper gastrointestinal endoscopy: A European Society of Gastrointestinal Endoscopy (E.S.G.E.) Quality Improvement Initiative. Endoscopy 2016, 48, 843–864. [Google Scholar]
- Ukashi, O.; Pflantzer, B.; Barash, Y.; Klang, E.; Segev, S.; Ozeri, D.J.; Veisman, I.; Lahat, A.; Laish, I.; Kopylov, U.; et al. Cardiovascular Risk Factors and Physical Fitness Among Subjects with Asymptomatic Colonic Diverticulosis. Dig. Dis. Sci. 2022, 68, 902–912. [Google Scholar] [CrossRef] [PubMed]
- Tam, I.; Liu, P.-H.; Ma, W.; Cao, Y.; Jovani, M.; Wu, K.; Rimm, E.B.; Strate, L.L.; Giovannucci, E.L.; Chan, A.T. History of Diverticulitis and Risk of Incident Cardiovascular Disease in Men: A Cohort Study. Dig. Dis. Sci. 2022, 67, 1337–1344. [Google Scholar] [CrossRef]
- Strate, L.L.; Erichsen, R.; Horváth-Puhó, E.; Pedersen, L.; Baron, J.A.; Sørensen, H.T. Diverticular disease is associated with increased risk of subsequent arterial and venous thromboembolic events. Clin. Gastroenterol. Hepatol. 2014, 12, 1695–1701.e1. [Google Scholar] [CrossRef]
- Tursi, A.; Elisei, W. Role of Inflammation in the Pathogenesis of Diverticular Disease. Mediat. Inflamm. 2019, 2019, 8328490. [Google Scholar] [CrossRef]
- Alfaddagh, A.; Martin, S.S.; Leucker, T.M.; Michos, E.D.; Blaha, M.J.; Lowenstein, C.J.; Jones, S.R.; Toth, P.P. Inflammation and cardiovascular disease: From mechanisms to therapeutics. Am. J. Prev. Cardiol. 2020, 4, 100130. [Google Scholar] [CrossRef]
- Wang, Z.; Klipfell, E.; Bennett, B.J.; Koeth, R.; Levison, B.S.; DuGar, B.; Feldstein, A.E.; Britt, E.B.; Fu, X.; Chung, Y.-M.; et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011, 472, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Chistiakov, D.A.; Bobryshev, Y.V.; Kozarov, E.; Sobenin, I.A.; Orekhov, A.N. Role of gut microbiota in the modulation of atherosclerosis-associated immune response. Front. Microbiol. 2015, 6, 671. [Google Scholar] [CrossRef] [PubMed]
- West, A.B. The pathology of diverticulitis. J. Clin. Gastroenterol. 2008, 42, 1137–1138. [Google Scholar] [CrossRef] [PubMed]
- Storz, C.; Rothenbacher, T.; Rospleszcz, S.; Linseisen, J.; Messmann, H.; De Cecco, C.N.; Machann, J.; Lorbeer, R.; Kiefer, L.S.; Wintermeyer, E.; et al. Characteristics and associated risk factors of diverticular disease assessed by magnetic resonance imaging in subjects from a Western general population. Eur. Radiol. 2019, 29, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Li, A.; Yan, J.; Zhao, Y.; Yu, Z.; Tian, S.; Khan, A.H.; Zhu, Y.; Wu, A.; Zhang, C.; Tian, X.-L. Vascular Aging: Assessment and Intervention. Clin. Interv. Aging 2023, 18, 1373–1395. [Google Scholar] [CrossRef] [PubMed]
- Völkerer, A.; Wernly, S.; Semmler, G.; Flamm, M.; Aigner, E.; Datz, C.; Wernly, B. Diverticulosis and cardiometabolic risk factors: A systematic literature review. Int. J. Color. Dis. 2023, 38, 236. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics-2023 Update: A Report from the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef] [PubMed]

| Total | Low–Moderate Risk | High Risk | Very High Risk | p-Value | |
|---|---|---|---|---|---|
| N = 3935 | N = 1512 | N = 1651 | N = 772 | ||
| AGE | 56 (51–61) | 53 (50–56) | 57 (51–62) | 63 (58–67) | <0.001 |
| <50 | 17% (685) | 21% (321) | 19% (318) | 6% (46) | |
| 50–69 | 83% (3250) | 79% (1191) | 81% (1333) | 94% (726) | |
| SEX | <0.001 | ||||
| Female | 45% (1756) | 71% (1080) | 32% (525) | 20% (151) | |
| Male | 55% (2179) | 29% (432) | 68% (1126) | 80% (621) | |
| BMI | 26 (24–30) | 25 (22–28) | 27 (25–30) | 28 (26–32) | <0.001 |
| BMI ≥ 30 | 23% (913) | 14% (217) | 24% (403) | 38% (293) | |
| BMI 25 to <29 | 41% (1616) | 34% (512) | 47% (774) | 43% (330) | |
| BMI < 25 | 36% (1406) | 52% (783) | 29% (474) | 19% (149) | |
| Hypertension | 53% (2088) | 31% (464) | 59% (980) | 83% (644) | <0.001 |
| RR ≥ 140 or ≥90 mmHg | 43% (1689) | 23% (355) | 47% (783) | 71% (551) | |
| RR intermediate | 53% (2070) | 69% (1045) | 49% (816) | 27% (209) | |
| RR < 120/80 mmHg | 4% (176) | 7% (112) | 3% (52) | 2% (12) | |
| Kreatinin | 0.9 (0.8–1.0) | 0.8 (0.8–0.9) | 0.9 (0.8–1.0) | 0.9 (0.8–1.0) | <0.001 |
| HGB | 14.7 (13.9–15.5) | 14.2 (13.5–14.9) | 15.0 (14.3–15.7) | 15.2 (14.3–15.9) | <0.001 |
| MCV | 87 (85–90) | 87 (84–90) | 87 (85–89) | 88 (85–90) | 0.003 |
| Thrombo | 232 (201–270) | 243 (211–278) | 229 (198–265) | 219 (190–258) | <0.001 |
| Leuko | 5.8 (4.9–7.0) | 5.5 (4.7–6.5) | 5.8 (5.0–7.1) | 6.4 (5.3–7.6) | <0.001 |
| CRP | 0.2 (0.1–0.3) | 0.1 (0.1–0.3) | 0.2 (0.1–0.3) | 0.2 (0.1–0.5) | <0.001 |
| BSG | 5 (2–9) | 5 (2–8) | 5 (2–8) | 6 (3–10) | <0.001 |
| Cholesterin | 221 (193–249) | 218 (192–244) | 224 (197–253) | 218 (186–254) | <0.001 |
| Cholesterol ≥ 240 mg/dL | 33% (1290) | 30% (451) | 36% (587) | 33% (252) | |
| Cholesterol 200 to 239 mg/dL or treated | 46% (1793) | 43% (647) | 46% (761) | 50% (385) | |
| Cholesterol < 200 or untreated | 22% (852) | 27% (414) | 18% (303) | 17% (135) | |
| LDL | 141 (117–168) | 136 (113–159) | 147 (123–173) | 143 (114–173) | <0.001 |
| HDL | 55 (46–66) | 63 (53–74) | 52 (45–62) | 47 (40–56) | <0.001 |
| Metabolic syndrome | 77% (3013) | 62% (937) | 82% (1360) | 93% (716) | <0.001 |
| Smoking status | <0.001 | ||||
| Never smoker | 31% (1222) | 39% (584) | 28% (468) | 22% (170) | |
| Ex-smoker | 42% (1636) | 47% (705) | 41% (673) | 34% (258) | |
| Active smoker | 27% (1064) | 14% (217) | 31% (505) | 44% (342) |
| (a) | Low–Moderate Risk | High Risk | Very High Risk | p-Value |
|---|---|---|---|---|
| N = 1512 | N = 1651 | N = 772 | ||
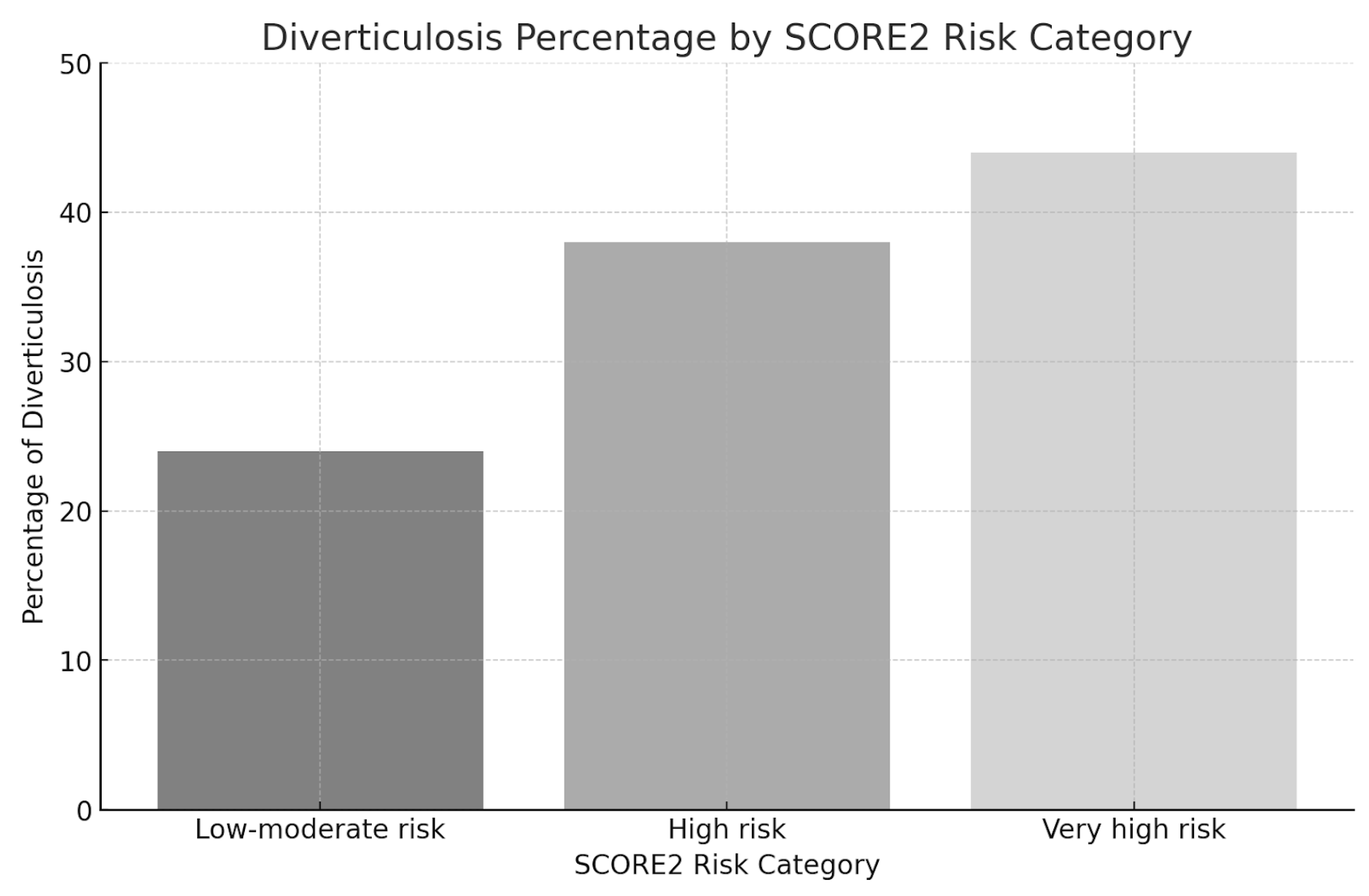
| Diverticulosis | 24% (357) | 38% (630) | 44% (339) | <0.001 |
| No diverticulosis | 76% (1155) | 62% (1021) | 56% (433) | |
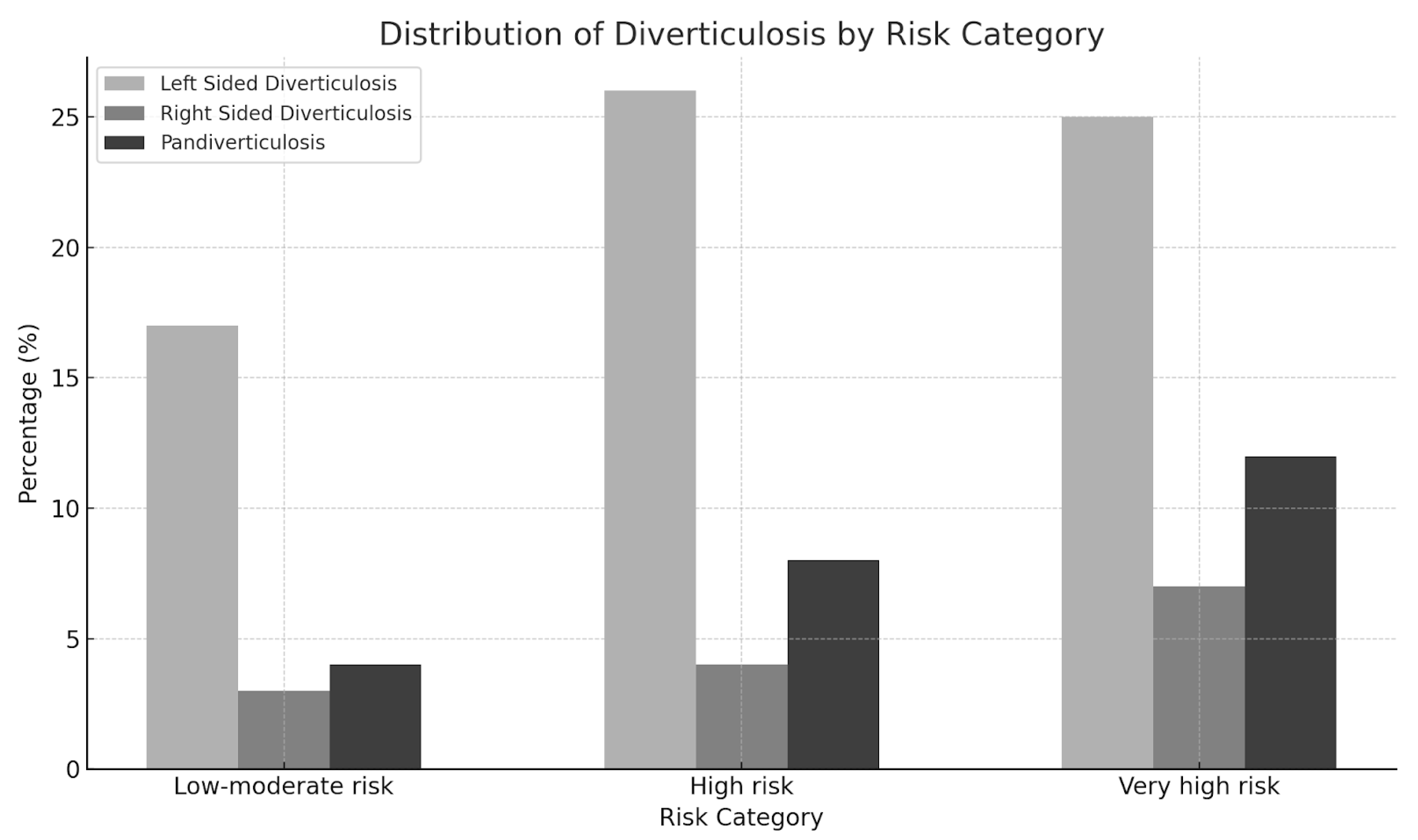
| Left-sided diverticulosis | 17% (253) | 26% (427) | 25% (193) | |
| Right-sided diverticulosis | 3% (40) | 4% (71) | 7% (53) | |
| Pandiverticulosis | 4% (64) | 8% (132) | 12% (93) | |
| (b) | Low–Moderate Risk | High Risk | Very High Risk | |
| OR | OR | |||
| Diverticulosis | ref | 1.99 | 2.53 | |
| No diverticulosis | ref | 0.50 | 0.40 | |
| Left-sided diverticulosis | ref | 1.74 | 1.66 | |
| Right-sided diverticulosis | ref | 1.66 | 2.71 | |
| Pandiverticulosis | ref | 1.97 | 3.10 |
| Low/Moderate Risk | High Risk | Very High Risk | R2 | |
|---|---|---|---|---|
| Model-1 | Ref. | OR 2.00; 95%CI 1.71–2.33; p < 0.001 | OR 2.53; 95%CI 2.10–3.05; p < 0.001 | 0.0243 |
| Model-2 | Ref. | aOR 1.86; 95%CI 1.59–2.18; p < 0.001 | aOR 2.27; 95%CI 1.88–2.75; p < 0.001 | 0.0280 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Völkerer, A.; Wernly, S.; Semmler, G.; Flamm, M.; Radzikowski, K.; Datz, L.; Götz, N.; Hofer, H.; Aigner, E.; Datz, C.; et al. Association between Cardiovascular Risk Assessment by SCORE2 and Diverticulosis: A Cross-Sectional Analysis. J. Pers. Med. 2024, 14, 862. https://doi.org/10.3390/jpm14080862
Völkerer A, Wernly S, Semmler G, Flamm M, Radzikowski K, Datz L, Götz N, Hofer H, Aigner E, Datz C, et al. Association between Cardiovascular Risk Assessment by SCORE2 and Diverticulosis: A Cross-Sectional Analysis. Journal of Personalized Medicine. 2024; 14(8):862. https://doi.org/10.3390/jpm14080862
Chicago/Turabian StyleVölkerer, Andreas, Sarah Wernly, Georg Semmler, Maria Flamm, Konrad Radzikowski, Leonora Datz, Nikolaus Götz, Hannah Hofer, Elmar Aigner, Christian Datz, and et al. 2024. "Association between Cardiovascular Risk Assessment by SCORE2 and Diverticulosis: A Cross-Sectional Analysis" Journal of Personalized Medicine 14, no. 8: 862. https://doi.org/10.3390/jpm14080862
APA StyleVölkerer, A., Wernly, S., Semmler, G., Flamm, M., Radzikowski, K., Datz, L., Götz, N., Hofer, H., Aigner, E., Datz, C., & Wernly, B. (2024). Association between Cardiovascular Risk Assessment by SCORE2 and Diverticulosis: A Cross-Sectional Analysis. Journal of Personalized Medicine, 14(8), 862. https://doi.org/10.3390/jpm14080862







