Proteomics in Diagnostic Evaluation and Treatment of Breast Cancer: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search
2.3. Selection of Sources of Evidence
2.4. Data Charting Process, Data Items, and Synthesis of Results
3. Results
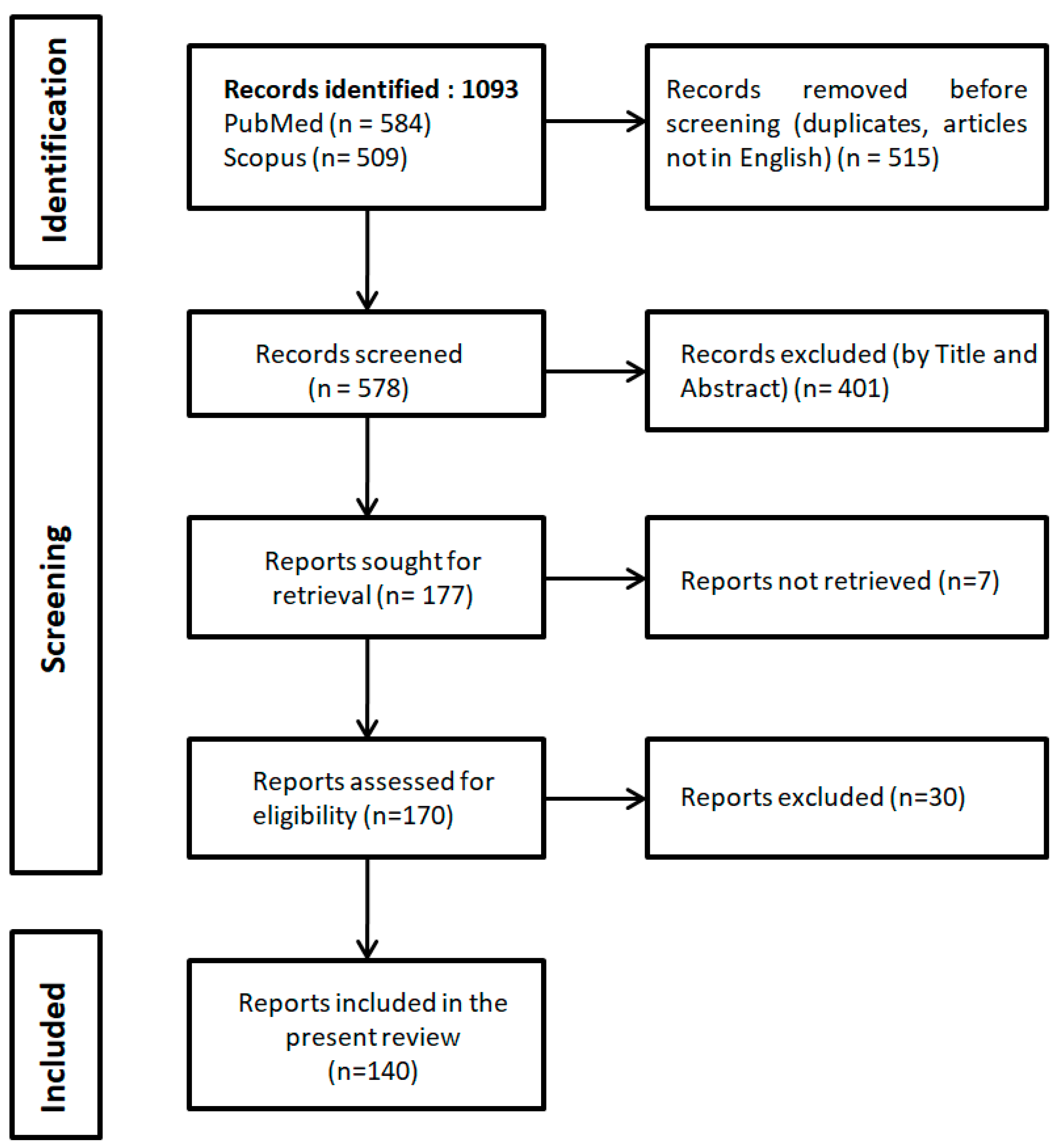
3.1. Search Results
3.2. Year of Publication and Geographical Area of Included Studies
3.3. Clinical Application, Disease Stage and Specimen Type of Included Studies
3.3.1. Proteomic Studies in Breast Cancer Tissue
3.3.2. Proteomic Studies in Plasma and Serum from Breast Cancer Patients
3.3.3. Proteomic Studies in Other Biologic Material from Breast Cancer Patients
3.4. Possible Clinical Use of Biomarkers Identified by the Included Studies
3.5. Overview of the Most Important Findings from the Largest Studies and the Most Commonly Used Proteomic Platforms Across the Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Giaquinto, A.N.; Sung, H.; Newman, L.A.; Freedman, R.A.; Smith, R.A.; Star, J.; Jemal, A.; Siegel, R.L. Breast cancer statistics 2024. CA Cancer J. Clin. 2024, 74, 477–495. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; McCarron, P.; Parkin, D.M. The changing global patterns of female breast cancer incidence and mortality. Breast Cancer Res. 2004, 6, 229–239. [Google Scholar] [CrossRef]
- van ‘t Veer, L.J.; Dai, H.; van de Vijver, M.J.; He, Y.D.; Hart, A.A.M.; Mao, M.; Peterse, H.L.; van der Kooy, K.; Marton, M.J.; Witteveen, A.T.; et al. Gene expression profiling predicts clinical outcome of breast cancer. Nature 2002, 415, 530–536. [Google Scholar] [CrossRef]
- van de Vijver, M.J.; He, Y.D.; van’t Veer, L.J.; Dai, H.; Hart, A.A.M.; Voskuil, D.W.; Schreiber, G.J.; Peterse, J.L.; Roberts, C.; Marton, M.J.; et al. A gene expression signature as a predictor of survival in breast cancer. N. Engl. J. Med. 2002, 347, 1999–2009. [Google Scholar] [CrossRef]
- Goldhirsch, A.; Winer, E.P.; Coates, A.S.; Gelber, R.D.; Piccart-Gebhart, M.; Thürlimann, B.; Senn, H.-J.; Panel members. Personalizing the treatment of women with early breast cancer: Highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann. Oncol. 2013, 24, 2206–2223. [Google Scholar] [CrossRef]
- Zeng, C.; Zhang, J. A narrative review of five multigenetic assays in breast cancer. Transl. Cancer Res. 2022, 11, 897–907. [Google Scholar] [CrossRef]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Breast Cancer Screening and Diagnosis Version 6.2024—November 11, 2024. Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1419 (accessed on 12 January 2025).
- Geisow, M.J. Proteomics: One small step for a digital computer, one giant leap for humankind. Nat. Biotechnol. 1998, 16, 206. [Google Scholar] [CrossRef]
- Anderson, N.L.; Anderson, N.G. Proteome and proteomics: New technologies, new concepts, and new words. Electrophoresis 1998, 19, 1853–1861. [Google Scholar] [CrossRef]
- Brožová, K.; Hantusch, B.; Kenner, L.; Kratochwill, K. Spatial Proteomics for the Molecular Characterization of Breast Cancer. Rev. Proteomes 2023, 11, 17. [Google Scholar] [CrossRef]
- Neagu, A.N.; Jayathirtha, M.; Whitham, D.; Mutsengi, P.; Sullivan, I.; Petre, B.A.; Darie, C.C. Proteomics-Based Identification of Dysregulated Proteins in Breast Cancer. Proteomes 2022, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Abdullah Al-Dhabi, N.; Srigopalram, S.; Ilavenil, S.; Kim, Y.O.; Agastian, P.; Baaru, R.; Balamurugan, K.; Choi, K.C.; Valan Arasu, M. Proteomic Analysis of Stage-II Breast Cancer from Formalin-Fixed Paraffin-Embedded Tissues. Biomed Res. Int. 2016, 2016, 3071013. [Google Scholar] [CrossRef] [PubMed]
- Akcakanat, A.; Zheng, X.; Cruz Pico, C.X.; Kim, T.B.; Chen, K.; Korkut, A.; Sahin, A.; Holla, V.; Tarco, E.; Singh, G.; et al. Genomic, Transcriptomic, and Proteomic Profiling of Metastatic Breast Cancer. Clin. Cancer Res. 2021, 27, 3243–3252. [Google Scholar] [CrossRef]
- Akpinar, G.; Simsek, T.; Guler, A.; Kasap, M.; Canturk, N.Z. Elucidation of a Conserved Proteomic Pattern of Breast Cancer Tissue and Metastatic Axillary Lymph Node. Chirurgia 2017, 112, 443–448. [Google Scholar] [CrossRef]
- Alvarez, F.A.; Kaddour, H.; Lyu, Y.; Preece, C.; Cohen, J.; Baer, L.; Stopeck, A.T.; Thompson, P.; Okeoma, C.M. Blood plasma derived extracellular vesicles (BEVs): Particle purification liquid chromatography (PPLC) and proteomic analysis reveals BEVs as a potential minimally invasive tool for predicting response to breast cancer treatment. Breast Cancer Res. Treat. 2022, 196, 423–437. [Google Scholar] [CrossRef]
- Al-Wajeeh, A.S.; Salhimi, S.M.; Al-Mansoub, M.A.; Khalid, I.A.; Harvey, T.M.; Latiff, A.; Ismail, M.N. Comparative proteomic analysis of different stages of breast cancer tissues using ultra high performance liquid chromatography tandem mass spectrometer. PLoS ONE 2020, 15, e0227404. [Google Scholar] [CrossRef]
- An, R.; Yu, H.; Wang, Y.; Lu, J.; Gao, Y.; Xie, X.; Zhang, J. Integrative analysis of plasma metabolomics and proteomics reveals the metabolic landscape of breast cancer. Cancer Metab. 2022, 10, 13. [Google Scholar] [CrossRef]
- Asleh, K.; Negri, G.L.; Spencer Miko, S.E.; Colborne, S.; Hughes, C.S.; Wang, X.Q.; Gao, D.; Gilks, C.B.; Chia, S.K.L.; Nielsen, T.O.; et al. Proteomic analysis of archival breast cancer clinical specimens identifies biological subtypes with distinct survival outcomes. Nat. Commun. 2022, 13, 896. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, A.L.K.; Gomig, T.H.B.; Batista, M.; Marchini, F.K.; Spautz, C.C.; Rabinovich, I.; Sebastião, A.P.M.; Oliveira, J.C.; Gradia, D.F.; Cavalli, I.J.; et al. High-throughput proteomics of breast cancer subtypes: Biological characterization and multiple candidate biomarker panels to patients’ stratification. J. Proteom. 2023, 285, 104955. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, A.L.K.; Gomig, T.H.B.; Giner, I.S.; Batista, M.; Marchini, F.K.; Lima, R.S.; Urban, C.A.; Sebastião, A.P.M.; Cavalli, I.J.; Ribeiro, E.M.S.F. Comprehensive analysis of the large and small ribosomal proteins in breast cancer: Insights on proteomic and transcriptomic expression patterns, regulation, mutational landscape, and prognostic significance. Comput. Biol. Chem. 2022, 100, 107746. [Google Scholar] [CrossRef] [PubMed]
- Bateman, N.W.; Sun, M.; Bhargava, R.; Hood, B.L.; Darfler, M.M.; Kovatich, A.J.; Hooke, J.A.; Krizman, D.B.; Conrads, T.P. Differential proteomic analysis of late-stage and recurrent breast cancer from formalin-fixed paraffin-embedded tissues. J. Proteome Res. 2011, 10, 1323–1332. [Google Scholar] [CrossRef]
- Belluco, C.; Petricoin, E.F.; Mammano, E.; Facchiano, F.; Ross-Rucker, S.; Nitti, D.; Di Maggio, C.; Liu, C.; Lise, M.; Liotta, L.A.; et al. Serum proteomic analysis identifies a highly sensitive and specific discriminatory pattern in stage 1 breast cancer. Ann. Surg. Oncol. 2007, 14, 2470–2476. [Google Scholar] [CrossRef]
- Bera, A.; Russ, E.; Manoharan, M.S.; Eidelman, O.; Eklund, M.; Hueman, M.; Pollard, H.B.; Hu, H.; Shriver, C.D.; Srivastava, M. Proteomic Analysis of Inflammatory Biomarkers Associated with Breast Cancer Recurrence. Mil. Med. 2020, 185, 669–675. [Google Scholar] [CrossRef]
- Beretov, J.; Wasinger, V.C.; Millar, E.K.; Schwartz, P.; Graham, P.H.; Li, Y. Proteomic Analysis of Urine to Identify Breast Cancer Biomarker Candidates Using a Label-Free LC-MS/MS Approach. PLoS ONE 2015, 10, e0141876. [Google Scholar] [CrossRef]
- Bernhardt, S.; Bayerlová, M.; Vetter, M.; Wachter, A.; Mitra, D.; Hanf, V.; Lantzsch, T.; Uleer, C.; Peschel, S.; John, J.; et al. Proteomic profiling of breast cancer metabolism identifies SHMT2 and ASCT2 as prognostic factors. Breast Cancer Res. 2017, 19, 112. [Google Scholar] [CrossRef]
- Bjørnstad, O.V.; Carrasco, M.; Finne, K.; Ardawatia, V.; Winge, I.; Askeland, C.; Arnes, J.B.; Knutsvik, G.; Kleftogiannis, D.; Paulo, J.A.; et al. Global and single-cell proteomics view of the co-evolution between neural progenitors and breast cancer cells in a co-culture model. EBioMedicine 2024, 108, 105325. [Google Scholar] [CrossRef]
- Böhm, D.; Keller, K.; Pieter, J.; Boehm, N.; Wolters, D.; Siggelkow, W.; Lebrecht, A.; Schmidt, M.; Kölbl, H.; Pfeiffer, N.; et al. Comparison of tear protein levels in breast cancer patients and healthy controls using a de novo proteomic approach. Oncol. Rep. 2012, 28, 429–438. [Google Scholar] [CrossRef]
- Bonneterre, J.; Révillion, F.; Desauw, C.; Blot, E.; Kramar, A.; Fournier, C.; Hornez, L.; Peyrat, J.P. Plasma and tissue proteomic prognostic factors of response in primary breast cancer patients receiving neoadjuvant chemotherapy. Oncol. Rep. 2013, 29, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Bouchal, P.; Dvořáková, M.; Roumeliotis, T.; Bortlíček, Z.; Ihnatová, I.; Procházková, I.; Ho, J.T.; Maryáš, J.; Imrichová, H.; Budinská, E.; et al. Combined Proteomics and Transcriptomics Identifies Carboxypeptidase B1 and Nuclear Factor κB (NF-κB) Associated Proteins as Putative Biomarkers of Metastasis in Low Grade Breast Cancer. Mol. Cell Proteom. 2015, 14, 1814–1830. [Google Scholar] [CrossRef]
- Braakman, R.B.; Bezstarosti, K.; Sieuwerts, A.M.; de Weerd, V.; van Galen, A.M.; Stingl, C.; Luider, T.M.; Timmermans, M.A.; Smid, M.; Martens, J.W.; et al. Integrative analysis of genomics and proteomics data on clinical breast cancer tissue specimens extracted with acid guanidinium thiocyanate-phenol-chloroform. J. Proteome Res. 2015, 14, 1627–1636. [Google Scholar] [CrossRef]
- Brunoro, G.V.F.; Carvalho, P.C.; Barbosa, V.C.; Pagnoncelli, D.; De Moura Gallo, C.V.; Perales, J.; Zahedi, R.P.; Valente, R.H.; Neves-Ferreira, A.G.D.C. Differential proteomic comparison of breast cancer secretome using a quantitative paired analysis workflow. BMC Cancer 2019, 19, 365. [Google Scholar] [CrossRef]
- Cabezón, T.; Gromova, I.; Gromov, P.; Serizawa, R.; Timmermans Wielenga, V.; Kroman, N.; Celis, J.E.; Moreira, J.M. Proteomic profiling of triple-negative breast carcinomas in combination with a three-tier orthogonal technology approach identifies Mage-A4 as potential therapeutic target in estrogen receptor negative breast cancer. Mol. Cell Proteom. 2013, 12, 381–394. [Google Scholar] [CrossRef] [PubMed]
- Cancemi, P.; Di Cara, G.; Albanese, N.N.; Costantini, F.; Marabeti, M.R.; Musso, R.; Lupo, C.; Roz, E.; Pucci-Minafra, I. Large-scale proteomic identification of S100 proteins in breast cancer tissues. BMC Cancer 2010, 10, 476. [Google Scholar] [CrossRef] [PubMed]
- Cancemi, P.; Di Cara, G.; Albanese, N.N.; Costantini, F.; Marabeti, M.R.; Musso, R.; Riili, I.; Lupo, C.; Roz, E.; Pucci-Minafra, I. Differential occurrence of S100A7 in breast cancer tissues: A proteomic-based investigation. Proteom. Clin. Appl. 2012, 6, 364–373. [Google Scholar] [CrossRef]
- Cawthorn, T.R.; Moreno, J.C.; Dharsee, M.; Tran-Thanh, D.; Ackloo, S.; Zhu, P.H.; Sardana, G.; Chen, J.; Kupchak, P.; Jacks, L.M.; et al. Proteomic analyses reveal high expression of decorin and endoplasmin (HSP90B1) are associated with breast cancer metastasis and decreased survival. PLoS ONE 2012, 7, e30992. [Google Scholar] [CrossRef]
- Champattanachai, V.; Netsirisawan, P.; Chaiyawat, P.; Phueaouan, T.; Charoenwattanasatien, R.; Chokchaichamnankit, D.; Punyarit, P.; Srisomsap, C.; Svasti, J. Proteomic analysis and abrogated expression of O-GlcNAcylated proteins associated with primary breast cancer. Proteomics 2013, 13, 2088–2099. [Google Scholar] [CrossRef]
- Corrêa, S.; Panis, C.; Binato, R.; Herrera, A.C.; Pizzatti, L.; Abdelhay, E. Identifying potential markers in Breast Cancer subtypes using plasma label-free proteomics. J. Proteom. 2017, 151, 33–42. [Google Scholar] [CrossRef]
- Creighton, C.J.; Fu, X.; Hennessy, B.T.; Casa, A.J.; Zhang, Y.; Gonzalez-Angulo, A.M.; Lluch, A.; Gray, J.W.; Brown, P.H.; Hilsenbeck, S.G.; et al. Proteomic and transcriptomic profiling reveals a link between the PI3K pathway and lower estrogen-receptor (ER) levels and activity in ER+ breast cancer. Breast Cancer Res. 2010, 12, R40. [Google Scholar] [CrossRef] [PubMed]
- Dalenc, F.; Doisneau-Sixou, S.F.; Allal, B.C.; Marsili, S.; Lauwers-Cances, V.; Chaoui, K.; Schiltz, O.; Monsarrat, B.; Filleron, T.; Renée, N.; et al. Tipifarnib plus tamoxifen in tamoxifen-resistant metastatic breast cancer: A negative phase II and screening of potential therapeutic markers by proteomic analysis. Clin. Cancer Res. 2010, 16, 1264–1271. [Google Scholar] [CrossRef]
- Debets, D.O.; Stecker, K.E.; Piskopou, A.; Liefaard, M.C.; Wesseling, J.; Sonke, G.S.; Lips, E.H.; Altelaar, M. Deep (phospho)proteomics profiling of pre- treatment needle biopsies identifies signatures of treatment resistance in HER2+ breast cancer. Cell Rep. Med. 2023, 4, 101203. [Google Scholar] [CrossRef]
- Di Cara, G.; Marabeti, M.R.; Musso, R.; Riili, I.; Cancemi, P.; Pucci Minafra, I. New Insights into the Occurrence of Matrix Metalloproteases -2 and -9 in a Cohort of Breast Cancer Patients and Proteomic Correlations. Cells 2018, 7, 89. [Google Scholar] [CrossRef]
- Drukier, A.K.; Ossetrova, N.; Schors, E.; Krasik, G.; Grigoriev, I.; Koenig, C.; Sulkowski, M.; Holcman, J.; Brown, L.R.; Tomaszewski, J.E.; et al. High-sensitivity blood-based detection of breast cancer by multi photon detection diagnostic proteomics. J. Proteome Res. 2006, 5, 1906–1915. [Google Scholar] [CrossRef] [PubMed]
- Duan, J.; Zhao, Y.; Sun, Q.; Liang, D.; Liu, Z.; Chen, X.; Li, Z.C. Imaging-proteomic analysis for prediction of neoadjuvant chemotherapy responses in patients with breast cancer. Cancer Med. 2023, 12, 21256–21269. [Google Scholar] [CrossRef]
- Fernandez-Pol, J.A.; Hamilton, P.D.; Klos, D.J. Genomics, Proteomics and Cancer: Specific Ribosomal, Mitochondrial, and Tumor Reactive Proteins Can Be Used as Biomarkers for Early Detection of Breast Cancer in Serum. Cancer Genom. Proteom. 2005, 2, 1–24. [Google Scholar]
- Fonseca-Sánchez, M.A.; Rodríguez Cuevas, S.; Mendoza-Hernández, G.; Bautista-Piña, V.; Arechaga Ocampo, E.; Hidalgo Miranda, A.; Quintanar Jurado, V.; Marchat, L.A.; Alvarez-Sánchez, E.; Pérez Plasencia, C.; et al. Breast cancer proteomics reveals a positive correlation between glyoxalase 1 expression and high tumor grade. Int. J. Oncol. 2012, 41, 670–680. [Google Scholar] [CrossRef]
- Fredolini, C.; Pathak, K.V.; Paris, L.; Chapple, K.M.; Tsantilas, K.A.; Rosenow, M.; Tegeler, T.J.; Garcia-Mansfield, K.; Tamburro, D.; Zhou, W.; et al. Shotgun proteomics coupled to nanoparticle-based biomarker enrichment reveals a novel panel of extracellular matrix proteins as candidate serum protein biomarkers for early-stage breast cancer detection. Breast Cancer Res. 2020, 22, 135. [Google Scholar] [CrossRef]
- Gajbhiye, A.; Dabhi, R.; Taunk, K.; Jagadeeshaprasad, M.G.; RoyChoudhury, S.; Mane, A.; Bayatigeri, S.; Chaudhury, K.; Santra, M.K.; Rapole, S. Multipronged quantitative proteomics reveals serum proteome alterations in breast cancer intrinsic subtypes. J. Proteom. 2017, 163, 1–13. [Google Scholar] [CrossRef]
- Gajbhiye, A.; Dabhi, R.; Taunk, K.; Vannuruswamy, G.; RoyChoudhury, S.; Adhav, R.; Seal, S.; Mane, A.; Bayatigeri, S.; Santra, M.K.; et al. Urinary proteome alterations in HER2 enriched breast cancer revealed by multipronged quantitative proteomics. Proteomics 2016, 16, 2403–2418. [Google Scholar] [CrossRef] [PubMed]
- Gámez-Pozo, A.; Berges-Soria, J.; Arevalillo, J.M.; Nanni, P.; López-Vacas, R.; Navarro, H.; Grossmann, J.; Castaneda, C.A.; Main, P.; Díaz-Almirón, M.; et al. Combined Label-Free Quantitative Proteomics and microRNA Expression Analysis of Breast Cancer Unravel Molecular Differences with Clinical Implications. Cancer Res. 2015, 75, 2243–2253. [Google Scholar] [CrossRef]
- Gámez-Pozo, A.; Trilla-Fuertes, L.; Berges-Soria, J.; Selevsek, N.; López-Vacas, R.; Díaz-Almirón, M.; Nanni, P.; Arevalillo, J.M.; Navarro, H.; Grossmann, J.; et al. Functional proteomics outlines the complexity of breast cancer molecular subtypes. Sci. Rep. 2017, 7, 10100. [Google Scholar] [CrossRef]
- Gámez-Pozo, A.; Trilla-Fuertes, L.; Prado-Vázquez, G.; Chiva, C.; López-Vacas, R.; Nanni, P.; Berges-Soria, J.; Grossmann, J.; Díaz-Almirón, M.; Ciruelos, E.; et al. Prediction of adjuvant chemotherapy response in triple negative breast cancer with discovery and targeted proteomics. PLoS ONE 2017, 12, e0178296. [Google Scholar] [CrossRef] [PubMed]
- García-Adrián, S.; Trilla-Fuertes, L.; Gámez-Pozo, A.; Chiva, C.; López-Vacas, R.; López-Camacho, E.; Zapater-Moros, A.; Lumbreras-Herrera, M.I.; Hardisson, D.; Yébenes, L.; et al. Molecular characterization of triple negative breast cancer formaldehyde-fixed paraffin-embedded samples by data-independent acquisition proteomics. Proteomics 2022, 22, e2100110. [Google Scholar] [CrossRef]
- Garrisi, V.M.; Tommasi, S.; Facchiano, A.; Bongarzone, I.; De Bortoli, M.; Cremona, M.; Cafagna, V.; Abbate, I.; Tufaro, A.; Quaranta, M.; et al. Proteomic profile in familial breast cancer patients. Clin. Biochem. 2013, 46, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Garrisi, V.M.; Tufaro, A.; Trerotoli, P.; Bongarzone, I.; Quaranta, M.; Ventrella, V.; Tommasi, S.; Giannelli, G.; Paradiso, A. Body mass index and serum proteomic profile in breast cancer and healthy women: A prospective study. PLoS ONE 2012, 7, e49631. [Google Scholar] [CrossRef]
- Gast, M.C.; Zapatka, M.; van Tinteren, H.; Bontenbal, M.; Span, P.N.; Tjan-Heijnen, V.C.; Knol, J.C.; Jimenez, C.R.; Schellens, J.H.; Beijnen, J.H. Postoperative serum proteomic profiles may predict recurrence-free survival in high-risk primary breast cancer. J. Cancer Res. Clin. Oncol. 2011, 137, 1773–1783. [Google Scholar] [CrossRef][Green Version]
- Giri, K.; Maity, S.; Ambatipudi, K. Targeted proteomics using parallel reaction monitoring confirms salivary proteins indicative of metastatic triple-negative breast cancer. J. Proteom. 2022, 267, 104701. [Google Scholar] [CrossRef]
- Gonçalves, A.; Esterni, B.; Bertucci, F.; Sauvan, R.; Chabannon, C.; Cubizolles, M.; Bardou, V.J.; Houvenaegel, G.; Jacquemier, J.; Granjeaud, S.; et al. Postoperative serum proteomic profiles may predict metastatic relapse in high-risk primary breast cancer patients receiving adjuvant chemotherapy. Oncogene 2006, 25, 981–989. [Google Scholar] [CrossRef]
- Gonzalez-Angulo, A.M.; Hennessy, B.T.; Meric-Bernstam, F.; Sahin, A.; Liu, W.; Ju, Z.; Carey, M.S.; Myhre, S.; Speers, C.; Deng, L.; et al. Functional proteomics can define prognosis and predict pathologic complete response in patients with breast cancer. Clin. Proteom. 2011, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez-Angulo, A.M.; Liu, S.; Chen, H.; Chavez-Macgregor, M.; Sahin, A.; Hortobagyi, G.N.; Mills, G.B.; Do, K.A.; Meric-Bernstam, F. Functional proteomics characterization of residual breast cancer after neoadjuvant systemic chemotherapy. Ann. Oncol. 2013, 24, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Grassmann, F.; Mälarstig, A.; Dahl, L.; Bendes, A.; Dale, M.; Thomas, C.E.; Gabrielsson, M.; Hedman, Å.K.; Eriksson, M.; Margolin, S.; et al. The impact of circulating protein levels identified by affinity proteomics on short-term, overall breast cancer risk. Br. J. Cancer 2024, 130, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Gromova, I.; Espinoza, J.A.; Grauslund, M.; Santoni-Rugiu, E.; Møller Talman, M.L.; van Oostrum, J.; Moreira, J.M.A. Functional Proteomic Profiling of Triple-Negative Breast Cancer. Cells 2021, 10, 2768. [Google Scholar] [CrossRef]
- Guerin, M.; Gonçalves, A.; Toiron, Y.; Baudelet, E.; Pophillat, M.; Granjeaud, S.; Fourquet, P.; Jacot, W.; Tarpin, C.; Sabatier, R.; et al. Development of parallel reaction monitoring (PRM)-based quantitative proteomics applied to HER2-Positive breast cancer. Oncotarget 2018, 9, 33762–33777. [Google Scholar] [CrossRef]
- Gustafsson, A.; Jonasson, E.; Ståhlberg, A.; Landberg, G. Proteomics of cell-free breast cancer scaffolds identify clinically relevant imprinted proteins and cancer-progressing properties. Cancer Commun. 2024, 44, 695–699. [Google Scholar] [CrossRef]
- He, J.; Shen, D.; Chung, D.U.; Saxton, R.E.; Whitelegge, J.P.; Faull, K.F.; Chang, H.R. Tumor proteomic profiling predicts the susceptibility of breast cancer to chemotherapy. Int. J. Oncol. 2009, 35, 683–692. [Google Scholar] [CrossRef]
- He, J.; Whelan, S.A.; Lu, M.; Shen, D.; Chung, D.U.; Saxton, R.E.; Faull, K.F.; Whitelegge, J.P.; Chang, H.R. Proteomic-based biosignatures in breast cancer classification and prediction of therapeutic response. Int. J. Proteom. 2011, 896476. [Google Scholar] [CrossRef]
- Henderson, M.C.; Hollingsworth, A.B.; Gordon, K.; Silver, M.; Mulpuri, R.; Letsios, E.; Reese, D.E. Integration of Serum Protein Biomarker and Tumor Associated Autoantibody Expression Data Increases the Ability of a Blood-Based Proteomic Assay to Identify Breast Cancer. PLoS ONE 2016, 11, e0157692. [Google Scholar] [CrossRef]
- Henderson, M.C.; Silver, M.; Tran, Q.; Letsios, E.E.; Mulpuri, R.; Reese, D.E.; Lourenco, A.P.; LaBaer, J.; Anderson, K.S.; Alpers, J.; et al. A Noninvasive Blood-based Combinatorial Proteomic Biomarker Assay to Detect Breast Cancer in Women over age 50 with BI-RADS 3, 4, or 5 Assessment. Clin. Cancer Res. 2019, 25, 142–149. [Google Scholar] [CrossRef]
- Hu, Y.; Zhang, S.; Yu, J.; Liu, J.; Zheng, S. SELDI-TOF-MS: The proteomics and bioinformatics approaches in the diagnosis of breast cancer. Breast 2005, 14, 250–255. [Google Scholar] [CrossRef]
- Hulahan, T.S.; Spruill, L.; Wallace, E.N.; Park, Y.; West, R.B.; Marks, J.R.; Hwang, E.S.; Drake, R.R.; Angel, P.M. Extracellular Microenvironment Alterations in Ductal Carcinoma In Situ and Invasive Breast Cancer Pathologies by Multiplexed Spatial Proteomics. Int. J. Mol. Sci. 2024, 25, 6748. [Google Scholar] [CrossRef]
- Jeanmard, N.; Bissanum, R.; Sriplung, H.; Charoenlappanit, S.; Roytrakul, S.; Navakanitworakul, R. Proteomic profiling of urinary extracellular vesicles differentiates breast cancer patients from healthy women. PLoS ONE 2023, 18, e0291574. [Google Scholar] [CrossRef] [PubMed]
- Jeon, Y.; Lee, G.; Jeong, H.; Gong, G.; Kim, J.; Kim, K.; Jeong, J.H.; Lee, H.J. Proteomic analysis of breast cancer based on immune subtypes. Clin. Proteom. 2024, 21, 17. [Google Scholar] [CrossRef]
- Johansson, H.J.; Sanchez, B.C.; Forshed, J.; Stål, O.; Fohlin, H.; Lewensohn, R.; Hall, P.; Bergh, J.; Lehtiö, J.; Linderholm, B.K. Proteomics profiling identify CAPS as a potential predictive marker of tamoxifen resistance in estrogen receptor positive breast cancer. Clin. Proteom. 2015, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Jordan, K.R.; Hall, J.K.; Schedin, T.; Borakove, M.; Xian, J.J.; Dzieciatkowska, M.; Lyons, T.R.; Schedin, P.; Hansen, K.C.; Borges, V.F. Extracellular vesicles from young women’s breast cancer patients drive increased invasion of non-malignant cells via the Focal Adhesion Kinase pathway: A proteomic approach. Breast Cancer Res. 2020, 22, 128. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.; Kim, M.J.; An, H.; Kim, B.G.; Choi, Y.P.; Kang, K.S.; Gao, M.Q.; Park, H.; Na, H.J.; Kim, H.K.; et al. Proteomic molecular portrait of interface zone in breast cancer. J. Proteome Res. 2010, 9, 5638–5645. [Google Scholar] [CrossRef]
- Kaur, J.; Jung, S.Y.; Austdal, M.; Arun, A.K.; Helland, T.; Mellgren, G.; Lende, T.H.; Janssen, E.A.M.; Søiland, H.; Aneja, R. Quantitative proteomics reveals serum proteome alterations during metastatic disease progression in breast cancer patients. Clin. Proteom. 2024, 21, 52. [Google Scholar] [CrossRef]
- Kim, D.H.; Bae, J.; Lee, J.W.; Kim, S.Y.; Kim, Y.H.; Bae, J.Y.; Yi, J.K.; Yu, M.H.; Noh, D.Y.; Lee, C. Proteomic analysis of breast cancer tissue reveals upregulation of actin-remodeling proteins and its relevance to cancer invasiveness. Proteom. Clin. Appl. 2009, 3, 30–40. [Google Scholar] [CrossRef]
- Kim, Y.; Kang, U.B.; Kim, S.; Lee, H.B.; Moon, H.G.; Han, W.; Noh, D.Y. A Validation Study of a Multiple Reaction Monitoring-Based Proteomic Assay to Diagnose Breast Cancer. J. Breast Cancer 2019, 22, 579–586. [Google Scholar] [CrossRef]
- Kuerer, H.M.; Coombes, K.R.; Chen, J.N.; Xiao, L.; Clarke, C.; Fritsche, H.; Krishnamurthy, S.; Marcy, S.; Hung, M.C.; Hunt, K.K. Association between ductal fluid proteomic expression profiles and the presence of lymph node metastases in women with breast cancer. Surgery 2004, 136, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Le Naour, F.; Misek, D.E.; Krause, M.C.; Deneux, L.; Giordano, T.J.; Scholl, S.; Hanash, S.M. Proteomics-based identification of RS/DJ-1 as a novel circulating tumor antigen in breast cancer. Clin. Cancer Res. 2001, 7, 3328–3335. [Google Scholar]
- Lebrecht, A.; Boehm, D.; Schmidt, M.; Koelbl, H.; Schwirz, R.L.; Grus, F.H. Diagnosis of breast cancer by tear proteomic pattern. Cancer Genom. Proteom. 2009, 6, 177–182. [Google Scholar]
- Li, Y.; Yue, L.; Zhang, S.; Wang, X.; Zhu, Y.N.; Liu, J.; Ren, H.; Jiang, W.; Wang, J.; Zhang, Z.; et al. Proteomic, single-cell and bulk transcriptomic analysis of plasma and tumor tissues unveil core proteins in response to anti-PD-L1 immunotherapy in triple negative breast cancer. Comput. Biol. Med. 2024, 176, 108537. [Google Scholar] [CrossRef]
- Lin, Y.; Lin, L.; Fu, F.; Wang, C.; Hu, A.; Xie, J.; Jiang, M.; Wang, Z.; Yang, L.; Guo, R.; et al. Quantitative proteomics reveals stage-specific protein regulation of triple negative breast cancer. Breast Cancer Res. Treat. 2021, 185, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Lötsch, J.; Mustonen, L.; Harno, H.; Kalso, E. Machine-Learning Analysis of Serum Proteomics in Neuropathic Pain after Nerve Injury in Breast Cancer Surgery Points at Chemokine Signaling via SIRT2 Regulation. Int. J. Mol. Sci. 2022, 23, 3488. [Google Scholar] [CrossRef]
- Lourenco, A.P.; Benson, K.L.; Henderson, M.C.; Silver, M.; Letsios, E.; Tran, Q.; Gordon, K.J.; Borman, S.; Corn, C.; Mulpuri, R.; et al. A Noninvasive Blood-based Combinatorial Proteomic Biomarker Assay to Detect Breast Cancer in Women Under the Age of 50 Years. Clin. Breast Cancer 2017, 17, 516–525.e6. [Google Scholar] [CrossRef]
- Magara, K.; Takasawa, A.; Takasawa, K.; Aoyama, T.; Ota, M.; Kyuno, D.; Ono, Y.; Murakami, T.; Yamamoto, S.; Nakamori, Y.; et al. Multilayered proteomics reveals that JAM-A promotes breast cancer progression via regulation of amino acid transporter LAT1. Cancer Sci. 2024, 115, 3153–3168. [Google Scholar] [CrossRef]
- Majidzadeh, A.K.; Gharechahi, J. Plasma proteomics analysis of tamoxifen resistance in breast cancer. Med. Oncol. 2013, 30, 753. [Google Scholar] [CrossRef]
- Mayayo-Peralta, I.; Debets, D.O.; Prekovic, S.; Schuurman, K.; Beerthuijzen, S.; Almekinders, M.; Sanders, J.; Moelans, C.B.; Saleiro, S.; Wesseling, J.; et al. Proteomics on malignant pleural effusions reveals ERα loss in metastatic breast cancer associates with SGK1-NDRG1 deregulation. Mol. Oncol. 2024, 18, 156–169. [Google Scholar] [CrossRef]
- Meric-Bernstam, F.; Akcakanat, A.; Chen, H.; Sahin, A.; Tarco, E.; Carkaci, S.; Adrada, B.E.; Singh, G.; Do, K.A.; Garces, Z.M.; et al. Influence of biospecimen variables on proteomic biomarkers in breast cancer. Clin. Cancer Res. 2014, 20, 3870–3883. [Google Scholar] [CrossRef] [PubMed]
- Michaut, M.; Chin, S.F.; Majewski, I.; Severson, T.M.; Bismeijer, T.; de Koning, L.; Peeters, J.K.; Schouten, P.C.; Rueda, O.M.; Bosma, A.J.; et al. Integration of genomic, transcriptomic and proteomic data identifies two biologically distinct subtypes of invasive lobular breast cancer. Sci. Rep. 2016, 6, 18517. [Google Scholar] [CrossRef]
- Minton, O.; Stone, P.C. The identification of plasma proteins associated with cancer-related fatigue syndrome (CRFS) in disease-free breast cancer patients using proteomic analysis. J. Pain Symptom Manag. 2013, 45, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Moriggi, M.; Giussani, M.; Torretta, E.; Capitanio, D.; Sandri, M.; Leone, R.; De Palma, S.; Vasso, M.; Vozzi, G.; Tagliabue, E.; et al. ECM Remodeling in Breast Cancer with Different Grade: Contribution of 2D-DIGE Proteomics. Proteomics 2018, 18, e1800278. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, T.; Huang, S.K.; Martinez, S.R.; Tran, A.N.; Elashoff, D.; Ye, X.; Turner, R.R.; Giuliano, A.E.; Hoon, D.S. Proteomic profiling of primarybreast cancer predicts axillary lymph node metastasis. Cancer Res. 2006, 66, 11825–11830. [Google Scholar] [CrossRef]
- Neubauer, H.; Clare, S.E.; Kurek, R.; Fehm, T.; Wallwiener, D.; Sotlar, K.; Nordheim, A.; Wozny, W.; Schwall, G.P.; Poznanović, S.; et al. Breast cancer proteomics by laser capture microdissection, sample pooling, 54-cm IPGIEF, and differential iodine radioisotope detection. Electrophoresis 2006, 27, 1840–1852. [Google Scholar] [CrossRef]
- Neubauer, H.; Clare, S.E.; Wozny, W.; Schwall, G.P.; Poznanovic, S.; Stegmann, W.; Vogel, U.; Sotlar, K.; Wallwiener, D.; Kurek, R.; et al. Breast cancer proteomics reveals correlation between estrogen receptor status and differential phosphorylation of PGRMC1. Breast Cancer Res. 2008, 10, R85. [Google Scholar] [CrossRef]
- Niméus, E.; Malmström, J.; Johnsson, A.; Marko-Varga, G.; Fernö, M. Proteomic analysis identifies candidate proteins associated with distant recurrences in breast cancer after adjuvant chemotherapy. J. Pharm. Biomed. Anal. 2007, 43, 1086–1093. [Google Scholar] [CrossRef]
- Othman, M.I.; Majid, M.I.; Singh, M.; Subathra, S.; Seng, L.; Gam, L.H. Proteomics of Grade 3 infiltrating ductal carcinoma in Malaysian Chinese breast cancer patients. Biotechnol. Appl. Biochem. 2009, 52, 209–219. [Google Scholar] [CrossRef]
- Ou, K.; Yu, K.; Kesuma, D.; Hooi, M.; Huang, N.; Chen, W.; Lee, S.Y.; Goh, X.P.; Tan, L.K.; Liu, J.; et al. Novel breast cancer biomarkers identified by integrative proteomic and gene expression mapping. J. Proteome Res. 2008, 7, 1518–1528. [Google Scholar] [CrossRef]
- Panis, C.; Pizzatti, L.; Herrera, A.C.; Cecchini, R.; Abdelhay, E. Putative circulating markers of the early and advanced stages of breast cancer identified by high-resolution label-free proteomics. Cancer Lett. 2013, 330, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Pathania, S.; Khan, M.I.; Bandyopadhyay, S.; Singh, S.S.; Rani, K.; Parashar, T.R.; Jayaram, J.; Mishra, P.R.; Srivastava, A.; Mathur, S.; et al. iTRAQ proteomics of sentinel lymph nodes for identification of extracellular matrix proteins to flag metastasis in early breast cancer. Sci. Rep. 2022, 12, 8625. [Google Scholar] [CrossRef]
- Paweletz, C.P.; Trock, B.; Pennanen, M.; Tsangaris, T.; Magnant, C.; Liotta, L.A.; Petricoin, E.F., 3rd. Proteomic patterns of nipple aspirate fluids obtained by SELDI-TOF: Potential for new biomarkers to aid in the diagnosis of breast cancer. Dis. Markers 2001, 17, 301–307. [Google Scholar] [CrossRef]
- Pawlik, T.M.; Hawke, D.H.; Liu, Y.; Krishnamurthy, S.; Fritsche, H.; Hunt, K.K.; Kuerer, H.M. Proteomic analysis of nipple aspirate fluid from women with early-stage breast cancer using isotope-coded affinity tags and tandem mass spectrometry reveals differential expression of vitamin D binding protein. BMC Cancer 2006, 6, 68. [Google Scholar] [CrossRef]
- Pires, B.R.B.; Panis, C.; Alves, V.D.; Herrera, A.C.S.A.; Binato, R.; Pizzatti, L.; Cecchini, R.; Abdelhay, E. Label-Free Proteomics Revealed Oxidative Stress and Inflammation as Factors That Enhance Chemoresistance in Luminal Breast Cancer. Oxidative Med. Cell. Longev. 2019, 2019, 5357649. [Google Scholar] [CrossRef]
- Pozniak, Y.; Balint-Lahat, N.; Rudolph, J.D.; Lindskog, C.; Katzir, R.; Avivi, C.; Pontén, F.; Ruppin, E.; Barshack, I.; Geiger, T. System-wide Clinical Proteomics of Breast Cancer Reveals Global Remodeling of Tissue Homeostasis. Cell Syst. 2016, 2, 172–184. [Google Scholar] [CrossRef]
- Procházková, I.; Lenčo, J.; Bouchal, P. Targeted Proteomics Driven Verification of Biomarker Candidates Associated with Breast Cancer Aggressiveness. Methods Mol. Biol. 2018, 1788, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Pucci-Minafra, I.; Cancemi, P.; Albanese, N.N.; Di Cara, G.; Marabeti, M.R.; Marrazzo, A.; Minafra, S. New protein clustering of breast cancer tissue proteomics using actin content as a cellularity indicator. J. Proteome Res. 2008, 7, 1412–1418. [Google Scholar] [CrossRef] [PubMed]
- Pucci-Minafra, I.; Di Cara, G.; Musso, R.; Cancemi, P.; Albanese, N.N.; Roz, E.; Minafra, S. Retrospective Proteomic Screening of 100 Breast Cancer Tissues. Proteomes 2017, 5, 15. [Google Scholar] [CrossRef]
- Riley, C.P.; Zhang, X.; Nakshatri, H.; Schneider, B.; Regnier, F.E.; Adamec, J.; Buck, C. A large, consistent plasma proteomics data set from prospectively collected breast cancer patient and healthy volunteer samples. J. Transl. Med. 2011, 9, 80. [Google Scholar] [CrossRef]
- Roberts, K.; Bhatia, K.; Stanton, P.; Lord, R. Proteomic analysis of selected prognostic factors of breast cancer. Proteomics 2004, 4, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Rui, Z.; Jian-Guo, J.; Yuan-Peng, T.; Hai, P.; Bing-Gen, R. Use of serological proteomic methods to find biomarkers associated with breast cancer. Proteomics 2003, 3, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Rojas, L.K.; Trilla-Fuertes, L.; Gámez-Pozo, A.; Chiva, C.; Sepúlveda, J.; Manso, L.; Prado-Vázquez, G.; Zapater-Moros, A.; López-Vacas, R.; Ferrer-Gómez, M.; et al. Proteomics characterisation of central nervous system metastasis biomarkers in triple negative breast cancer. Ecancermedicalscience 2019, 13, 891. [Google Scholar] [CrossRef]
- Ruckhäberle, E.; Karn, T.; Hanker, L.; Schwarz, J.; Schulz-Knappe, P.; Kuhn, K.; Böhm, G.; Selzer, S.; Erhard, N.; Engels, K.; et al. Breast Cancer Proteomics—Differences in Protein Expression between Estrogen Receptor-Positive and -Negative Tumors Identified by Tandem Mass Tag Technology. Breast Care 2010, 5, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Sanders, M.E.; Dias, E.C.; Xu, B.J.; Mobley, J.A.; Billheimer, D.; Roder, H.; Grigorieva, J.; Dowsett, M.; Arteaga, C.L.; Caprioli, R.M. Differentiating proteomic biomarkers in breastcancer by laser capture microdissection and MALDI MS. J. Proteome Res. 2008, 7, 1500–1507. [Google Scholar] [CrossRef]
- Santana, M.F.M.; Sawada, M.I.B.A.C.; Junior, D.R.S.; Giacaglia, M.B.; Reis, M.; Xavier, J.; Côrrea-Giannella, M.L.; Soriano, F.G.; Gebrim, L.H.; Ronsein, G.E.; et al. Proteomic Profiling of HDL in Newly Diagnosed Breast Cancer Based on Tumor Molecular Classification and Clinical Stage of Disease. Cells 2024, 13, 1327. [Google Scholar] [CrossRef]
- Sauter, E.R.; Zhu, W.; Fan, X.J.; Wassell, R.P.; Chervoneva, I.; Du Bois, G.C. Proteomic analysis of nipple aspirate fluid to detect biologic markers of breast cancer. Br. J. Cancer 2002, 86, 1440–1443. [Google Scholar] [CrossRef]
- Schaub, N.P.; Jones, K.J.; Nyalwidhe, J.O.; Cazares, L.H.; Karbassi, I.D.; Semmes, O.J.; Feliberti, E.C.; Perry, R.R.; Drake, R.R. Serum proteomic biomarker discovery reflective of stage and obesity in breast cancer patients. J. Am. Coll. Surg. 2009, 208, 970–980. [Google Scholar] [CrossRef]
- Shenoy, A.; Belugali Nataraj, N.; Perry, G.; Loayza Puch, F.; Nagel, R.; Marin, I.; Balint, N.; Bossel, N.; Pavlovsky, A.; Barshack, I.; et al. Proteomic patterns associated with response to breast cancer neoadjuvant treatment. Mol. Syst. Biol. 2020, 16, e9443. [Google Scholar] [CrossRef]
- Shi, X.; Liu, C.; Zheng, W.; Cao, X.; Li, W.; Zhang, D.; Zhu, J.; Zhang, X.; Chen, Y. Proteomic Analysis Revealed the Potential Role of MAGE-D2 in the Therapeutic Targeting of Triple-Negative Breast Cancer. Mol. Cell. Proteom. 2024, 23, 100703. [Google Scholar] [CrossRef]
- Shin, D.; Park, J.; Han, D.; Moon, J.H.; Ryu, H.S.; Kim, Y. Identification of TUBB2A by quantitative proteomic analysis as a novel biomarker for the prediction of distant metastatic breast cancer. Clin. Proteom. 2020, 17, 16. [Google Scholar] [CrossRef] [PubMed]
- Sinha, I.; Fogle, R.L.; Gulfidan, G.; Stanley, A.E.; Walter, V.; Hollenbeak, C.S.; Arga, K.Y.; Sinha, R. Potential Early Markers for Breast Cancer: A Proteomic Approach Comparing Saliva and Serum Samples in a Pilot Study. Int. J. Mol. Sci. 2023, 24, 4164. [Google Scholar] [CrossRef] [PubMed]
- Sohn, J.; Do, K.A.; Liu, S.; Chen, H.; Mills, G.B.; Hortobagyi, G.N.; Meric-Bernstam, F.; Gonzalez-Angulo, A.M. Functional proteomics characterization of residual triple-negative breast cancer after standard neoadjuvant chemotherapy. Ann. Oncol. 2013, 24, 2522–2526. [Google Scholar] [CrossRef]
- Starodubtseva, N.L.; Tokareva, A.O.; Rodionov, V.V.; Brzhozovskiy, A.G.; Bugrova, A.E.; Chagovets, V.V.; Kometova, V.V.; Kukaev, E.N.; Soares, N.C.; Kovalev, G.I.; et al. Integrating Proteomics and Lipidomics for Evaluating the Risk of Breast Cancer Progression: A Pilot Study. Biomedicines 2023, 11, 1786. [Google Scholar] [CrossRef]
- Stemke-Hale, K.; Gonzalez-Angulo, A.M.; Lluch, A.; Neve, R.M.; Kuo, W.L.; Davies, M.; Carey, M.; Hu, Z.; Guan, Y.; Sahin, A.; et al. An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res. 2008, 68, 6084–6091. [Google Scholar] [CrossRef] [PubMed]
- Suman, S.; Basak, T.; Gupta, P.; Mishra, S.; Kumar, V.; Sengupta, S.; Shukla, Y. Quantitative proteomics revealed novel proteins associated with molecular subtypes of breast cancer. J. Proteom. 2016, 148, 183–193. [Google Scholar] [CrossRef]
- Tamesa, M.S.; Kuramitsu, Y.; Fujimoto, M.; Maeda, N.; Nagashima, Y.; Tanaka, T.; Yamamoto, S.; Oka, M.; Nakamura, K. Detection of autoantibodies against cyclophilin A and triosephosphate isomerase in sera from breast cancer patients by proteomic analysis. Electrophoresis 2009, 30, 2168–2181. [Google Scholar] [CrossRef]
- Terkelsen, T.; Pernemalm, M.; Gromov, P.; Børresen-Dale, A.L.; Krogh, A.; Haakensen, V.D.; Lethiö, J.; Papaleo, E.; Gromova, I. High-throughput proteomics of breast cancer interstitial fluid: Identification of tumor subtype-specific serologically relevant biomarkers. Clin. Trial Mol. Oncol. 2021, 15, 429–461. [Google Scholar] [CrossRef]
- Tutanov, O.; Orlova, E.; Proskura, K.; Grigor’eva, A.; Yunusova, N.; Tsentalovich, Y.; Alexandrova, A.; Tamkovich, S. Proteomic Analysis of Blood Exosomes from Healthy Females and Breast Cancer Patients Reveals an Association between Different Exosomal Bioactivity on Non-tumorigenic Epithelial Cell and Breast Cancer Cell Migration in Vitro. Biomolecules 2020, 10, 495. [Google Scholar] [CrossRef]
- Tyanova, S.; Albrechtsen, R.; Kronqvist, P.; Cox, J.; Mann, M.; Geiger, T. Proteomic maps of breast cancer subtypes. Nat. Commun. 2016, 7, 10259. [Google Scholar] [CrossRef]
- Valo, I.; Raro, P.; Boissard, A.; Maarouf, A.; Jézéquel, P.; Verriele, V.; Campone, M.; Coqueret, O.; Guette, C. OLFM4 Expression in Ductal Carcinoma In Situ and in Invasive Breast Cancer Cohorts by a SWATH-Based Proteomic Approach. Proteomics 2019, 19, e1800446. [Google Scholar] [CrossRef]
- Vinik, Y.; Ortega, F.G.; Mills, G.B.; Lu, Y.; Jurkowicz, M.; Halperin, S.; Aharoni, M.; Gutman, M.; Lev, S. Proteomic analysis of circulating extracellular vesicles identifies potential markers of breast cancer progression, recurrence, and response. Sci. Adv. 2020, 6, eaba5714. [Google Scholar] [CrossRef]
- Xu, G.; Huang, R.; Wumaier, R.; Lyu, J.; Huang, M.; Zhang, Y.; Chen, Q.; Liu, W.; Tao, M.; Li, J.; et al. Proteomic Profiling of Serum Extracellular Vesicles Identifies Diagnostic Signatures and Therapeutic Targets in Breast Cancer. Cancer Res. 2024, 84, 3267–3285. [Google Scholar] [CrossRef]
- Xu, Q.; Zhu, M.; Yang, T.; Xu, F.; Liu, Y.; Chen, Y. Quantitative assessment of human serum transferrin receptor in breast cancer patients pre- and post-chemotherapy using peptide immunoaffinity enrichment coupled with targeted proteomics. Clin. Chim. Acta 2015, 448, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Yan, Y.; Zhou, Y.; Wang, K.; Qiao, Y.; Zhao, L.; Chen, M. Apolipoprotein C1 (APOC1), A Candidate Diagnostic Serum Biomarker for Breast Cancer Identified by Serum Proteomics Study. Crit. Rev. Eukaryot. Gene Expr. 2022, 32, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Fu, Z.; Zhang, Y.; Wang, M.; Mao, C.; Ge, W. Serum proteomics analysis of candidate predictive biomarker panel for the diagnosis of trastuzumab-based therapy resistant breast cancer. Biomed. Pharmacother. 2020, 129, 110465. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Xu, F.; Fang, D.; Chen, Y. Targeted Proteomics Enables Simultaneous Quantification of Folate Receptor Isoforms and Potential Isoform-based Diagnosis in Breast Cancer. Sci. Rep. 2015, 5, 16733. [Google Scholar] [CrossRef]
- Yang, T.; Xu, F.; Sheng, Y.; Zhang, W.; Chen, Y. A targeted proteomics approach to the quantitative analysis of ERK/Bcl-2-mediated anti-apoptosis and multi-drug resistance in breast cancer. Anal. Bioanal. Chem. 2016, 408, 7491–7503. [Google Scholar] [CrossRef]
- Yang, T.; Xu, F.; Zhao, Y.; Wang, S.; Yang, M.; Chen, Y. A liquid chromatography-tandem mass spectrometry-based targeted proteomics approach for the assessment of transferrin receptor levels in breast cancer. Proteom. Clin. Appl. 2014, 8, 773–782. [Google Scholar] [CrossRef]
- Yang, W.S.; Moon, H.G.; Kim, H.S.; Choi, E.J.; Yu, M.H.; Noh, D.Y.; Lee, C. Proteomic approach reveals FKBP4 and S100A9 as potential prediction markers of therapeutic response to neoadjuvant chemotherapy in patients with breast cancer. J. Proteome Res. 2012, 11, 1078–1088. [Google Scholar] [CrossRef]
- Yanovich, G.; Agmon, H.; Harel, M.; Sonnenblick, A.; Peretz, T.; Geiger, T. Clinical Proteomics of Breast Cancer Reveals a Novel Layer of Breast Cancer Classification. Cancer Res. 2018, 78, 6001–6010. [Google Scholar] [CrossRef] [PubMed]
- Ye, H.; Shen, X.; Li, Y.; Zou, W.; Hassan, S.S.U.; Feng, Y.; Wang, X.; Tian, J.; Shao, X.; Tao, Y.; et al. Proteomic and metabolomic characterization of bone, liver, and lung metastases in plasma of breast cancer patients. Proteom. Clin. Appl. 2024, 18, e2300136. [Google Scholar] [CrossRef]
- Zeidan, B.; Manousopoulou, A.; Garay-Baquero, D.J.; White, C.H.; Larkin, S.E.T.; Potter, K.N.; Roumeliotis, T.I.; Papachristou, E.K.; Copson, E.; Cutress, R.I.; et al. Increased circulating resistin levels in early-onset breast cancer patients of normal body mass index correlate with lymph node negative involvement and longer disease free survival: A multi-center POSH cohort serum proteomics study. Breast Cancer Res. 2018, 20, 19. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Zhong, J.; He, G.; Li, F.; Li, J.; Zhou, W.; Liu, W.; Zhang, Y.; Huang, S.; Liu, Z.; et al. Identification of Nucleobindin-2 as a Potential Biomarker for Breast Cancer Metastasis Using iTRAQ-based Quantitative Proteomic Analysis. J. Cancer 2017, 8, 3062–3069. [Google Scholar] [CrossRef]
- Zhang, D.; Tai, L.K.; Wong, L.L.; Putti, T.C.; Sethi, S.K.; Teh, M.; Koay, E.S. Proteomic characterization of differentially expressed proteins in breast cancer: Expression of hnRNP H1, RKIP and GRP78 is strongly associated with HER-2/neu status. Proteom. Clin. Appl. 2008, 2, 99–107. [Google Scholar] [CrossRef]
- Zhang, D.H.; Tai, L.K.; Wong, L.L.; Sethi, S.K.; Koay, E.S. Proteomics of breast cancer: Enhanced expression of cytokeratin19 in human epidermal growth factor receptor type 2 positive breast tumors. Proteomics 2005, 5, 1797–1805. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Chen, J.; Wang, M.; Drabier, R. A neural network approach to multi-biomarker panel discovery by high-throughput plasma proteomics profiling of breast cancer. BMC Proc. 2013, 7, S10. [Google Scholar] [CrossRef]
- Zhang, F.; Deng, Y.; Wang, M.; Cui, L.; Drabier, R. Pathway-based Biomarkers for Breast Cancer in Proteomics. Cancer Inform. 2015, 13, 101–108. [Google Scholar] [CrossRef]
- Zhang, F.; Wang, M.; Michael, T.; Drabier, R. Novel alternative splicing isoform biomarkers identification from high-throughput plasma proteomics profiling of breast cancer. BMC Syst. Biol. 2013, 7 (Suppl. S5), S8. [Google Scholar] [CrossRef]
- Zhang, L.; Xiao, H.; Karlan, S.; Zhou, H.; Gross, J.; Elashoff, D.; Akin, D.; Yan, X.; Chia, D.; Karlan, B.; et al. Discovery and preclinical validation of salivary transcriptomic and proteomic biomarkers for the non-invasive detection of breast cancer. PLoS ONE 2010, 5, e15573. [Google Scholar] [CrossRef]
- Zhao, M.; Jiang, Y.; Kong, X.; Liu, Y.; Gao, P.; Li, M.; Zhu, H.; Deng, G.; Feng, Z.; Cao, Y.; et al. The Analysis of Plasma Proteomics for Luminal A Breast Cancer. Cancer Med. 2024, 13, e70470. [Google Scholar] [CrossRef]
- Zhong, J.M.; Li, J.; Kang, A.D.; Huang, S.Q.; Liu, W.B.; Zhang, Y.; Liu, Z.H.; Zeng, L. Protein S100-A8: A potential metastasis-associated protein for breast cancer determined via iTRAQ quantitative proteomic and clinicopathological analysis. Oncol. Lett. 2018, 15, 5285–5293. [Google Scholar] [CrossRef] [PubMed]
- Tomar, A.K.; Thapliyal, A.; Mathur, S.R.; Parshad, R.; Suhani Yadav, S. Exploring Molecular Alterations in Breast Cancer Among Indian Women Using Label-Free Quantitative Serum Proteomics. Biochem. Res. Int. 2024, 2024, 5584607. [Google Scholar] [CrossRef] [PubMed]
- Ku, W.C.; Liu, C.Y.; Huang, C.J.; Liao, C.C.; Huang, Y.C.; Kong, P.H.; Chen-Chan, H.; Tseng, L.M.; Huang, C.C. Integrating functional proteomics and next generation sequencing reveals potential therapeutic targets for Taiwanese breast cancer. Clin. Proteom. 2025, 22, 4. [Google Scholar] [CrossRef] [PubMed]
- Morrow, M. Sentinel-Lymph-Node Biopsy in Early-Stage Breast Cancer—Is It Obsolete? N. Engl. J. Med. 2024, in press. [Google Scholar] [CrossRef]
- Reimer, T.; Stachs, A.; Veselinovic, K.; Kühn, T.; Heil, J.; Polata, S.; Marmé, F.; Müller, T.; Hildebrandt, G.; Krug, D.; et al. Axillary Surgery in Breast Cancer—Primary Results of the INSEMA Trial. N. Engl. J. Med. 2024, in press. [Google Scholar] [CrossRef]
- Otte, M.; Zafrakas, M.; Riethdorf, L.; Pichlmeier, U.; Löning, T.; Jänicke, F.; Pantel, K. MAGE-A gene expression pattern in primary breast cancer. Cancer Res. 2001, 61, 6682–6687. [Google Scholar]
- Rutgers, E.; Piccart-Gebhart, M.J.; Bogaerts, J.; Delaloge, S.; Veer, L.V.; Rubio, I.T.; Viale, G.; Thompson, A.M.; Passalacqua, R.; Nitz, U.; et al. The EORTC 10041/BIG 03-04 MINDACT trial is feasible: Results of the pilot phase. Eur. J. Cancer 2011, 47, 2742–2749. [Google Scholar] [CrossRef]
- Sparano, J.A.; Gray, R.J.; Makower, D.F.; Pritchard, K.I.; Albain, K.S.; Hayes, D.F.; Geyer, C.E., Jr.; Dees, E.C.; Goetz, M.P.; Olson, J.A.; et al. Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. N. Engl. J. Med. 2018, 379, 111–121. [Google Scholar] [CrossRef]
- Lænkholm, A.V.; Jensen, M.B.; Eriksen, J.O.; Rasmussen, B.B.; Knoop, A.S.; Buckingham, W.; Ferree, S.; Schaper, C.; Nielsen, T.O.; Haffner, T.; et al. PAM50 Risk of Recurrence Score Predicts 10-Year Distant Recurrence in a Comprehensive Danish Cohort of Postmenopausal Women Allocated to 5 Years of Endocrine Therapy for Hormone Receptor-Positive Early Breast Cancer. J. Clin. Oncol. 2018, 36, 735–740. [Google Scholar] [CrossRef]
- Soliman, H.; Flake, D.D., 2nd; Magliocco, A.; Robson, M.; Schwartzberg, L.; Sharma, P.; Brown, K.; Wehnelt, S.; Kronenwett, R.; Gutin, A.; et al. Predicting Expected Absolute Chemotherapy Treatment Benefit in Women with Early-Stage Breast Cancer Using EndoPredict, an Integrated 12-Gene Clinicomolecular Assay. JCO Precis. Oncol. 2019, 3, PO.18.00361. [Google Scholar] [CrossRef] [PubMed]
| Study | Country | Setting | BC Stage | Number of BC Specimens | Primary Proteomic Method | Additional Laboratory Methods | Main Findings |
|---|---|---|---|---|---|---|---|
| Abdullah et al., 2016 [16] | Saudi Arabia | Diagnosis | Primary | 20 | MALDI–TOF | n.a. | Biomarkers for diagnosis and pathogenesis |
| Akcakanat et al., 2021 [17] | USA | Therapy | Metastatic | 37 | RPPA | DNA and RNA sequencing | Biomarkers differentiating primary from metastatic BC |
| Akpinar et al., 2017 [18] | Turkey | Diagnosis | Primary | 10 | 2D–PAGE | n.a. | Biomarkers differentiating primary from metastatic BC |
| Al-Wajeeh et al., 2020 [20] | Malaysia | Diagnosis | Primary | 80 | SDS–PAGE andLC–MS/MS | n.a. | Biomarkers for staging |
| Asleh et al., 2022 [22] | Canada | Diagnosis | Primary | 300 | LC–MS/MS-based proteomics | IHC | Biomarkers for diagnosis and prognosis |
| Azevedo et al., 2023 [23] | Brazil | Diagnosis | Primary | 19 | High-throughput MS | IHC | Biomarkers for BC subtypes |
| Azevedo et al., 2022 [24] | Brazil | Diagnosis | Primary | 19 | LC–MS/MS | In silico transcriptomic analysis | Biomarkers for diagnosis and prognosis |
| Bateman et al., 2010 [25] | USA | Diagnosis | P, R, DCIS | 25 | LC–MS/MS | IHC | Biomarkers for disease progression and recurrence |
| Bernhardt et al., 2017 [29] | Germany | Diagnosis | Primary | 801 | RPPA | IHC | Biomarkers for prognosis |
| Bjørnstad et al., 2024 [30] | Norway | Diagnosis | Primary | 107 | MS | Ms in vitro | Biomarkers for diagnosis and pathogenesis |
| Bonneterre et al., 2013 [32] | France | Therapy | Primary | 149 | SELDI–TOF MS | n.a. | Biomarkers for response to therapy |
| Bouchal et al., 2015 [33] | Czech Republic | Diagnosis | Primary | 160 | iTRAQ-based proteomics | IHC, transcriptomics | Biomarkers for staging and nodal status |
| Braakman et al., 2015 [34] | Nedetherlands | Diagnosis | Primary | 11 | nano-LC–MS/MS | DNA analysis | Biomarkers for BC subtypes |
| Cabezón et al., 2012 [36] | Denmark | Therapy | Primary | 78 | 2D-PAGE and MS | 2D Western Immunoblotting, IHC | Biomarkers for therapy |
| Cancemi et al., 2012 [37] | Italy | Diagnosis | Primary | 100 | MALDI–TOF MS | IHC, Western blot | Biomarkers for disease progression |
| Cancemi et al., 2010 [38] | Italy | Diagnosis | Primary | 100 | MALDI–TOF MS | Western blot, n terminal microsequencing | Biomarkers for prognosis |
| Cawthorn et al., 2012 [39] | Canada | Diagnosis | Primary | 990 | iTRAQ and LC–MS/MS | IHC, SRM–MS | Biomarkers for prognosis |
| Champattanachai et al., 2013 [40] | Thailand | Diagnosis | Primary | 26 | LC–MS/MS | in vitro assays | Biomarkers for diagnosis and pathogenesis |
| Creighton et al., 2010 [42] | Spain | D and T | Primary | 429 | RPPA | In vitro assays and quantitative real-time PCR | Biomarkers for BC subtypes |
| Debets et al., 2023 [44] | Netherlands | Therapy | Primary | 45 | Phosphoproteomics | n.a. | Biomarkers for response to therapy |
| Di Cara et al., 2019 [45] | Italy | Diagnosis | Primary | 80 | MALDI–TOF MS | n.a. | Biomarkers for disease progression and prognosis |
| Duan et al., 2023 [47] | China | Therapy | Primary | 139 | MS | n.a. | Biomarkers for response to therapy |
| Fonseca-Sánchez et al., 2012 [49] | Mexico | Diagnosis | Primary | 105 | LC/ESI-MS/MS | IHC, Western blot | Biomarkers for BC subtypes |
| Gámez-Pozo et al., 2017 [53] | Spain | Diagnosis | Primary | 106 | LC–MS | MicroRNA expression analysis | Biomarkers for BC subtypes |
| Gámez-Pozo et al., 2017 [54] | Spain | Diagnosis | Primary | 60 | LC–MS | Parallel reaction monitoring | Biomarkers for prognosis |
| Gámez-Pozo et al., 2015 [55] | Spain | D and T | Primary | 96 | LC–MS/MS | MicroRNA expression and in vitro assays | Biomarkers for BC subtypes |
| García-Adrián et al., 2021 [56] | Spain | Therapy | Primary | 125 | MS | n.a. | Biomarkers for therapy |
| Gonzalez-Angulo et al., 2013 [62] | USA | Therapy | Primary | 175 | RPPA | IHC | Biomarkers for therapy |
| Gonzalez-Angulo et al., 2011 [63] | USA | D and T | P, M, DCIS | 880 | RPPA | IHC | Biomarkers for prognosis and response to therapy |
| Gromova et al., 2021 [65] | Denmark | Therapy | Primary | 44 | RPPA | IHC and PCR | Biomarkers for response to therapy |
| Guerin et al., 2018 [66] | France | Therapy | Primary | 46 | MS RPLC | Western blot | Biomarkers for response to therapy |
| Gustafsson et al., 2024 [67] | Sweden | Diagnosis | Primary | 63 | LC–MS/MS | n.a. | Biomarkers for diagnosis and pathogenesis |
| He et al., 2011 [68] | USA | D and T | Primary | 39 | LC–MS | IHC | Biomarkers for BC subtypes and response to therapy |
| He et al., 2009 [69] | USA | D and T | Primary | 52 | SELDI–TOF MS | IHC | Biomarkers for response to therapy |
| Hulahan et al., 2024 [73] | USA | Diagnosis | P and DCIS | 22 | Multiplexed spatial proteomics | n.a. | Biomarkers differentiating invasive from DCIS |
| Izani Othman et al., 2009 [74] | Malaysia | Diagnosis | Primary | 20 | LC–MS/MS | Western blot, MS | Biomarkers for diagnosis and pathogenesis |
| Jeon et al., 2024 [76] | South Korea | Therapy | Primary | 56 | Mass spectrometry | n.a. | Biomarkers for BC subtypes |
| Johansson et al., 2015 [77] | Sweden | Therapy | Primary | 24 | nanoLC–MS/MS | Western blot, ELISA | Biomarkers for response to therapy |
| Kang et al., 2010 [79] | South Korea | Diagnosis | P and DCIS | 164 | MALDI–TOF MS | IHC, Western blot | Biomarkers for diagnosis and pathogenesis |
| Kim et al., 2009 [82] | South Korea | Diagnosis | Primary | 17 | MALDI–TOF MS | n.a. | Biomarkers for disease progression |
| Ku et al., 2025 [155] | Taiwan | Therapy | Primary | 61 | nanoLC–MS/MS | NGS | Biomarkers for therapy |
| Lin et al., 2021 [87] | China | D and T | Primary | 24 | iTRAQ LC–MS/MS | Western blot | Biomarkers for BC subtypes |
| Magara et al., 2024 [90] | Japan | Therapy | P and DCIS | 133 | Multilayered proteomics | Multilayered proteomics in BC cells | Biomarkers for therapy |
| Meric-Bernstam et al., 2014 [93] | USA | Diagnosis | primary | 53 | RPPA | IHC | Response to surgical treatment |
| Michaut et al., 2016 [94] | Netherlands | Diagnosis | Primary | 55 | RPPA | cDNA-microarrays, DNA-sequencing, Western blot | Biomarkers for BC subtypes |
| Moriggi et al., 2018 [96] | Italy | Diagnosis | Primary | 26 | 2-DE, MALDI–MS | Gene expression microarrays, immunoblotting. | Biomarkers for BC subtypes |
| Nakagawa et al., 2006 [97] | USA | Diagnosis | Primary | 65 | SELDI–TOF MS | n.a. | Biomarkers for nodal status |
| Neubauer et al., 2008 [98] | Germany | Diagnosis | Primary | 16 | Quantitative multiplex proteomics | Western blot, immunofluoresence | Biomarkers for BC subtypes |
| Neubauer et al., 2006 [99] | Germany | Diagnosis | Primary | 24 | MALDI–TOF MS | n.a. | Biomarkers for response to therapy |
| Niméus et al., 2007 [100] | Sweden | D and T | Primary | 20 | MALDI–TOF-TOF MS | transcriptomics | Biomarkers for response to therapy |
| Ou et al., 2008 [101] | Singapore | Diagnosis | Primary | 63 | MALDI–TOF MS | cDNA microarrays, IHC, Western blot | Biomarkers for diagnosis and pathogenesis |
| Panis et al., 2013 [102] | Brazil | Diagnosis | P and M | 135 | label-free MS | Western blot, ELISA, IHC | Biomarkers for staging |
| Pozniak et al., 2016 [107] | Israel | Diagnosis | Primary | 41/25 | MS | Pulsed-SILAC Assay, IHC | High similarity in protein expression |
| Procházková et al., 2017 [108] | Czech Republic | Diagnosis | Primary | 96 | mTRAQ labeling (mTRAQ–SRM) | Transcriptomics, IHC | Biomarkers for disease progression |
| Pucci-Minafra et al., 2017 [109] | Italy | Diagnosis | Primary | 13 | 2D gel electrophoresis and MS | Western blot | Biomarkers for prognosis |
| Pucci-Minafra et al., 2007 [110] | Italy | Diagnosis | Primary | 37 | MALDI–TOF | Western blot | Biomarkers for diagnosis and pathogenesis |
| Roberts et al., 2004 [112] | Australia | Diagnosis | Primary | 27 | 2-DE | Western blot | Biomarkers for diagnosis and pathogenesis |
| Rojas et al., 2019 [113] | Spain | Diagnosis | P and M | 51 | PRM targeted proteomics | n.a. | Biomarkers for prediction of distant recurrence |
| Ruckhäberle et al., 2010 [114] | Germany | Diagnosis | Primary | 19 | Isobaric TMT label-based proteomics | Western blot, IHC, RNA expression microarray, LC–MS | Biomarkers for BC subtypes |
| Sanders et al., 2008 [116] | USA | Diagnosis | primary | 122 | MALDI–TOF MS | LC–MS/MS, IHC, HPLC | Biomarkers for disease progression, diagnosis and subtypes |
| Shenoy et al., 2020 [120] | Israel | Therapy | Primary | 113 | LC–MS/MS-based proteomic analysis | IHC, in vitro assays | Biomarkers for response to therapy |
| Shi et al., 2024 [121] | China | Therapy | Primary | 50 | MS-Based Label-Free Proteomics | in vitro assays | Biomarkers for therapy |
| Shin et al., 2020 [122] | South Korea | Diagnosis | P and M | 36 | Reversed-phase (RP)-nano LC–ESI–MS/MS | in vitro assays | Biomarkers for prediction of distant recurrence |
| Sohn et al., 2013 [124] | USA | Therapy | Primary | 54 | RPPA | n.a. | Biomarkers for response to therapy |
| Stemke-Hale et al., 2008 [126] | USA | D and T | Primary | 547 | RPPA | LC–MS/MS, IHC, Western blot, transcriptomics | Biomarkers for therapy |
| Tamesa et al., 2009 [128] | Japan | Diagnosis | Primary | 40/30 | LC–MS/MS | Western blot, transcriptomics | Biomarkers for diagnosis |
| Tyanova et al., 2016 [131] | Germany | Diagnosis | Primary | 40 | MS analysis | n.a. | Biomarkers for BC subtypes |
| Valo et al., 2019 [132] | France | Diagnosis | P and DCIS | 72 | SWATH–MS | IHC, ELISA | Biomarkers for diagnosis |
| Yang et al., 2016 [138] | China | Therapy | Primary | 36 | LC–MS/MS | n.a. | Biomarkers for response to therapy |
| Yang et al., 2015 [139] | China | Diagnosis | Primary | 60 | LC–MS/MS | n.a. | Biomarkers for BC subtypes |
| Yang et al., 2014 [140] | China | Diagnosis | Primary | 36 | LC–MS/MS | in vitro assays | Biomarkers for response to therapy |
| Yang et al., 2012 [141] | South Korea | Therapy | P and M | 83 | LC–MS/MS | IHC Western blot | Biomarkers for response to therapy |
| Yanovich et al., 2018 [142] | Israel | Diagnosis | Primary | 109 | LC–MS | n.a. | Biomarkers for BC subtypes |
| Zeng et al., 2017 [145] | China | Diagnosis | Primary | 23/23 | Quantitative iTRAQ | IHC | Biomarkers for prediction of distant recurrence |
| Zhang et al., 2008 [149] | Singapore | Diagnosis | primary | 94 | MALDI–TOF–TOF MS | IHC Western blot | Biomarkers for prognosis |
| Zhang et al., 2005 [150] | Singapore | Diagnosis | Primary | 25 | MALDI–TOF | IHC western blot, transcriptomics | Biomarkers for BC subtypes |
| Zhong et al., 2018 [153] | China | Diagnosis | Primary | 54/54 | iTRAQ | IHC | Biomarkers for nodal status |
| Study | Country | Setting | BC Stage | Type of Specimen | Number of BC Specimens | Primary Proteomic Method | Additional Laboratory Methods | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Alvarez et al., 2022 [19] | USA | Therapy | Primary | Plasma Evs | 17 | PPLC and LC–MS/MS | Western blot | Biomarkers for response to therapy |
| An et al., 2022 [21] | China | Diagnosis | Primary | Plasma | 107 | Nano-LC–MS/MS | Metabolomic analysis | Biomarkers for diagnosis |
| Belluco et al., 2007 [26] | Italy | Diagnosis | Primary | Serum | 155 | SELDI–TOF MS | n.a. | Biomarkers for early diagnosis |
| Bera et al., 2020 [27] | USA | Diagnosis | Primary | Serum | 240 | Antibody Microarrays and MSD Multi-array | n.a. | Biomarkers for recurrence prediction |
| Corrêa et al., 2017 [41] | Brazil | Diagnosis | Primary | Plasma | 107 | Nano-LC–MS/MS | IHC, FISH, Western blot | Biomarkers for BC subtypes |
| Dalenc et al., 2010 [43] | France | Therapy | Metastatic | Serum | 57 | SELDI–TOF MS | LC–MS/MS | Biomarkers for response to therapy |
| Drukier et al., 2006 [46] | USA | Diagnosis | Primary | Serum | 264 | IA/MPD | ELISA, Luminex | Biomarkers for early diagnosis |
| Fernandez-Pol et al., 2005 [48] | USA | D and T | P and M | Serum | 243 | HPLC | MS, Western blot, Radioimmunoassay | Biomarkers for diagnosis and response to therapy |
| Fredolini et al., 2020 [50] | USA | Diagnosis | Primary | Serum | 20 | Affinity hydrogel nanoparticles coupled with LC–MS/MS | n.a. | Biomarkers for early diagnosis |
| Gajbhiye et al., 2017 [51] | India | Diagnosis | Primary | Serum | 76 | 2D-DIGE, iTRAQ and SWATH–MS | n.a. | Biomarkers for BC subtypes |
| Garisi, Tommasi et al., 2012 [57] | Italy | Diagnosis | Primary | Serum | 192 | SELDI–TOF MS | n.a. | Biomarkers for BC subtypes |
| Garisi, Tufaro et al., 2012 [58] | Italy | Diagnosis | Primary | Serum | 138 | SELDI–TOF MS | n.a. | Biomarkers for diagnosis |
| Gast et al., 2011 [59] | Netherlands | Diagnosis | primary | Serum | 82 | SELDI–TOF MS | MALDI–TOF | Biomarkers for recurrence prediction |
| Goncalves et al., 2006 [61] | France | Diagnosis | primary | Serum | 81 | SELDI–TOF MS | Immunodepletion | Biomarkers for recurrence prediction |
| Grassmann et al., 2024 [64] | Sweden | Diagnosis | primary | Plasma | 796 | Proximity Extension Assay | n.a. | No benefit for recurrence prediction |
| Henderson et al., 2019 [70] | USA | Diagnosis | P and DCIS | Serum | 123 | Modified ECL based ELISA | n.a. | Biomarkers for early diagnosis |
| Henderson et al., 2016 [71] | USA | Diagnosis | P and DCIS | Serum | 100 | modified ELISA | n.a. | Biomarkers for early diagnosis |
| Hu et al., 2005 [72] | China | Diagnosis | P and M | Serum | 49 | SELDI–TOF MS | n.a. | Biomarkers for early diagnosis |
| Jordan et al., 2020 [77] | USA | D and T | primary | Plasma Evs | 20 | MS | Western blot, in vitro assays, Multiplex gene expression analysis | Biomarkers for diagnosis and therapy |
| Kaur et al., 2024 [79] | USA | Diagnosis | P and M | Serum | 73 | MS | n.a. | Biomarkers for disease progression |
| Kim et al., 2019 [81] | South Korea | Diagnosis | primary | Plasma | 575 | MRM MS | n.a. | Biomarkers for early diagnosis |
| Le Naour et al., 2001 [83] | USA | Diagnosis | primary | Serum | 30 | MALDI–TOF | Western blot, IHC | Biomarkers for early diagnosis |
| Li et al., 2024 [85] | China | Therapy | primary | Plasma | 40 | MS | Protein-protein interaction (PPI) analysis and Single-cell RNA sequencing | Biomarkers for response to therapy |
| Lötsch et al., 2022 [87] | Germany | Diagnosis | primary | Serum | 27 | PEA | n.a. | Biomarkers for neuropathic pain |
| Lourenco et al., 2017 [88] | USA | Diagnosis | primary | Serum | 26 | modified ELISA | n.a. | Biomarkers for early diagnosis |
| Majidzadeh-A et al., 2013 [90] | Iran | Therapy | primary | Serum | 10 | MALDI–TOF | n.a. | Biomarkers for response to therapy |
| Minton et al., 2013 [94] | UK | Diagnosis | primary | Serum | 45 | SELDI–TOF MS | LC–MS | Biomarkers for cancer Related Fatigue Syndrome |
| Pires et al., 2019 [106] | Brazil | Therapy | primary | Plasma | 200 | MS | Oxidative Stress Analyses | Biomarkers for response to therapy |
| Riley et al., 2011 [111] | USA | Diagnosis | P and DCIS | Serum | 216 | LC–MS/MS | n.a. | Biomarkers for diagnosis |
| Rui et al., 2003 [113] | China | Diagnosis | primary | Serum | 145 | MALDI–TOF | N-terminal sequencing | Biomarkers for diagnosis |
| Santana et al., 2024 [117] | Brazil | Diagnosis | primary | Plasma | 143 | LC–MS/MS | n.a. | Biomarkers for BC subtypes |
| Schaub et al., 2009 [119] | USA | Diagnosis | P, M and DCIS | Serum | 125 | MALDI–TOF MS | n.a. | Biomarkers for staging and nodal status |
| Sinha et al., 2023 [123] | USA | Diagnosis | primary | Saliva and Serum | 15 | iTRAQ analysis | n.a. | Biomarkers for early diagnosis |
| Starodubtseva et al., 2023 [125] | Russia | Diagnosis | metastatic | Serum | 25 | LC–MRM MS | Lipidomics | Biomarkers differentiating primary from metastatic BC |
| Suman et al., 2016 [127] | India | Diagnosis | primary | Plasma | 32 | iTRAQ analysis | Western blot, ELISA and IHC | Biomarkers for BC subtypes |
| Tomar et al. [154] | India | Diagnosis | P and M | Serum | 12 | MS | n.a | Biomarkers for diagnosis |
| Tutanova et al., 2020 [130] | Russia | Diagnosis | primary | Plasma, WBE | 23 | MS | Flow Cytometry | Biomarkers for diagnosis |
| Vinik et al., 2020 [133] | USA | Diagnosis | primary | Plasma Evs | 52 | RPPA | Immunoblotting | Biomarkers for early diagnosis |
| Xu et al., 2015 [135] | China | Diagnosis | primary | Serum | 60 | LC–MS/MS | ELISA | Biomarkers for response to therapy |
| Xu et al., 2024 [134] | China | Diagnosis | primary | Serum Evs | 126 | MS | IHC and in vitro cell assays | Biomarkers for early diagnosis and staging |
| Yan et al., 2022 [136] | China | Diagnosis | primary | Serum | 64 | MB–IMAC-Cu and MALDI–TOF MS | LC-ESI-MS/MS, ELISA | Biomarkers for diagnosis |
| Yang et al., 2020 [137] | China | Therapy | primary | Serum | 51 | Isobaric TMT label-based quantitative proteomics | LC–MS/MS | Biomarkers for response to therapy |
| Ye et al., 2024 [143] | China | Diagnosis | P and M | Plasma | 51 | UPLC–MS/MS | ELISA, metabolomics | Biomarkers differentiating different sites of metastasis |
| Zeidan et al., 2018 [144] | UK | Diagnosis | primary | Serum | 399 | LC–MS/MS | ELISA | Biomarkers for staging and nodal status |
| Zhang et al., 2013 [148] | USA | Diagnosis | P and DCIS | Serum | 100 | LC–MS/MS | n.a. | Biomarkers for early diagnosis |
| Zhang et al., 2015 [149] | USA | Diagnosis | primary | Serum | 80 | LC–MS/MS | n.a. | Biomarkers for early diagnosis |
| Zhang et al., 2013 [150] | USA | Diagnosis | primary | Plasma | 80 | LC–ESI–MS/MS | n.a. | Biomarkers for early diagnosis |
| Zhao et al., 2024 [152] | China | Diagnosis | primary | Plasma | 10 | LC–MS/MS | n.a. | Biomarkers for BC subtypes |
| Study | Country | Setting | BC Stage | Type of Specimen | Number of BC Specimens | Primary Proteomic Method | Additional Laboratory Methods | Main Findings |
|---|---|---|---|---|---|---|---|---|
| Brunoro et al., 2019 [35] | Brazil | Diagnosis | primary | NAF | 10 | MS | n.a. | Biomarkers differentiating BC from healthy |
| Kuerer et al., 2004 [82] | USA | Diagnosis | primary | NAF | 23 | SELDI–TOF MS | n.a. | Biomarkers for nodal status |
| Paweletz et al., 2001 [104] | USA | Diagnosis | primary | NAF | 12 | SELDI–TOF MS | n.a. | Biomarkers differentiating BC from healthy |
| Pawlik et al., 2006 [105] | USA | Diagnosis | primary | NAF | 18 | LC–MS/MS | Western blot | Biomarkers differentiating BC from healthy |
| Sauter et al., 2002 [118] | USA | Diagnosis | primary | NAF | 20 | SELDI–TOF MS | n.a. | Biomarkers differentiating BC from healthy |
| Beretov et al., 2015 [28] | Australia | Diagnosis | P and DCIS | Urine | 20 | LC–MS/MS | Western blot, IHC | Biomarkers differentiating BC from healthy |
| Gajbhiye et al., 2016 [52] | India | Diagnosis | primary | Urine | 43 | 2D-DIGE, iTRAQ, SWATH MS | Western blot | Biomarkers differentiating BC from healthy |
| Jeanmard et al., 2023 [74] | Thailand | Diagnosis | primary | Urinary EVs | 47 | LC–MS/MS | Western blot | Biomarkers differentiating BC from healthy |
| Giri et al., 2022 [60] | India | Diagnosis | metastatic | Saliva | 20 | PRM–MS | Western blot | Biomarkers differentiating BC from healthy |
| Zhang et al., 2010 [151] | USA | Diagnosis | primary | saliva | 40 | MALDI–TOF | Western blot | Biomarkers differentiating BC from healthy |
| Sinha et al., 2023 [123] | USA | Diagnosis | primary | Saliva, Serum | 15 | iTRAQ proteomic analysis | n.a. | Biomarkers differentiating BC from healthy |
| Böhm et al., 2012 [31] | Germany | Diagnosis | primary | Tear fluid | 25 | MALDI–TOF | n.a. | Biomarkers differentiating BC from healthy |
| Lebrecht et al., 2009 [84] | Germany | Diagnosis | primary | Tear fluid | 50 | SELDI–TOF MS | n.a. | Biomarkers differentiating BC from healthy |
| Mayayo-Peralta et al., 2024 [91] | Netherlands | Therapy | metastatic | Pleural effusions | 47 | Phosphoproteomics analysis | n.a. | Biomarkers for response to therapy |
| Terkelsen et al., 2020 [129] | Denmark | Diagnosis | primary | TIF | 35 | LC–MS/MS | IHC | Biomarkers for BC subtypes |
| Pathania et al., 2022 [103] | India | Diagnosis | primary | SLN | 13 | iTRAQ proteomic analysis and MS | ELISA | Biomarkers for nodal status |
| Pozniak et al., 2016 [107] | Israel | Diagnosis | primary | BC, LN | 41+25 | MS | Pulsed-SILAC, IHC | No difference in protein expression |
| Zeng et al., 2017 [145] | China | Diagnosis | primary | BC, LN | 23+23 | iTRAQ proteomic analysis | IHC | Biomarkers for nodal status |
| Zhong et al., 2018 [153] | China | Diagnosis | primary | BC, LN | 54+54 | iTRAQ proteomic analysis | IHC | Biomarkers for nodal status |
| Study | BC Stage | Type of Specimen | Number of BC Specimens | Primary Proteomic Method | Additional Laboratory Methods | Main Findings |
|---|---|---|---|---|---|---|
| Cawthorn et al., 2012 [39] | primary | Tumor | 990 | iTRAQ and LC–MS/MS | IHC, SRM–MS | High expression levels of Decorin and Endoplasmin (HSP90B1) are associated with increased metastasis-poorer survival and may guide the use of hormonal therapy. |
| Gonzalez-Angulo et al., 2011 [63] | P, M, DCIS | Tumor | 880 | RPPA | IHC | A 10-protein biomarker panel was developed that classifies breast cancer into prognostic groups that may have potential utility in the management of patients who receive anthracycline-taxane-based neoadjuvant systemic therapy. |
| Bernhardt et al., 2017 [29] | primary | Tumor | 801 | RPPA | IHC | SHMT2 and ASCT2 protein expression were identified as novel potential prognostic biomarkers for BC, as their high protein expression is associated with poor outcome. |
| Asleh et al., 2022 [22] | primary | Tumor | 300 | LC–MS/MS-based proteomics | IHC | Potential diagnostic and prognostic biomarkers were identified. |
| Cancemi et al., 2012 [37] | primary | Tumor | 100 | MALDI–TOF MS | IHC, Western blot | Deregulation of proteins of S100 family is associated with breast cancer progression and may serve as potential prognostic biomarkers for patient stratification. |
| Cancemi et al., 2010 [38] | primary | Tumor | 100 | MALDI–TOF MS | Western blot, n terminal microsequencing | S100A7 protein, with its two isoforms, serve a potential role in the progression and biological mechanisms of infiltrating ductal carcinoma. |
| Procházková et al., 2017 [108] | primary | Tumor | 96 | mTRAQ labeling (mTRAQ-SRM) | Transcriptomics, IHC | A panel of gene products that can contribute to breast cancer aggressiveness and metastasis was identified. |
| Zhang et al., 2008 [149] | primary | Tumor | 94 | MALDI–TOF-TOF MS | IHC Western blot | CK19 in HER-2+ breast cancer is associated with tumor aggressiveness, suggesting CK19’s potential role as a biomarker for identifying more aggressive BC subtypes. |
| Di Cara et al., 2019 [45] | primary | Tumor | 80 | MALDI–TOF MS | n.a. | MMP-2 and MMP-9 can be involved in the complicated scenario in which the mechanisms of tumor progression are correlated with unfavorable prognosis. |
| Kaur et al., 2024 [79] | P and M | Serum | 73 | MS | n.a. | A set of proteins that could be involved in breast cancer progression in serum was identified. |
| Gámez-Pozo et al., 2017 [54] | primary | Tumor | 60 | LC–MS | Parallel reaction monitoring | Some ER+/PR+ samples had a protein expression profile similar to that of triple negative breast cancer (TNBC) and had a clinical outcome similar to those with TNBC. |
| Study | BC Stage | Type of Specimen | Number of BC Specimens | Primary Proteomic Method | Additional Methods | Main Findings |
|---|---|---|---|---|---|---|
| Grassmann et al., 2024 [64] | primary | Plasma | 796 | Proximity Extension Assay | n.a. | No benefit for recurrence prediction |
| Kim et al., 2019 [81] | primary | Plasma | 575 | MRM MS | n.a. | Three specific peptides can be a useful tool for breast cancer screening and its accuracy is cancer-type specific. |
| Drukier et al., 2006 [46] | primary | Tumor | 264 | IA/MPD | ELISA, Luminex | Ultrasensitive, multi-biomarker immunoassays significantly improve early breast cancer detection accuracy. |
| Belluco et al., 2007 [26] | primary | Serum | 155 | SELDI–TOF MS | n.a. | A proteomic pattern consisting of 7 low-molecular-weight ion peaks is a highly sensitive and specific method for early detection of stage 1 breast cancer. |
| Xu et al., 2024 [134] | primary | Serum Evs | 126 | MS | IHC and in vitro cell assays | Proteins carried by breast cancer–derived EVs could be used as minimally invasive liquid biopsy tool for the early detection of breast cancer and for discriminating lymph node involvement and distant metastasis. |
| Henderson et al., 2019 [70] | P and DCIS | Serum | 123 | Modified ECL based ELISA | n.a. | Serum biomarkers provide clinicians with additional information for patients with indeterminate breast imaging results, potentially reducing false-positive breast biopsies. |
| Zhang et al., 2013 [148] | P and DCIS | Serum | 100 | LC–MS/MS | n.a. | Feed Forward Neural Network (FFNN) enhances the development of more accurate and reliable biomarker panels for the early diagnosis of breast cancer. |
| Henderson et al., 2016 [71] | P and DCIS | Serum | 100 | modified ELISA | n.a. | SPB and TAAb combinatorial protein biomarker assays may aid in the detection of early BC and guide decisions between imaging and tissue biopsy. |
| Zhang et al., 2015 [149] | primary | Serum | 80 | LC–MS/MS | n.a. | Pathway-based biomarkers can significantly enhance the early detection and diagnostic accuracy of breast cancer. |
| Zhang et al., 2013 [150] | primary | Plasma | 80 | LC-ESI-MS/MS | n.a. | Identification of eight alternative splicing isoform biomarkers can assist the early diagnosis of breast cancer. |
| Vinik et al., 2020 [133] | primary | Plasma Evs | 52 | RPPA | Immunoblotting | Several potential markers that could contribute to early detection of BC were identified. |
| Hu et al., 2005 [72] | P and M | Serum | 49 | SELDI–TOF MS | n.a. | SELDI–TOF-MS combined with bioinformatics tools is a promising approach for the early detection of breast cancer, identifying four candidate biomarkers. |
| Le Naour et al., 2001 [83] | primary | Serum | 30 | MALDI–TOF | Western blot, IHC | RS/DJ-1 is a novel circulating tumor antigen eliciting a humoral immune response in breast cancer patients and can be used for early detection and monitoring of BCr. |
| Study | BC Stage | Type of Specimen | Number of BC Specimens | Primary Proteomic Method | Additional Laboratory Methods | Main Findings |
|---|---|---|---|---|---|---|
| Creighton et al., 2010 [42] | primary | Tumor | 429 | RPPA | In vitro assays and quantitative real-time PCR | Hyperactive PI3K signaling is associated with low estrogen receptor (ER) levels and luminal B molecular subtype in ER-positive BC. |
| Garisi et al., 2012 [57] | primary | Serum | 192 | SELDI–TOF MS | n.a. | The serum profile of familial breast cancer patients was different when compared with that of sporadic breast cancer patients. |
| Santana et al., 2024 [117] | primary | Plasma | 143 | LC–MS/MS | n.a. | The HDL proteome showed discriminatory abilities across different clinical stages of breast cancer and a distinct profile in triple negative breast cancer. |
| Sanders et al., 2008 [116] | primary | Tumor | 122 | MALDI–TOF MS | LC–MS/MS, IHC, HPLC | S100A6 (calcyclin) and S100A8 (calgranulin A) highlight potential roles in cancer progression, diagnosis, and molecular classification. |
| Yanovich et al., 2018 [142] | primary | Tumor | 109 | LC–MS | n.a. | A novel luminal subtype characterized by increased PI3K signaling has been identified. |
| Corrêa et al., 2017 [41] | primary | Plasma | 107 | Nano-LC–MS/MS | IHC, FISH, Western blot | The plasma proteomic profile of breast cancer subtypes was determined. |
| Gámez-Pozo et al., 2017 [53] | primary | Tumor | 106 | LC–MS | MicroRNA expression analysis | ER+ BC and triple negative breast cancer exhibit distinct molecular and metabolic profiles. |
| Fonseca-Sánchez et al., 2012 [49] | primary | Tumor | 105 | LC/ESI-MS/MS | IHC, Western blot | Glyoxalase 1 (GLO1) is overexpressed in breast cancer and correlates significantly with high tumor grade. |
| Gámez-Pozo et al., 2015 [55] | primary | Tumor | 96 | LC–MS/MS | MicroRNA expression and in vitro assays | Some ER+/PR+ samples had a protein expression profile similar to that of triple negative breast cancer (TNBC) and had a clinical outcome similar to those with TNBC. |
| Gajbhiye et al., 2017 [51] | primary | Serum | 76 | 2D-DIGE, iTRAQ and SWATH-MS | n.a. | Serum proteome alterations may help to distinguish breast cancer subtypes (luminal A and, B, HER2-positive and triple negative BCr). |
| Jeon et al., 2024 [76] | primary | Tumor | 56 | Mass spectrometry | n.a. | Coronin-1A and titin were upregulated in the immune-inflamed subtype, and α-1-antitrypsin was upregulated in the immune-excluded/desert subtype. |
| Michaut et al., 2016 [94] | primary | Tumor | 55 | RPPA | cDNA-microarrays, DNA-sequencing, Western blot | Two biologically distinct subtypes of invasive lobular breast cancer were identified. |
| He et al., 2009 [69] | primary | Tumor | 52 | SELDI–TOF MS | IHC | Protein biosignatures were identified as having potential utility in tumor classification and predicting therapeutic responses. |
| Tyanova et al., 2016 [131] | primary | Tumor | 40 | MS analysis | n.a. | Global profiling of breast cancer clinical samples allows the attribution of biological processes to the different breast cancer subtypes (ER/PR, HER2 positive and TNBC). |
| Yang et al., 2014 [140] | primary | Tumor | 36 | LC–MS/MS | in vitro assays | The level of FR isoforms was associated with several histopathological features and molecular subtypes. |
| Terkelsen et al., 2020 [129] | primary | TIF | 35 | LC–MS/MS | IHC | Ten proteins, AGR3, BCAM, CELSR1, MIEN1, NAT1, PIP4K2B, SEC23B, THTPA, TMEM51, and ULBP2 stratify the tumor subtype-specific TIFs. |
| Suman et al., 2016 [127] | primary | Plasma | 32 | iTRAQ analysis | Western blot, ELISA and IHC | Four proteins (FN1, A2M, C4BPA and CFB) had strong association with molecular subtypes of breast cancer. |
| Study | BC Stage | Type of Specimen | Number of BC Specimens | Primary Proteomic Method | Additional Laboratory Methods | Main Findings |
|---|---|---|---|---|---|---|
| Gonzalez-Angulo et al., 2011 [63] | P, M, DCIS | Tumor | 880 | RPPA | IHC | A 10-protein biomarker panel was developed that classifies breast cancer into prognostic groups that may have potential utility in the management of patients who receive anthracycline-taxane-based neoadjuvant systemic therapy. |
| Fernandez-Pol et al., 2005 [48] | P and M | Serum | 243 | HPLC | MS, Western blot, Radioimmunoassay | MPS-1 is useful for early detection, monitoring, and management of breast cancer, superior than CA-15-3 and CEA. |
| Pires et al., 2019 [106] | primary | Plasma | 200 | MS | Oxidative Stress Analyses | The connection between inflammation, the complement and oxidative stress seems to be a pivotal axis in chemoresistance of luminal A breast cancer. |
| Bonneterre et al., 2013 [32] | primary | Tumor | 149 | SELDI–TOF MS | n.a. | A combined signature using the cytosol and plasma proteomic data may identify breast cancer patients like to achieve complete response in neoadjuvant chemotherapy. |
| Duan et al., 2023 [47] | primary | Tumor | 139 | MS | n.a. | 115 proteins were differentially expressed between patients with pathologic Complete Response (pCR) and the non-pCR group. |
| Shenoy et al., 2020 [120] | primary | Tumor | 113 | LC–MS/MS-based proteomic analysis | IHC, in vitro assays | Two proteins of proline biosynthesis pathway, PYCR1 and ALDH18A1, were significantly associated with resistance to treatment. |
| Yang et al., 2012 [141] | P and M | Tumor | 83 | LC–MS/MS | IHC Western blot | ERK/Bcl-2-mediated anti-apoptosis was investigated in general and in the development of drug resistance. |
| Xu et al., 2015 [135] | primary | Serum | 60 | LC–MS/MS | ELISA | SISCAPA-targeted proteomics alllowed quatification of low-abundant serum transferrin receptor in breast cancer patients pre- and post-chemotherapy. |
| Yang et al., 2015 [139] | primary | Tumor | 60 | LC–MS/MS | n.a. | TfR levels in breast tissue can be measured precisely with LC–MS/MS and could possibly improve the diagnosis of breast cancer and assessment of drug resistance. |
| Dalenc et al., 2010 [43] | metastatic | Serum | 57 | SELDI–TOF MS | LC–MS/MS | Fibrinogen α peptide could serve as a predictive biomarker for therapeutic response in ER+ breast cancer patients undergoing the tipifarnib and tamoxifen combination therapy. |
| Sohn et al., 2013 [124] | primary | Tumor | 54 | RPPA | n.a. | AKT, IGFBP2, LKB1, S6 and Stathmin predict relapse-free survival (RFS) in residual triple negative BC patients after neoadjuvant chemotherapy, while PI3K pathway may represent a potential therapeutic target. |
| Meric-Bernstam et al., 2014 [93] | primary | Tumor | 53 | RPPA | IHC | PI3K pathway activation is greater in core needle biopsy compared with postexcision surgical samples, suggesting a potential loss of phosphorylation during surgical manipulation, or with cold ischemia of surgical specimens. |
| He et al., 2009 [69] | primary | Tumor | 52 | SELDI–TOF MS | IHC | Protein biosignatures were identified as having potential utility in tumor classification and predicting therapeutic responses. |
| Yang et al., 2020 [137] | primary | Serum | 51 | Isobaric TMT quantitative proteomics | LC–MS/MS | A serum-based protein signature that potentially predicts the therapeutic effects of trastuzumab-based therapy for HER2-positive breast cancer patients was developed. |
| Mayayo-Peralta et al., 2024 [91] | metastatic | Pleural effusions | 47 | Phosphoproteomics analysis | n.a. | Evidence for decreased activity of several key kinases in ERα-converted metastases was found. |
| Guerin et al., 2018 [66] | primary | Tumor | 46 | MS RPLC | Western blot | Differential gene expression correlated with sensitivity to trastuzumab. |
| Debets et al., 2023 [44] | primary | Tumor | 45 | Phosphoproteomics | n.a. | Treatment response to trastuzumab, pertuzumab may be predicted. |
| Gromova et al., 2021 [65] | primary | Tumor | 44 | RPPA | IHC and PCR | High-level c-Kit expression is a frequent event in triple negative BC (TNBC), and activating mutations were also present, suggesting a potential effect of c-Kit inhibitors on TNBCs. |
| Li et al., 2024 [85] | primary | Plasma | 40 | MS | Protein-protein interaction (PPI) analysis and Single-cell RNA sequencing | Specific plasma proteins act as predictive biomarkers of response to immunotherapy. |
| He et al., 2011 [68] | primary | Tumor | 39 | LC–MS | IHC | Proteomic profiling of breast cancer tissues can predict tumor response to neoadjuvant chemotherapy. |
| Yang et al., 2016 [138] | primary | Tumor | 36 | LC–MS/MS | n.a. | FKBP4 and S100A9 are promising predictive biomarkers for determining drug resistance in breast cancer patients undergoing neoadjuvant chemotherapy. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zafrakas, M.; Gavalas, I.; Papasozomenou, P.; Emmanouilides, C.; Chatzidimitriou, M. Proteomics in Diagnostic Evaluation and Treatment of Breast Cancer: A Scoping Review. J. Pers. Med. 2025, 15, 177. https://doi.org/10.3390/jpm15050177
Zafrakas M, Gavalas I, Papasozomenou P, Emmanouilides C, Chatzidimitriou M. Proteomics in Diagnostic Evaluation and Treatment of Breast Cancer: A Scoping Review. Journal of Personalized Medicine. 2025; 15(5):177. https://doi.org/10.3390/jpm15050177
Chicago/Turabian StyleZafrakas, Menelaos, Ioannis Gavalas, Panayiota Papasozomenou, Christos Emmanouilides, and Maria Chatzidimitriou. 2025. "Proteomics in Diagnostic Evaluation and Treatment of Breast Cancer: A Scoping Review" Journal of Personalized Medicine 15, no. 5: 177. https://doi.org/10.3390/jpm15050177
APA StyleZafrakas, M., Gavalas, I., Papasozomenou, P., Emmanouilides, C., & Chatzidimitriou, M. (2025). Proteomics in Diagnostic Evaluation and Treatment of Breast Cancer: A Scoping Review. Journal of Personalized Medicine, 15(5), 177. https://doi.org/10.3390/jpm15050177






