Short-Term Effects of Land-Based Versus Water-Based Resistance Training Protocols on Post-Exercise Hypotension in Normotensive Men: A Crossover Study
Abstract
:1. Introduction
2. Materials and Methods
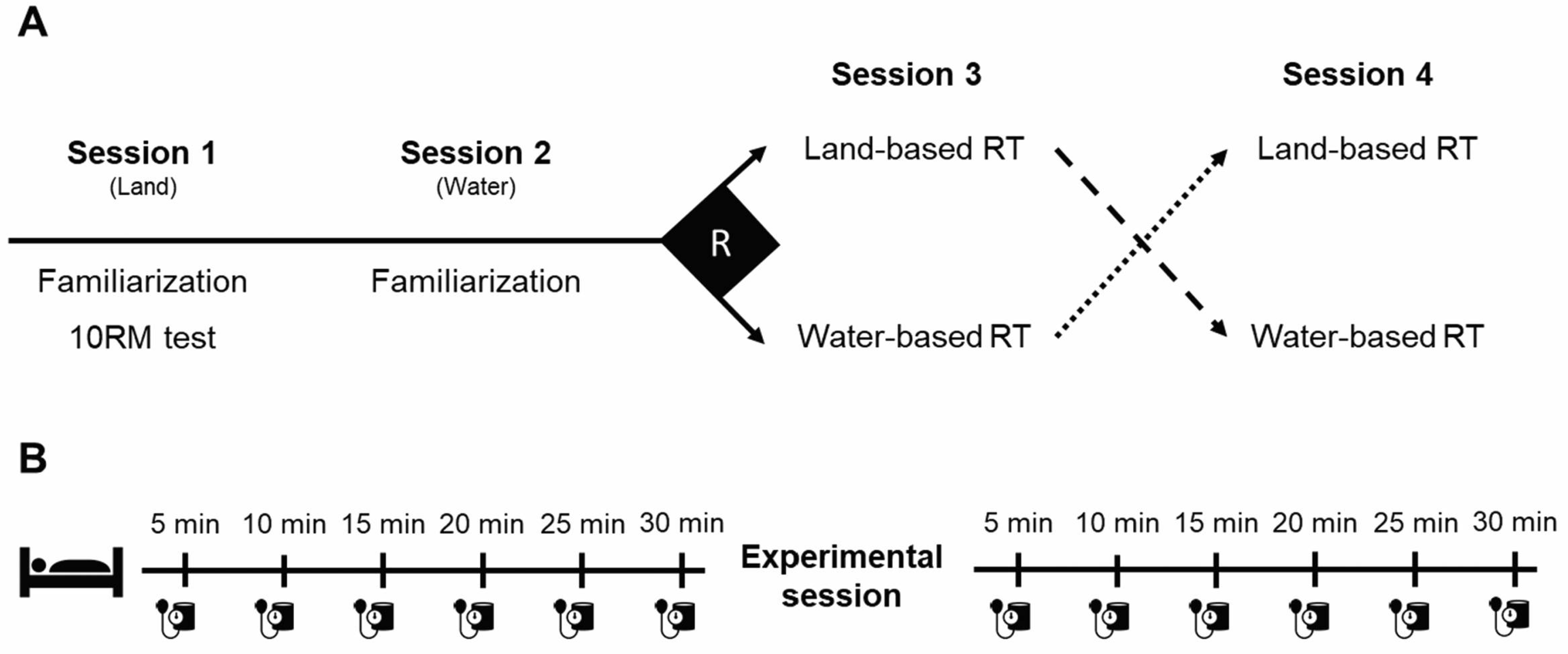
2.1. Experimental Design
2.2. Participants
2.3. Procedures
2.3.1. Familiarization
2.3.2. Resistance Training Protocols
2.4. Outcome Assessments
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 9 November 2022).
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Casonatto, J.; Goessler, K.F.; Cornelissen, V.A.; Cardoso, J.R.; Polito, M.D. The blood pressure-lowering effect of a single bout of resistance exercise: A systematic review and meta-analysis of randomised controlled trials. Eur. J. Prev. Cardiolog. 2016, 23, 1700–1714. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.S.; Franklin, B.A.; Fagard, R.; Farquhar, W.B.; Kelley, G.A.; Ray, C.A. American College of Sports Medicine position stand. Exercise and Hypertension. Med. Sci. Sports Exerc. 2004, 36, 533–553. [Google Scholar] [CrossRef]
- de Brito, L.C.; Fecchio, R.Y.; Peçanha, T.; Lima, A.; Halliwill, J.; de Moraes Forjaz, C.L. Recommendations in post-exercise hypotension: Concerns, best practices and interpretation. Int. J. Sports Med. 2019, 40, 487–497. [Google Scholar] [CrossRef] [Green Version]
- Craig, A.B.J.; Medd, W.L. Man’s responses to breath-hold exercise in air and in water. J. Appl. Physiol. 1968, 24, 773–777. [Google Scholar] [CrossRef]
- Srámek, P.; Simecková, M.; Janský, L.; Savlíková, J.; Vybíral, S. Human physiological responses to immersion into water of different temperatures. Eur. J. Appl. Physiol. 2000, 81, 436–442. [Google Scholar] [CrossRef]
- Rim, H.; Yun, Y.M.; Lee, K.M.; Kwak, J.T.; Ahn, D.W.; Choi, J.K.; Kim, K.R.; Joh, Y.D.; Kim, J.Y.; Park, Y.S. Effect of physical exercise on renal response to head-out water immersion. Appl. Hum. Sci. 1997, 16, 35–43. [Google Scholar] [CrossRef] [Green Version]
- Bocalini, D.S.; Bergamin, M.; Evangelista, A.L.; Rica, R.L.; Pontes, F.L.; Figueira, A.; Serra, A.J.; Rossi, E.M.; Tucci, P.J.F.; Dos Santos, L. Post-exercise hypotension and heart rate variability response after water- and land-ergometry exercise in hypertensive patients. PLoS ONE 2017, 12, e0180216. [Google Scholar] [CrossRef] [Green Version]
- Cunha, R.M.; Vilaça-Alves, J.; Noleto, M.V.; Silva, J.S.; Costa, A.M.; Silva, C.N.F.; Póvoa, T.I.R.; Lehnen, A.M. Acute blood pressure response in hypertensive elderly women immediately after water aerobics exercise: A crossover study. Clin. Exp. Hypertens. 2017, 39, 17–22. [Google Scholar] [CrossRef]
- Sosner, P.; Gayda, M.; Dupuy, O.; Garzon, M.; Lemasson, C.; Gremeaux, V.; Lalongé, J.; Gonzales, M.; Hayami, D.; Juneau, M.; et al. Ambulatory blood pressure reduction following high-intensity interval exercise performed in water or dryland condition. J. Am. Soc. Hypertens. 2016, 10, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Pontes, F.L.J.; Bacurau, R.F.P.; Moraes, M.R.; Navarro, F.; Casarini, D.; Pesquero, J.L.; Pesquero, J.B.; Araújo, R.C.; Piçarro, I.C. Kallikrein kinin system activation in post-exercise hypotension in water running of hypertensive volunteers. Int. Immunopharmacol. 2008, 8, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, D.; Silva, V.; Prestes, J.; Rica, R.L.; Serra, A.J.; Bocalini, D.S.; Pontes, F.L. Hypotensive response after water-walking and land-walking exercise sessions in healthy trained and untrained women. Int. J. Gen. Med. 2011, 4, 549–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cunha, R.M.; Macedo, C.B.; Araújo, S.F.; Santos, J.C.; Borges, V.S.; Soares, A.A.; Ayres, F.; Pfrimer, L.M. Subacute blood pressure response in elderly hypertensive women after a water exercise session: A controlled clinical trial. High Blood Press Cardiovasc. Prev. 2012, 19, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Cunha, R.M.; Costa, A.M.; Silva, C.N.F.; Póvoa, T.I.R.; Pescatello, L.S.; Lehnen, A.M. Postexercise hypotension after aquatic exercise in older women with hypertension: A randomized crossover clinical trial. Am. J. Hypertens. 2018, 31, 247–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ngomane, A.; Fernandes, B.; Guimarães, G.; Ciolac, E. Hypotensive effect of heated water-based exercise in older individuals with hypertension. Int. J. Sports Med. 2019, 40, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Terblanche, E.; Millen, A.M.E. The magnitude and duration of post-exercise hypotension after land and water exercises. Eur. J. Appl. Physiol. 2012, 112, 4111–4118. [Google Scholar] [CrossRef]
- Kruel, L.F.M.; Bgeginski, R.; Kanitz, A.C.; Pinto, S.S.; Almada, B.P.; Finatto, P.; Alberton, C.L. Blood pressure responses in hypertensive women to water aerobics. Apunt. Educ. Fís. Deporte. 2021, 144, 25–32. [Google Scholar]
- Pinto, S.S.; Umpierre, D.; Ferreira, H.K.; Nunes, G.N.; Ferrari, R.; Alberton, C.L. Postexercise hypotension during different water-based concurrent training intrasession sequences in young women. J. Am. Soc. Hypertens. 2017, 11, 653–659. [Google Scholar] [CrossRef]
- Guimaraes, G.V.; de Barros Cruz, L.G.; Fernandes-Silva, M.M.; Dorea, E.L.; Bocchi, E.A. Heated water-based exercise training reduces 24-hour ambulatory blood pressure levels in resistant hypertensive patients: A randomized controlled trial (HEx trial). Int. J. Cardiol. 2014, 172, 434–441. [Google Scholar] [CrossRef] [Green Version]
- Häfele, M.S.; Alberton, C.L.; Häfele, V.; Schaun, G.Z.; Nunes, G.N.; Calonego, C.; Castro, T.F.; Andrade, L.S.; Pinto, S.S. Water-based training programs improve functional capacity, cognitive and hemodynamic outcomes? The ACTIVE randomized clinical trial. Res. Q. Exerc. Sport 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Kercher, V.M.; Kercher, K.; Bennion, T.; Levy, P.; Alexander, C.; Amaral, P.C.; Li, Y.-M.; Han, J.; Liu, Y.; Wang, R.; et al. Fitness trends from around the globe. ACSMs Health Fit. J. 2022, 26, 21–37. [Google Scholar] [CrossRef]
- Prado, A.K.G.; Reichert, T.; Conceição, M.O.; Delevatti, R.S.; Kanitz, A.C.; Kruel, L.F.M. Effects of aquatic exercise on muscle strength in young and elderly adults: A systematic review and meta-analysis of randomized trials. J. Strength Cond. Res. 2022, 36, 1468–1483. [Google Scholar] [CrossRef] [PubMed]
- Carpio-Rivera, E.; Moncada-Jiménez, J.; Salazar-Rojas, W.; Solera-Herrera, A. Acute effects of exercise on blood pressure: A meta-analytic investigation. Arq. Bras. Cardiol. 2016, 106, 422–433. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.S.; Pollock, M.L. Generalized equations for predicting body density of men. Br. J. Nutr. 1978, 40, 497–504. [Google Scholar] [CrossRef] [Green Version]
- Siri, W.E. Body composition from fluid spaces and density: Analysis of methods. Nutrition 1993, 9, 480–491. [Google Scholar]
- Patteson Lombardi, V. Beginning Weight Training: The Safe and Effective Way; Brown & Benchmark Pub: Dallas, TX, USA, 1989. [Google Scholar]
- Pinto, S.S.; Cadore, E.L.; Alberton, C.L.; Zaffari, P.; Bagatini, N.C.; Baroni, B.M.; Radaelli, R.; Lanferdini, F.J.; Colado, J.C.; Pinto, R.S.; et al. Effects of intra-session exercise sequence during water-based concurrent training. Int. J. Sports Med. 2014, 35, 41–48. [Google Scholar] [CrossRef]
- Schoenell, M.C.; Alberton, C.L.; Tiggemann, C.L.; Noll, M.; Costa, R.; Santos, N.S.; Kruel, L.F. Effects of single vs. multiple sets during 10 weeks of water-based resistance training on neuromuscular adaptations in young women. Int. J. Sports Med. 2016, 37, 813–818. [Google Scholar] [CrossRef]
- Pöyhönen, T.; Kyröläinen, H.; Keskinen, K.L.; Hautala, A.; Savolainen, J.; Mälkiä, E. Electromyographic and kinematic analysis of therapeutic knee exercises under water. Clin. Biomech. 2001, 16, 496–504. [Google Scholar] [CrossRef]
- Sawilowsky, S.S. New effect size rules of thumb. J. Mod. Appl. Stat. Methods 2009, 8, 597–599. [Google Scholar] [CrossRef]
- Coelho-Junior, H.J.; Irigoyen, M.C.; Aguiar, S.D.S.; Gonçalves, I.O.; Câmara, N.O.S.; Cenedeze, M.A.; Asano, R.Y.; Rodrigues, B.; Uchida, M.C. Acute effects of power and resistance exercises on hemodynamic measurements of older women. Clin. Interv. Aging 2017, 12, 1103–1114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Queiroz, A.C.C.; Sousa, J.C.; Cavalli, A.A.; Silva, N.D.; Costa, L.A.; Tobaldini, E.; Montano, N.; Silva, G.V.; Ortega, K.; Mion, D.; et al. Post-resistance exercise hemodynamic and autonomic responses: Comparison between normotensive and hypertensive men. Scand. J. Med. Sci. Sports 2015, 25, 486–494. [Google Scholar] [CrossRef] [PubMed]
- Tajra, V.; Vieira, D.C.; Tibana, R.A.; Teixeira, T.G.; Silva, A.O.; Farias, D.L.; Nascimento, D.C.; De Sousa, N.M.; Willardson, J.; Prestes, J. Different acute cardiovascular stress in response to resistance exercise leading to failure versus not to failure in elderly women with and without hypertension—a pilot study. Clin. Physiol. Funct. Imaging 2015, 35, 127–133. [Google Scholar] [CrossRef] [PubMed]
- de Freitas, M.C.; Ricci-Vitor, A.L.; Quizzini, G.H.; De Oliveira, J.V.N.S.; Vanderlei, L.C.M.; Lira, F.S.; Rossi, F.E. Postexercise hypotension and autonomic modulation response after full versus split body resistance exercise in trained men. J. Exerc. Rehabil. 2018, 14, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Keese, F.; Farinatti, P.; Pescatello, L.; Monteiro, W. A Comparison of the immediate effects of resistance, aerobic, and concurrent exercise on postexercise hypotension. J. Strength Cond. Res. 2011, 25, 1429–1436. [Google Scholar] [CrossRef]
- Stavres, J.; Fischer, S.M.; McDaniel, J. Exaggerated post exercise hypotension following concentric but not eccentric resistance exercise: Implications for metabolism. Eur. J. Sport Sci. 2019, 19, 983–993. [Google Scholar] [CrossRef]
- Halliwill, J.R. Mechanisms and clinical implications of post-exercise hypotension in humans. Exerc. Sport Sci. Rev. 2001, 29, 65–70. [Google Scholar] [CrossRef]
- Cadore, E.L.; Lhullier, F.L.; Alberton, C.L.; Almeida, A.P.; Sapata, K.B.; Korzenowski, A.L.; Kruel, L.F. Salivary hormonal responses to different water-based exercise protocols in young and elderly men. J. Strength Cond. Res. 2009, 23, 2695–2701. [Google Scholar] [CrossRef] [Green Version]
- Costa, R.R.; Kanitz, A.C.; Reichert, T.; Prado, A.K.G.; Coconcelli, L.; Buttelli, A.C.K.; Pereira, L.F.; Masiero, M.P.B.; Meinerz, A.P.; Conceição, M.O.; et al. Water-based aerobic training improves strength parameters and cardiorespiratory outcomes in elderly women. Exp. Gerontol. 2018, 108, 231–239. [Google Scholar] [CrossRef]
- Halliwill, J.R.; Buck, T.M.; Lacewell, A.N.; Romero, S.A. Postexercise hypotension and sustained postexercise vasodilatation: What happens after we exercise? Exp. Physiol. 2013, 98, 7–18. [Google Scholar] [CrossRef]
- Pendergast, D.R.; Moon, R.E.; Krasney, J.J.; Held, H.E.; Zamparo, P. Human physiology in an aquatic environment. Compr. Physiol. 2015, 5, 1705–1750. [Google Scholar] [CrossRef] [PubMed]
- Gabrielsen, A.; Pump, B.; Bie, P.; Christensen, N.J.; Warberg, J.; Norsk, P. Atrial distension, haemodilution, and acute control of renin release during water immersion in humans. Acta Physiol. Scand. 2002, 174, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Hammerum, M.S.; Bie, P.; Pump, B.; Johansen, L.B.; Christensen, N.J.; Norsk, P. Vasopressin, angiotensin II and renal responses during water immersion in hydrated humans. J. Physiol. 1998, 511, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Pendergast, D.R.; de Bold, A.J.; Pazik, M.; Hong, S.K. Effect of head-out immersion on plasma atrial natriuretic factor in man. Proc. Soc. Exp. Biol. Med. 1987, 184, 429–435. [Google Scholar] [CrossRef]
- Pantoja, P.D.; Alberton, C.L.; Pilla, C.; Vendrusculo, A.P.; Kruel, L.F.M. Effect of resistive exercise on muscle damage in water and on land. J. Strength Cond. Res. 2009, 23, 1051–1054. [Google Scholar] [CrossRef]
- Batrakoulis, A.; Jamurtas, A.Z.; Metsios, G.S.; Perivoliotis, K.; Liguori, G.; Feito, Y.; Riebe, D.; Thompson, W.R.; Angelopoulos, T.J.; Krustrup, P.; et al. Comparative efficacy of five exercise types on cardiometabolic health in overweight and obese adults: A systematic review and network meta-analysis of randomized controlled trials. Circ. Cardiovasc. Qual Outcomes 2022, 15, e008243. [Google Scholar] [CrossRef]
- Pescatello, L.S.; MacDonald, H.V.; Lamberti, L.; Johnson, B.T. Exercise for hypertension: A prescription update integrating existing recommendations with emerging research. Curr. Hypertens. Rep. 2015, 17, 87. [Google Scholar] [CrossRef] [Green Version]
- MacDonald, H.V.; Johnson, B.T.; Huedo-Medina, T.B.; Livingston, J.; Forsyth, K.C.; Kraemer, W.J.; Farinatti, P.T.; Pescatello, L.S. Dynamic resistance training as stand-alone antihypertensive lifestyle therapy: A meta-analysis. J. Am. Heart Assoc. 2016, 5, e003231. [Google Scholar] [CrossRef]


| Variables | Mean ± SD |
|---|---|
| Age (years) | 23.2 ± 3.12 |
| Body mass (kg) | 75.7 ± 9.0 |
| Height (cm) | 175.0 ± 0.3 |
| Body fat (%) | 13.5 ± 3.0 |
| Variables | Land-Based Resistance Training Protocol | Water-Based Resistance Training Protocol | |
|---|---|---|---|
| Mean (95% CI) | Mean (95% CI) | d (95% CI) | |
| SBP (mmHg) | |||
| 5 min post | −4.4 (−10.2 to 1.4) | −11.6 (−20.9 to −2.3) | 0.67 (−0.24 to 1.47) |
| 10 min post | 0.1 (−6.5 to 6.7) | −11.6 (−21.1 to −2.1) | 1.02 (0.06 to 1.83) |
| 15 min post | 3.7 (−3.9 to 11.3) | −11.9 (−21.2 to −2.6) | 1.32 (0.30 to 2.12) |
| 20 min post | −0.5 (−7.2 to 6.2) | −9.0 (−17.8 to −0.2) | 0.78 (−0.14 to 1.59) |
| 25 min post | 2.0 (−3.9 to 7.9) | −12.1 (−23.1 to −1.1) | 1.00 (0.04 to 1.80) |
| 30 min post | 0.5 (−7.0 to 8.0) | −7.3 (−14.6 to 0.0) | 0.75 (−0.17 to 1.56) |
| DBP (mmHg) | |||
| 5 min post | −12.8 (−17.8 to −7.8) | −16.4 (−23.2 to −9.1) | 0.41 (−0.46 to 1.22) |
| 10 min post | −11.0 (−16.7 to −5.3) | −15.0 (−24.0 to −6.0) | 0.38 (−0.49 to 1.19) |
| 15 min post | −9.3 (−14.9 to −3.7) | −11.9 (−19.9 to −3.9) | 0.27 (−0.59 to 1.09) |
| 20 min post | −9.9 (−16.1 to −3.8) | −14.6 (−21.7 to −7.5) | 0.50 (−0.38 to 1.31) |
| 25 min post | −7.0 (−13.1 to −0.9) | −12.3 (−19.5 to −5.1) | 0.52 (−0.37 to 1.33) |
| 30 min post | −6.7 (−13.3 to −0.9) | −11.4 (−17.5 to −5.3) | 0.53 (−0.36 to 1.34) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
David, G.B.; Schaun, G.Z.; Mendes, A.R.; Nunes, G.N.; Bocalini, D.S.; Pinto, S.S.; Alberton, C.L. Short-Term Effects of Land-Based Versus Water-Based Resistance Training Protocols on Post-Exercise Hypotension in Normotensive Men: A Crossover Study. Sports 2022, 10, 181. https://doi.org/10.3390/sports10110181
David GB, Schaun GZ, Mendes AR, Nunes GN, Bocalini DS, Pinto SS, Alberton CL. Short-Term Effects of Land-Based Versus Water-Based Resistance Training Protocols on Post-Exercise Hypotension in Normotensive Men: A Crossover Study. Sports. 2022; 10(11):181. https://doi.org/10.3390/sports10110181
Chicago/Turabian StyleDavid, Gabriela Barreto, Gustavo Zaccaria Schaun, Amanda Ricardo Mendes, Gabriela Neves Nunes, Danilo Sales Bocalini, Stephanie Santana Pinto, and Cristine Lima Alberton. 2022. "Short-Term Effects of Land-Based Versus Water-Based Resistance Training Protocols on Post-Exercise Hypotension in Normotensive Men: A Crossover Study" Sports 10, no. 11: 181. https://doi.org/10.3390/sports10110181
APA StyleDavid, G. B., Schaun, G. Z., Mendes, A. R., Nunes, G. N., Bocalini, D. S., Pinto, S. S., & Alberton, C. L. (2022). Short-Term Effects of Land-Based Versus Water-Based Resistance Training Protocols on Post-Exercise Hypotension in Normotensive Men: A Crossover Study. Sports, 10(11), 181. https://doi.org/10.3390/sports10110181








