Abstract
This study aimed to investigate the effects of eight weeks of barefoot running exercise on sand versus control on measures of walking kinetics and muscle activities in individuals with diagnosed pronated feet. Sixty physically active male adults with pronated feet were randomly allocated into an intervention or a waiting control group. The intervention group conducted an 8-weeks progressive barefoot running exercise program on sand (e.g., short sprints) with three weekly sessions. Pre and post intervention, participants walked at a constant speed of 1.3 m/s ± 5% on a 18 m walkway with a force plate embedded in the middle of the walkway. Results showed significant group-by-time interactions for peak impact vertical and lateral ground reaction forces. Training but not control resulted in significantly lower peak impact vertical and lateral ground reaction forces. Significant group-by-time interactions were observed for vastus lateralis activity during the loading phase. Training-induced increases were found for the vastus lateralis in the intervention but not in the control group. This study revealed that the applied exercise program is a suitable means to absorb ground reaction forces (e.g., lower impact vertical and lateral peaks) and increase activities of selected lower limb muscles (e.g., vastus lateralis) when walking on stable ground.
1. Introduction
Foot pronation has previously been defined as a normal rolling movement localized at the subtalar joint of the foot [1]. More specifically, foot pronation primarily occurs during the first half of the walking stance phase [2] and is characterized by ankle eversion and dorsiflexion as well as abduction of the forefoot [2]. However, excessive foot pronation is related to lower limb malalignment and may cause musculoskeletal injuries [3]. In youth aged 2–16 years, prevalence rates for individuals with pronated feet (PF) range between 48% and 78% [4]. For adults aged 18–50 years, prevalence rates are in the range of 2–23% [5,6,7].
With regards to the biomechanics of walking, there is evidence that individuals with PF show a significantly lower second peak (propulsion phase) of vertical ground reaction force (GRF) [1], greater lateral-medial GRF [8], and greater [9] or similar [8] peak-free moment amplitudes. Of note, different researchers have observed that greater peak vertical GRF during heel contact and vertical loading rates are associated with walking and/or running-related injuries [8,10]. Pronation velocity has previously been used to assess running stability properties, and there seems to be an association between pronation velocity and running injuries such as patella femoral pain syndrome [11,12,13].
Free moment amplitudes have been introduced as a marker of lower limb torsional load [14,15], and greater free moment amplitudes may constitute a risk factor for tibial stress fractures in runners [8,14]. With regards to muscle activities, there is evidence that individuals with PF compared with age-matched healthy controls showed both, higher lower limb muscle activities (i.e., tibialis anterior/posterior, plantar flexors) as well as lower activities of evertor muscles (e.g., peroneus) [16]. Data from original research [17] indicated that participants with a history of lower limb overuse injuries such as stress fractures showed a greater subtalar pronation excursion. A recent systematic review and meta-analysis reported high effect sizes in the range of 0.78 to 1.52 for PF posture as a risk factor for developing the tibial stress fracture and low effect sizes (effect size = 0.28 to 0.33) for PF posture as a risk factor to suffer from patellofemoral pain [18]. Another systematic review [19] showed trivial to moderate effects (effect size = 0.10 to 0.61) for rearfoot kinematic variables as a risk factor for patellofemoral pain. A recent meta-analysis indicated that peak rearfoot eversion was the only significant risk factor associated with the development of lower limb tendinopathy [20]. Accordingly, Mousavi et al. [20] concluded that rearfoot kinematics and kinematic chain movements should be considered in the prevention and management of lower limb tendinopathy. Therefore, it is important to design and develop adequate training regimens for PF treatment.
Sand could be a promising means to be used in PF therapy because it is rather easy to access worldwide and cost-effective. Of note, sand is characterized by high shock absorption during the loading phase [21]. At the same time, the unstable surface poses great demands on the somatosensory system due to its unpredictable three-dimensional surface [21]. There is preliminary evidence that walking or running on sand has a significant impact on the kinetics and kinematics of locomotion [21,22]. In addition, a previous study has shown that exercise on sand compared with training on firm ground increases energy costs and reduces impact forces [23].
Of note, specific biomechanical and physiological characteristics are associated with exercising on sand [22,23]. For instance, walking on sand resulted in significant increases in hip flexion, knee flexion, and ankle dorsiflexion angles in multiple sclerosis patients during the swing phase of walking [21]. Another study demonstrated lower free moment amplitudes and vertical loading rates when walking on sand [22]. Accordingly, sand seems to absorb impact forces and may thus reduce muscle damage and soreness [24]. In a previous study, we evaluated the effects of long-term training on sand on lower limb muscle activities during running but not walking [25]. Of note, walking mechanics are different from running mechanics with regard to the magnitude of ground reaction forces and muscle activities [26,27,28]. Therefore, it is timely to examine the effects of long-term exercising on sand on walking kinetics and muscle activities since walking is a natural human activity. Therefore, this study aimed to investigate the effects of 8-weeks of barefoot running exercise on sand versus control on measures of walking kinetics and muscle activities in individuals with diagnosed pronated feet. We hypothesized that exercise on sand decreases GRF amplitudes, loading rates, and free moment amplitudes and increases muscle activities during walking [21,22].
2. Materials and Methods
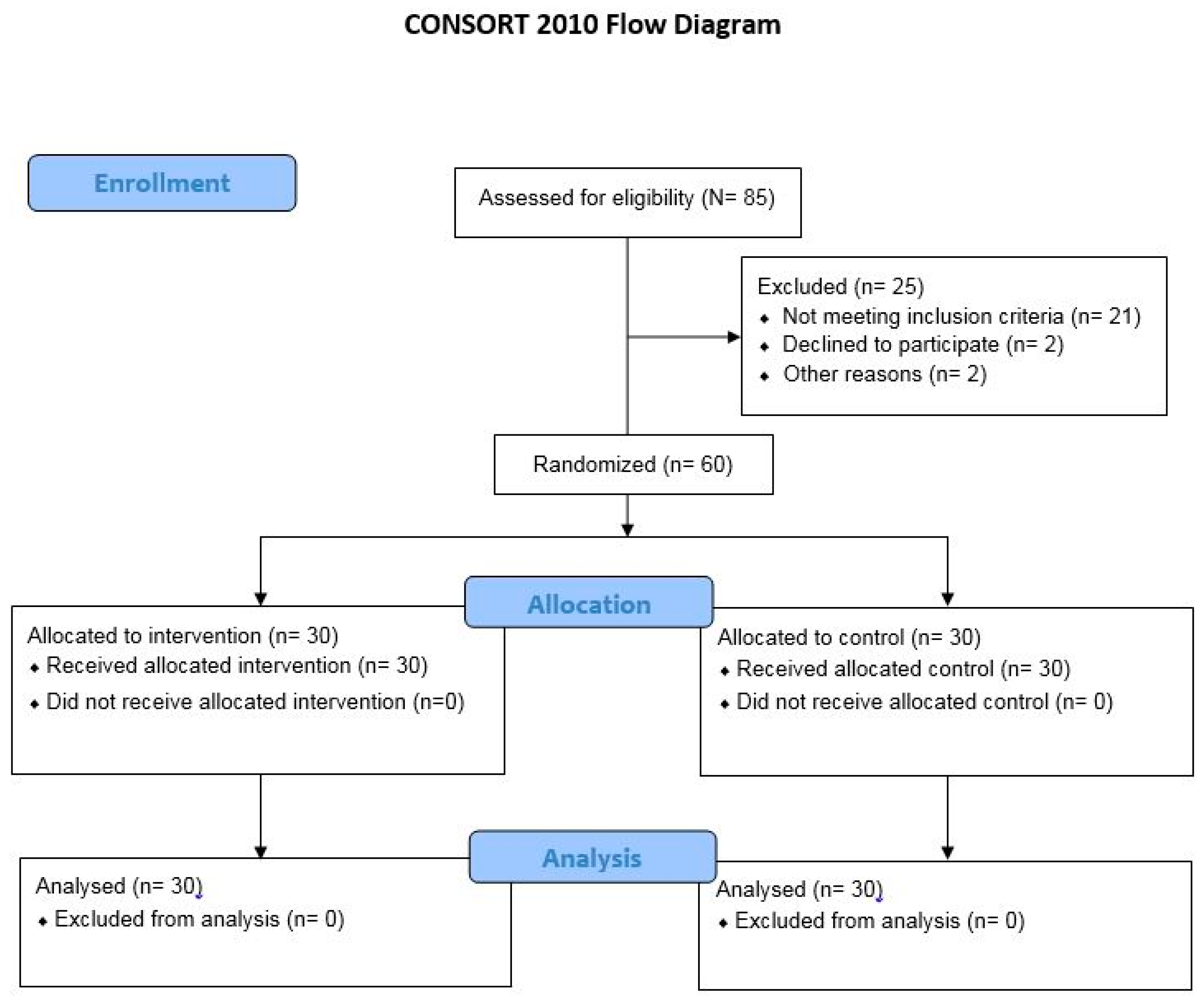
This study was designed as a double-blinded randomized controlled trial (Figure 1). An envelope concealment method was used to allocate study participants. Participants and examiners were unaware of group allocation. In other words, participants and assessors were blinded.
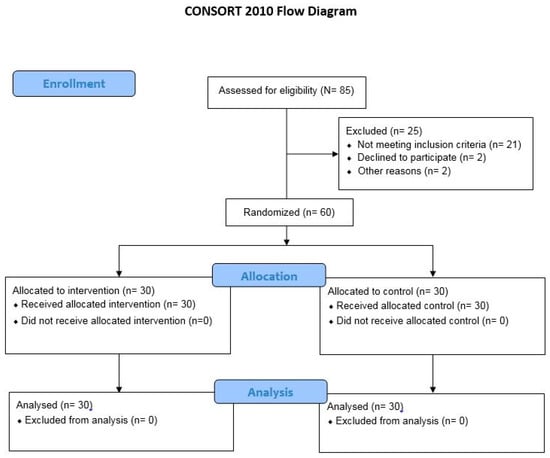
Figure 1.
Flow diagram of the randomized controlled trial.
The G*Power software was used to calculate an a priori power analysis with the F-test family using a related study as a reference that evaluated the kinetics of walking in male adults with PF [8]. An alpha level of 0.05, a type II error rate of 0.20, and an effect size of 0.80 for peak vertical GRF from the study of Jafarnezhadgero et al. [22] were used to compute the power analysis. Findings showed that at least 20 participants per group would be needed to receive a significant group-by-time interaction effect.
Sixty participants aged 18–26 years with diagnosed PF were recruited from a clinic in Ardabil City, Iran, and were randomly allocated into an intervention or a waiting control group. A kicking ball test indicated that all participants were right foot dominant [29]. Given that males and females differ with regard to their biomechanical characteristics during walking, we recruited males only [30]. To be included in this study, participants had to be male, show a navicular drop of >10 mm [22], rear foot eversion of >4° [31], and a Foot Posture Index of >10 [22]. An orthopedic specialist diagnosed the participants during static standing [32,33]. The static measurements of the calcaneal deviation and the medial arch angle were recorded while the participants stood barefoot and in an erect stance position on a level floor [31]. Calcaneal deviation was defined as the angle between the posterior midline of the calcaneus and perpendicular line to the level floor that was measured with a protractor. The Foot Posture Index includes six items in order to classify foot type [33,34]. A full definition of the Foot Posture Index has previously been reported in the literature [33,34]. As exclusion criteria, we defined: (i) history of trunk and/or lower limbs surgery, (ii) orthopedic conditions (except for PF), and (iii) greater than 5 mm limb length differences. Prior to the start of the study, the study procedures were described to all participants. Thereafter, written informed consent was obtained from the study participants. The study protocol was approved by the local ethics committee of the Ardabil Medical Sciences University (IR.ARUMS.REC.1398.484) and registered by the Iranian clinical trial organization (IRCT20191211045704N1). The study was conducted in agreement with the latest version of the Declaration of Helsinki. Appendix A (Table A1) illustrates the CONSORT 2010 checklist.
2.1. Experimental Set-Up and Data Processing
To collect GRF data during walking on stable ground, a force platform (Bertec Corporation, Columbus, OH, USA) was used and embedded in an 18-m walkway. During testing, subjects walked barefoot at a constant speed of ~1.3 m/s ± 5%. Speed of walking was monitored through two sets of infrared photocells. As previously described by Jafarnezhadgero et al. [35], kinetic data were sampled at 1000 Hz. GRFs were smoothed using a 20 Hz (4th order Butterworth filter, zero lag) low-pass filter. Heel contact and toe off were determined through the Bertec force plate. A 10 N threshold was used to determine the stance phase of the walking. The dependent variables extracted from GRF data include [35] first (FzHC) and second vertical peak force (FzPO), braking (FyHC) and propulsion forces (FyPO), and the lateral (FxHC) and medial GRF (FxPO) peaks. Peak GRF values were normalized using body weight (BW). The time period between the heel strike and the corresponding peak of FzHC was defined as TTP [8]. The slope between heel strike and FzHC on the vertical curve was defined as loading rate [8]. The free moment values were calculated as follows [8]:
where Mz is defined as the moment around the vertical axis, x and y are medio-lateral and anterior-posterior components of the center of pressure (CoP), and Fx and Fy are the medio-lateral and anterior-posterior GRF components. Moreover, free moment values were normalized using BW × height. All dependent variables were averaged across five trials [35].
An electromyographic apparatus (Biometrics Ltd., Nine Mile Point Ind. Est, Newport, U.K.) with bipolar Ag/AgCl surface electrodes (25 mm center-to-center distance; input impedance of 100 MΩ; and common mode rejection ratio of >110 dB) was applied to record electromyographic data of the tibialis anterior, medial gastrocnemius, biceps femoris, semitendinosus, vastus lateralis, vastus medialis, rectus femoris, and gluteus medius muscles of the right limb [36]. Raw electromyographic data were recorded at a sampling rate of 1000 Hz. The skin surface was cleaned and shaved using alcohol to lower impedance in accordance with the European recommendations for surface electromyography (SENIAM). The stance phase was divided into the loading (0–20% of gait cycle), mid-stance (20–47% of gait cycle), and push-off (47–70% of gait cycle) sub-phases for electromyographic analyses [22]. Maximum voluntary isometric contraction (MVIC) was recorded using a handheld dynamometer along with an isometric belt (where the joint is locked) [37] for each muscle separately to normalize electromyographic amplitudes during walking to MVIC (Appendix B, Table A2). The applied normalization procedures were realized in accordance with recommendations from Besomi et al. [37]. For example, the participants were encouraged to perform the tests at maximal effort [37]. Three test trials were conducted with rest periods of 1–2 min in between [37]. This instrument is important to standardize the test during the performance of maximal contractions. The maximum value of the MVIC test was considered for normalization purposes [37].
2.2. Experimental Procedures
A 5 min warm-up protocol consisting of 2 min jogging followed by 3 min stretching was conducted with all participants prior to testing. Participants walked barefoot across the 18-m walkway at a constant speed of 1.3 m/s. Walking speed was monitored using electronic timing gates (Swift Performance Equipment, Wacol, New South Wales, Australia). Five successful test trials had to be performed. If the foot touched the middle of the force plate and if electromyography signals were artifact-free, a trial was considered successful. MVIC tests were performed after the walking trials for each muscle to normalize electromyography data (Appendix B, Table A2). Similar procedures were applied during pre and post testing.
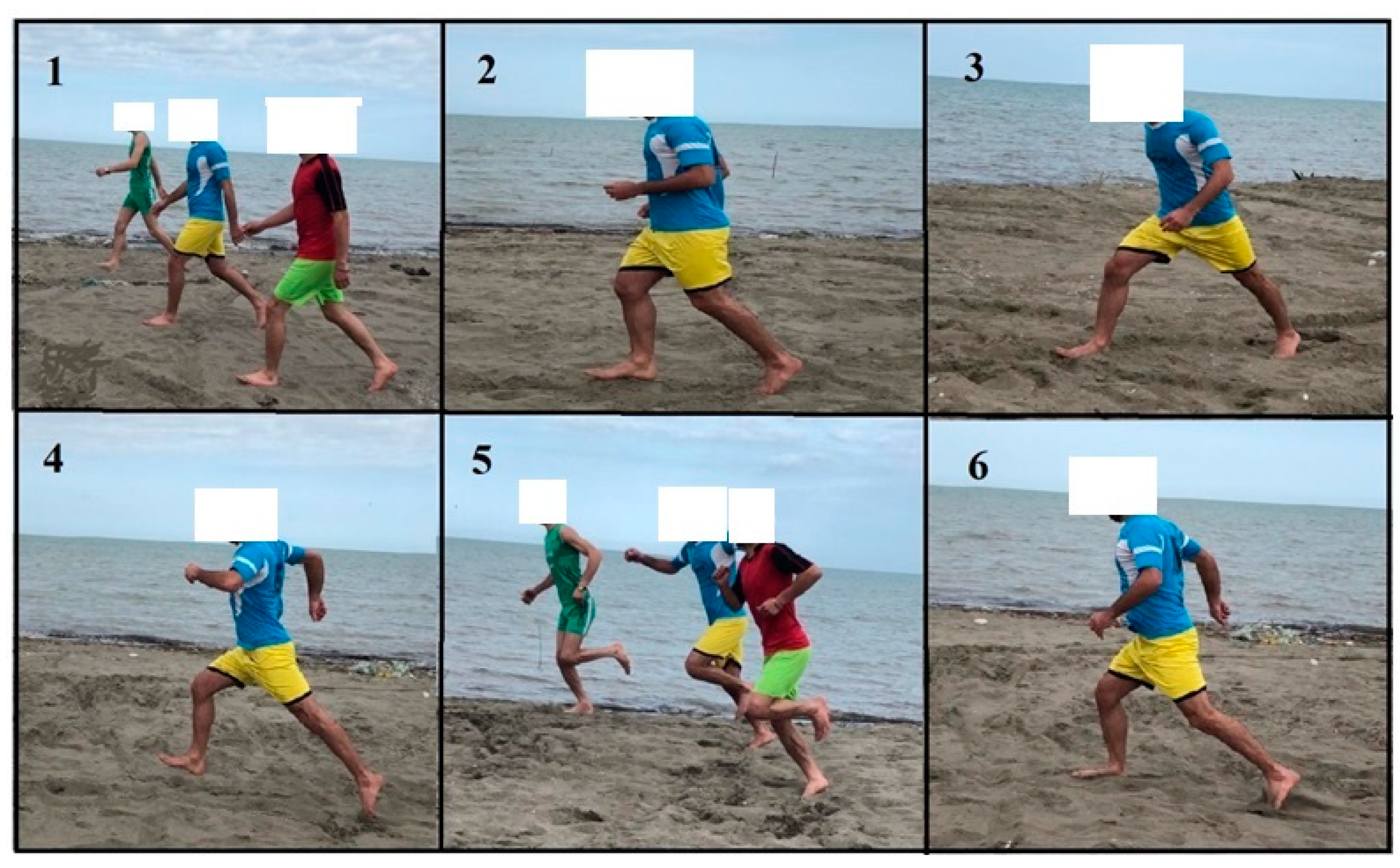
The intervention group performed running exercises on sand over a period of 8 weeks with three sessions per week. The intervention program was progressively designed using walking, jogging, striding, bounding, and galloping exercises and, finally, short sprints [38] (Figure 2). Exercises were always performed barefoot and on sand. Every training session started with a 5 min warm-up program, including walking and submaximal running exercises and a dynamic stretching program. The main part of the exercise session lasted 40 min and included different types of exercises on sand [25]. The session ended with a 5 min cool-down [38]. Taken together, the duration of a single training session lasted 50 min [38]. Exercise intensity (i.e., running speed) was controlled using a stopwatch and predefined running distances on the sand-based exercise court. More detailed information on the exercise program is presented in Table 1 and Figure 2 and in a previous study by Jafarnezhadgero et al. [25]. During the intervention period, the control group performed their regular daily activities and did not perform any additional training or treatment protocols. After the post-test, individuals from the control group had the chance to receive the same training protocol as the intervention group.
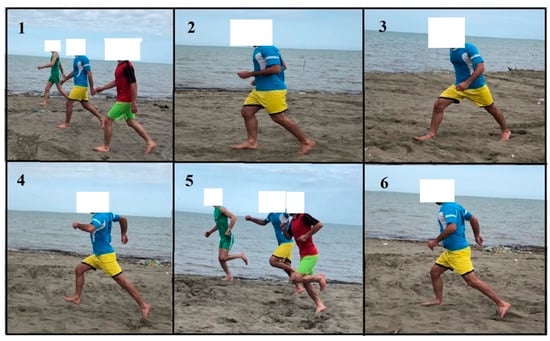
Figure 2.
Exemplified exercises of the intervention on sand. (1) Walking task; (2) jogging task; (3) striding task; (4) bounding task; (5) galloping task; and (6) short sprints. Written informed consent was obtained from the individual for the publication of the image.

Table 1.
Exemplified exercises on sand together with training volume and intensity of the intervention group.
2.3. Statistical Analyses
The normal distribution of data was confirmed through the Shapiro–Wilk test. An independent-sample t-test was applied to detect between-group differences at baseline. A 2 (groups: intervention, control) by 2 (time: pre, post) ANOVA for repeated measures was used to evaluate potential intervention effects. In the case of statistically significant group-by-time interactions, group-specific and Bonferroni-adjusted post-hoc tests were applied. Moreover, effect sizes were calculated by converting partial eta-squared (η2p) from ANOVA output to Cohen’s d. In accordance with Cohen [39], d < 0.50 demonstrate small effects, 0.50 ≤ d < 0.80 demonstrate medium effects, and d ≥ 0.80 demonstrate large effects. Statistical significance was set at p < 0.05. The Statistical Package for Social Sciences (SPSS) version 20.0 was used for all statistical analyses.
3. Results
All participants received treatments as allocated. Table 2 illustrates group-specific baseline data for all outcome variables. No significant between-group baseline differences were found for all examined parameters (Table 2), but the static rear foot eversion was reduced (p < 0.001; d = 2.83) in the intervention group at post compared with pre test (pre: 7.0 ± 0.5; post: 5.3 ± 0.7). No statistically significant pre-post differences were found for static rear foot eversion for the control group (p > 0.05; pre: 7.0 ± 0.8; post: 7.0 ± 0.7).

Table 2.
Mean (SD) baseline values for the intervention and the waiting control group for all reported outcome variables.
Significant main effects of “time” (p < 0.002; d = 0.87–0.89) and group-by-time interactions (p < 0.001; d = 0.94–1.18) were found for FzHC and FxHC (Table 3). Exercise resulted in significant reductions in FzHC (p = 0.001; d = 0.86) and FxHC (p < 0.001; d = 1.33) in the intervention but not the control group.

Table 3.
Group-specific pre-post data for ground reaction forces during walking at constant speed. Descriptive data are illustrated as means (SD) and 95% confidence intervals.
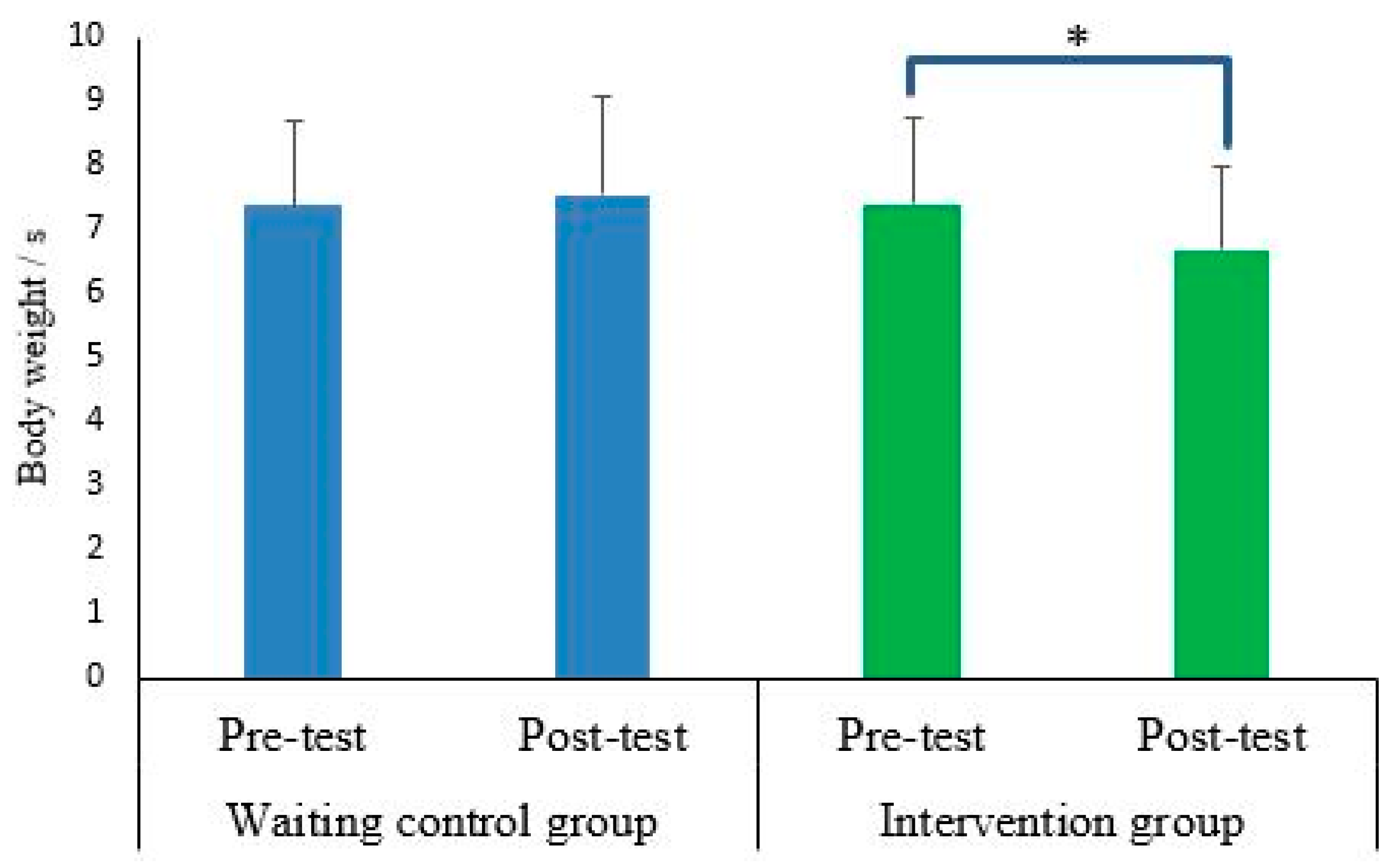
Findings demonstrated significant main effects of “time” for peak negative free moment amplitudes (p < 0.034; d = 0.56–0.58) (Table 3). In addition, significant group-by-time interactions were found for the loading rate (p = 0.037; d = 0.56) (Figure 3). In the intervention but not the control group, a significantly lower loading rate (p = 0.003; d = 0.51) was observed at post test.
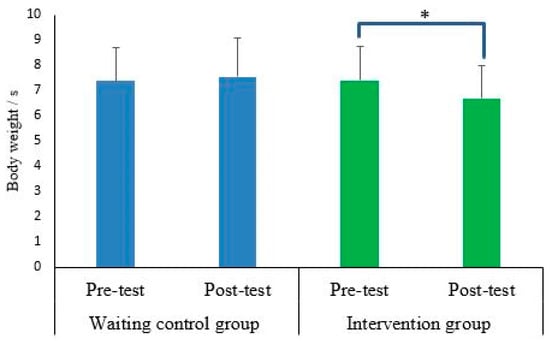
Figure 3.
Group-specific pre-post data for loading rate (body weight/s) during walking at constant speed. Descriptive data are illustrated as means (SD). Asterisk denotes statistical significance (e.g., * p < 0.05).
With regards to electromyographic activity, results showed significant main effects of “time” for tibialis anterior and vastus lateralis activities during the loading phase (p < 0.049; d = 0.52–0.53) (Table 4). Moreover, significant group-by-time interactions were observed for the vastus lateralis during the loading phase (p < 0.019; d = 0.63) (Table 4). Training-induced increases in vastus lateralis activity were found in the intervention but not in the control group (p = 0.004; d = 0.67).

Table 4.
Group-specific pre-post data for muscle activities during the loading phase expressed in % of the maximum isometric voluntary contraction (MVIC). Descriptive data are illustrated as means (SD) and 95% confidence intervals.
4. Discussion
This study aimed to examine the effects of exercising on sand versus control on GRFs and muscle activities during walking on stable ground in individuals with PF.
The main results of the present study were that (i) exercising on sand resulted in significant reductions in the first peak of vertical and lateral GRFs at the heel contact along with reduced loading rates; (ii) exercising on sand induced significant increases in vastus lateralis activities at the loading phase of walking in individuals with PF.
4.1. Effects on Walking Kinetics
Our findings on the effects of exercise on sand on walking biomechanics in individuals with PF are in agreement with the literature [40,41]. Since there is not any other study that evaluated the effects of exercise on sand on walking mechanics in adult males with PF, we decided to discuss our results in the context of studies that evaluated the effects of running exercise on walking or running biomechanics in different cohorts (e.g., healthy recreational runners [41]). For instance, a recent study reported that a six weeks exercise program (simulated barefoot running) with three sessions per week resulted in significant decreases in loading rates and impact forces in healthy adult female runners [40]. In another study, we evaluated the acute effects of running on sand vs. stable ground and not the long-term (chronic) training effects of running on sand as performed in this study [42].
In this study, running exercise on sand induced significant reductions in the first peak of vertical and lateral GRFs during heel contact, along with reduced loading rates. There is evidence that barefoot activity, particularly if conducted on unstable surfaces (i.e., sand), stimulates plantar cutaneous mechanoreceptors [43]. The enhanced afferent input may result in better pronation control and could ultimately lead to a reduction in GRFs [44]. This, however, is speculative and needs to be verified in future studies. Nevertheless, peak vertical impact GRFs and high loading rates have proven to be predictors for lower limb injuries [10]. For instance, higher loading rates and impact force values may be related to orthopedic injuries such as stress fractures [10]. Our results demonstrated that exercise on sand has the potential to lower peak impact vertical GRFs and loading rates during walking on stable ground in active male adults with PF. Therefore, the applied exercise program could have an injury preventive effect. Future studies should examine whether regular exercise on sand really reduces injury occurrence.
Besides peak vertical GRFs, medio-lateral GRFs may also contribute to injuries of the knee and hip joints [45]. A previous cross-sectional study has demonstrated that walking on sand compared with stable ground walking resulted in larger medio-lateral GRFs in healthy adult males [46]. Of note, Jafarnezhadgero and colleagues [22] could not show surface-related effects (sand vs. stable ground) while walking on peak medio-lateral GRFs in healthy controls and individuals with PF. In contrast, our results demonstrated that exercise on sand reduced peak lateral GRFs. The contrast between our findings compared with Jafarnezhadgero and colleagues [22] may be due to different study designs (cross-sectional study vs. longitudinal study) used in these two studies.
4.2. Effects on Muscle Activities during Walking
Our results did not demonstrate exercise-induced changes in tibialis anterior activity at the mid-stance phase of gait. It has been demonstrated that long-term training on sand did not change tibialis anterior activity at the mid-stance phase of running [25]. A previous study has shown that tibialis anterior muscle activity during loading but not during the mid-stance phase was higher in PF individuals compared with healthy ones [47,48]. This study was able to detect exercise-induced increases in vastus lateralis activity at the loading phase. Higher vastus lateralis and vastus medialis muscle activities in healthy individuals than that PF individuals during drop landing were reported in the literature [49]. Accordingly, Chang et al. [49] recommended that knee extensor muscle activation should be realized during the rehabilitation of PF individuals [49]. When taking our findings and the results of Chang [49] into consideration, it can be hypothesized that exercise on sand may have enabled participants to walk more efficiently. A recent cross-sectional study could not find any surface-related effects (sand vs. stable ground) on selected lower limb muscle activities at the loading phase in both healthy adults and individuals with PF [22]. PF is characterized by an excessive inward rotation of the foot that continues through the leg in distal-proximal sequence and ultimately results in lower limb malalignment [22]. The abnormal inward rotation of the leg may specifically affect the knee joint in as much as there is stress on the lateral facet of the patella [50]. There is evidence that PF can develop through leg length asymmetries [50]. More specifically, foot pronation can lower the ankle joint axis and may thus reduce the lower limb length slightly. Lowered arches are frequently seen in PF individuals and may put pressure on the plantar ligaments and the plantar aponeurosis (plantar fascia) [50]. If these structures are stressed over longer periods of time, micro tears, pain, and inflammation may accrue [50,51,52]. The observed training-induced increase in vastus lateralis activity could contribute to lowering the risk of injury in PF individuals by reducing the excessive inward rotation of the leg in PF individuals.
4.3. Strengths and Limitations
This study has some strengths and limitations that should be discussed. In terms of strengths, exercising on sand is easy to administer in many countries globally, and it is a low-cost intervention. Accordingly, large proportions of the respective populations should have access to this type of exercise. Besides its therapeutic use, exercising on sand may also contribute to fighting the pandemic of physical inactivity and sedentarism because exercising on sand is a joyful, safe (no injuries were reported in this and other studies), and effective exercise type. With regards to the study limitations, the intervention group performed the exercise training on sand while the waiting control group did not perform any additional exercise during the intervention period. It would be interesting to contrast the intervention group with an active control group performing the same exercises on stable ground in future studies. In addition, we tested young, physically active men only. Therefore, our findings are specific to this cohort and cannot necessarily be transferred to females or different age or patient groups. More research is needed in this area with different age or patient groups. In this study, we did not record kinematic data. This should be realized in future research combining kinematic, kinetic, and electromyographic data to elucidate effects and the underlying physiological mechanisms following exercising on sand. It would be worthwhile to record additional muscles such as the peroneus longus. Overall, the results of this study are useful for therapists and medical staff in general who work with PF individuals.
5. Conclusions
This intervention study examined the effects of 8 weeks of exercising on sand on walking kinetics and muscle activities in male individuals with PF. We found lower impact vertical and lateral peak forces and increased lower limb muscle activity (e.g., vastus lateralis) after training. Accordingly, we recommend implementing running exercises on sand as an effective treatment for individuals with PF. Further research is needed to verify whether this exercise program has the potential to reduce injury occurrence.
Author Contributions
Conceptualization, A.A.J. and U.G.; methodology, A.F.; formal analysis, A.A.J.; investigation, A.F.; resources, U.G.; data curation, A.F.; writing—original draft preparation, A.A.J. and A.F.; writing—review and editing, U.G.; supervision, A.A.J. and U.G.; project administration, A.A.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol was approved by the local ethics committee of the Ardabil Medical Sciences University (IR.ARUMS.REC.1398.484) and registered by the Iranian clinical trial organization (IRCT20191211045704N1). The study was conducted in agreement with the latest version of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be available at request.
Acknowledgments
We gratefully thank all participants for having volunteered to participate in this study.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
CONSORT 2010 checklist.
Table A1.
CONSORT 2010 checklist.
| Section/Topic | Item No | Checklist Item | Reported on Page No |
|---|---|---|---|
| Title and abstract | |||
| 1a | Identification as a randomized trial in the title | P1 | |
| 1b | Structured summary of trial design, methods, results, and conclusions (for specific guidance see CONSORT for abstracts) | P1-2 | |
| Introduction | |||
| Background and objectives | 2a | Scientific background and explanation of rationale | P3-5 |
| 2b | Specific objectives or hypotheses | P5 | |
| Methods | |||
| Trial design | 3a | Description of trial design (such as parallel, factorial) including allocation ratio | P5-6 |
| 3b | Important changes to methods after trial commencement (such as eligibility criteria), with reasons | P6 | |
| Participants | 4a | Eligibility criteria for participants | P6-7 |
| 4b | Settings and locations where the data were collected | P5 | |
| Interventions | 5 | The interventions for each group with sufficient details to allow replication, including how and when they were actually administered | P5-6 |
| Outcomes | 6a | Completely defined pre-specified primary and secondary outcome measures, including how and when they were assessed | P7-9 |
| 6b | Any changes to trial outcomes after the trial commenced, with reasons | P5-6 | |
| Sample size | 7a | How sample size was determined | P5-6 |
| 7b | When applicable, explanation of any interim analyses and stopping guidelines | P5-6 | |
| Randomization: | |||
| Sequence generation | 8a | Method used to generate the random allocation sequence | P5-6 |
| 8b | Type of randomization; details of any restriction (such as blocking and block size) | P5 | |
| Allocation concealment mechanism | 9 | Mechanism used to implement the random allocation sequence (such as sequentially numbered containers), describing any steps taken to conceal the sequence until interventions were assigned | P5-6 |
| Implementation | 10 | Who generated the random allocation sequence, who enrolled participants, and who assigned participants to interventions | P5-6 |
| Blinding | 11a | If done, who was blinded after assignment to interventions (for example, participants, care providers, those assessing outcomes) and how | P5-6 |
| 11b | If relevant, description of the similarity of interventions | P7-10 | |
| Statistical methods | 12a | Statistical methods used to compare groups for primary and secondary outcomes | P10 |
| 12b | Methods for additional analyses, such as subgroup analyses and adjusted analyses | NA | |
| Results | |||
| Participant flow (a diagram is strongly recommended) | 13a | For each group, the numbers of participants who were randomly assigned, received intended treatment, and were analyzed for the primary outcome | P7 |
| 13b | For each group, losses and exclusions after randomization, together with reasons | P7 | |
| Recruitment | 14a | Dates defining the periods of recruitment and follow-up | P6-8 |
| 14b | Why the trial ended or was stopped | P6-9 | |
| Baseline data | 15 | A table showing baseline demographic and clinical characteristics for each group | P11 |
| Numbers analyzed | 16 | For each group, number of participants (denominator) included in each analysis and whether the analysis was by original assigned groups | P11 |
| Outcomes and estimation | 17a | For each primary and secondary outcome, results for each group, and the estimated effect size and its precision (such as 95% confidence interval) | P11-12 |
| 17b | For binary outcomes, presentation of both absolute and relative effect sizes is recommended | P11-12 | |
| Ancillary analyses | 18 | Results of any other analyses performed, including subgroup analyses and adjusted analyses, distinguishing pre-specified from exploratory | NA |
| Harms | 19 | All important harms or unintended effects in each group (for specific guidance, see CONSORT for harms) | P11 |
| Discussion | |||
| Limitations | 20 | Trial limitations, addressing sources of potential bias, imprecision, and, if relevant, multiplicity of analyses | P15 |
| Generalisability | 21 | Generalisability (external validity, applicability) of the trial findings | P13-15 |
| Interpretation | 22 | Interpretation consistent with results, balancing benefits and harms, and considering other relevant evidence | P13-15 |
| Other information | |||
| Registration | 23 | Registration number and name of trial registry | P6 |
| Protocol | 24 | Where the full trial protocol can be accessed, if available | P6 |
| Funding | 25 | Sources of funding and other support (such as supply of drugs), role of funders | P16 |
Appendix B

Table A2.
Description of the maximum voluntary isometric contraction (MVIC) tests for the tibialis anterior (TA), the gastrocnemius medialis (Gas-M), the biceps femoris (BF), the semitendinosus (ST), the vastus lateralis (VL), the vastus medialis (VM), the rectus femoris (RF), and the gluteus medius (Glut-M) muscle.
Table A2.
Description of the maximum voluntary isometric contraction (MVIC) tests for the tibialis anterior (TA), the gastrocnemius medialis (Gas-M), the biceps femoris (BF), the semitendinosus (ST), the vastus lateralis (VL), the vastus medialis (VM), the rectus femoris (RF), and the gluteus medius (Glut-M) muscle.
| Muscles | Test Protocol |
|---|---|
| TA | In seated position on a chair with back rest, with 90° hip, knee, and ankle joint flexion. Participants were asked to activate TA at maximal effort against resistance. |
| Gas-M | In seated position on the examination table with the hip flexed by 90° and the knee and ankle in neutral position. Participants activated their plantar flexors at maximal effort against resistance. |
| BF | In seated position on a chair with hip and knees flexed at 90°. Participants activated the hamstring muscles at maximal effort against resistance. |
| ST | In seating position on a chair with hip and knees flexed at 90°. Participants maximally activated their knee flexors against resistance. |
| VL | In seated position on a chair with hip and knees flexed at 90°. Participant maximally activated their knee extensors against resistance. |
| VM | In seated position on a chair with hip and knees flexed at 90°. Participants maximally activated their knee extensors against resistance. |
| RF | In seated position on a chair with hip and knees flexed at 90°. Participants maximally activated their knee extensors against resistance. |
| Glut-M | In standing position, participants maximally activated their hip abductors against resistance. |
References
- Kothari, A.; Dixon, P.; Stebbins, J.; Zavatsky, A.; Theologis, T. Are flexible flat feet associated with proximal joint problems in children? Gait Posture 2016, 45, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Muscolino, J.E. Kinesiology-E-Book: The Skeletal System and Muscle Function; Elsevier Health Sciences: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Resende, R.A.; Deluzio, K.J.; Kirkwood, R.N.; Hassan, E.A.; Fonseca, S.T. Increased unilateral foot pronation affects lower limbs and pelvic biomechanics during walking. Gait Posture 2015, 41, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-C.; Tung, L.-C.; Tung, C.-H.; Yeh, C.-J.; Yang, J.-F.; Wang, C.-H. An investigation of the factors affecting flatfoot in children with delayed motor development. Res. Dev. Disabil. 2014, 35, 639–645. [Google Scholar] [CrossRef]
- Dunn, J.; Link, C.; Felson, D.; Crincoli, M.; Keysor, J.; McKinlay, J. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am. J. Epidemiol. 2004, 159, 491–498. [Google Scholar] [CrossRef]
- Kosashvili, Y.; Fridman, T.; Backstein, D.; Safir, O.; Ziv, Y.B. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008, 29, 910–913. [Google Scholar] [CrossRef] [PubMed]
- Carroll, N. The Pediatric Foot: Principles of Orthopedic Practice; McGraw-Hill: Montréal, QC, Canada, 1997; pp. 820–823. [Google Scholar]
- Farahpour, N.; Jafarnezhad, A.; Damavandi, M.; Bakhtiari, A.; Allard, P. Gait ground reaction force characteristics of low back pain patients with pronated foot and able-bodied individuals with and without foot pronation. J. Biomech. 2016, 49, 1705–1710. [Google Scholar] [CrossRef]
- Yazdani, F.; Razeghi, M.; Ebrahimi, S. A comparison of the free moment pattern between normal and hyper-pronated aligned feet in female subjects during the stance phase of gait. J. Biomed. Phys. Eng. 2020, 10, 93. [Google Scholar] [CrossRef]
- Zadpoor, A.A.; Nikooyan, A.A. The relationship between lower-extremity stress fractures and the ground reaction force: A systematic review. Clin. Biomech. 2011, 26, 23–28. [Google Scholar] [CrossRef]
- Hennig, E.; Milani, T. Pressure distribution measurements for evaluation of running shoe properties. Sportverletz. Sportschaden 2000, 14, 90–97. [Google Scholar] [CrossRef]
- Hornestam, J.F.; Souza, T.R.; Arantes, P.; Ocarino, J.; Silva, P.L. The effect of walking speed on foot kinematics is modified when increased pronation is induced. J. Am. Podiatr. Med. Assoc. 2016, 106, 419–426. [Google Scholar] [CrossRef]
- de Oliveira, V.M.; Detoni, G.C.; Ferreira, C.; Portela, B.S.; Queiroga, M.R.; Tartaruga, M.P. Influência do gradiente de inclinação na pronação subtalar em corrida submáxima. Acta Ortopédica Bras. 2013, 21, 163–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milner, C.E.; Davis, I.S.; Hamill, J. Free moment as a predictor of tibial stress fracture in distance runners. J. Biomech. 2006, 39, 2819–2825. [Google Scholar] [CrossRef] [PubMed]
- Ohkawa, T.; Atomi, T.; Hasegawa, K.; Atomi, Y. The free moment is associated with torsion between the pelvis and the foot during gait. Gait Posture 2017, 58, 415–420. [Google Scholar] [CrossRef]
- Murley, G.S.; Landorf, K.B.; Menz, H.B.; Bird, A.R. Effect of foot posture, foot orthoses and footwear on lower limb muscle activity during walking and running: A systematic review. Gait Posture 2009, 29, 172–187. [Google Scholar] [CrossRef] [PubMed]
- Willems, T.; Witvrouw, E.; De Cock, A.; De Clercq, D. Gait-related risk factors for exercise-related lower-leg pain during shod running. Med. Sci. Sports Exerc. 2007, 39, 330–339. [Google Scholar] [CrossRef]
- Neal, B.S.; Griffiths, I.B.; Dowling, G.J.; Murley, G.S.; Munteanu, S.E.; Smith, M.M.F.; Collins, N.J.; Barton, C.J. Foot posture as a risk factor for lower limb overuse injury: A systematic review and meta-analysis. J. Foot Ankle Res. 2014, 7, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Dowling, G.J.; Murley, G.S.; E Munteanu, S.; Smith, M.M.F.; Neal, B.S.; Griffiths, I.B.; Barton, C.J.; Collins, N.J. Dynamic foot function as a risk factor for lower limb overuse injury: A systematic review. J. Foot Ankle Res. 2014, 7, 53. [Google Scholar] [CrossRef] [Green Version]
- Mousavi, S.H.; Hijmans, J.M.; Rajabi, R.; Diercks, R.; Zwerver, J.; van der Worp, H. Kinematic risk factors for lower limb tendinopathy in distance runners: A systematic review and meta-analysis. Gait Posture 2019, 69, 13–24. [Google Scholar] [CrossRef] [Green Version]
- van den Berg, M.E.; Barr, C.J.; McLoughlin, J.V.; Crotty, M. Effect of walking on sand on gait kinematics in individuals with multiple sclerosis. Mult. Scler. Relat. Disord. 2017, 16, 15–21. [Google Scholar] [CrossRef]
- Jafarnezhadgero, A.; Fatollahi, A.; Amirzadeh, N.; Siahkouhian, M.; Granacher, U. Ground reaction forces and muscle activity while walking on sand versus stable ground in individuals with pronated feet compared with healthy controls. PLoS ONE 2019, 14, e0223219. [Google Scholar] [CrossRef] [Green Version]
- Zamparo, P.; Perini, R.; Orizio, C.; Sacher, M.; Ferretti, G. The energy cost of walking or running on sand. Eur. J. Appl. Physiol. Occup. Physiol. 1992, 65, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Binnie, M.J.; Dawson, B.; Pinnington, H.; Landers, G.; Peeling, P. Sand training: A review of current research and practical applications. J. Sports Sci. 2014, 32, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Jafarnezhadgero, A.; Fatollahi, A.; Sheykholeslami, A.; Dionisio, V.C.; Akrami, M. Long-term training on sand changes lower limb muscle activities during running in runners with over-pronated feet. BioMed. Eng. OnLine 2021, 20, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, G.; Ivanenko, Y.P.; Poppele, R.E.; Lacquaniti, F. Motor patterns in human walking and running. J. Neurophysiol. 2006, 95, 3426–3437. [Google Scholar] [CrossRef] [Green Version]
- Farris, D.J.; Sawicki, G.S. The mechanics and energetics of human walking and running: A joint level perspective. J. R. Soc. Interface 2012, 9, 110–118. [Google Scholar] [CrossRef] [Green Version]
- Biewener, A.A.; Farley, C.T.; Roberts, T.J.; Temaner, M. Muscle mechanical advantage of human walking and running: Implications for energy cost. J. Appl. Physiol. 2004, 97, 2266–2274. [Google Scholar] [CrossRef] [Green Version]
- Jafarnezhadgero, A.A.; Shad, M.M.; Majlesi, M. Effect of foot orthoses on the medial longitudinal arch in children with flexible flatfoot deformity: A three-dimensional moment analysis. Gait Posture 2017, 55, 75–80. [Google Scholar] [CrossRef]
- Jakobsen, M.D.; Sundstrup, E.; Andersen, C.H.; Bandholm, T.; Thorborg, K.; Zebis, M.K.; Andersen, L.L. Muscle activity during knee-extension strengthening exercise performed with elastic tubing and isotonic resistance. Int. J. Sports Phys. Ther. 2012, 7, 606. [Google Scholar]
- Hunt, A.E.; Fahey, A.J.; Smith, R.M. Static measures of calcaneal deviation and arch angle as predictors of rearfoot motion during walking. Aust. J. Physiother. 2000, 46, 9–16. [Google Scholar] [CrossRef]
- Cote, K.P.; Brunet, M.E., II; Gansneder, B.M.; Shultz, S.J. Effects of pronated and supinated foot postures on static and dynamic postural stability. J. Athl. Train. 2005, 40, 41. [Google Scholar]
- Gijon-Nogueron, G.; Sanchez-Rodriguez, R.; Lopezosa-Reca, E.; Cervera-Marin, J.A.; Martinez-Quintana, R.; Martinez-Nova, A. Normal values of the Foot Posture Index in a young adult Spanish population: A cross-sectional study. J. Am. Podiatr. Med. Assoc. 2015, 105, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Redmond, A.C.; Crosbie, J.; Ouvrier, R.A. Development and validation of a novel rating system for scoring standing foot posture: The Foot Posture Index. Clin. Biomech. 2006, 21, 89–98. [Google Scholar] [CrossRef] [PubMed]
- Farahpour, N.; Jafarnezhadgero, A.; Allard, P.; Majlesi, M. Muscle activity and kinetics of lower limbs during walking in pronated feet individuals with and without low back pain. J. Electromyogr. Kinesiol. 2018, 39, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Hermens, H.J.; Freriks, B.; Merletti, R.; Stegeman, D.; Blok, J.; Rau, G.; Disselhorst-Klug, C.; Hägg, G. European recommendations for surface electromyography. Roessingh Res. Dev. 1999, 8, 13–54. [Google Scholar]
- Besomi, M.; Hodges, P.W.; Clancy, E.A.; Van Dieën, J.; Hug, F.; Lowery, M.; Merletti, R.; Søgaard, K.; Wrigley, T.; Besier, T.; et al. Consensus for experimental design in electromyography (CEDE) project: Amplitude normalization matrix. J. Electromyogr. Kinesiol. 2020, 53, 102438. [Google Scholar] [CrossRef] [PubMed]
- Durai, D.B.J.; Shaju, M.F. Effect of sand running training on speed among school boys. Int. J. Phys. Educ. Sports Health 2019, 6, 117–122. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Oxfordshire, UK, 2013. [Google Scholar]
- Khowailed, I.A.; Petrofsky, J.; Lohman, E.; Daher, N. Six weeks habituation of simulated barefoot running induces neuromuscular adaptations and changes in foot strike patterns in female runners. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2015, 21, 2021. [Google Scholar]
- Dunn, M.D.; Claxton, D.B.; Fletcher, G.; Wheat, J.S.; Binney, D.M. Effects of running retraining on biomechanical factors associated with lower limb injury. Hum. Mov. Sci. 2018, 58, 21–31. [Google Scholar] [CrossRef] [Green Version]
- Jafarnezhadgero, A.; Amirzadeh, N.; Fatollahi, A.; Siahkouhian, M.; Oliveira, A.S.; Granacher, U. Effects of Running on Sand vs. Stable Ground on Kinetics and Muscle Activities in Individuals with Over-Pronated Feet. Front. Physiol. 2022, 12, 2496. [Google Scholar] [CrossRef]
- Kavounoudias, A.; Roll, R.; Roll, J.-P. The plantar sole is a ‘dynamometric map’ for human balance control. Neuroreport 1998, 9, 3247–3252. [Google Scholar] [CrossRef] [Green Version]
- Rowlands, C.; Plumb, M.S. The effects of a 4-week barefoot exercise intervention on plantar pressure, impact, balance and pain in injured recreational runners: A pilot study. Int. J. Osteopath. Med. 2019, 33, 1–7. [Google Scholar] [CrossRef]
- Sculco, T.P.; Martucci, E.A. Knee Arthroplasty; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2002. [Google Scholar]
- Yoo, B. The Effect of Carrying a Military Backpack on a Transverse Slope and Sand Surface on Lower Limb during Gait; The University of Utah: Salt Lake City, UT, USA, 2014. [Google Scholar]
- Murley, G.S.; Menz, H.B.; Landorf, K.B. Foot posture influences the electromyographic activity of selected lower limb muscles during gait. J. Foot Ankle Res. 2009, 2, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khodaveisi, H.; Sadeghi, H.; Memar, R.; Anbarian, M. Comparison of selected muscular activity of trunk and lower extremities in young women’s walking on supinated, pronated and normal foot. Apunt. Med. L’esport 2016, 51, 13–19. [Google Scholar] [CrossRef] [Green Version]
- Chang, J.S. Comparisons of vastus medialis and vastus lateralis muscle activities according to different heights during drop landing in flatfooted adults. J. Korean Phys. Ther. 2020, 32, 302–306. [Google Scholar] [CrossRef]
- Letafatkar, A.; Zandi, S.; Khodayi, M.; Vashmesara, J.B. Flat foot deformity, Q angle and knee pain are Interrelated in Wrestlers. J. Nov. Physiother. 2013, 3, 138. [Google Scholar] [CrossRef]
- Fourchet, F.; Horobeanu, C.; Loepelt, H.; Taiar, R.; Millet, G. Foot, ankle, and lower leg injuries in young male track and field athletes. Int. J. Athl. Ther. Train. 2011, 16, 19–23. [Google Scholar]
- Fourchet, F.; Kelly, L.; Horobeanu, C.; Loepelt, H.; Taiar, R.; Millet, G.P. Comparison of plantar pressure distribution in adolescent runners at low vs. high running velocity. Gait Posture 2012, 35, 685–687. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).