Effects of Cycling on Spine: A Case–Control Study Using a 3D Scanning Method
Abstract
:1. Introduction
2. Materials and Methods
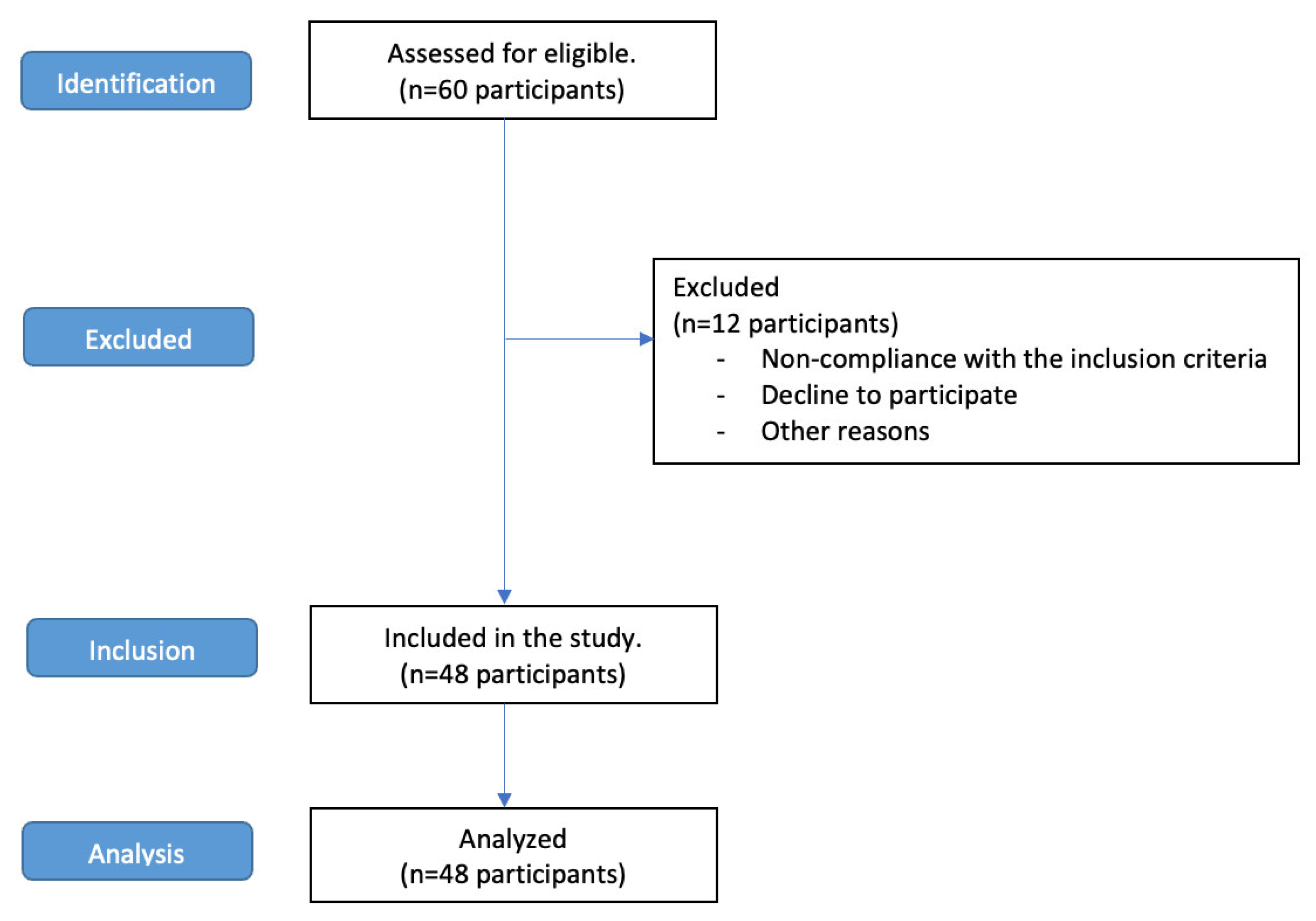
2.1. Study Design and Procedure
2.2. Participants
2.3. Instrument
2.4. Reliability of the Instrument
2.5. Parameters of the Instrument
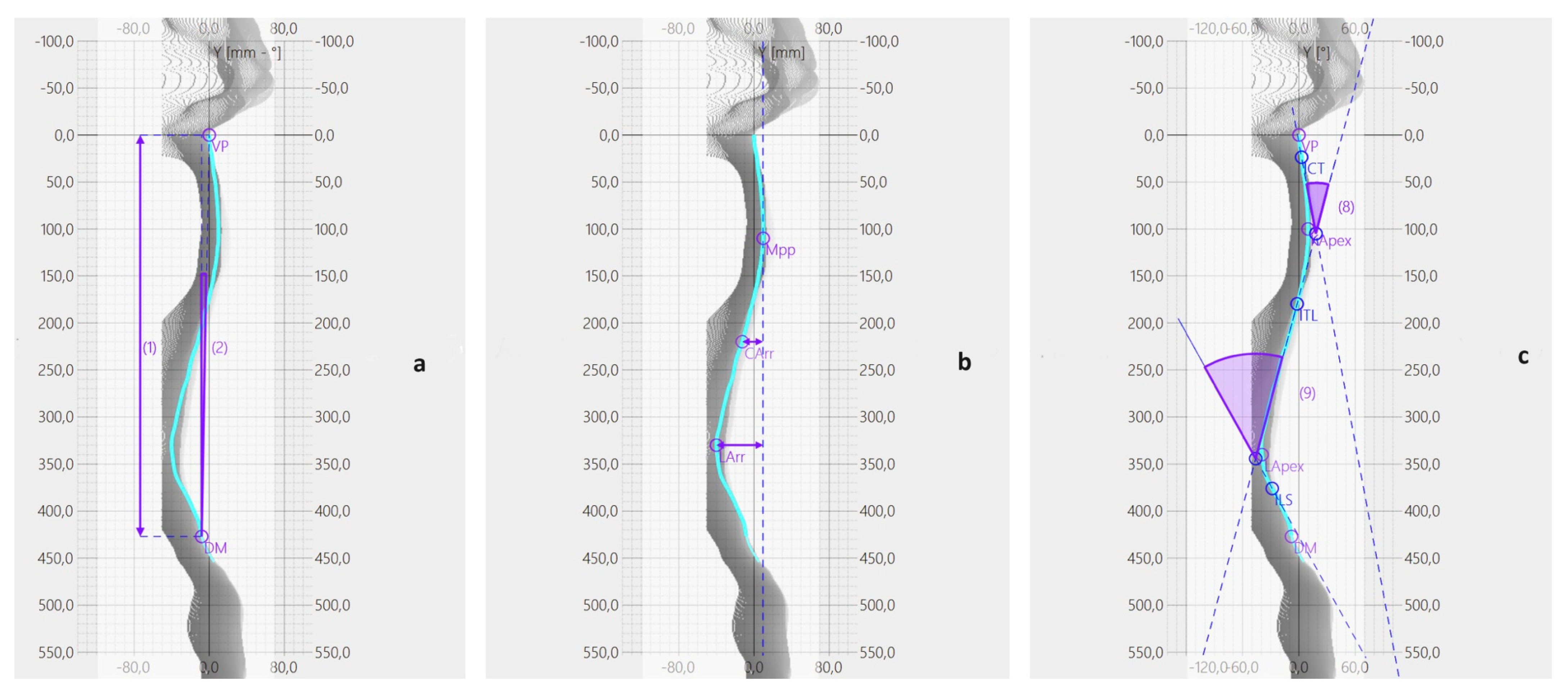
- Spine Length (Figure 3a): this is the length of the perpendicular segment from the VP to DM.
- Spine Inclination (Figure 3a): this measures the angle between the line passing through the VP and DM and the line perpendicular to the transversal plane passing through the DM.
- Cervical Lordosis (Figure 3b): this parameter represents the distance between VP and the tangent to the kyphotic apex, perpendicular to the transversal plane.
- Lumbar Lordosis (Figure 3b): this quantifies the distance between the lumbar apex and the tangent to the kyphotic apex, perpendicular to the transversal plane.
- Kyphotic Angle (Figure 3c): this angle is formed by the tangents to the surface at the cervico-thoracic inversion (ICT) and the thoraco-lumbar inversion (ITL) points.
- Lordotic Angle (Figure 3c): this angle is formed by the tangents to the surface at ITL and the lumbosacral inversion (ILS) points.
- Coronal Imbalance (Figure 4a): this is the distance between the line perpendicular to the transversal plane passing through the VP and the line perpendicular to the transversal plane passing through the DM.
- Spine Imbalance (Figure 4b): This measures the angle between the line passing through the VP and DM and the line perpendicular to the transversal plane passing through the DM. The instrument evaluates the degrees of inclination, which are positive (indicating an inclination to the right) or negative (indicating an inclination to the left).
- Shoulder Obliquity (Figure 4a): this parameter quantifies the distance between the line parallel to the transverse plane passing through the SL and the line parallel to the transverse plane passing through the SR.
- Shoulder Inclination (Figure 4b): this calculates the angle between the line parallel to the transverse plane passing through the SL and the line passing through the SL and SR.
- Pelvic Obliquity (Figure 4a): this represents the distance between the line parallel to the transverse plane passing through the DL and the line parallel to the transverse plane passing through the DR.
- Pelvic Inclination (Figure 4b): this measures the angle between the line parallel to the transverse plane passing through the DL and the line passing through the DL and DR.
2.6. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fitzgibbon, S.; Vicenzino, B.; Sisto, S. Intervention at the foot-shoe-pedal interface in competitive cyclists. Int. J. Sports Phys. Ther. 2016, 11, 637–650. [Google Scholar] [PubMed]
- Too, D. Biomechanics of cycling and factors affecting performance. Sports Med. 1990, 10, 286–302. [Google Scholar] [CrossRef] [PubMed]
- Giustino, V.; Zangla, D.; Messina, G.; Pajaujiene, S.; Feka, K.; Battaglia, G.; Bianco, A.; Palma, A.; Patti, A. Kinematics of Cervical Spine during Rowing Ergometer at Different Stroke Rates in Young Rowers: A Pilot Study. Int. J. Environ. Res. Public. Health 2022, 19, 6790. [Google Scholar] [CrossRef] [PubMed]
- Wojtys, E.; Ashton-Miller, J.; Huston, L.; Moga, P. The Association between Athletic Training Time and the Sagittal Curvature of the Immature Spine. Am. J. Sports Med. 2000, 28, 490–498. [Google Scholar] [CrossRef]
- Chavarrias, M.; Carlos-Vivas, J.; Collado-Mateo, D.; Perez-Gomez, J. Health Benefits of Indoor Cycling: A Systematic Review. Medicina 2019, 55, 452. [Google Scholar] [CrossRef] [PubMed]
- Bourne, J.E.; Sauchelli, S.; Perry, R.; Page, A.; Leary, S.; England, C.; Cooper, A.R. Health benefits of electrically-assisted cycling: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 116. [Google Scholar] [CrossRef] [PubMed]
- Oja, P.; Titze, S.; Bauman, A.; de Geus, B.; Krenn, P.; Reger-Nash, B.; Kohlberger, T. Health benefits of cycling: A systematic review. Scand. J. Med. Sci. Sports 2011, 21, 496–509. [Google Scholar] [CrossRef]
- de Vey Mestdagh, K. Personal perspective: In search of an optimum cycling posture. Appl. Ergon. 1998, 29, 325–334. [Google Scholar] [CrossRef]
- Antequera-Vique, J.A.; Oliva-Lozano, J.M.; Muyor, J.M. Effects of cycling on the morphology and spinal posture in professional and recreational cyclists: A systematic review. Sports Biomech. 2022, 22, 567–596. [Google Scholar] [CrossRef]
- Beach, T.A.; Parkinson, R.J.; Stothart, J.P.; Callaghan, J.P. Effects of prolonged sitting on the passive flexion stiffness of the in vivo lumbar spine. Spine J. 2005, 5, 145–154. [Google Scholar] [CrossRef]
- Muyor, J.M. The influence of handlebar-hands position on spinal posture in professional cyclists. J. Back. Musculoskelet. Rehabil. 2015, 28, 167–172. [Google Scholar] [CrossRef]
- Muyor, J.M.; Zabala, M. Road Cycling and Mountain Biking Produces Adaptations on the Spine and Hamstring Extensibility. Int. J. Sports Med. 2016, 37, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Muyor, J.; Alacid, F.; López-Miñarro, P.; Casimiro, A. Evolution of Spinal Morphology and Pelvic Tilt in Cyclists of Different Ages. A Cross Sectional Study. Int. J. Morphol. 2012, 30, 199–204. [Google Scholar] [CrossRef]
- Muyor, J.; López-Miñarro, P.; Alacid, F. Spinal Posture of Thoracic and Lumbar Spine and Pelvic Tilt in Highly Trained Cyclists. J. Sports Sci. Med. 2011, 10, 355–361. [Google Scholar] [PubMed]
- Salai, M.; Brosh, T.; Blankstein, A.; Oran, A.; Chechik, A. Effect of changing the saddle angle on the incidence of low back pain in recreational bicyclists. Br. J. Sports Med. 1999, 33, 398–400. [Google Scholar] [CrossRef] [PubMed]
- Bressel, E.; Larson, B.J. Bicycle seat designs and their effect on pelvic angle, trunk angle, and comfort. Med. Sci. Sports Exerc. 2003, 35, 327–332. [Google Scholar] [CrossRef] [PubMed]
- Wilder, D.G.; Pope, M.H.; Frymoyer, J.W. The biomechanics of lumbar disc herniation and the effect of overload and instability. J. Spinal Disord. 1988, 1, 16–32. [Google Scholar] [CrossRef]
- Nachemson, A. The load on lumbar disks in different positions of the body. Clin. Orthop. Relat. Res. 1966, 45, 107–122. [Google Scholar] [CrossRef]
- Burnett, A.F.; Cornelius, M.W.; Dankaerts, W.; O’Sullivan, P.B. Spinal kinematics and trunk muscle activity in cyclists: A comparison between healthy controls and non-specific chronic low back pain subjects-a pilot investigation. Man. Ther. 2004, 9, 211–219. [Google Scholar] [CrossRef]
- Taylor, D.C.; Dalton, J.D., Jr.; Seaber, A.V.; Garrett, W.E., Jr. Viscoelastic properties of muscle-tendon units. The biomechanical effects of stretching. Am. J. Sports Med. 1990, 18, 300–309. [Google Scholar] [CrossRef]
- Wallace, A.L.; Hollinshead, R.M.; Frank, C.B. Creep behavior of a rabbit model of ligament laxity after electrothermal shrinkage in vivo. Am. J. Sports Med. 2002, 30, 98–102. [Google Scholar] [CrossRef] [PubMed]
- Piotrowska, S.E.; Majchrzycki, M.; Rogala, P.; Mazurek-Sitarz, M. Lower extremity and spine pain in cyclists. Ann. Agric. Environ. Med. 2017, 24, 654–658. [Google Scholar] [CrossRef] [PubMed]
- Cyr, A. Cervical Spine, Upper Extremity Neuropathies, and Overuse Injuries in Cyclists. Phys. Med. Rehabil. Clin. N. Am. 2022, 33, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Raso, V.J.; Lou, E.; Hill, D.L.; Mahood, J.K.; Moreau, M.J.; Durdle, N.G. Trunk distortion in adolescent idiopathic scoliosis. J. Pediatr. Orthop. 1998, 18, 222–226. [Google Scholar] [CrossRef]
- Nash, C.L., Jr.; Gregg, E.C.; Brown, R.H.; Pillai, K. Risks of exposure to X-rays in patients undergoing long-term treatment for scoliosis. J. Bone Jt. Surg. Am. 1979, 61, 371–374. [Google Scholar] [CrossRef]
- Betsch, M.; Wild, M.; Rath, B.; Tingart, M.; Schulze, A.; Quack, V. Radiation-free diagnosis of scoliosis: An overview of the surface and spine topography. Orthopade 2015, 44, 845–851. [Google Scholar] [CrossRef]
- Betsch, M.; Wild, M.; Johnstone, B.; Jungbluth, P.; Hakimi, M.; Kuhlmann, B.; Rapp, W. Evaluation of a novel spine and surface topography system for dynamic spinal curvature analysis during gait. PLoS ONE 2013, 8, e70581. [Google Scholar] [CrossRef]
- Willner, S. Moire topography for the diagnosis and documentation of scoliosis. Acta Orthop. Scand. 1979, 50, 295–302. [Google Scholar] [CrossRef]
- Bugane, F.; Benedetti, M.G.; D’Angeli, V.; Leardini, A. Estimation of pelvis kinematics in level walking based on a single inertial sensor positioned close to the sacrum: Validation on healthy subjects with stereophotogrammetric system. Biomed. Eng. Online 2014, 13, 146. [Google Scholar] [CrossRef]
- Bruni, D.; Bragonzoni, L.; Gagliardi, M.; Bontempi, M.; Akkawi, I.; Raspugli, G.F.; Iacono, F.; Patella, S.; Marcacci, M. Roentgen stereophotogrammetric analysis: An effective tool to predict implant survival after an all-poly unicompartmental knee arthroplasty-a 10 year follow-up study. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3273–3280. [Google Scholar] [CrossRef]
- Marin, L.; Lovecchio, N.; Pedrotti, L.; Manzoni, F.; Febbi, M.; Albanese, I.; Patane, P.; Carnevale Pellino, V.; Vandoni, M. Acute Effects of Self-Correction on Spine Deviation and Balance in Adolescent Girls with Idiopathic Scoliosis. Sensors 2022, 22, 1883. [Google Scholar] [CrossRef]
- Roggio, F.; Petrigna, L.; Trovato, B.; Zanghi, M.; Sortino, M.; Vitale, E.; Rapisarda, L.; Testa, G.; Pavone, V.; Pavone, P.; et al. Thermography and rasterstereography as a combined infrared method to assess the posture of healthy individuals. Sci. Rep. 2023, 13, 4263. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Lucia, A.; Hoyos, J.; Chicharro, J.L. Physiology of professional road cycling. Sports Med. 2001, 31, 325–337. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guidetti, L.; Bonavolonta, V.; Tito, A.; Reis, V.M.; Gallotta, M.C.; Baldari, C. Intra- and interday reliability of spine rasterstereography. Biomed. Res. Int. 2013, 2013, 745480. [Google Scholar] [CrossRef]
- Rosner, B. Fundamentals of Biostatistics; Cengage Learning: Boston, MA, USA, 2015. [Google Scholar]
- Patti, A.; Maggio, M.C.; Corsello, G.; Messina, G.; Iovane, A.; Palma, A. Evaluation of Fitness and the Balance Levels of Children with a Diagnosis of Juvenile Idiopathic Arthritis: A Pilot Study. Int. J. Environ. Res. Public. Health 2017, 14, 806. [Google Scholar] [CrossRef]
- Kang, H. Sample size determination and power analysis using the G*Power software. J. Educ. Eval. Health Prof. 2021, 18, 17. [Google Scholar] [CrossRef] [PubMed]
- Bowring, A.; Telschow, F.J.E.; Schwartzman, A.; Nichols, T.E. Confidence Sets for Cohen’s d effect size images. Neuroimage 2021, 226, 117477. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, G.M.; Feinn, R. Using Effect Size-or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Chicco, D.; Warrens, M.J.; Jurman, G. The coefficient of determination R-squared is more informative than SMAPE, MAE, MAPE, MSE and RMSE in regression analysis evaluation. PeerJ Comput. Sci. 2021, 7, e623. [Google Scholar] [CrossRef]
- Streisfeld, G.M.; Bartoszek, C.; Creran, E.; Inge, B.; McShane, M.D.; Johnston, T. Relationship Between Body Positioning, Muscle Activity, and Spinal Kinematics in Cyclists With and Without Low Back Pain: A Systematic Review. Sports Health 2017, 9, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Clarsen, B.; Krosshaug, T.; Bahr, R. Overuse injuries in professional road cyclists. Am. J. Sports Med. 2010, 38, 2494–2501. [Google Scholar] [CrossRef]
- Wang, Z.; Mac-Thiong, J.M.; Parent, S.; Petit, Y.; Labelle, H. The relevance of sacral and sacro-pelvic morphology in developmental lumbosacral spondylolisthesis: Are they equally important? Eur. Spine J. 2014, 23, 157–162. [Google Scholar] [CrossRef]
- Rauter, S.; Simenko, J. Morphological Asymmetries Profile and the Difference between Low- and High-Performing Road Cyclists Using 3D Scanning. Biology 2021, 10, 1199. [Google Scholar] [CrossRef]
- Rauter, S.; Vodicar, J.; Šimenko, J. Body Asymmetries in Young Male Road Cyclists. Int. J. Morphol. 2017, 35, 907–912. [Google Scholar] [CrossRef]
- Marsden, M.; Schwellnus, M. Lower back pain in cyclists: A review of epidemiology, pathomechanics and risk factors. Int. Sportmed. J. 2010, 11, 216–225. [Google Scholar]
- Mellion, M.B. Common cycling injuries. Management and prevention. Sports Med. 1991, 11, 52–70. [Google Scholar] [CrossRef]
- Iplikcioglu, A.C.; Karabag, H. Analysis of Components of Upper Cervical Lordosis in Asymptomatic Lordotic and Kyphotic Subjects. World Neurosurg. 2023, 171, e852–e858. [Google Scholar] [CrossRef] [PubMed]
- Tan, L.A.; Riew, K.D.; Traynelis, V.C. Cervical Spine Deformity-Part 1: Biomechanics, Radiographic Parameters, and Classification. Neurosurgery 2017, 81, 197–203. [Google Scholar] [CrossRef]
- Greco, G.; Messina, G.; Angiulli, A.; Patti, A.; Iovane, A.; Fischetti, F. A preliminary comparative study on the effects of Pilates training on physical fitness of young female volleyball players. Acta Medica Mediterr. 2019, 2, 783. [Google Scholar] [CrossRef]
- Patti, A.; Thornton, J.S.; Giustino, V.; Drid, P.; Paoli, A.; Schulz, J.M.; Palma, A.; Bianco, A. Effectiveness of Pilates exercise on low back pain: A systematic review with meta-analysis. Disabil. Rehabil. 2023, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Vicari, D.S.S.; Patti, A.; Giustino, V.; Figlioli, F.; Alamia, G.; Palma, A.; Bianco, A. Saddle Pressures Factors in Road and Off-Road Cyclists of Both Genders: A Narrative Review. J. Funct. Morphol. Kinesiol. 2023, 8, 71. [Google Scholar] [CrossRef] [PubMed]
- Giustino, V.; Messina, G.; Patti, A.; Padua, E.; Zangla, D.; Drid, P.; Battaglia, G.; Palma, A.; Bianco, A. Effects of a Postural Exercise Program on Vertical Jump Height in Young Female Volleyball Players with Knee Valgus. Int. J. Environ. Res. Public. Health 2022, 19, 3953. [Google Scholar] [CrossRef]



| Spine Parameters | Cy-G (25) | CG (23) | df | p | Cohen’s d (Effect Size) | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Sagittal Plane | |||||||
| Spine Length (mm) | 450 ± 18.3 | 444 ± 45.8 | 22.0 | 0.621 | 0.1047 | −0.3063 | 0.5134 |
| Spine Inclination (°) | 5.80 ± 3.50 | 3.25 ± 2.54 | 22.0 | 0.009 | 0.5981 | 0.1475 | 1.0372 |
| Cervical Lordosis (mm) | 58.2 ± 19.1 | 46.7 ± 20.4 | 22.0 | 0.106 | 0.3518 | −0.0735 | 0.7696 |
| Lumbar Lordosis (mm) | 34 ± 12.4 | 48.3 ± 12.7 | 22.0 | 0.003 | 0.7110 | −1.1635 | −0.2456 |
| Kyphotic Angle (°) | 42.8 ± 10.0 | 42.7 ± 13.0 | 22.0 | 0.944 | 0.0148 | −0.3941 | 0.4233 |
| Lordotic Angle (°) | 36.2 ± 10.3 | 42.3 ± 16.7 | 22.0 | 0.110 | 0.3472 | −0.7647 | 0.0777 |
| Frontal Plane | |||||||
| Coronal Imbalance (mm) | 3.04 ± 10.9 | 0.73 ± 7.68 | 22.0 | 0.371 | 0.1904 | −0.2242 | 0.6008 |
| Spine Imbalance (°) | −0.40 ± 1.38 | −0.12 ± 0.986 | 22.0 | 0.413 | 0.1739 | −0.5838 | 0.2399 |
| Shoulder Obliquity (mm) | −1.36 ± 11.2 | −1.17 ± 5.31 | 22.0 | 0.832 | 0.0449 | −0.3645 | 0.4533 |
| Shoulder Inclination (°) | −4.13 ± 19.4 | −0.20 ± 1.04 | 22.0 | 0.345 | 0.2012 | −0.6119 | 0.2140 |
| Pelvic Obliquity (mm) | 0.20 ±4.20 | 0.87 ± 2.93 | 22.0 | 0.735 | 0.0716 | −0.4800 | 0.3384 |
| Pelvic Inclination (°) | 0.51 ± 2.73 | 0.55 ± 1.71 | 22.0 | 0.754 | 0.0662 | −0.3437 | 0.4746 |
| Predictor | Estimate | SE | t | p |
|---|---|---|---|---|
| Intercept | −87.027 | 16.5516 | −5.26 | <0.001 |
| Spine Length | 0.190 | 0.0389 | 4.89 | <0.001 |
| Spine Inclination | 3.458 | 0.3650 | 9.47 | <0.001 |
| Kyphotic Angle | 0.887 | 0.1163 | 7.62 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patti, A.; Giustino, V.; Messina, G.; Figlioli, F.; Cataldi, S.; Poli, L.; Belmonte, G.; Valenza, A.; Amato, A.; Thomas, E.; et al. Effects of Cycling on Spine: A Case–Control Study Using a 3D Scanning Method. Sports 2023, 11, 227. https://doi.org/10.3390/sports11110227
Patti A, Giustino V, Messina G, Figlioli F, Cataldi S, Poli L, Belmonte G, Valenza A, Amato A, Thomas E, et al. Effects of Cycling on Spine: A Case–Control Study Using a 3D Scanning Method. Sports. 2023; 11(11):227. https://doi.org/10.3390/sports11110227
Chicago/Turabian StylePatti, Antonino, Valerio Giustino, Giuseppe Messina, Flavia Figlioli, Stefania Cataldi, Luca Poli, Giacomo Belmonte, Alessandro Valenza, Alessandra Amato, Ewan Thomas, and et al. 2023. "Effects of Cycling on Spine: A Case–Control Study Using a 3D Scanning Method" Sports 11, no. 11: 227. https://doi.org/10.3390/sports11110227















