Gait Pattern, Impact to the Skeleton and Postural Balance in Overweight and Obese Children: A Review
Abstract
:1. Introduction
2. Methods
3. Gait Pattern
4. Impact/Loads to the Lower Extremities and the Lower Back
5. Postural Balance
Falling Risk
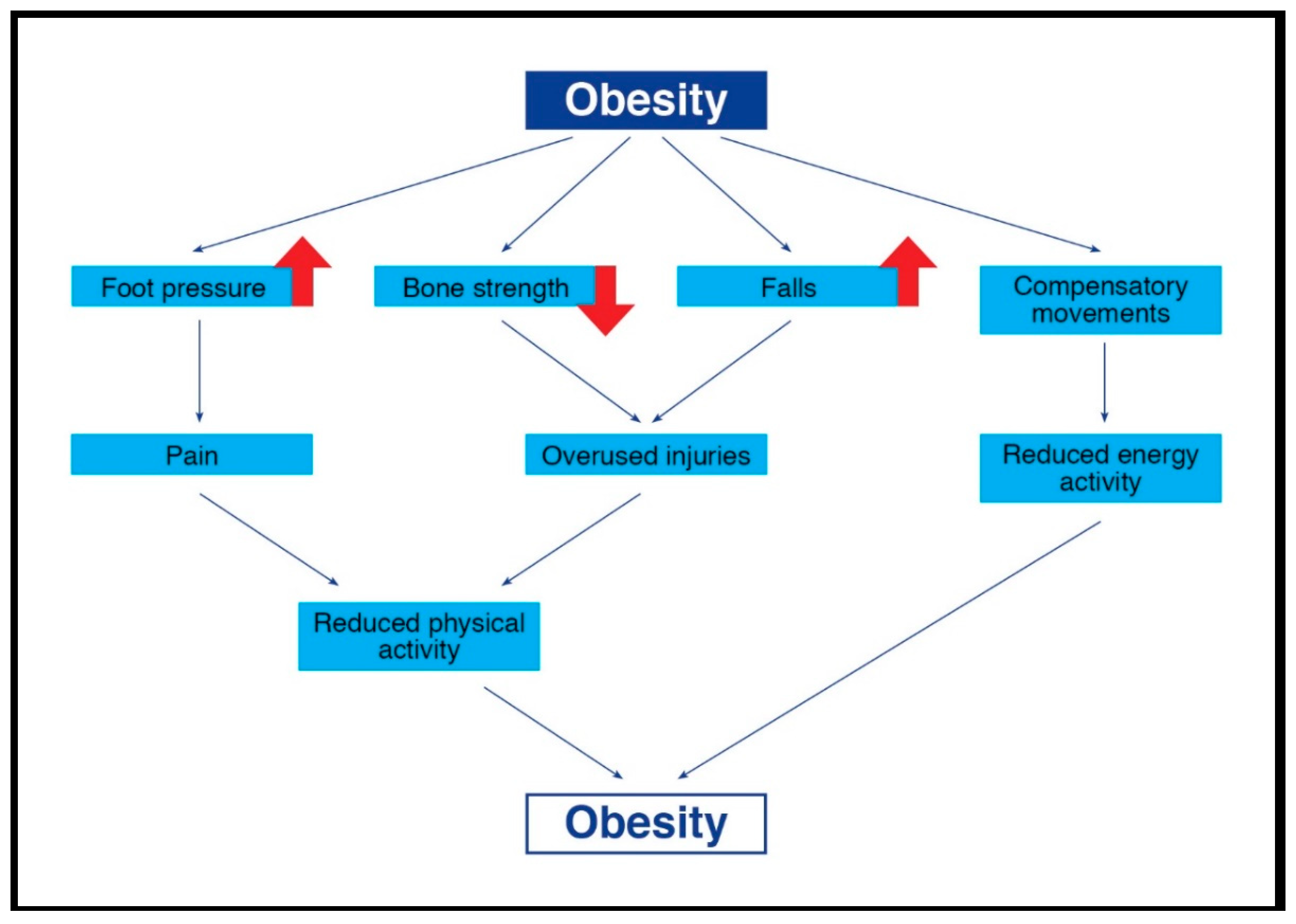
6. Malalignments and Injuries
6.1. Fractures and Other Types of Injuries
6.2. Malalignment
7. Intervention Programs
8. Conclusions and Clinical Implications
- (1)
- Gait analyses: These analyses should identify gait impairments. If such deficiencies exist, these children should participate in a specific program, such as a locomotion-emphasis program for improving biomechanical characteristics [28], prior to participation in the weight-management intervention. This program should focus mainly on improving the ankle-foot gait movements (e.g., exercises for improving ankle mobility and stability, improving postural balance, improving proprioception ability, and strengthening muscles such as the calf muscles and the extrinsic and intrinsic foot muscles).
- (2)
- Impact/loads to the lower extremities and the lower back: As increased impact/loads might increase the chance for foot malalignment and musculoskeletal injuries, interventions such as visual biofeedback gait retraining should be advised for these children. Furthermore, in order to decrease plantar pressures beneath the feet, a potential implication for innovative children’s footwear design is suggested [46,87].
- (3)
- Postural balance assessment: Safety measures to identify the overweight/obese children who suffer from postural balance deficiencies might decrease their chances of falling and of subsequent injuries during participation in physical activities. It is important that the initial phases of exercise interventions focus on balance improvement (using exercise on stable and unstable surfaces, with open and closed eyes, static and dynamic, etc.) [108].
- (4)
- Bone strength: Bone strength should be determined in order to detect overweight/obese children with reduced bone properties [85]. Children with reduced strength and increased fracture risk should start intervention programs with non-weight-bearing exercises, such as bicycle riding or swimming [37], and gradually increase the amount of weight-bearing exercises.
- (5)
- Mal-alignments and previous injuries: As mal-alignments and previous injuries may affect the overweight/obese children’s performance and increase the risk for new injuries, it is suggested that a clinical orthopedic examination should be undertaken before starting an exercise program [87]. Individualized and gradually adapted exercise program should be implemented for each child.
Funding
Conflicts of Interest
References
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar] [PubMed]
- Lerner, Z.F.; Board, W.J.; Browning, R.C. Effects of obesity on lower extremity muscle function during walking at two speeds. Gait Posture 2014, 39, 978–984. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deforche, B.I.; Hills, A.P.; Worringham, C.J.; Davies, P.S.; Murphy, A.J.; Bouckaert, J.J.; De Bourdeaudhuij, I.M. Balance and postural skills in normal-weight and overweight prepubertal boys. Int. J. Pediatr. Obes. 2009, 4, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Tsiros, M.D.; Coates, A.M.; Howe, P.R.; Grimshaw, P.N.; Walkley, J.; Shield, A.; Mallows, R.; Hills, A.P.; Kagawa, M.; Shultz, S.; et al. Knee extensor strength differences in obese and healthy-weight 10-to 13-year-olds. Eur. J. Appl. Physiol. 2013, 113, 1415–1422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shultz, S.P.; D’Hondt, E.; Lenoir, M.; Fink, P.W.; Hills, A.P. The role of excess mass in the adaptation of children’s gait. Hum. Mov. Sci. 2014, 36, 12–19. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Deforche, B.; De Bourdeaudhuij, I.; Lenoir, M. Childhood obesity affects fine motor skill performance under different postural constraints. Neurosci. Lett. 2008, 440, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Tsiros, M.D.; Coates, A.M.; Howe, P.R.; Grimshaw, P.N.; Buckley, J.D. Obesity: The new childhood disability? Obes. Rev. 2011, 12, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Adamo, K.B.; Wilson, S.; Harvey, A.L.; Grattan, K.P.; Naylor, P.J.; Temple, V.A.; Goldfield, G.S. Does intervening in childcare settings impact fundamental movement skill development? Med. Sci. Sports Exerc. 2016, 48, 926–932. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.P.; Sitler, M.R.; Tierney, R.T.; Hillstrom, H.J.; Song, J. Effects of pediatric obesity on joint kinematics and kinetics during 2 walking cadences. Arch. Phys. Med. Rehabil. 2009, 90, 2146–2154. [Google Scholar] [CrossRef] [PubMed]
- Hootman, J.M.; Macera, C.A.; Ainsworth, B.E.; Martin, M.; Addy, C.L.; Blair, S.N. Association among physical activity level, cardiorespiratory fitness, and risk of musculoskeletal injury. Am. J. Epidemiol. 2001, 154, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Huang, L. The Implications of Childhood Obesity on the Musculoskeletal and Locomotor Systems: Biomechanical Analyses and Exercise Intervention; The University of Auckland: Philadelphia, PA, USA, 2014. [Google Scholar]
- Smith, A.J.J.; Lemaire, E.D. Temporal-spatial gait parameter models of very slow walking. Gait Posture 2018, 61, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Al-Obaidi, S.; Wall, J.C.; Al-Yaqoub, A.; Al-Ghanim, M. Basic gait parameters: A comparison of reference data for normal subjects 20 to 29 years of age from Kuwait and Scandinavia. J. Rehabil. Res. Dev. 2003, 40, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Wall, J.C.; Charteris, J.; Turnbull, G.I. Two steps equals one stride equals what? The applicability of normal gait nomenclature to abnormal walking patterns. Clin. Biomech. 1987, 2, 119–125. [Google Scholar] [CrossRef]
- Loudon, J.; Swift, M.; Bell, S. The Clinical Orthopedic Assessment Guide; Human Kinetics: Kansas City, KS, USA, 2008. [Google Scholar]
- Oliveira, L.C.; Ferrari, G.L.M.; Araujo, T.L.; Matsudo, V. Overweight, obesity, steps, and moderate to vigorous physical activity in children. Rev. Saude Publica 2017, 51, 38. [Google Scholar] [CrossRef] [PubMed]
- Carlin, A.; Murphy, M.H.; Gallagher, A.M. Do interventions to increase walking work? A systematic review of interventions in children and adolescents. Sports Med. 2016, 46, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Logan, S.W.; Robinson, L.E.; Wilson, A.E.; Lucas, W.A. Getting the fundamentals of movement: A meta-analysis of the effectiveness of motor skill interventions in children. Child Care Health Dev. 2012, 38, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Dufek, J.S.; Currie, R.L.; Gouws, P.L.; Candela, L.; Gutierrez, A.P.; Mercer, J.A.; Putney, L.G. Effects of overweight and obesity on walking characteristics in adolescents. Hum. Mov. Sci. 2012, 31, 897–906. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.P.; Hennig, E.M.; Byrne, N.M.; Steele, J.R. The biomechanics of adiposity–structural and functional limitations of obesity and implications for movement. Obes. Rev. 2002, 3, 35–43. [Google Scholar] [CrossRef] [PubMed]
- McMillan, A.G.; Auman, N.L.; Collier, D.N.; Blaise Williams, D.S. Frontal plane lower extremity biomechanics during walking in boys who are overweight versus healthy weight. Pediatr. Phys. Ther. 2009, 21, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Rubinstein, M.; Nemet, D.; Ayalon, M.; Zeev, A.; Pantanowitz, M.; Brosh, T.; Eliakim, A. Effects of a program for improving biomechanical characteristics during walking and running in children who are obese. Pediatr. Phys. Ther. 2017, 29, 330–340. [Google Scholar] [CrossRef] [PubMed]
- Cimolin, V.; Galli, M. Summary measures for clinical gait analysis: A literature review. Gait Posture 2014, 39, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Chen, P.; Zhuang, J.; Walt, S. Metabolic cost, mechanical work, and efficiency during normal walking in obese and normal-weight children. Res. Q. Exerc. Sport 2013, 84, S72–S79. [Google Scholar] [CrossRef] [PubMed]
- Plummer, P.; Apple, S.; Dowd, C.; Keith, E. Texting and walking: Effect of environmental setting and task prioritization on dual-task interference in healthy young adults. Gait Posture 2015, 41, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.; Wang, L.J.; Wang, L. Effects of weight management program on postural stability and neuromuscular function among obese children: Study protocol for a randomized controlled trial. Trials 2015, 16, 143. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.P.; Parker, A.W. Gait characteristics of obese children. Arch. Phys. Med. Rehabil. 1991, 72, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Rubinstein, M.; Eliakim, A.; Steinberg, N.; Nemet, D.; Ayalon, M.; Zeev, A.; Pantanowitz, M.; Brosh, T. Biomechanical characteristics of overweight and obese children during five different walking and running velocities. Footwear Sci. 2018, in press. [Google Scholar] [CrossRef]
- Hung, Y.C.; Mangiafreno, M.; Gill, S.V. Whole body organization during a symmetric bimanual pick up task in overweight and obese children. Gait Posture 2017, 52, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.H.; Zhang, K.; Tan, G.Q.; Yang, J.; Liu, Z.C. Effects of obesity on dynamic plantar pressure distribution in Chinese prepubescent children during walking. Gait Posture 2013, 37, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Mueller, S.; Carlsohn, A.; Mueller, J.; Baur, H.; Mayer, F. Influence of obesity on foot loading characteristics in gait for children aged 1 to 12 years. PLoS ONE 2016, 11, e0149924. [Google Scholar] [CrossRef] [PubMed]
- Mickle, K.J.; Steele, J.R.; Munro, B.J. Does excess mass affect plantar pressure in young children? Int. J. Pediatr. Obes. 2006, 1, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Dowling, A.M.; Steele, J.R.; Baur, L.A. Does obesity influence foot structure and plantar pressure patterns in prepubescent children? Int. J. Obes. 2001, 25, 845–852. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colne, P.; Frelut, M.L.; Peres, G.; Thoumie, P. Postural control in obese adolescents assessed by limits of stability and gait initiation. Gait Posture 2008, 28, 164–169. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Nemet, D.; Kohen-Raz, R.; Zeev, A.; Pantanowitz, M.; Eliakim, A. Posturography characteristics of obese children with and without associated disorders. Percept. Mot. Skills 2013, 116, 564–580. [Google Scholar] [CrossRef] [PubMed]
- Goulding, A.; Jones, I.E.; Taylor, R.W.; Piggot, J.M.; Taylor, D. Dynamic and static tests of balance and postural sway in boys: Effects of previous wrist bone fractures and high adiposity. Gait Posture 2003, 17, 136–141. [Google Scholar] [CrossRef]
- Taylor, E.D.; Theim, K.R.; Mirch, M.C.; Ghorbani, S.; Tanofsky-Kraff, M.; Adler-Wailes, D.C.; Brady, S.; Reynolds, J.C.; Calis, K.A.; Yanovski, J.A. Orthopedic complications of overweight in children and adolescents. Pediatrics 2006, 117, 2167–2174. [Google Scholar] [CrossRef] [PubMed]
- Mickle, K.J.; Steele, J.R.; Munro, B.J. The feet of overweight and obese young children: Are they flat or fat? Obesity 2006, 14, 1949–1953. [Google Scholar] [CrossRef] [PubMed]
- Witt, C.E.; Arbabi, S.; Nathens, A.B.; Vavilala, M.S.; Rivara, F.P. Obesity in pediatric trauma. J. Pediatr. Surg. 2017, 52, 628–632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mastrangelo, M.A.; Chaloupka, E.C.; Rattigan, P. Cardiovascular fitness in obese versus nonobese 8-11-year-old boys and girls. Res. Q. Exerc. Sport 2008, 79, 356–362. [Google Scholar] [CrossRef] [PubMed]
- Saibene, F.; Minetti, A.E. Biomechanical and physiological aspects of legged locomotion in humans. Eur. J. Appl. Physiol. 2003, 88, 297–316. [Google Scholar] [CrossRef] [PubMed]
- Peyrot, N.; Morin, J.B.; Thivel, D.; Isacco, L.; Taillardat, M.; Belli, A.; Duche, P. Mechanical work and metabolic cost of walking after weight loss in obese adolescents. Med. Sci. Sports Exerc. 2010, 42, 1914–1922. [Google Scholar] [CrossRef] [PubMed]
- Peyrot, N.; Thivel, D.; Isacco, L.; Morin, J.B.; Duche, P.; Belli, A. Do mechanical gait parameters explain the higher metabolic cost of walking in obese adolescents? J. Appl. Physiol. 2009, 106, 1763–1770. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malatesta, D.; Vismara, L.; Menegoni, F.; Galli, M.; Romei, M.; Capodaglio, P. Mechanical external work and recovery at preferred walking speed in obese subjects. Med. Sci. Sports Exerc. 2009, 41, 426–434. [Google Scholar] [CrossRef] [PubMed]
- McMillan, A.G.; Pulver, A.M.; Collier, D.N.; Williams, D.S. Sagittal and frontal plane joint mechanics throughout the stance phase of walking in adolescents who are obese. Gait Posture 2010, 32, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Riddiford-Harland, D.L.; Steele, J.R.; Cliff, D.P.; Okely, A.D.; Morgan, P.J.; Jones, R.A.; Baur, L.A. Lower activity levels are related to higher plantar pressures in overweight children. Med. Sci. Sports Exerc. 2015, 47, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Hung, Y.C.; Gill, S.V.; Meredith, G.S. Influence of dual-task constraints on whole-body organization during walking in children who are overweight and obese. Am. J. Phys. Med. Rehabil. 2013, 92, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Crowell, D.H.; Prentice, W.E.; Onate, J.A. The effect of fatigue on postural stability and neuropsychological function (Abstract). J. Athl. Train. 2001, 36, S-33. [Google Scholar]
- Tirosh, O.; Orland, G.; Eliakim, A.; Nemet, D.; Steinberg, N. Tibial impact accelerations in gait of primary school children: The effect of age and speed. Gait Posture 2017, 57, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Browning, R.C.; Kram, R. Effects of obesity on the biomechanics of walking at different speeds. Med. Sci. Sports Exerc. 2007, 39, 1632–1641. [Google Scholar] [CrossRef] [PubMed]
- Haight, D.J.; Lerner, Z.F.; Board, W.J.; Browning, R.C. A comparison of slow, uphill and fast, level walking on lower extremity biomechanics and tibiofemoral joint loading in obese and nonobese adults. J. Orthop. Res. 2014, 32, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Dowling, A.M.; Steele, J.R.; Baur, L.A. What are the effects of obesity in children on plantar pressure distributions? Int. J. Obes. 2004, 28, 1514–1519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, Q.; Yu, B.; Zhang, C.; Sun, W.; Mao, D. Effects of backpack weight on posture, gait patterns and ground reaction forces of male children with obesity during stair descent. Res. Sports Med. 2014, 22, 172–184. [Google Scholar] [CrossRef] [PubMed]
- McGraw, B.; McClenaghan, B.A.; Williams, H.G.; Dickerson, J.; Ward, D.S. Gait and postural stability in obese and nonobese prepubertal boys. Arch. Phys. Med. Rehabil. 2000, 81, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Song-Hua, Y.; Lu, W.; Kuan, Z. Effects of different movement modes on plantar pressure distribution patterns in obese and non-obese Chinese children. Gait Posture 2017, 57, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Kim, S.; Nussbaum, M.A. Does load carriage differentially alter postural sway in overweight vs. normal-weight schoolchildren? Gait Posture 2012, 35, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Lerner, Z.F.; Browning, R.C. Compressive and shear hip joint contact forces are affected by pediatric obesity during walking. J. Biomech. 2016, 49, 1547–1553. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Franklyn-Miller, A.; Wilson, C.; Bilzon, J.; McCrory, P. Foot orthoses in the prevention of injury in initial military training: A randomized controlled trial. Am. J. Sports Med. 2011, 39, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Mickle, K.J.; Cliff, D.P.; Munro, B.J.; Okely, A.D.; Steele, J.R. Relationship between plantar pressures, physical activity and sedentariness among preschool children. J. Sci. Med. Sport 2011, 14, 36–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cousins, S.D.; Morrison, S.C.; Drechsler, W.I. Foot loading patterns in normal weight, overweight and obese children aged 7 to 11 years. J. Foot Ankle Res. 2013, 6, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pollock, A.S.; Durward, B.R.; Rowe, P.J.; Paul, J.P. What is balance? Clin. Rehabil. 2000, 14, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Hrysomallis, C. Balance ability and athletic performance. Sports Med. 2011, 41, 221–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferber-Viart, C.; Ionescu, E.; Morlet, T.; Froehlich, P.; Dubreuil, C. Balance in healthy individuals assessed with Equitest: Maturation and normative data for children and young adults. Int. J. Pediatr. Otorhinolaryngol. 2007, 71, 1041–1046. [Google Scholar] [CrossRef] [PubMed]
- Mirovsky, Y.; Blankstein, A.; Shlamkovitch, N. Postural control in patients with severe idiopathic scoliosis: A prospective study. J. Pediatr. Orthop. B 2006, 15, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Cintas, X.; Holly, M. The accomplishment of walking: Aspects of the ascent. Pediatr. Phys. Ther. 1993, 5, 61–68. [Google Scholar] [CrossRef]
- Cieslinska-Swider, J.; Furmanek, M.P.; Blaszczyk, J.W. The influence of adipose tissue location on postural control. J. Biomech. 2017, 60, 162–169. [Google Scholar] [CrossRef] [PubMed]
- Villarrasa-Sapina, I.; Serra-Ano, P.; Pardo-Ibanez, A.; Gonzalez, L.M.; Garcia-Masso, X. Relationship between body composition and vertical ground reaction forces in obese children when walking. Clin. Biomech. 2017, 41, 77–81. [Google Scholar] [CrossRef] [PubMed]
- Boucher, F.; Handrigan, G.A.; Mackrous, I.; Hue, O. Childhood obesity affects postural control and aiming performance during an upper limb movement. Gait Posture 2015, 42, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Osika, W.; Montgomery, S.M.; Longitudinal Birth Cohort, S. Physical control and coordination in childhood and adult obesity: Longitudinal Birth Cohort Study. Br. Med. J. 2008, 337, a699. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Deforche, B.; Gentier, I.; De Bourdeaudhuij, I.; Vaeyens, R.; Philippaerts, R.; Lenoir, M. A longitudinal analysis of gross motor coordination in overweight and obese children versus normal-weight peers. Int. J. Obes. 2013, 37, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Verbecque, E.; Vereeck, L.; Hallemans, A. Postural sway in children: A literature review. Gait Posture 2016, 49, 402–410. [Google Scholar] [CrossRef] [PubMed]
- D’Hondt, E.; Segers, V.; Deforche, B.; Shultz, S.P.; Tanghe, A.; Gentier, I.; De Bourdeaudhuij, I.; De Clercq, D.; Lenoir, M. The role of vision in obese and normal-weight children’s gait control. Gait Posture 2011, 33, 179–184. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Madigan, M.L. Impaired plantar sensitivity among the obese is associated with increased postural sway. Neurosci. Lett. 2014, 583, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Wills, M. Orthopedic complications of childhood obesity. Pediatr. Phys. Ther. 2004, 16, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Goulding, A.; Jones, I.E.; Taylor, R.W.; Williams, S.M.; Manning, P.J. Bone mineral density and body composition in boys with distal forearm fractures: A dual-energy x-ray absorptiometry study. J. Pediatr. 2001, 139, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Goulding, A.; Taylor, R.W.; Jones, I.E.; McAuley, K.A.; Manning, P.J.; Williams, S.M. Overweight and obese children have low bone mass and area for their weight. Int. J. Obes. 2000, 24, 627–662. [Google Scholar] [CrossRef]
- Landauer, F.; Huber, G.; Paulmichl, K.; O’Malley, G.; Mangge, H.; Weghuber, D. Timely diagnosis of malalignment of the distal extremities is crucial in morbidly obese juveniles. Obes. Facts 2013, 6, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Stovitz, S.D.; Pardee, P.E.; Vazquez, G.; Duval, S.; Schwimmer, J.B. Musculoskeletal pain in obese children and adolescents. Acta Paediatr. 2008, 97, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Sundin, B.A.; Moreno, E.; Neher, J.O.; St Anna, L. FPIN’s clinical inquiries. Obesity and joint injuries in children. Am. Fam. Phys. 2015, 91, 320–322. [Google Scholar]
- Kim, S.J.; Ahn, J.; Kim, H.K.; Kim, J.H. Obese children experience more extremity fractures than nonobese children and are significantly more likely to die from traumatic injuries. Acta Paediatr. 2016, 105, 1152–1157. [Google Scholar] [CrossRef] [PubMed]
- Leonard, M.B.; Shults, J.; Wilson, B.A.; Tershakovec, A.M.; Zemel, B.S. Obesity during childhood and adolescence augments bone mass and bone dimensions. Am. J. Clin. Nutr. 2004, 80, 514–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandewalle, S.; Taes, Y.; Van Helvoirt, M.; Debode, P.; Herregods, N.; Ernst, C.; Roef, G.; Van Caenegem, E.; Roggen, I.; Verhelle, F.; et al. Bone size and bone strength are increased in obese male adolescents. J. Clin. Endocrinol. Metab. 2013, 98, 3019–3028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wetzsteon, R.J.; Petit, M.A.; Macdonald, H.M.; Hughes, J.M.; Beck, T.J.; McKay, H.A. Bone structure and volumetric BMD in overweight children: A longitudinal study. J. Bone Miner. Res. 2008, 23, 1946–1953. [Google Scholar] [CrossRef] [PubMed]
- Dimitri, P.; Jacques, R.M.; Paggiosi, M.; King, D.; Walsh, J.; Taylor, Z.A.; Frangi, A.F.; Bishop, N.; Eastell, R. Leptin may play a role in bone microstructural alterations in obese children. J. Clin. Endocrinol. Metab. 2015, 100, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Eliakim, A.; Nemet, D.; Wolach, B. Quantitative ultrasound measurements of bone strength in obese children and adolescents. J. Pediatr. Endocrinol. Metab. 2001, 14, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Moon, R.J.; Lim, A.; Farmer, M.; Segaran, A.; Clarke, N.M.; Dennison, E.M.; Harvey, N.C.; Cooper, C.; Davies, J.H. Differences in childhood adiposity influence upper limb fracture site. Bone 2015, 79, 88–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Rocha, E.S.; Bratz, D.T.; Gubert, L.C.; de David, A.; Carpes, F.P. Obese children experience higher plantar pressure and lower foot sensitivity than non-obese. Clin. Biomech. 2014, 29, 822–827. [Google Scholar] [CrossRef] [PubMed]
- Davidson, P.L.; Goulding, A.; Chalmers, D.J. Biomechanical analysis of arm fracture in obese boys. J. Paediatr. Child Health 2003, 39, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Manning Ryan, L.; Teach, S.J.; Searcy, K.; Singer, S.A.; Wood, R.; Wright, J.L.; Hunting, K.L.; Chamberlain, J.M. The association between weight status and pediatric forearm fractures resulting from ground-level falls. Pediatr. Emerg. Care 2015, 31, 835–838. [Google Scholar] [CrossRef] [PubMed]
- Wearing, S.C.; Hennig, E.M.; Byrne, N.M.; Steele, J.R.; Hills, A.P. The impact of childhood obesity on musculoskeletal form. Obes. Rev. 2006, 7, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Gushue, D.L.; Houck, J.; Lerner, A.L. Effects of childhood obesity on three-dimensional knee joint biomechanics during walking. J. Pediatr. Orthop. 2005, 25, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Strutzenberger, G.; Richter, A.; Schneider, M.; Mundermann, A.; Schwameder, H. Effects of obesity on the biomechanics of stair-walking in children. Gait Posture 2011, 34, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Bout-Tabaku, S.; Shults, J.; Zemel, B.S.; Leonard, M.B.; Berkowitz, R.I.; Stettler, N.; Burnham, J.M. Obesity is associated with greater valgus knee alignment in pubertal children, and higher body mass index is associated with greater variability in knee alignment in girls. J. Rheumatol. 2015, 42, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, M.; Kotz, R.; Ledl, T.; Hauser, G.; Sluga, M. Prevalence of flat foot in preschool-aged children. Pediatrics 2006, 118, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Felson, D.T.; Goggins, J.; Niu, J.; Zhang, Y.; Hunter, D.J. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004, 50, 3904–3909. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson, K.; Sayers, S.P.; Minor, M.A. Measurement of varus/valgus alignment in obese individuals with knee osteoarthritis. Arthritis Care Res. 2010, 62, 690–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anandacoomarasamy, A.; Caterson, I.; Sambrook, P.; Fransen, M.; March, L. The impact of obesity on the musculoskeletal system. Int. J. Obes. 2008, 32, 211–222. [Google Scholar] [CrossRef] [PubMed]
- Widhalm, H.K.; Marlovits, S.; Welsch, G.H.; Dirisamer, A.; Neuhold, A.; van Griensven, M.; Seemann, R.; Vecsei, V.; Widhalm, K. Obesity-related juvenile form of cartilage lesions: A new affliction in the knees of morbidly obese children and adolescents. Eur. Radiol. 2012, 22, 672–681. [Google Scholar] [CrossRef] [PubMed]
- Benson, A.C.; Torode, M.E.; Fiatarone Singh, M.A. The effect of high-intensity progressive resistance training on adiposity in children: A randomized controlled trial. Int. J. Obes. 2008, 32, 1016–1027. [Google Scholar] [CrossRef] [PubMed]
- Horsak, B.; Artner, D.; Baca, A.; Pobatschnig, B.; Greber-Platzer, S.; Nehrer, S.; Wondrasch, B. The effects of a strength and neuromuscular exercise programme for the lower extremity on knee load, pain and function in obese children and adolescents: Study protocol for a randomised controlled trial. Trials 2015, 16, 586. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Zhang, Y.; Zhuang, J. The effect of weight loss on gait characteristicsof obese children. Obes. Res. Clin. Pract. 2012, 6, 35. [Google Scholar] [CrossRef]
- Korsten-Reck, U.; Kaspar, T.; Korsten, K.; Kromeyer-Hauschild, K.; Bos, K.; Berg, A.; Dickhuth, H.H. Motor abilities and aerobic fitness of obese children. Int. J. Sports Med. 2007, 28, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Kuni, B.; Ruhling, N.E.; Hegar, U.; Roth, C.; Schmitt, H. Ball games and nutrition counseling improve postural control in overweight children. BMC Pediatr. 2015, 15, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larsen, K.T.; Huang, T.; Larsen, L.R.; Olesen, L.G.; Andersen, L.B.; Moller, N.C. The effect of a multi-component camp-based weight-loss program on children’s motor skills and physical fitness: A randomized controlled trial. BMC Pediatr. 2016, 16, 91. [Google Scholar] [CrossRef] [PubMed]
- Morano, M.; Colella, D.; Rutigliano, I.; Fiore, P.; Pettoello-Mantovani, M.; Campanozzi, A. A multi-modal training programme to improve physical activity, physical fitness and perceived physical ability in obese children. J. Sports Sci. 2014, 32, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Morrison, R.; Reilly, J.J.; Penpraze, V.; Westgarth, C.; Ward, D.S.; Mutrie, N.; Hutchison, P.; Young, D.; McNicol, L.; Calvert, M.; et al. Children, parents and pets exercising together (CPET): Exploratory randomised controlled trial. BMC Public Health 2013, 13, 1096. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sola, K.; Brekke, N.; Brekke, M. An activity-based intervention for obese and physically inactive children organized in primary care: Feasibility and impact on fitness and BMI A one-year follow-up study. Scand. J. Prim. Health Care 2010, 28, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Eliakim, A.; Pantanowitz, M.; Kohen-Raz, R.; Zeev, A.; Nemet, D. The effect of a weight management program on postural balance in obese children. Eur. J. Pediatr. 2013, 172, 1619–1626. [Google Scholar] [CrossRef] [PubMed]
- Riethmuller, A.M.; Jones, R.; Okely, A.D. Efficacy of interventions to improve motor development in young children: A systematic review. Pediatrics 2009, 124, e782–e792. [Google Scholar] [CrossRef] [PubMed]
- Zask, A.; Barnett, L.M.; Rose, L.; Brooks, L.O.; Molyneux, M.; Hughes, D.; Adams, J.; Salmon, J. Three year follow-up of an early childhood intervention: Is movement skill sustained? Int. J. Behav. Nutr. Phys. Act. 2012, 9, 127. [Google Scholar] [CrossRef] [PubMed]
- Nemet, D.; Barkan, S.; Epstein, Y.; Friedland, O.; Kowen, G.; Eliakim, A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics 2005, 115, e443–e449. [Google Scholar] [CrossRef] [PubMed]
- Niederer, I.; Kriemler, S.; Zahner, L.; Burgi, F.; Ebenegger, V.; Hartmann, T.; Meyer, U.; Schindler, C.; Nydegger, A.; Marques-Vidal, P.; et al. Influence of a lifestyle intervention in preschool children on physiological and psychological parameters (Ballabeina): Study design of a cluster randomized controlled trial. BMC Public Health 2009, 9, 94. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.; de Silva-Sanigorski, A.; Hall, B.J.; Brown, T.; Campbell, K.J.; Gao, Y.; Armstrong, R.; Prosser, L.; Summerbell, C.D. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2011, 12, CD001871. [Google Scholar] [CrossRef] [PubMed]
- Westerterp, K.R. Physical activity, food intake, and body weight regulation: Insights from doubly labeled water studies. Nutr. Rev. 2010, 68, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Fu, A.; Cobley, S.; Sanders, R.H. Effectiveness of exercise intervention on improving fundamental movement skills and motor coordination in overweight/obese children and adolescents: A systematic review. J. Sci. Med. Sport 2018, 21, 89–102. [Google Scholar] [CrossRef] [PubMed]

| Authors | Gr. | Age | BMI | Measured Parameter | Results | |
|---|---|---|---|---|---|---|
| Gait Pattern | ||||||
| Dufek et al. [19] | OW | 14.9 ± 1.2 | 95.5% | Custom walkway software was used to visually inspect walkingTrial performed for completeness | Double support percent of cycle | 24.0 ± 3.1 |
| 20.2 ± 3.3 | ||||||
| Swing phase percent of cycle | 38.1 ± 2.0 | |||||
| NW | 14.7 ± 1.5 | 57.9% | 40.0 ± 1.2 | |||
| Heel to heel stance width | 11.2 ± 3.5 | |||||
| 8.8 ± 2.6 | ||||||
| Rubinstein et al. [28] | OW | 9.9 ± 1.3 | 24.3 ± 3.5 | Temporal parameters measured for 120% of the self-selected preferred walking speeds | Cycle length | 1.3 ± 0.1 |
| 1.1 ± 0.18 | ||||||
| NW | 9.9 ± 1.2 | 17.1 ± 2.0 | Cycle time | 0.8 ± 0.1 | ||
| 0.7 ± 0.1 | ||||||
| Stance phase time | 0.5 ± 0.1 | |||||
| 0.4 ± 0.0 | ||||||
| Hung et al. [29] | OW | 8.2 ± 0.3 | 22 ± 4.6 | Anterior/posterior center of pressure measurements during picking up an empty box to waist height at a self-selected pace | Normalized COP Ant/post Excursion | 8.5 ± 1.5 |
| 7.0 ± 1.4 | ||||||
| Speed of COP Move Anterior | 16.7 ± 4.3 | |||||
| 12.2 ± 3.5 | ||||||
| COP Kept Anteriorly Time | 0.3 ± 0.1 | |||||
| 0.01 ± 0.0 | ||||||
| Yan et al. [30] | OW | 9.6 ± 1.6 | 23.7 ± 3.0 | Gait data (LT) such as arch index and foot balance parameters | Arch index | 0.32 ± 0.06 |
| 0.28 ± 0.04 | ||||||
| Midfoot Relative regional impulse | 7.01 ± 3.35 | |||||
| 5.56 ± 2.08 | ||||||
| NW | 10.3 ± 0.7 | 17.1 ± 1.3 | Maximum Heel strike phase | 13.8 ± 8.6 | ||
| 20.1 ± 11.7 | ||||||
| Maximum Mid- stance phase | 7.7 ± 7.7 | |||||
| 19.6 ± 10.4 | ||||||
| Propulsion phase | 10.8 ± 8.9 | |||||
| 16.8 ± 12.7 | ||||||
| Impact/loads to the Lower Extremities and the Lower Back | ||||||
| Rubinstein et al. [28] | OW | 9.9 ± 1.3 | 24.3 ± 3.5 | Foot pressure parameters in lateral forefoot area in 120% of the self-selected preferred walking speeds | Contact area | 4.2 ± 0.9 |
| 3.4 ± 1.2 | ||||||
| NW | 9.9 ± 1.2 | 17.1 ± 2.0 | Peak pressure | 172.5 ± 46.9 | ||
| 108.8 ± 42.7 | ||||||
| Mueller et al. [31] | OB | 7.2 ± 3.2 | 23.1 ± 3.3 | Peak pressure measurements | Force time integral in midfoot | 22.4 ± 19.4 |
| 7.9 ± 6.7 | ||||||
| NW | 7.0 ± 2.8 | 16.4 ± 1.5 | Peak pressure (total foot) aged 12 | 512 ± 177 | ||
| 409 ± 124 | ||||||
| Mickle et al. [32] 2006 | OW | 4.5 ± 0.8 | 18.6 ± 1.3 | Plantar pressures were assessed to characterize dynamic foot function | Force-time integrals in midfoot | 10.2 ± 5.6 |
| 5.5 ± 4.1 | ||||||
| NW | 4.5 ± 0.7 | 5.8 ± 0.7 | Pressure-timeIntegral in midfoot | 2.0 ± 0.7 | ||
| 1.6 ± 0.5 | ||||||
| Dowling et al. [33] | OW | 8.1 ± 1.2 | >95% | Dynamic plantar pressure assessment with the subjects loaded with an additional 20% of their body mass | Static peak force | 394.3 ± 112.1 |
| 278.1 ± 52.6 | ||||||
| Static peak area | 72.6 ± 17.3 | |||||
| 51.5 ± 7.6 | ||||||
| Dynamic peak force | 558.9 ± 119.3 | |||||
| 365.6 ± 61.8 | ||||||
| Dynamic peak area | 101.1 ± 12.0 | |||||
| 78.1 ± 9.9 | ||||||
| Dynamic rear foot force | 399.2 ± 91.9 | |||||
| 260.3 ± 38.4 | ||||||
| Dynamic rear foot area | 39.3 ± 6.4 | |||||
| 25.1 ± 5.0 | ||||||
| Dynamic forefoot force | 515.3 ± 89.5 | |||||
| 354.4 ± 60.8 | ||||||
| Dynamic forefoot area | 50.0 ± 5.7 | |||||
| 41.3 ± 4.1 | ||||||
| Yan et al. [30] | OW | 9.6 ± 1.6 | 23.7 ± 3.0 | Dynamic plantar pressure distribution: sub-phases during foot-ground contact duration (LT) | Midstance phase duration | 49.5 ± 7.7 |
| 43.1 ± 10.6 | ||||||
| NW | 10.3 ± 0.7 | 17.1 ± 1.3 | Propulsion phase | 41.8 ± 7.8 | ||
| 46.2 ± 9.2 | ||||||
| Postural Balance | ||||||
| Deforche et al. [3] | OW | 9.3 ± 1.0 | 23.8 ± 3.1 | Balance Master, a computerized pressure plate system | Weight transfer time | 0.45 ± 0.60 |
| 0.21 ± 0.16 | ||||||
| Rising index | 36.2 ± 7.9 | |||||
| 44.8 ± 12.3 | ||||||
| Centre of gravity sway velocity | 5.1 ± 0.9 | |||||
| 4.1 ± 1.1 | ||||||
| NW | 9.3 ± 0.8 | 16.3 ± 1.2 | Steps width | 22.1 ± 3.0 | ||
| 19.5 ± 3.4 | ||||||
| Unilateral stance dominant leg | 8.9 ± 1.8 | |||||
| 10.0 ± 0.0 | ||||||
| Heel-to-toe walk | 3.7 ± 1.8 | |||||
| 5.6 ± 1.2 | ||||||
| Five times up and down | 10.3 ± 1.3 | |||||
| 8.6 ± 2.0 | ||||||
| Colne et al. [34] | OW | Adolesc. | 40 ± 5 | Postural stability and gait initiation | Double support | 158 ± 26 |
| 142 ± 19 | ||||||
| Length of first step of gait initiation | 0.85 ± 0.13 | |||||
| 0.87 ± 0.07 | ||||||
| NW | Adolesc. | 20 ± 2 | Peak of the post-ant velocity of CG | 1.36 ± 0.19 | ||
| 1.65 ± 0.09 | ||||||
| Mean velocity of the CP | 1.69 ± 0.33 | |||||
| 1.83 ± 0.21 | ||||||
| Steinberg et al. [35] | OW | 6–128.8 ± 1.7 G9.6 ± 1.9 B | 92% OB8% OV | Low Falling Index (FI) ≤ 36 points, moderate FI = 36–40 points, severe FI ≥ 41points | Mean FI for NW = 36 points | Mean = 28.2FI |
| 27.6% mod. FI | ||||||
| 12% severe FI | ||||||
| Goulding et al. [36] | OW | 14.8 ± 2.4 | 21.4 ± 4.2 | The Bruininks/Oseretsky sub-test of balance; the Equitest sensory organization test; and Balance Master limits of stability test | Bruininks/Oseretsky composite score | 24.5 ± 3.2 |
| 26.6 ± 2.5 | ||||||
| Equitest SOT score * | 74.6 ± 7.0 | |||||
| 73.7 ± 8.4 | ||||||
| Equitest SOT score * | 0.65 ± 0.21 | |||||
| NW | 14.9 ± 2.4 | 19.6 ± 2.6 | 0.67 ± 0.25 | |||
| Movement velocity * | 5.66 ± 2.22 | |||||
| 5.35 ± 1.98 | ||||||
| Directional control * | 73.2 ± 8.5 | |||||
| 75.0 ± 9.1 | ||||||
| Malalignments and Injuries | ||||||
| Taylor et al. [37] | OW | 12.6 ± 2.7 | 36.4 ± 8.9 | Malalignment: metaphyseal-diaphyseal angle (MDA) and anatomic tibiofemoral angle (A-TFA) | MDA (RT) | −6.5 ± 4.6° |
| −5.2 ± 3.9° | ||||||
| NW | 11.8 ± 2.9 | 19.6 ± 3.5 | Abnormal MDA and A-TFA | >11% | ||
| <3.2% | ||||||
| Mickle et al. [38] | OW | 4.3 ± 0.9 | 18.6 ± 1.2 | Foot anthropometry | Arch index | 0.26 ± 0.05 |
| 0.20 ± 0.9 | ||||||
| NW | 4.3 ± 0.7 | 15.7 ± 0.7 | Plantar arch height | 0.9 ± 0.3 | ||
| 1.1 ± 0.2 | ||||||
| Witt et al. [39] | OB | 11.9 ± 4.7 | 97.3 ± 1.2% | Operative interventions for patients with severe injury to body region | Femur fixation | 47.8% |
| 45.0% | ||||||
| NW | 12.2 ± 5.4 | 51.3 ± 23.7% | Intensive care unit, length of stay | 4.5 ± 6.9 | ||
| 4.0 ± 5.7 | ||||||
| Authors | BMI | Age | Type of Intervention | Duration of Intervention | Main Findings |
|---|---|---|---|---|---|
| Gait Pattern | |||||
| Huang [1] | 30.2 ± 3.3 | 10.7 ± 1.1 | Weight loss intervention (fun-based exercise, nutrition and behavior education) | 4 weeks | Weight loss with reduced body circumferences causes mass-driven changes in joint kinematics and kinetics; yet, the spatiotemporal gait parameters did not change |
| 26.5 ± 1.5 | 10–12 years | Muscle strengthening (dynamic, resistance exercises) | 8 weeks | Significant increases in absolute and relative muscle strength of the lower extremities compared with controls | |
| Huang et al. [101] | Exercise weight-loss program | 4 weeks | Reduce stance phase after weight loss | ||
| Peyrot et al. [42] | M: 32.0 ± 3.9 F: 36.5 ± 5.4 | 12–16 years | Weight reduction program, including nutritional education, caloric restriction, and physical activities | 12 weeks | Increased stride length with less leg muscle work to raise the center of mass after weight loss |
| Steinberg et al. [22] | 96.99 ± 2.14 percentile | 9.4 ± 0.8 | Multidisciplinary program with locomotion-emphasis exercises | 6 months | Improved foot pressure (at the heel, medial midfoot, lateral midfoot, and lateral forefoot) Improved temporal parameters (cycle length, stance phase time, relative stance phase, and swing phase time) |
| Postural Balance | |||||
| Kuni et al. [103] | F: 25.2 ± 3.6 M: 26.2 ± 2.8 | 6–12 years | “Ball School Heidelberg”—A basic introduction to ball games for school children | 6 months | Ball games and nutrition counseling improved postural control |
| Steinberg et al. [108] | 96.9 ± 2.3 percentile | 6–14 years | weight management program (including dietary intervention and exercise program) | 6 months | Improved postural stability and decreased falling probability |
| Physical Fitness and Muscle Strength | |||||
| Benson et al. [99] | High-intensity progressive resistance training | 8 weeks | Improvement in central and whole body adiposity in association with improved muscle strength | ||
| D’Hondt et al. [72] | 29.1 ± 3.6 | 10.5 ± 1.4 | Multidisciplinary residential obesity treatment program including gross motor and co-ordination exercises (assessed using the Körperkoordinationstest für Kinder—KTK) | 4 months | Treatment was found to be efficacious in generating a significant progress in gross motor co-ordination performance, with a greater increase in KTK score The amount of relative weight loss explained 26.9% of the variance in improvement in overall KTK performance |
| Horsak et al. [100] | > 97th percentile | 10–18 years | Muscle strength training and neuromuscular exercises | 12 weeks | - |
| Korsten-Reck et al. [102] | > 97th percentile | 8–12 years | FITOC (Freiburg Intervention Trial for Obese Children) consists of a combination of organized sports, behavioral therapy and nutritional advice | 8 months | Performance in all motor abilities tests improved (The AST-test battery included two speed tests, one aerobic capacity test, two strength tests and three coordinative tests) The difference between the strength of the obese children and the strength of the reference group decreased |
| Larsen et al. [104] | 24.8 (22.8–27.1) | 12.0 ± 0.4 | Two groups: Day-Camp Intervention (DCIA), with a subsequent family-based support program; and low-intense Standard Intervention Arm (SIA) | 52 weeks | Balance skills were improved post-camp in DCIA group compared to the SIA Children from the SIA improved motor skills relative to the DCIA children |
| Morano et al. [105] | ≥95th percentile | 9.2 ± 1.2 | Multi-component treatment program focused on attaining a physically active lifestyle by increasing their actual and perceived competence in performing motor tasks | 8 months | Gross motor performance (such as squat jump and countermovement jump) and actual and perceived physical abilities (perception of strength, speed and coordinative abilities) significantly improved 8 months after treatment in obese boys and girls |
| Sola et al. [107] | 27.4 (24.8–29.3) | 11.5 (9.0–12.5) | Physical fitness with motor abilities (such as balance, speed, agility, coordination and strength) | 6–12 months | All physical fitness abilities improved over the intervention period |
| Walking Energetics | |||||
| Peyrot et al. [42] | 34.6 ± 5.1 | 12–16 years | Obesity management program | 12 weeks | After weight loss, the increased walking economy was induced by the lower metabolic rate of the isometric muscular contractions required to support the lower body weight and maintain balance during walking |
| Hills & Parker [27] | - | - | Exercise and diet intervention | 16 weeks | More stable and symmetrical gait pattern (better symmetry indicators, step length and relative step); improved body composition. |
| Morrison et al. [106] | 13% of all children who participated were overweight and 7% were obese | 9–11 years | A do- based PA intervention that were motivated and supported to increase the frequency, intensity and duration of dog walking using a number of behavior change techniques | 10 weeks | Using pet dogs as the agent of lifestyle change in PA interventions in children and their parents is both feasible and acceptable |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Steinberg, N.; Nemet, D.; Pantanowitz, M.; Eliakim, A. Gait Pattern, Impact to the Skeleton and Postural Balance in Overweight and Obese Children: A Review. Sports 2018, 6, 75. https://doi.org/10.3390/sports6030075
Steinberg N, Nemet D, Pantanowitz M, Eliakim A. Gait Pattern, Impact to the Skeleton and Postural Balance in Overweight and Obese Children: A Review. Sports. 2018; 6(3):75. https://doi.org/10.3390/sports6030075
Chicago/Turabian StyleSteinberg, Nili, Dan Nemet, Michal Pantanowitz, and Alon Eliakim. 2018. "Gait Pattern, Impact to the Skeleton and Postural Balance in Overweight and Obese Children: A Review" Sports 6, no. 3: 75. https://doi.org/10.3390/sports6030075
APA StyleSteinberg, N., Nemet, D., Pantanowitz, M., & Eliakim, A. (2018). Gait Pattern, Impact to the Skeleton and Postural Balance in Overweight and Obese Children: A Review. Sports, 6(3), 75. https://doi.org/10.3390/sports6030075





