Abstract
This study investigated the influence of corrosion-induced deterioration of the tensile properties of a Mg-1 wt.% Ca alloy on the performance of a coronary artery stent model fabricated using the alloy wire. Finite element analysis was used to determine the change in various characteristics of the model when immersed in a biosimulation aqueous solution (Earle’s Balanced Salt Solution). Results from tensile tests on wires fabricated from the alloy (non-treated versus ultrasound-assisted casting (US)) were used as input to a shape optimisation study of the stent, which aimed at reducing stent strut thickness and minimising corrosion-related parameters such as equivalent plastic strain and residual stress. For each of the characteristics, it was found that the US treatment produced a more desirable result compared to the stents modelled using non-treated material data; for example, the decrease in strut thickness, equivalent plastic strain, and residual stress were each markedly greater, while keeping the stent’s functionality. These results suggest that US-treated Mg-1 wt./wt.% Ca alloy may be promising for fabricating biodegradable coronary artery stents.
1. Introduction
Permanent bare metal stents, once regarded as the optimal treatment for blood vessel obstruction, are now known to cause undesirable effects such as chronic inflammatory response, lack of or delayed endothelialisation, in-stent restenosis, and stent thrombosis [1]. Consequently, drug-eluting stents—scaffolds coated with antiproliferative drugs—were developed and showed promising results in reducing stent restenosis [2]. However, after fully absorbing the drug coating, the late catch-up phenomenon promoted late stent restenosis, highlighting the need for developing an alternative [3].
Bioresorbable stents emerged as a revolutionary treatment to address the issues posed by their predecessors [4]. Made of biodegradable materials, these stents can be deployed at the occlusion site, remodelling the artery to restore normal blood flow, after which they are fully absorbed [5]. This innovation has the potential to reduce the risks of late stent thrombosis, stent restenosis, and malapposition due to stent fracture, making it especially promising for paediatric patients [6].
Among the biodegradable metals, magnesium and its alloys have emerged as promising candidates for stent manufacturing, primarily due to their biocompatibility, biosafety, and favourable mechanical properties [7]. Particularly, AZ91 has triggered the researcher’s interest due to the combination of good mechanical properties and good biocompatibility properties [8]. Recent studies reported that AZ91 had shown adequate cell adhesion and promising biological response [9]; however, corrosion resistance and aluminium release control remain challenging [8]. On the other hand, adding calcium to magnesium alloys brings advantages such as (i) increasing their ignition temperature and reducing the flammability, making the casting process easier [10], and (ii) enhancing corrosion resistance [11].
Still, the initial excitement around magnesium was tempered by its mechanical strength being approximately five times lower than those of conventional metallic drug-eluting stents, alongside an excessively high degradation rate [12]. Additionally, the high corrosion of magnesium in aqueous environments, such as blood, is exacerbated by adverse conditions like pulsatile loading from blood pressure cycles and elevated body temperature, which continues to limit the use of magnesium-based stents since it lowers the mechanical performance of the material [13,14]. Furthermore, 50% thicker struts are required to match the mechanical performance of permanent metals like stainless steel, which impacts the stent’s profile and deliverability and may increase the risk of acute thrombotic events due to flow disturbances [12,15,16].
Material processing plays a crucial role in addressing these challenges. Advanced techniques like ultrasound melt treatment can significantly enhance magnesium alloys’ mechanical properties and degradation behaviour by refining their microstructure and improving tensile strength and corrosion [14]. These enhancements enable the design of stents with thinner struts, which are essential for reducing adverse flow events and improving deliverability without compromising mechanical integrity. On the other hand, maintaining mechanical strength over a prolonged degradation period is critical for ensuring that the stent provides adequate support during the healing process while minimising the risk of fracture and thrombosis [6]. Moreover, finite element analysis (FEA) can be employed to optimise the stent’s design, identifying the minimal strut thickness that still provides adequate mechanical support. Several optimisation-based strategies have already been documented in the literature [17,18,19]. Gharleghi et al. [20] developed a multiobjective optimisation based on hemodynamic indices. They used seven design variables, such as strut thickness and the connector shape, to reduce wall shear stress and enhance radial stiffness. A different methodology was adopted by Chen et al. [21], who performed shape optimisation of a biodegradable magnesium stent to achieve uniform deformation during crimping and expansion, enhancing mechanical performance but still resulting in thick struts. These studies underscore the challenge of enhancing radial strength and reducing residual stress in biodegradable stents.
In this sense, there is a need to explore new processing routes to produce magnesium-based alloys with superior mechanical properties that enable thinner struts, relying on finite element-based optimisation for stent design. Furthermore, the investigation of the effect of material degradation on the mechanical performance of stents over time is still lacking in the literature, with only a few studies published in the scope of biodegradable polymer stents [22,23]. Investigating this factor is critical, as the stent must retain suitable mechanical properties during degradation to prevent fracture and fragment separation [24,25].
In this study, ultrasound (US) melt treatment was applied to produce a cast ingot, which was subsequently extruded into 1 mm diameter wires. For comparison, a billet was also produced without using the ultrasonic processing. This paper examines the impact of the material’s processing route and mechanical properties deterioration on the stent’s radial strength through FEA. Tensile test results of AZ91D-1.0% Ca (wt.%) wires immersed in Earle’s Balanced Salt Solution (EBSS) for periods ranging from 48 h to 7 days (168 h) were used as input data for the analysis. Furthermore, a shape optimisation study was conducted to reduce the stent strut thickness, making it suitable for clinical practice without compromising the device’s integrity and mechanical performance by minimising residual stress and equivalent plastic strain.
2. Materials and Methods
The workflow outlining the development of the research described in this study is illustrated in Figure 1
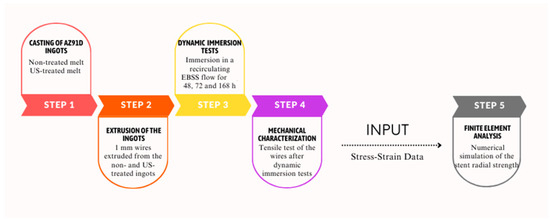
Figure 1.
Workflow of the study presented.
The study was conducted systematically, establishing a symbiosis between the experimental characterisation of AZ91D-1% wires and the numerical modelling of the stent’s radial strength and geometry optimisation.
The process’s first stage comprised the casting of AZ91D-1% Ca ingots using both non- and US-treated melts (Step 1). These ingots were then extruded into 1 mm wires (Step 2), after which they underwent dynamic immersion tests in EBSS for intervals of 48, 72, and 168 h to simulate in vivo degradation (Step 3). Following the immersion tests, mechanical characterisation was performed via tensile testing of the wires to assess changes in their mechanical properties promoted by their degradation (Step 4). The stress–strain data obtained from these tests served as input for the numerical model to simulate the stent’s radial strength under physiological conditions, considering the material degradation over time (Step 5). This comprehensive process enabled a detailed evaluation of the relationship between the material’s degradation due to exposure to the EBSS medium and the deterioration of mechanical properties. Furthermore, the results allowed the study of ultrasound’s potential for enhancing the corrosion response of the material, which was then used as a cornerstone for the stent’s shape optimisation.
2.1. Dynamic Degradation Tests and Mechanical Characterisation
Under an argon atmosphere, 400 g of AZ91D-1% Ca alloy (8.90 Al, 0.56 Zn, 0.30 Mn, 0.98 Ca, wt.%) was melted in a SiAlON crucible. The melt was held at 620 ± 5 °C for 20 min, then raised to 680 ± 5 °C for homogenisation. A pre-heated acoustic radiator was immersed 15 mm into the melt, and ultrasonic vibration (300 W, 20.1 ± 0.25 kHz) was applied for 120 s. The melt was then poured into a metallic mould pre-heated to 250 ± 5 °C, producing a billet 150 mm long and 50 mm in diameter. For comparison, a billet without ultrasound treatment was also cast.
Before extrusion, the billets were heated to 350 °C for 30 min. Extrusion was performed with a 2.5 MN automated press at 0.1 mm/s, using a die with four 1 mm diameter nozzles.
The corrosion tests were conducted in EBSS, favoured for in vitro testing of biodegradable magnesium materials due to its degradation rate closely mirroring in vivo conditions [26,27]. The wires were encased in antifatigue silicone tubes and positioned in an acrylic column filled with water at 37 °C by a circulating water bath. A peristaltic pump maintained a steady flow of the medium at 25 mL/min through the silicone tubes. Two reservoirs of 5 L collected the solution circulating within the channels containing non-treated and US-treated samples. The pH was monitored in 12-h intervals and kept between 7–7.4. For each manufacturing condition, nine replicates were tested at 48, 72, and 168-h intervals. Tensile tests on the as-extruded wires before and after immersion in EBSS were conducted using an H100KS Hounsfield Universal Testing Instrument at a constant crosshead speed of 1 mm/s. The ultimate tensile strength and elongation at break were determined by averaging the results from nine tests.
2.2. Numerical Simulation Methodology
Radial strength is a critical metric for evaluating stent performance, closely linked to the material’s mechanical properties [28]. Degradation of magnesium alloys under physiological conditions typically leads to diminished mechanical properties, reducing the stent’s radial support capacity [29]. To address this topic, a numerical analysis was conducted using tensile test data from both non-degraded and degraded wires. This analysis assessed the loss of mechanical strength due to material degradation and facilitated the optimisation of stent design to enhance performance and durability.
Tensile test data of non-treated and US-treated AZ91D-1.0% Ca (wt.%) wires immersed in EBSS for 48, 72, and 168 h were used as input data. The stress–strain curves allowed for evaluating the influence of mechanical properties’ degradation on the stent’s radial strength, while stress–strain curves of non-degraded materials were used to simulate stent expansion.
The NG stent geometry (Figure 2a) with nonexpanded inner radius, length and thickness of 2.50 mm, 12.00 mm, and 0.20 mm, respectively, was selected. The NG stent model was chosen because it features curved link elements that deform during expansion, effectively balancing longitudinal shrinkage. This design ensures uniform expansion and enhances structural integrity during deployment, making it an ideal choice for this investigation [30].
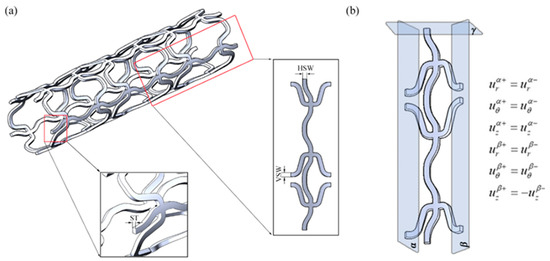
Figure 2.
(a) Identification of the geometric variables of NG stent: ST—strut thickness; HSW—horizontal strut width; VSW—vertical strut width; (b) representation of the symmetry boundary conditions (α and β planes represent the radial symmetry and γ plane stands for the longitudinal symmetry).
Due to the geometric periodicity of the stent in the circumferential and longitudinal directions, only one-tenth of the model was considered, reducing the number of degrees of freedom and computation time without compromising result accuracy. Symmetry conditions were applied to the lateral and central faces of the stent on planes α, β, and γ (Figure 2b).
A two-step model (Figure 3) was developed, consisting of (i) the stent radial expansion and recoil followed by (ii) the simulation of the radial pressure exerted by the artery on the stent. In the first stage, the stent was subjected to a radial displacement that increased its internal radius from 2.50 mm to 3.15 mm, followed by recoil. In the second stage, an inward force was applied linearly until the von Mises stress reached the material’s tensile strength at each degradation time point, determining the stent’s radial strength evolution over immersion time.
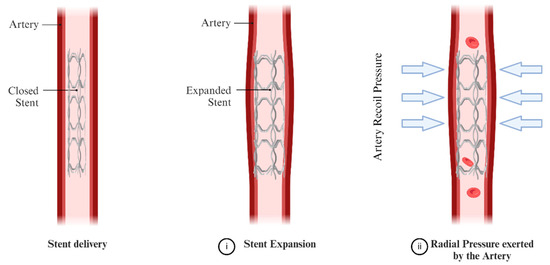
Figure 3.
Overview of the Simulation Steps Considered.
A mesh convergence study was conducted to ensure the accuracy of the numerical model. The mesh was systematically refined, with a convergence criterion set as a 5% change in the maximum stress value over the stent. Mesh refinement continued until the variation in maximum stress between successive mesh densities was within this 5% threshold, ensuring that the results were independent of further refinement.
The developed numerical model was validated by reproducing studies reported in the literature.
The stress–strain curve for the 168-h immersion period, representing the lowest mechanical properties observed in the study, was used in the optimisation study to optimise the design under the most demanding scenario. In this scenario, the radial force applied in the initial simulation stage was substituted with a radial pressure of 0.20 MPa to simulate arterial recoil [31]. The multiobjective optimisation process was based on the Constrained Optimisation by Linear Approximation (COBYLA) numerical method. COBYLA minimises an objective function F(X) subject to M inequality constraints of the form g(X) ≥ 0 on X, where X is a vector of variables that has N components. This algorithm employs linear approximations for both objective and constraint functions through linear interpolation at N + 1 points within the variable space. When determining new variable values, each constraint is evaluated individually rather than being integrated into a single penalty function [32].
Stent optimisation involves many variables, including geometrical parameters, material properties, and physiological conditions [33], leading to most research focusing on a limited number of elements.
The optimisation strategy targets key variables that significantly impact the performance and durability of Mg alloy stents. Critical factors include stent strut thickness, residual stress post-expansion, and equivalent plastic strain, which influence clinical outcomes and device integrity. Minimising strut thickness is pivotal in affecting inflammation levels at the lesion site and neo-intima coverage, which is crucial for reducing restenosis and thrombosis rates [34,35]. Managing residual stress after stent expansion is essential to prevent stress corrosion, micro-cracks, and potential fractures, thus safeguarding device reliability and patient safety. Additionally, minimising equivalent plastic strain is vital for mitigating high-stress areas within the stent structure, ensuring long-term mechanical strength stability [36].
In this sense, the optimisation process aims to minimise an objective function that includes three individual objectives: (i) strut thickness, (ii) average residual stress post-recoiling, and (iii) average equivalent plastic strain at full stent expansion. The design variables, including the widths of horizontal and vertical struts (Figure 2a), are used as design control variables to achieve optimal stent performance, while the constraint was that no more than 5.0% of the stent volume (Vstent) experiences a mean von Mises stress (σVM) that is equal to or greater than the tensile strength of the material before immersion in EBSS (σult). Such a criterion was intended to ensure that most of the stent structure remains below the material’s ultimate tensile strength, thus preventing premature failure and enhancing its durability. This threshold results from a balance between achieving optimal performance and maintaining structural integrity, as it allows for some localised high-stress regions without compromising the overall integrity and functionality of the stent.
The optimisation process is described by Equations (1) and (2) as follows:
3. Results and Discussion
3.1. Wires Characterisation before and after Immersion
The stress–strain curves from tensile testing of non-treated and US-treated AZ91D-1.0% Ca (wt.%) wires immersed in EBSS for 48, 72, and 168 h and as-cast are presented in Figure 4.
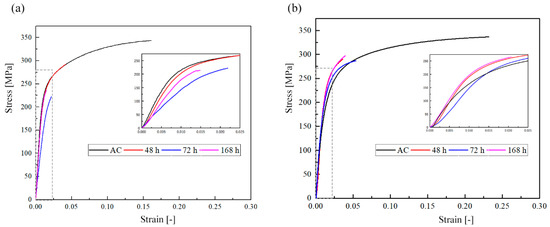
Figure 4.
Stress–strain curves from uniaxial tensile testing of (a) non- and (b) US-treated AZ91D-1 wt.% Ca wires after immersion in EBSS.
As can be observed, both materials exhibited a gradual decrease in mechanical properties, namely ultimate tensile strength and elongation at fracture, with increasing immersion time. However, the degradation patterns were different between the two material processing conditions. For non-treated samples (Figure 4a), the as-cast condition displayed the highest ultimate tensile strength and elongation at fracture, which remarkably decreased with increasing immersion time. After immersion for 168 h, the material exhibited the lowest mechanical properties, indicating their severe degradation. On the other hand, US-treated samples (Figure 4b) demonstrated a superior ability to retain mechanical properties over immersion time. While the as-cast condition still exhibited the highest strength, the difference in ductility between the immersion times was less pronounced compared to non-treated samples. The decrease in strength with immersion time was also less severe, leading to an ultimate tensile strength after immersion for 168 h that was significantly higher than that shown by the non-treated material. The mechanical properties analysed are presented in Table 1 for the non- and US-treated materials before and after immersion in EBSS for 168 h.

Table 1.
Mechanical properties of the non- and US-treated wires before and after immersion in EBSS for 168 h.
The difference observed in the mechanical properties of non- and US-treated materials can be explained by the distinct corrosion behaviour exhibited. The wires’ surface after removing the corrosion products formed after immersion in EBSS for 168 h are presented in Figure 5.
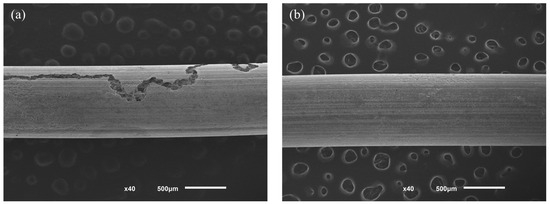
Figure 5.
Surface morphology of the wires obtained from (a) non- and (b) US-treated ingots after removing the corrosion products formed after immersion for 168 h.
After immersion in EBSS and subsequent removal of corrosion products, the surface morphologies of non-treated (Figure 5a) and US-treated (Figure 5b) wires showed notable differences. The non-treated samples displayed significant deterioration, marked by severe corrosion that appeared to propagate along the extrusion direction, correlating with the distribution of intermetallic particles, as reported in our previous work. Conversely, the wires from US-treated ingots exhibited a regular surface, indicating that uniform corrosion occurred.
The surface morphology of the wires can be helpful in the analysis of the deterioration of the mechanical properties. Indeed, severe localised corrosion observed in the non-treated wires resulted in deep cracks and extensive deterioration along the extrusion direction. This non-uniform corrosion pattern corresponded to a significant decrease in mechanical properties. US-treated wires, on the other hand, displayed a more uniform corrosion pattern, which allowed the material to retain its mechanical integrity longer.
Briefly, the stress–strain curves resulting from the tensile tests of the materials before immersion in EBSS were used as input data to simulate the radial expansion of the stent. In contrast, its response to an increasing radial force mimicking the artery radial recoil was simulated using the data from mechanical characterisation after immersion for 48, 72, and 168 h. The design optimisation targeted minimising the strut thickness, average residual stress post-recoiling, and average equivalent plastic strain at full stent expansion to achieve optimal stent performance, as these parameters can be associated with better stent performance and clinical outcomes.
3.2. Numerical Simulation Results
Figure 6a illustrates the evolution of the stent radius in response to increasing inner surface pressure during expansion, while Figure 6b shows the distribution of von Mises stress across the stent unit.
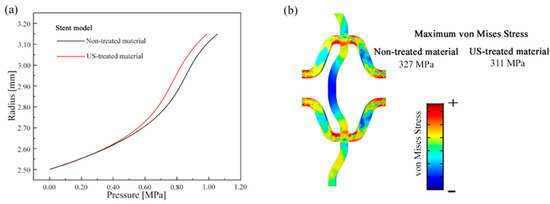
Figure 6.
(a) Evolution of the strut radius as a function of the expanding pressure applied in its inner surface and (b) von Mises distribution over the stent unit.
The results (Figure 6) indicate that the stent modelled using US-treated material data expanded more easily than the non-treated alloy. This improved ease of expansion is attributed to the higher ductility of the US-treated material, which allows it to deform more readily under lower pressures. Supporting this, von Mises stress analysis showed that the maximum stress was lower in the US-treated material compared to the non-treated alloy. However, the stress distribution was similar for both materials, with higher stress concentrations observed in the curved regions of the stent’s struts, where deformation was more pronounced.
Figure 7 depicts the progression of radial force in stents fabricated from non-treated and US-treated AZ91D-1.0% Ca (wt.%) wires. The results suggest that the radial force supported by the stent made from non-treated material was initially higher than that of those treated by the US. This trend persisted for up to 48 h of immersion, after which a reversal occurred. By 72 h of immersion, the radial force of the US-treated stents was ≈4.0% higher than that of the non-treated stents, a difference that widened to ≈14.0% after 168 h. Furthermore, the stents modelled using US-treated material data exhibited a slower deterioration in mechanical strength with prolonged immersion times compared to the non-treated ones, likely due to their distinct degradation behaviour, as previously discussed in [10]. Nonetheless, non-treated and US-treated stents showed a marked drop in radial force, underscoring the need for additional modifications to ensure stent integrity over the typical treatment duration of six months.
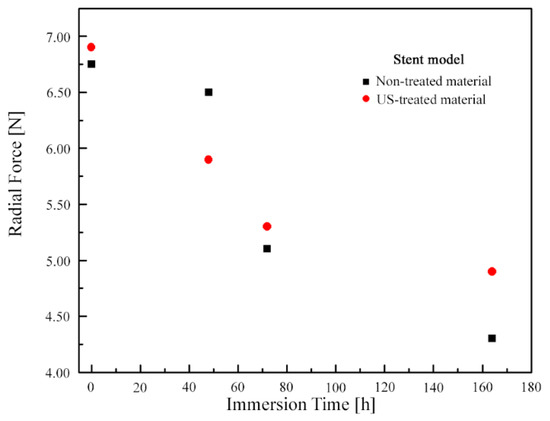
Figure 7.
Evolution of the radial force of the stents built from non- and US-treated wires over the duration of immersion time.
Concerning the optimisation study, Figure 8 illustrates the evolution of the objective function and design variables for the optimisation process for reducing (i) strut thickness, (ii) average residual stress after stent recoiling, and (iii) average equivalent plastic strain at the fully expanded configuration of the stents made of non- and US-treated AZ91D-1.0 wt.% Ca.
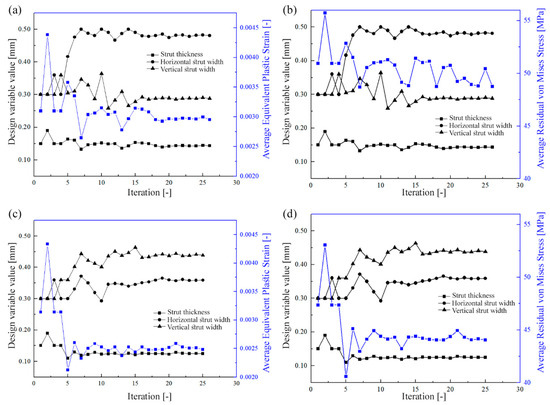
Figure 8.
Evolution of (a,c) mean equivalent plastic strain and (b,d) mean residual stress as a function of the design control variables for (a,b) non- and (c,d) US-treated stents.
The results presented in Figure 8 reveal that the impact of design control variables on the plastic strain and residual stress was similar for stents modelled with both non-treated and US-treated alloy data. When compared to the reference design (Figure 2a), the stents exhibited reductions in strut thickness to 0.160 mm and 0.125 mm, respectively. Additionally, these reductions in strut thickness were offset by increasing the width of both horizontal and vertical struts, which helped to reduce average residual stress and equivalent plastic strain while still meeting the design constraints. This achievement is meaningful as it enables a reduction in strut thickness without sacrificing radial strength, marking a notable advancement in the design of biodegradable stents. Indeed, typically, biodegradable devices rely on thicker struts to ensure adequate radial support during vessel remodelling [32]. However, these high-thickness struts are frequently associated with an increased risk of late thrombotic events and impaired endothelialisation [37].
Furthermore, while maintaining mechanical integrity, the optimised designs are inherently linked to improvements in residual stress distribution and the minimisation of high-stress areas within the stent structure. On the other hand, using thinner struts promotes the formation of a more uniform microstructure, which can be associated with higher corrosion resistance. The relationship between mechanical optimisation and microstructural phenomena, such as microstructure uniformity and degradation resistance, underscores the clinical viability of thinner biodegradable stents.
Table 2 compares the performance of the optimized (Opt.) and reference (Ref.) stent designs, numerically simulated considering non- and US-treated material, based on data from the wires immersed in EBSS for 168 h.

Table 2.
Summary of the main results concerning the reference (Ref.) and optimised (Opt.) stents geometry made from non- and US-treated material.
The optimized (Opt.) stent modelled with mechanical parameters derived from non- and US-treated material achieved an average reduction in residual stress of 8.1% and 15.5%, respectively, compared to the reference (Ref.) geometry. The decrease in average equivalent plastic strain was more pronounced, showing 28.4% and 46.0% reductions for stents modelled using non-treated and US-treated material parameters, respectively. Furthermore, the volume fraction of the stent that underwent high levels of von Mises residual stress (>100 MPa) was reduced for both material conditions. However, the reduction was marginal for the stent modelled with non-treated material properties (15.4% vs. 14.9%). On the contrary, the stent modelled with ultrasonically treated material properties exhibited a substantial reduction of approximately 45.1%, decreasing from about 14.2% to 7.8%.
The distribution of equivalent plastic strain at the fully expanded stent, modelled with mechanical properties from both non-treated and US-treated materials, is illustrated in Figure 9.
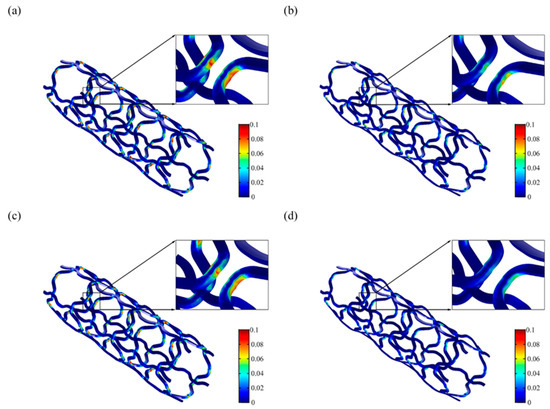
Figure 9.
Distribution of the equivalent plastic strain at the maximum expanded configuration of the (a,c) reference (Ref.) and (b,d) optimised (Opt.) stent geometry built using non- (a,b) and US-treated (c,d) alloy wires.
The highest values of equivalent plastic strain are consistently found in regions with high curvature radii for both the reference (Ref.) and optimised (Opt.) stent geometries, regardless of processing conditions. However, both the maximum equivalent plastic strain value and the affected volume have significantly decreased, with a more marked reduction observed in the stent modelled with the mechanical properties of US-treated material.
As expected, the distribution of the von Mises stress after stent recoiling (Figure 10) reveals that the highest stress values overlap the maximum equivalent plastic strain areas. The design optimization allowed a considerable reduction in the maximum von Mises stress for both stents modelled with mechanical properties of non-treated and US-treated materials, thereby enhancing the device’s mechanical strength during service.
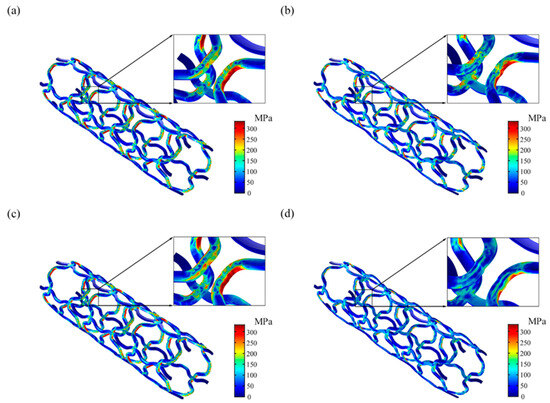
Figure 10.
Distribution of the von Mises stress after stent recoiling of the (a,c) reference (Ref.) and (b,d) optimised (Opt.) stent geometry built using non- (a,b) and US-treated (c,d) alloy wires.
The optimisation process resulted in a stent design capable of achieving superior functional performance by reducing both average equivalent plastic strain and average residual stress. This minimisation is critical in mitigating stress corrosion and preventing premature fracture, thereby potentially extending the stent’s ability to support arterial remodelling over an extended period [32]. On the other hand, the superior mechanical properties granted by the ultrasound treatment enabled a significant decrease in the strut thickness, which is advantageous from the perspectives of biocompatibility and endothelialisation [24].
3.3. Study Clinical Relevance and Limitations
The investigation conducted is highly relevant to clinical applications as it emphasizes the use of material processing to improve stent performance. The study shows that optimizing design and enhancing mechanical properties makes it possible to reduce corrosion-related issues such as equivalent plastic strain and residual stress, while allowing for thinner struts. Thinner struts are associated with better clinical outcomes. Combining experimental characterization with numerical modelling provides valuable insights into how AZ91D-1% stents, a promising material for biodegradable applications, can be optimized to improve radial strength and durability under physiological conditions. These findings have the potential to enhance stent performance, decrease the risk of restenosis, and improve patient outcomes by customizing stent design to account for material degradation over time [3,4].
Despite the relevance of this study, some limitations must be highlighted. Firstly, while informative, the in vitro degradation simulations may not fully replicate the complex in vivo environment, potentially affecting the accuracy of the numerical model’s predictions. Additionally, the stent crimping before deployment is also a source of residual stress, which can play a role in its subsequent response.
These limitations should be addressed in future studies to ensure the applicability and reliability of the optimized stent designs to clinical practice.
4. Conclusions
This study systematically integrated experimental and numerical methods to study the stent behaviour during its expansion and when subjected to an inward radial force that mimics artery recoil. Furthermore, an optimisation geometry study was also carried out to minimise strut thickness, equivalent plastic strain and residual stress after stent recoil. In this way, AZ91D-1% Ca wires were extruded from non- and US-treated ingots and subjected to dynamic immersion tests in EBSS to simulate degradation for different periods (ti). Afterwards, tensile testing to assess changes in mechanical properties was performed, and the resulting data were used in a numerical model to evaluate the stent’s radial strength and optimise its geometry.
The study results led to the following conclusions:
- When ti = 168 h, the decrease in radial force in the model when US-treated wire was used was less than when non-treated wire was used (~29% vs. ~36%).
- When ti = 168 h, the decrease in radial thickness, increase in horizontal strut width, increase in vertical strut width, decrease in mean residual stress, decrease in maximum residual stress, decrease in mean equivalent plastic strain, and decrease in maximum equivalent plastic strain when US-treated wire was used were each markedly greater than when the non-treated wire was used (difference ranging from ~6% to ~56%).
- These results suggest that the use of US-treated AZ91D wire may be promising for fabricating biodegradable coronary artery stents. Further studies in support of this suggestion are needed, among which is the determination of the ability of the expanded stent to withstand recoil when subjected to radial pressure exerted by the artery and fatigue performance.
Author Contributions
Conceptualization, I.V.G. and H.P.; Methodology, I.V.G.; Validation, H.P. and J.L.A.; Formal cAnalysis, I.V.G. and H.P.; Investigation, I.V.G.; Resources, H.P. and J.L.A.; Data Curation, I.V.G.; Writing—original draft preparation, I.V.G.; Visualization, I.V.G. and H.P.; Supervision, H.P. and J.L.A. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Fundação para a Ciência e Tecnologia (FCT) under the strategic program UIDB/04436/2020.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hensey, M.; Sathananthan, J.; Teguh, W.P.; Mulvihill, N. (Eds.) Primary Angioplasty: A Practical Guide [Internet]; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Moses, J.W.; Leon, M.B.; Popma, J.J.; Fitzgerald, P.J.; Holmes, D.R.; O’Shaughnessy, C.; Caputo, R.P.; Kereiakes, D.J.; Williams, D.O.; Teirstein, P.S.; et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N. Engl. J. Med. 2003, 349, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wu, S.; Kawashima, H.; Hara, H.; Ono, M.; Gao, C.; Wang, R.; Lunardi, M.; Sharif, F.; Wijns, W.; et al. Current perspectives on bioresorbable scaffolds in coronary intervention and other fields. Expert Rev. Med. Devices 2021, 18, 351–365. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, A.; Jepson, N.; Bressloff, N.W.; Loh, P.H.; Ray, T.; Beier, S. The road to the ideal stent: A review of stent design optimisation methods, findings, and opportunities. Mater. Des. 2024, 237, 112556. [Google Scholar] [CrossRef]
- Reddy, S.R.V.; Welch, T.R.; Nugent, A.W. Biodegradable stent use for congenital heart disease. Prog. Pediatr. Cardiol. 2021, 61, 101349. [Google Scholar] [CrossRef]
- Gallinoro, E.; Almendarez, M.; Alvarez-Velasco, R.; Barbato, E.; Avanzas, P. Bioresorbable stents: Is the game over? Int. J. Cardiol. 2022, 361, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Gu, X.; Zheng, Y.; Cheng, Y.; Zhong, S.; Xi, T. In vitro corrosion and biocompatibility of binary magnesium alloys. Biomaterials 2009, 30, 484–498. [Google Scholar] [CrossRef] [PubMed]
- Albayrak, S.; Gül, C.; Emin, N.; Gökmen, U.; Karakoç, H.; Uzun, A.; Çinici, H. Electrochemical, mechanical, and antibacterial properties of the AZ91 Mg alloy by hybrid and layered hydroxyapatite and tantalum oxide sol–gel coating. Mater. Test. 2023, 65, 1628–1644. [Google Scholar] [CrossRef]
- Brooks, E.K.; Der, S.; Ehrensberger, M.T. Corrosion and mechanical performance of AZ91 exposed to simulated inflammatory conditions. Mater. Sci. Eng.. C Mater. Biol. Appl. 2016, 60, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Fan, J.; Chen, Z.; Yang, W.; Fang, S.; Xu, B. Effect of yttrium, calcium and zirconium on ignition-proof principle and mechanical properties of magnesium alloys. J. Rare Earths 2012, 30, 74–78. [Google Scholar] [CrossRef]
- Harandi, S.E.; Mirshahi, M.; Koleini, S.; Idris, M.H.; Jafari, H.; Kadir, M.R.A. Effect of calcium content on the microstructure, hardness and in-vitro corrosion behavior of biodegradable Mg-Ca binary alloy. Mat. Res. 2013, 16, 11–18. [Google Scholar] [CrossRef]
- Ang, H.Y.; Ng, J.; Bulluck, H.; Wong, P.; Venkatraman, S.; Huang, Y.; Foin, N. Fundamentals of bioresorbable stents. In Functionalised Cardiovascular Stents; Elsevier: Amsterdam, The Netherlands, 2018; pp. 75–97. [Google Scholar]
- Jafari, S.; Harandi, S.E.; Raman, R.K.S. A Review of Stress-Corrosion Cracking and Corrosion Fatigue of Magnesium Alloys for Biodegradable Implant Applications. JOM 2015, 67, 1143–1153. [Google Scholar] [CrossRef]
- Gomes, I.V.; Pacheco, M.; Nienaber, M.; Neves, S.C.; Mei, D.; Barros, A.; Reis, R.L.; Alves, J.L.; Puga, H. Shielding AZ91D-1%Ca from corrosion through ultrasound melt treatment: A study for stent design. J. Magnes. Alloys 2023, 11, 2901–2915. [Google Scholar] [CrossRef]
- Berglund, J.; Guo, Y.; Wilcox, J. Challenges related to development of bioabsorbable vascular stents. EuroIntervention 2009, 5 (Suppl. F), F72–F79. [Google Scholar] [CrossRef] [PubMed]
- Foin, N.; Lee, R.D.; Torii, R.; Guitierrez-Chico, J.L.; Mattesini, A.; Nijjer, S.; Sen, S.; Petraco, R.; Davies, J.E.; Di Mario, C.; et al. Impact of stent strut design in metallic stents and biodegradable scaffolds. Int. J. Cardiol. 2014, 177, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, N.S.; Folgado, J.; Rodrigues, H.C. Surrogate-based multi-objective design optimization of a coronary stent: Altering geometry toward improved biomechanical performance. Int. J. Numer. Methods Biomed. Eng. 2021, 37, e3453. [Google Scholar] [CrossRef] [PubMed]
- Russ, J.B.; Li, R.L.; Herschman, A.R.; Waisman, H.; Vedula, V.; Kysar, J.W.; Kalfa, D. Design optimization of a cardiovascular stent with application to a balloon expandable prosthetic heart valve. Mater. Des. 2021, 209, 109977. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Bi, Y.; Zhao, H.; Wu, T.; Xu, F.; Zhao, G. Structural optimization and finite element analysis of poly-l-lactide acid coronary stent with improved radial strength and acute recoil rate. J. Biomed. Mater. Res. Part B Appl. Biomater. 2020, 108, 2754–2764. [Google Scholar] [CrossRef] [PubMed]
- Gharleghi, R.; Wright, H.; Luvio, V.; Jepson, N.; Luo, Z.; Senthurnathan, A.; Babaei, B.; Prusty, B.G.; Ray, T.; Beier, S. A multi-objective optimization of stent geometries. J. Biomech. 2021, 125, 110575. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Chen, J.; Wu, W.; Shi, Y.; Jin, L.; Petrini, L.; Shen, L.; Yuan, G.; Ding, W.; Ge, J.; et al. In vivo and in vitro evaluation of a biodegradable magnesium vascular stent designed by shape optimization strategy. Biomaterials 2019, 221, 119414. [Google Scholar] [CrossRef]
- Qiu, T.; He, R.; Abunassar, C.; Hossainy, S.; Zhao, L.G. Effect of two-year degradation on mechanical interaction between a bioresorbable scaffold and blood vessel. J. Mech. Behav. Biomed. Mater. 2018, 78, 254–265. [Google Scholar] [CrossRef]
- Polak-Kraśna, K.; Abaei, A.R.; Shirazi, R.N.; Parle, E.; Carroll, O.; Ronan, W.; Vaughan, T.J. Physical and mechanical degradation behaviour of semi-crystalline PLLA for bioresorbable stent applications. J. Mech. Behav. Biomed. Mater. 2021, 118, 104409. [Google Scholar] [CrossRef] [PubMed]
- Blair, R.W.; Dunne, N.J.; Lennon, A.B.; Menary, G.H. Multi-objective optimisation of material properties and strut geometry for poly(L-lactic acid) coronary stents using response surface methodology. PLoS ONE 2019, 14, e0218768. [Google Scholar] [CrossRef] [PubMed]
- Amnieh, S.K.; Mashayekhi, M.; Shahnooshi, E.; Tavafoghi, M.; Mosaddegh, P. Biodegradable performance of PLA stents affected by geometrical parameters: The risk of fracture and fragment separation. J. Biomech. 2021, 122, 110489. [Google Scholar] [CrossRef]
- Atrens, A.; Johnston, S.; Shi, Z.; Dargusch, M.S. Viewpoint-Understanding Mg corrosion in the body for biodegradable medical implants. Scr. Mater. 2018, 154, 92–100. [Google Scholar] [CrossRef]
- Johnston, S.; Shi, Z.; Venezuela, J.; Wen, C.; Dargusch, M.S.; Atrens, A. Investigating Mg Biocorrosion In Vitro: Lessons Learned and Recommendations. JOM 2019, 71, 1406–1413. [Google Scholar] [CrossRef]
- Jinnouchi, H.; Torii, S.; Sakamoto, A.; Kolodgie, F.D.; Virmani, R.; Finn, A.V. Fully bioresorbable vascular scaffolds: Lessons learned and future directions. Nat. Rev. Cardiol. 2019, 16, 286–304. [Google Scholar] [CrossRef] [PubMed]
- Peron, M.; Torgersen, J.; Berto, F. Mg and Its Alloys for Biomedical Applications: Exploring Corrosion and Its Interplay with Mechanical Failure. Metals 2017, 7, 252. [Google Scholar] [CrossRef]
- Gomes, I.V.; Puga, H.; Alves, J.L. Shape and functional optimization of biodegradable magnesium stents for manufacturing by ultrasonic-microcasting technique. Int. J. Interact. Des. Manuf. 2018, 12, 1059–1069. [Google Scholar] [CrossRef]
- Rieu, R.; Barragan, P.; Masson, C.; Fuseri, J.; Garitey, V.; Silvestri, M.; Roquebert, P. Radial force of coronary stents: A comparative analysis. Cathet. Cardiovasc. Intervent. 1999, 46, 380–391. [Google Scholar] [CrossRef]
- Powell, M.J.D. (Ed.) A Direct Search Optimization Method That Models the Objective and Constraint Functions by Linear Interpolation. 1994. Available online: https://link.springer.com/chapter/10.1007/978-94-015-8330-5_4 (accessed on 27 June 2024).
- Resor, C.D.; Bhatt, D.L. Thin to Ultrathin. Circ. Cardiovasc. Interv. 2018, 11, e007407. [Google Scholar] [CrossRef]
- Lupi, A.; Rognoni, A.; Secco, G.G.; Lazzero, M.; Nardi, F.; Fattori, R.; Bongo, A.S.; Agostoni, P.; Sheiban, I. Biodegradable versus durable polymer drug eluting stents in coronary artery disease: Insights from a meta-analysis of 5834 patients. Eur. J. Prev. Cardiol. 2014, 21, 411–424. [Google Scholar] [CrossRef] [PubMed]
- Otsuka, F.; Vorpahl, M.; Nakano, M.; Foerst, J.; Newell, J.B.; Sakakura, K.; Kutys, R.; Ladich, E.; Finn, A.V.; Kolodgie, F.D.; et al. Pathology of second-generation everolimus-eluting stents versus first-generation sirolimus- and paclitaxel-eluting stents in humans. Circulation 2014, 129, 211–223. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, J.; Sheng, K.; Miao, F.; Wang, Y.; Zhang, Y.; Hou, R.; Mei, D.; Sun, Y.; Zheng, Y.; et al. Optimizing structural design on biodegradable magnesium alloy vascular stent for reducing strut thickness and raising radial strength. Mater. Des. 2022, 220, 110843. [Google Scholar] [CrossRef]
- Chevalier, B. Stent Strut Thickness: Have We Reached the Minimum? Card. Interv. Todays 2018, 12, 66–67. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).