Monitoring and Predicting Occupant’s Sleep Quality by Using Wearable Device OURA Ring and Smart Building Sensors Data (Living Laboratory Case Study)
Abstract
:1. Introduction
2. Research Goals and Objectives
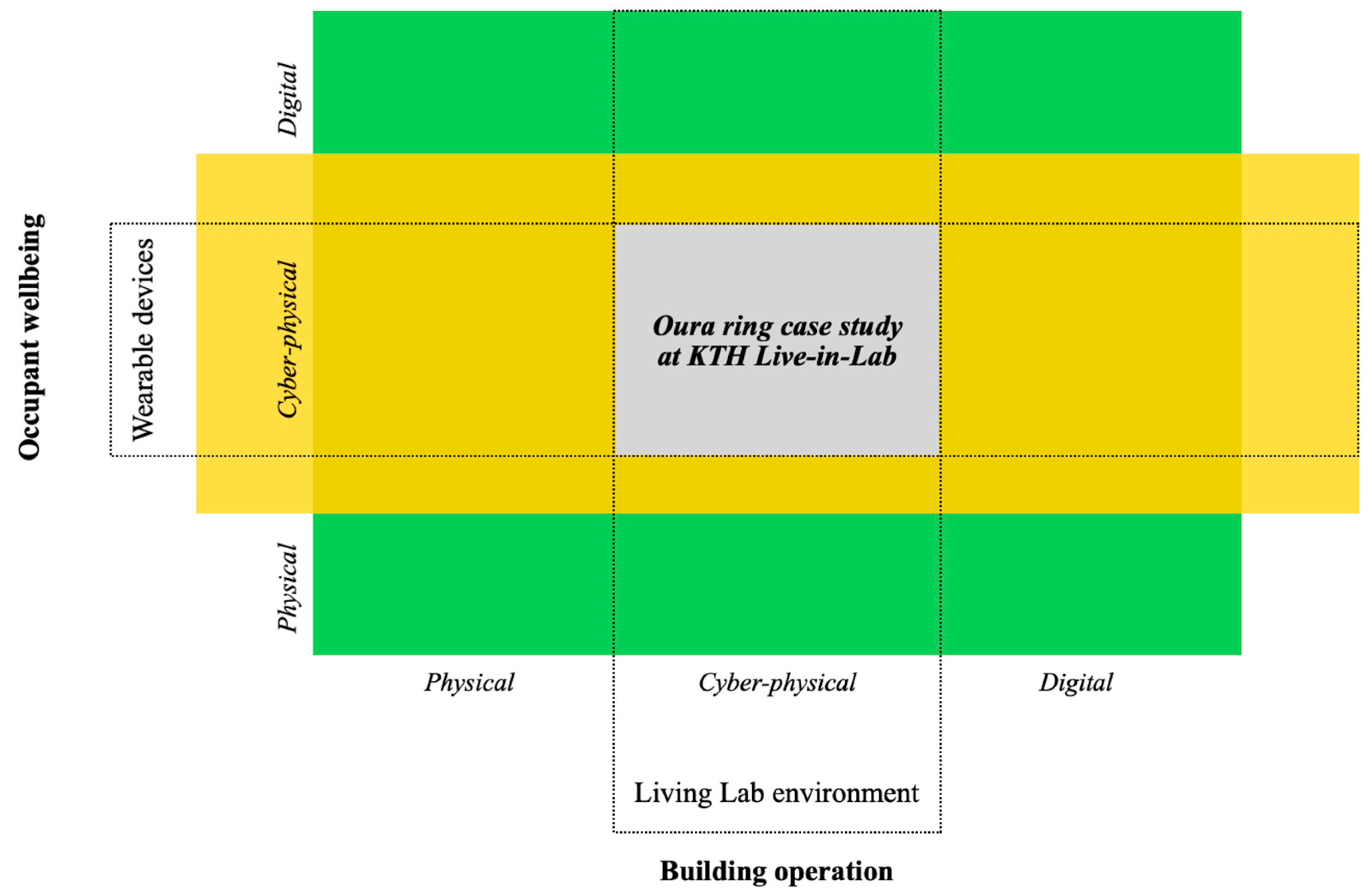
2.1. Research Big Picture: Human-Building Interaction
2.2. Research Goal and Objectives
- What are the possibilities and limitations of measuring sleep quality from built environments and a commercially-off-the-shelf wearable device (OURA ring) in a real-life context?
- Can the data from the OURA ring and smart meters be used for providing personalized instructions for its users to increase their sleep quality?
- Assess the quality of the data collected from the OURA ring.
- Investigate whether the data from commercially-off-the-shelf wearable device (OURA ring) can be used in combination with the ambient data to create an appropriate model for sleep quality evaluation.
- Data storage: Building a data storage with an appropriate data structure from the OURA ring and smart meters data.
- Data quality assessment: What are the possibilities and limitations of measuring sleep quality in a real-life context with the use of the OURA ring?
- Modeling: Building an ANN for improving sleep quality with the OURA ring and smart meters’ data based on the possibilities and limitations concluded about the data from sub-goal 2.
3. System Boundaries and Methodology Overview
3.1. System Boundaries
3.1.1. KTH Live-in-Lab
3.1.2. Wearable Device OURA Ring
- NTC Temperature Sensors: this sensor is responsible for measuring the body temperature directly from the skin. OURA claims that by using these sensors they are able to produce accurate measurements of the person’s body temperature. According to OURA, this is a better approach than estimating it from the surroundings;
- OURA uses a 3D accelerometer to measure different activity- and movement-related parameters, and they combine these parameters with the profile information that the user provided to perform accurate analysis and provide accurate data about energy expenditure and movement (steps, miles);
- Infrared light sensor: this sensor measures the respiratory rate, and the reason that OURA uses this sensor is due to its higher accuracy compared to other sensors such as green light LEDs.
- (1)
- The diversity of bio signals;
- (2)
- Raw data access for research support;
- (3)
- Convenience to wear 24/7, especially while sleeping.
3.1.3. Smart Meters by SE
3.2. Research Process
4. Implementation and Analysis
4.1. Database
4.2. Data Quality Assessment
- -
- Define: This process identifies the quality of information requested by information consumers. It also analyses the information life cycle that characterizes the production process. In our assessment, this process will identify the metrics and desired information that could potentially be used for the modeling stage of our research;
- -
- Measure: In this phase, we will measure the different data we have according to the metrics and desired information we identified in the previous process. That allows us to analyze and confirm what parts of our data can be used and what cannot;
- -
- Analyze: This is a fundamental part of the assessment process. In this step, we analyze the results we got from the previous steps. In addition, this phase helps us to identify the reasons behind the different data errors, which is essential for the improvement process;
- -
- Improve: This prioritizes the wrong data and starts by developing a plan to improve and correct these parts of the data. Thus, TDQM is a methodology that focuses both on data quality assessment and data improvement [42].
- From the OURA: To collect data (measuring), we distributed sample rings to students living in KTH LIL apartments. The students wore their rings for the agreed-on period. The measurement was taken entirely by using the ring’s sensors, and they were not manually manipulated.
- From SE sensors: This data is automatically measured by the different sensors placed inside the KTH Live-in-Lab buildings.
- Approved: This indicates that the data passed the dimension according to the established definition.
- Rejected: This indicates that the data did not pass the test, and it must be modified if the parameter is to be used in the modeling stage.
- NA: this means that not enough information was found for assessing the dimensions, but it is OK to proceed with using this data without any further improvements.
- Sleep Score: OURA states on their website that the sleep score is calculated based on many parameters, including your resting heart rate (RHR), heart rate variability (HRV), body temperature, respiratory rate, and movement. These parameters are directly measured from the three sensors that the company has installed on the ring. As this metric is OURA specific, we do not have actual data to compare its accuracy with, but in comparing the accuracy of the other parameters that the ring manufacturer uses for calculating this parameter, we found that RHR and HRV are 99.6% and 98% accurate [43].
- Temperature: This parameter is measured by a SE sensor that is installed inside the KTH LiL buildings, and according to SE, all their sensors provide accurate measurements up to +0.2/−0.2 degrees. So, the temperature is considered accurate [44].
- Activity: There is no defined measure for activity to assess whether it is accurate or not, however the approach that OURA uses is to take data from the 3D accelerometer which seems a common approach to measure activity. This sensor is considered a reliable tool for measuring different activity related parameters, and that is because it delivers accurate results [45].
- Readiness: This parameter measures how well your overall health is, and how prepared you are for the day following. OURA also calculates the readiness of a person based on data from the sensors such as the RHR and HRV, as proven before. Since those parameters are accurate enough, we could also consider the readiness to be accurate enough for this project [46].
- Restfulness: It is a measure of how soundly you slept through the night. Wakeups, excessive movement, and getting up from bed during the night will all take away from your overall restfulness. However, in this simple definition of restfulness, we cannot approve this parameter since any small hand move, in-bed rotation can decrease this score and thus give a misleading result [49].
- Sleep Latency: This parameter is defined to be the amount of time it took a person to fall asleep after they went to bed, according to OURA the optimal time for a person to fall asleep is 10–20 min, if a person falls asleep in less than 5 min, this can indicate that the person is over tired, and if the person struggles to sleep within 20 min, it indicates that this person is having some anxiety. However, OURA does not provide any information about the accuracy of this parameter, so it is not assessed.
- Total Burn: This parameter refers to the total number of calories burned throughout the day, OURA does not provide enough information about the accuracy of this parameter, but they claim it to be accurate enough, or slightly bounced if the person did not wear the ring when exercising. In an experiment that was performed to compare different wearables, OURA was the most consistent wearable device in the activity measuring [50].
- Total Sleep Time: OURA analyzes your sleep by measuring the dynamics of your resting heart rate, body temperature, movement. Again, we cannot determine the accuracy of sleep time since we have no access to the algorithm, and we think that there were no actual tests performed to test the accuracy of the algorithm [51].
4.3. Modelling
5. Results
5.1. Data Quality Assessment Results
5.2. Sleep Quality and Built Environment Parameters
5.3. Modelling Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jia, M.; Komeily, A.; Wang, Y.; Srinivasan, R. Adopting Internet of Things for the development of smart buildings: A review of enabling technologies and applications. Autom. Constr. 2019, 101, 111–126. [Google Scholar] [CrossRef]
- Hillier, B. Space Is the Machine; Space Syntax: London, UK, 2007. [Google Scholar]
- Shen, L.; Hoye, M.; Nelson, C.; Edwards, J. Human-Building Interaction (HBI): A User-Centered Approach to Energy Efficiency Innovations. In Proceedings of the 19th ACEEE Conference on Energy Efficiency in Buildings, Pacific Grove, CA, USA, 21–26 August 2016; Center for Energy and Environment: Minneapolis, MN, USA, 2016. [Google Scholar]
- Alavi, H.; Churchill, E.; Kirk, D.; Nembrini, J.; Lalanne, D.; Moncur, W. Future of Human-Building Interaction. In Proceedings of the 2016 Conference on Human Factors in Computing Systems, San Jose, CA, USA, 7–12 May 2016; pp. 3408–3414. [Google Scholar]
- Elena, M.; Lundqvist, P. End-user activities context information management framework for sustainable building operation. J. Phys. Conf. Ser. 2019, 1343, 012151. [Google Scholar]
- Lan, L.; Pan, L.; Lian, Z.; Huang, H.; Lin, Y. Experimental study on thermal comfort of sleeping people at different air temperatures. Build. Environ. 2013, 73, 24–31. [Google Scholar] [CrossRef]
- Tsang, T.W.; Mui, K.W.; Wong, L.T. Investigation of thermal comfort in sleeping environment and its association with sleep quality. Build. Environ. 2021, 187, 107406. [Google Scholar] [CrossRef]
- Zhang, B.; Wing, Y.K. Sex differences in insomnia: A meta-analysis. Sleep 2006, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Okamoto-Mizuno, K.; Mizuno, K. Effects of thermal environment on sleep and circadian rhythm. J. Physiol. Anthropol. 2012, 31, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.G.; Benca, R.M. Sleep and biological rhythms. In Handbook of Psychology, Behavioral Neuroscience; Weiner, I.N., Sheri, R.J.M., Eds.; Wiley Publish: Somerset, NJ, USA, 2012; Chapter 13; pp. 365–394. [Google Scholar]
- Carskadon, M.A.; Dement, W.C. Normal human sleep: An overview. In Principles and Practice of Sleep Medicine, 5th ed.; Kryger, M.H., Roth, T., Demen, W.C., Eds.; Elsevier Inc.: Philadelphia, PA, USA, 2011; pp. 16–26. [Google Scholar]
- Weitzman, E.D.; Czeisler, C.A.; Zimmerman, J.C.; Ronda, J.M. Timing of REM and stages 3 + 4 sleep during temporal isolation in man. Sleep 1980, 2, 391–407. [Google Scholar] [PubMed]
- VanSomeren, E.J.W. More than a marker: Interaction between the circadian regulation of temperature and sleep, age-related changes, and treatment possibilities. Chronobiol Int. 2000, 17, 313–354. [Google Scholar] [CrossRef]
- Miller, M.A.; Cappuccio, F.P. Biomarkers of cardiovascular risk in sleep-deprived people. J. Hum. Hypertens. 2013, 27, 583–588. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagai, M.; Hoshide, S.; Kario, K. Sleep duration as a risk factor for cardiovascular disease-a review of the recent literature. Curr. Cardiol. Rev. 2010, 6, 54–61. [Google Scholar] [CrossRef]
- De Zambotti, M.; Cellini, N.; Goldstone, A.; Colrain, I.M.; Baker, F.C. Wearable sleep technology in clinical and research settings. Med. Sci. Sport. Exerc. 2019, 51, 1538. [Google Scholar] [CrossRef] [PubMed]
- Depner, C.M.; Cheng, P.C.; Devine, J.K.; Khosla, S.; de Zambotti, M.; Robillard, R.; Vakulin, A.; Drummond, S.P. Wearable technologies for developing sleep and circadian biomarkers: A summary of workshop discussions. Sleep 2020, 43, zsz254. [Google Scholar] [CrossRef] [Green Version]
- Shelgikar, A.V.; Anderson, P.F.; Stephens, M.R. Sleep tracking, wearable technology, and opportunities for research and clinical care. Chest 2016, 150, 732–743. [Google Scholar] [CrossRef]
- Berryhill, S.; Morton, C.J.; Dean, A.; Berryhill, A.; Provencio-Dean, N.; Patel, S.I.; Estep, L.; Combs, D.; Mashaqi, S.; Gerald, L.B.; et al. Effect of wearables on sleep in healthy individuals: A randomized crossover trial and validation study. J. Clin. Sleep Med. 2020, 16, 775–783. [Google Scholar] [CrossRef]
- Liu, S.; Schiavon, S.; Das, H.P.; Jin, M.; Spanos, C.J. Personal thermal comfort models with wearable sensors. Build. Environ. 2019, 162, 106281. [Google Scholar] [CrossRef] [Green Version]
- Abdallah, M.; Clevenger, C.; Vu, T.; Nguyen, A. Sensing occupant comfort using wearable technologies. In Proceedings of the 2016 Construction Research Congress, San Juan, Puerto Rico, 31 May–2 June 2016; American Society of Civil Engineers: Reston, VA, USA, 2016; pp. 940–950. [Google Scholar]
- Alsaleem, F.; Tesfay, M.K.; Rafaie, M.; Sinkar, K.; Besarla, D.; Arunasalam, P. An IoT framework for modeling and controlling thermal comfort in buildings. Front. Built Environ. 2020, 6, 87. [Google Scholar] [CrossRef]
- Sugimoto, C. Human sensing using wearable wireless sensors for smart environments. In Proceedings of the 7th International Conference on Sensor Technologies and Applications, Barcelona, Spain, 25–31 August 2013; ICST: Saitama, Japan, 2013; pp. 188–192. [Google Scholar]
- Jeff, C.-C.; Huang, R.Y.; Newman, M.W. The potential and challenges of inferring thermal comfort at home using commodity sensors. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Osaka, Japan, 7–11 September 2015; ACM: New York, NY, USA, 2015; pp. 1089–1100. [Google Scholar]
- Ghahramani, A.; Castro, G.; Becerik-Gerber, B.; Yu, X. Infrared thermography of human face for monitoring thermoregulation performance and estimating personal thermal comfort. Build. Environ. 2016, 109, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Nkurikiyeyezu, K.N.; Suzuki, Y.; Tobe, Y.; Lopez, G.F.; Itao, K. Heart rate variability as an indicator of thermal comfort state. In Proceedings of the 56th Annual Conference of the Society of Instrument and Control Engineers of Japan, Kanazawa, Japan, 19–22 September 2017; pp. 1510–1512. [Google Scholar]
- Li, D.; Menassa, C.C.; Kamat, V. Personalized human comfort in indoor building environments under diverse conditioning modes. Build. Environ. 2017, 126, 304–317. [Google Scholar] [CrossRef]
- Kim, J.; Zhou, Y.; Schiavon, S.; Raftery, P.; Brager, G. Personal comfort models: Predicting individuals’ thermal preference using occupant heating and cooling behavior and machine learning. Build. Environ. 2018, 129, 96–106. [Google Scholar] [CrossRef] [Green Version]
- Akane, S.; Phillips, A.J.; Amy, Z.Y.; McHill, A.W.; Taylor, S.; Jaques, N.; Czeisler, C.A.; Klerman, B.E.; Picard, R.W. Recognizing academic performance, sleep quality, stress level, and mental health using personality traits, wearable sensors and mobile phones. In Proceedings of the IEEE 12th International Conference on Wearable and Implantable Body Sensor Networks (BSN), Cambridge, MA, USA, 9–12 July 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 1–6. [Google Scholar]
- Bunde, A.; Havlin, S.; Kantelhardt, J.W.; Penzel, T.; Peter, J.-H.; Voigt, K. Correlated and Uncorrelated Regions in Heart-Rate Fluctuations during Sleep. Phys. Rev. Lett. 2000, 85, 3736–3739. [Google Scholar] [CrossRef] [Green Version]
- Snyder, F.; Hobson, J.A.; Morrison, D.F.; Goldfrank, F. Changes in respiration, heart rate, and systolic blood pressure in human sleep. J. Appl. Physiol. 1964, 19, 417–422. [Google Scholar] [CrossRef]
- Kräuchi, K. How is the circadian rhythm of core body temperature regulated? Clin. Auton. Res. 2002, 12, 147–149. [Google Scholar] [CrossRef]
- de Arriba-Pérez, F.; Caeiro-Rodríguez, M.; Santos-Gago, J.M. How do you sleep? Using off the shelf wrist wearables to estimate sleep quality, sleepiness level, chronotype and sleep regularity indicators. J. Ambient. Intell. Humaniz. Comput. 2018, 9, 897–917. [Google Scholar] [CrossRef]
- Sadeh, A.; Mindell, J.A.; Luedtke, K.; Wiegand, B. Sleep and sleep ecology in the first 3 years: A web-based study. J. Sleep Res. 2009, 18, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Sadeh, A. The role and validity of actigraphy in sleep medicine: An update. Sleep Med. Rev. 2011, 15, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.fitbit.com/global/se/home (accessed on 20 September 2021).
- Available online: https://news.microsoft.com/uploads/2016/01/Band-Fact-Sheet.pdf (accessed on 20 September 2021).
- Chaudhry, B.M. Sleeping with an Android. mHealth 2017, 3, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altini, M.; Hannu, K. The Promise of Sleep: A Multi-Sensor Approach for Accurate Sleep Stage Detection Using the Oura Ring. Sensors 2021, 21, 4302. [Google Scholar] [CrossRef]
- Zambotti, M.; Rosas, L.; Colrain, I.M.; Baker, F.C. The sleep of the ring: Comparison of the ŌURA sleep tracker against polysomnography. Behav. Sleep Med. 2019, 17, 124–136. [Google Scholar] [CrossRef]
- GitHub. 2021. Available online: beamandrew/deep_learning_works (accessed on 20 September 2021).
- Francisco, M.M.C.; Alves-Souza, S.N.; Campos, E.G.L.; De Souza, L.S. Total data quality management and total information quality management applied to costumer relationship management. In Proceedings of the 9th International Conference on Information Management and Engineering, Barcelona, Spain, 9–11 October 2017. [Google Scholar]
- Team, O. Your Oura Temperature—The Pulse Blog. 2021. Available online: https://ouraring.com/blog/your-body-temperature-and-oura/ (accessed on 20 September 2021).
- Team, O. Your Oura Activity Score—The Pulse Blog. 2021. Available online: https://ouraring.com/blog/activity-score/ (accessed on 20 September 2021).
- Oura Help. Readiness Scores—The Pulse Blog. 2021. Available online: https://ouraring.com/blog/readiness-score/ (accessed on 20 September 2021).
- Oura Help. A Guide to Restfullness. 2020. Available online: https://support.ouraring.com/hc/en-us/articles/360057792293-A-Guide-to-Your-Sleep-Contributors (accessed on 20 September 2021).
- Lan, L.; Lian, Z. Ten questions concerning thermal environment and sleep quality. Build. Environ. 2016, 99, 252–259. [Google Scholar] [CrossRef]
- SHD100/SHD101 Duct Humidity Sensor with Temperature. 2020. Available online: https://www.se.com/ww/en/download/document/003-00109/ (accessed on 20 September 2021).
- Oura Help. Active Calorie Burn vs. Total Burn. 2020. Available online: https://support.ouraring.com/hc/en-us/articles/360025430914-Active-Calorie-Burn-vs-Total-Burn (accessed on 20 September 2021).
- Oura Help. An Introduction to Your Sleep Score. 2021. Available online: https://support.ouraring.com/hc/en-us/articles/360025445574-An-Introduction-to-Your-Sleep-Score (accessed on 20 September 2021).
- Fogliaroni, P.; D’Antonio, F.; Clementini, E. Data trustworthiness and user reputation as indicators of VGI quality. Geo. Spat. Inf. Sci. 2018, 21, 213–233. [Google Scholar] [CrossRef] [Green Version]
- Friedland, G.; Kerll, M. A Capacity Scaling Law for Artificial Neural Networks. arXiv 2018, arXiv:1708.06019. Available online: https://arxiv.org/abs/1708.06019 (accessed on 20 September 2021).
- Abu-Mostafa, Y. Hints. Neural Comput. 1995, 7, 639–671. [Google Scholar] [CrossRef]
- Baum, E.; Haussler, D. What Size Net Gives Valid Generalization? Neural Comput. 1989, 1, 151–160. [Google Scholar] [CrossRef]
- Hervé, B.; Goodrich, M.T. Almost optimal set covers in finite VC-dimension. Discret. Comput. Geom. 1995, 14, 463–479. [Google Scholar]
- Marvuglia; Antonino; Messineo, A.; Nicolosi, G. Coupling a neural network temperature predictor and a fuzzy logic controller to perform thermal comfort regulation in an office building. Build. Environ. 2014, 72, 287–299. [Google Scholar] [CrossRef]
- Beklemysheva, A. Why Use Python for AI and Machine Learning? 2021. Available online: https://steelkiwi.com/blog/python-for-ai-and-machine-learning/ (accessed on 20 September 2021).
- Ortiz-Rodríguez, J.M.; del Rosario Martínez-Blanco, M.; Viramontes, J.M.C.; Vega-Carrillo, H.R. Robust Design of Artificial Neural Networks Methodology in Neutron Spectrometry. In Artificial Neural Networks Architectures and Applications; IntechOpen: London, UK, 2013. [Google Scholar]
- Brownlee, J. A Gentle Introduction to the Rectified Linear Unit (ReLU). 2019. Available online: https://machinelearningmastery.com/rectified-linear-activation-function-for-deep-learning-neural-networks/ (accessed on 20 September 2021).
- Brownlee, J. How to Choose Loss Functions When Training Deep Learning Neural Networks. 2019. Available online: https://machinelearningmastery.com/how-to-choose-loss-functions-when-training-deep-learning-neural-networks/ (accessed on 20 September 2021).
- Kingma, D.P.; Ba, J. Adam: A Method for Stochastic Optimization. In Proceedings of the 3rd International Conference for Learning Representations, San Diego, CA, USA, 7–9 May 2015. [Google Scholar]
- Brownlee, J. Gentle Introduction to the Adam Optimization Algorithm for Deep Learning. 2017. Available online: https://machinelearningmastery.com/adam-optimization-algorithm-for-deep-learning/ (accessed on 20 September 2021).
- Afaq, S.; Rao, S. Significance Of Epochs On Training A Neural Network. Int. J. Sci. Technol. Res. 2020, 19, 485–488. [Google Scholar]
- Kandel, I.; Castelli, M. The effect of batch size on the generalizability of the convolutional neural networks on a histopathology dataset. ICT Express 2020, 6, 312–315. [Google Scholar] [CrossRef]
- Uhs.uga.edu. University Health Center, Managing Stress, Sleep. 2021. Available online: https://healthcenter.uga.edu/bewelluga-and-learn-about-managing-stress-sleep/ (accessed on 20 September 2021).











Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malakhatka, E.; Al Rahis, A.; Osman, O.; Lundqvist, P. Monitoring and Predicting Occupant’s Sleep Quality by Using Wearable Device OURA Ring and Smart Building Sensors Data (Living Laboratory Case Study). Buildings 2021, 11, 459. https://doi.org/10.3390/buildings11100459
Malakhatka E, Al Rahis A, Osman O, Lundqvist P. Monitoring and Predicting Occupant’s Sleep Quality by Using Wearable Device OURA Ring and Smart Building Sensors Data (Living Laboratory Case Study). Buildings. 2021; 11(10):459. https://doi.org/10.3390/buildings11100459
Chicago/Turabian StyleMalakhatka, Elena, Anas Al Rahis, Osman Osman, and Per Lundqvist. 2021. "Monitoring and Predicting Occupant’s Sleep Quality by Using Wearable Device OURA Ring and Smart Building Sensors Data (Living Laboratory Case Study)" Buildings 11, no. 10: 459. https://doi.org/10.3390/buildings11100459
APA StyleMalakhatka, E., Al Rahis, A., Osman, O., & Lundqvist, P. (2021). Monitoring and Predicting Occupant’s Sleep Quality by Using Wearable Device OURA Ring and Smart Building Sensors Data (Living Laboratory Case Study). Buildings, 11(10), 459. https://doi.org/10.3390/buildings11100459





