The Role of Resilience in Reducing Burnout: A Study with Healthcare Workers during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Theoretical Background
2.1. Burnout
2.2. Resilience as a Personal Resource
3. Method
3.1. Participants
3.2. Sample Description
3.3. Measures
3.4. Statistical Analysis
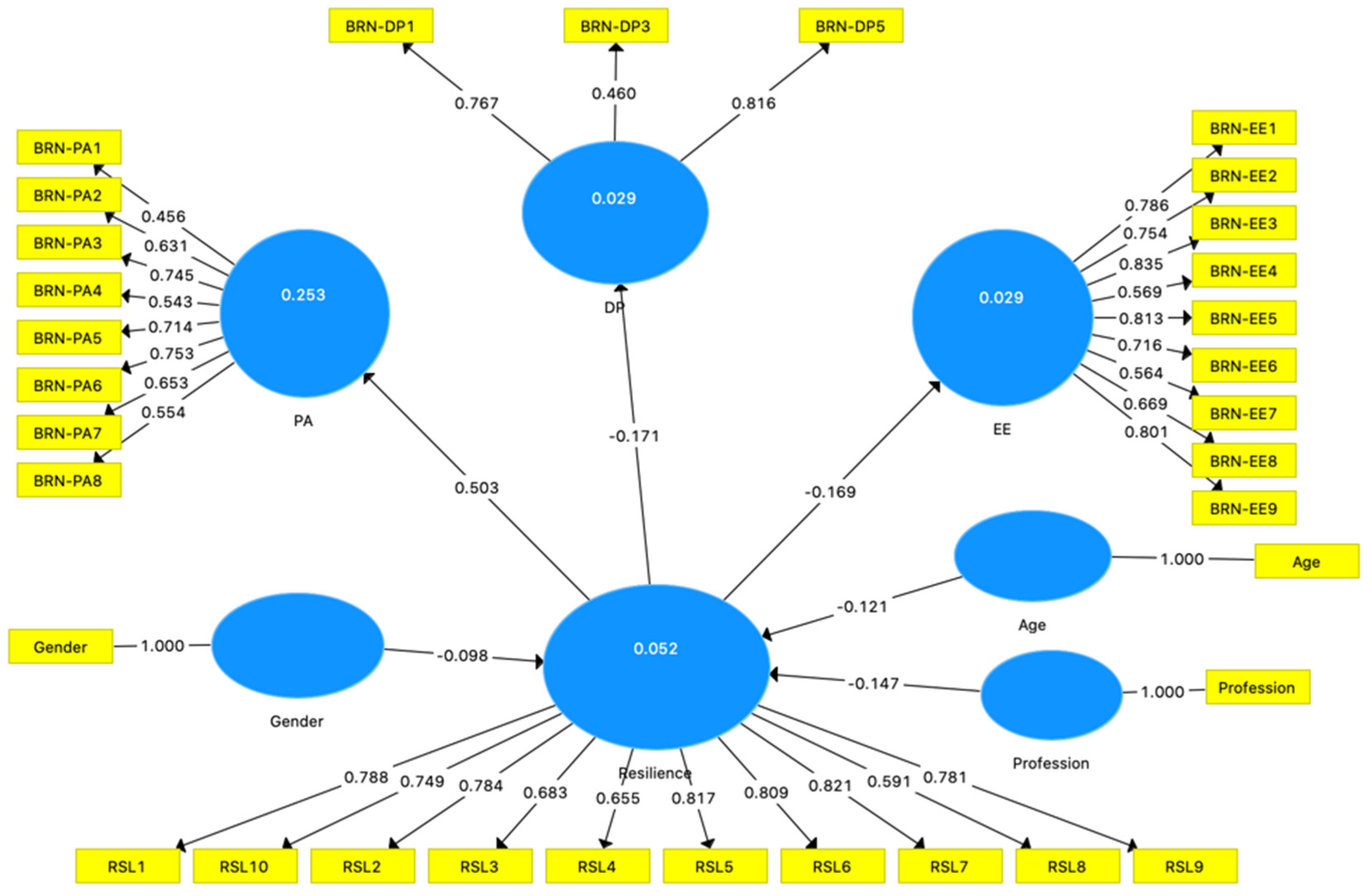
4. Results
5. Discussion
6. Practice Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Andries, Jan, Yvan Heyden, and Lutgarde Buydens. 2017. Improved variable reduction in partial least squares modelling by Global-Minimum Error Uninformative-Variable Elimination. Analytica Chimica Acta 982: 37–47. [Google Scholar] [CrossRef] [PubMed]
- Arrogante, Oscar, and Eva Aparício-Zaldivar. 2017. Burnout and health among critical care professionals: The mediational role of resilience. Intensive and Critical Care Nursing 42: 110–15. [Google Scholar] [CrossRef] [PubMed]
- Bakker, Arnold, and Juriena De Vries. 2021. Job Demands–Resources theory and self-regulation: New explanations and remedies for job burnout. Anxiety, Stress and Coping 34: 1–21. [Google Scholar] [CrossRef] [PubMed]
- Bakker, Arnold, and Evangelia Demerouti. 2007. The Job Demands-Resources model: State of the art. Journal of Managerial Psychology 22: 309–28. [Google Scholar] [CrossRef] [Green Version]
- Bakker, Arnold, and Evangelia Demerouti. 2017. Job demands-resources theory: Taking stock and looking forward. Journal of Occupational Health Psychology 22: 273–85. [Google Scholar] [CrossRef] [PubMed]
- Bakker, Arnold, Evangelia Demerouti, and Martin Euwema. 2005. Job Resources Buffer the Impact of Job Demands on Burnout. Journal of Occupational Health Psychology 10: 170–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batra, Kavita, Tejinder Pal Singh, Manoj Sharma, Ravi Batra, and Nena Schvaneveldt. 2020. Investigating the Psychological Impact of COVID-19 among Healthcare Workers: A Meta-Analysis. International Journal of Environmental Research and Public Health 17: 9096. [Google Scholar] [CrossRef] [PubMed]
- Britt, Thomas W., Marisa L. Shuffler, Riley Pegram, Phoebe Xoxakos, Patrick Rosopa, Emily Hirsh, and William Jackson. 2021. Job demands and resources among healthcare professionals during virus pandemics: A review and examination of fluctuations in mental health strain during COVID-19. Applied Psychology 70: 120–49. [Google Scholar] [CrossRef]
- Buck, Katherine, Meridith Williamson, Stacy Ogbeide, and Bethany Norberg. 2019. Family physician burnout and resilience: A cross-sectional analysis. Family Medicine 51: 657–63. [Google Scholar] [CrossRef] [Green Version]
- Busch, Isolde M., Francesca Moretti, Mariangela Mazzi, Albert W. Wu, and Michela Rimondini. 2021. What We Have Learned from Two Decades of Epidemics and Pandemics: A Systematic Review and Meta-Analysis of the Psychological Burden of Frontline Healthcare Workers. Psychotherapy and Psychosomatics 90: 1–13. [Google Scholar] [CrossRef]
- Campbell-Sills, Laura, and Murray B. Stein. 2007. Psychometric analysis and refinement of the conor–davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress. Official Publication of The International Society for Traumatic Stress Studies 20: 1019–28. [Google Scholar] [CrossRef] [PubMed]
- Contreras, Francoise, Juan C. Espinosa, and Gustavo A. Esguerra. 2020. Could Personal Resources Influence Work Engagement and Burnout? A Study in a Group of Nursing Staff. SAGE Open 10: 2158244019900563. [Google Scholar] [CrossRef] [Green Version]
- De Brier, Niels, Stijn Stroobants, Philippe Vandekerckhove, and Emmy De Buck. 2020. Factors affecting mental health of health care workers during coronavirus disease outbreaks (SARS, MERS and COVID-19): A rapid systematic review. PLoS ONE 15: e0244052. [Google Scholar] [CrossRef] [PubMed]
- Di Monte, Cinzia, Silvia Monaco, Rachele Mariani, and Michela Di Trani. 2020. From Resilience to Burnout: Psychological features of Italian General Practitioners during COVID-19 emergency. Frontiers in Psychology 11: 2476. [Google Scholar] [CrossRef]
- Duarte, Ivone, Andreia Teixeira, Luísa Castro, Sílvia Marina, Carla Ribeiro, Cristina Jácome, Vera Martins, Inês Ribeiro-Vaz, Hugo Celso Pinheiro, Andreia Rodrigues Silva, and et al. 2020. Burnout among Portuguese healthcare workers during the COVID-19 pandemic. BMC Public Health 20: 1885. [Google Scholar] [CrossRef] [PubMed]
- Earvolino-Ramirez, Marie. 2007. Resilience: A concept analysis. Nursing Forum 42: 73–82. [Google Scholar] [CrossRef]
- General Health Directorate. 2021. Estado Epidemiológico COVID19 Portugal (Epidemiological Status COVID19 Portugal. Available online: https://covid19estamoson.gov.pt/estado-epidemiologico-covid19-portugal/ (accessed on 1 April 2021).
- Grover, Steven L., Stephen T. T. Teo, David Pick, Maree Roche, and Cameron J. Newton. 2018. Psychological capital as a personal resource in the JD-R model. Personnel Review 47: 968–84. [Google Scholar] [CrossRef]
- Hair, Joseph F., Jeffrey J. Risher, Marko Sarstedt, and Christian M. Ringle. 2019. When to use and how to report the results of PLS-SEM. European Business Review 31: 2–24. [Google Scholar] [CrossRef]
- Hobfoll, Stevan E. 2002. Social and psychological resources and adaptation. Review of General Psychology 6: 307–24. [Google Scholar] [CrossRef]
- Huang, Jie, Yansong Wang, and Xuqun You. 2016. The Job Demands-Resources Model and Job Burnout: The Mediating Role of Personal Resources. Current Psychology 35: 562–69. [Google Scholar] [CrossRef]
- Janssen, Elias, Isabeau Van Strydonck, Anouk Decuypere, Adelien Decramer, and Mieke Audenaert. 2020. How to foster nurses’ well-being and performance in the face of work pressure? The role of mindfulness as personal resource. Journal of Advanced Nursing 76: 3495–505. [Google Scholar] [CrossRef]
- Jose, Sinu, Manju Dhandapani, and Maneesha C. Cyriac. 2020. Burnout and Resilience among Frontline Nurses during COVID-19 Pandemic: A Cross-sectional Study in the Emergency Department of a Tertiary Care Center, North India. Indian Journal of Critical Care Medicine 24: 1081–88. [Google Scholar] [CrossRef] [PubMed]
- Kalisch, Raffael, Marianne B. Müller, and Oliver Tüscher. 2015. A conceptual framework for the neurobiological study of resilience. Behavioral and Brain Sciences 38: e92. [Google Scholar] [CrossRef]
- Kim, Son Chae, Carlota Quiban, Christine Sloan, and Anna Montejano. 2021. Predictors of poor mental health among nurses during COVID-19 pandemic. Nursing Open 8: 900–7. [Google Scholar] [CrossRef] [PubMed]
- Maslach, Christina, and Susan E. Jackson. 1981. The measurement of experienced burnout. Journal of Organizational Behavior 2: 99–113. [Google Scholar] [CrossRef]
- McBride, Orla, Jamie Murphy, Mark Shevlin, Jilly Gibson-Mille, Todd K Hartman, Philip Hyland, Liat Levita, Liam Mason, Anton P. Martinez, Ryan McKay, and et al. 2021. Monitoring the psychological, social, and economic impact of the COVID-19 pandemic in the population: Context, design and conduct of the longitudinal COVID-19 psychological research consortium (C19PRC) study. International Journal of Methods in Psychiatric Research 30: e1861. [Google Scholar] [CrossRef]
- Nikam, Vinayak, Jhajhria Abimanyu, and Pal Suresh. 2019. Quantitative Methods for Social Sciences. New Delhi: NIAP, ISBN 978-81-940080-2-6. [Google Scholar]
- Orrù, Graziella, Francesca Marzetti, Ciro Conversano, Guido Vagheggini, Mario Miccoli, Rebecca Ciacchini, Eugenia Panait, and Angelo Gemignani. 2021. Secondary Traumatic Stress and Burnout in Healthcare Workers during COVID-19 Outbreak. International Journal of Environmental Research and Public Health 18: 337. [Google Scholar] [CrossRef]
- Pereira, Sandra de Sousa, Joana Fornés-Vives, Sara Guadalupe Unda-Rojas, Gerson Alves Pereira-Junior, Mario Francisco Juruena, and Lucilene Cardoso. 2021. Confirmatory factorial analysis of the Maslach Burnout Inventory–Human Services Survey in health professionals in emergency services. Revista Latino-Americana de Enfermagem 29: e3386. [Google Scholar] [CrossRef]
- Purvis, Taylor E., and Deanna Saylor. 2019. Burnout and Resilience among Neurosciences Critical Care Unit Staff. Neurocritical Care 31: 406–10. [Google Scholar] [CrossRef]
- Ringle, Christian M., Marko Sarstedt, Rebecca Mitchell, and Siegfried P. Gudergan. 2019. Partial least squares structural equation modeling in HRM research. The International Journal of Human Resource Management 31: 1617–43. [Google Scholar] [CrossRef]
- Ritchey, Ferris. 2008. The Statistical Imagination: Elementary Statistics for the Social Sciences, 2nd ed. New York: McGraw-Hill. [Google Scholar]
- Schaufeli, Wilmar B., and Tonn W. Taris. 2014. A critical review of the job demands-resources model: Implications for improving work and health. In Bridging Occupational, Organizational and Public Health: A Transdisciplinary Approach. Edited by Georg F. Bauer and Oliver Hämmig. Berlin: Springer Science + Business Media, pp. 43–68. [Google Scholar] [CrossRef]
- Schaufeli, Wilmar B., Michael P. Leiter, and Christina Maslach. 2009. Burnout: 35 years of research and practice. Career Development International 14: 204–220. [Google Scholar] [CrossRef] [Green Version]
- Seo, Yae Eun, Hyun Chung Kim, So Young Yoo, Kang Uk Lee, Hae Woo Lee, and So Hee Lee. 2020. Factors Associated with Burnout among Healthcare Workers during an Outbreak of MERS. Psychiatry Investigation 17: 674–80. [Google Scholar] [CrossRef]
- Shepherd, C. David, Armen Tashchian, and Rick E. Ridnour. 2011. An Investigation of the Job Burnout Syndrome in Personal Selling. Journal of Personal Selling and Sales Management 31: 397–409. [Google Scholar] [CrossRef]
- Wang, Cindy, Pamela Grassau, Peter G. Lawlor, Colleen Webber, Shirley H. Bush, Bruno Gagnon, Monisha Kabir, and Edward G. Spilg. 2020. Burnout and resilience among Canadian palliative care physicians. BMC Palliative Care 19: 169. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. 2020. WHO Director-General’s Statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) (accessed on 1 April 2021).
- Xanthopoulou, Despoina, Arnold B. Bakker, Evangelia Demerouti, and Wilmar B. Schaufeli. 2007. The role of personal resources in the job demands-resources model. International Journal of Stress Management 14: 121–41. [Google Scholar] [CrossRef] [Green Version]
- Yildirim, Murat, and Fatma Solmaz. 2020. COVID-19 burnout, COVID-19 stress and resilience: Initial psychometric properties of COVID-19 Burnout Scale. Death Studies, 1–9. [Google Scholar] [CrossRef]
- Zito, Margherita, Frederica Emanuel, Monica Molino, Claudio Giovanni Cortese, Chiara Ghislieri, and Lara Colombo. 2018. Turnover intentions in a call center: The role of emotional dissonance, job resources, and job satisfaction. PLoS ONE 13: e0192126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Age | DP | EE | Gender | PA | Profession | Resilience | |
|---|---|---|---|---|---|---|---|
| Cronbach’s Alpha | 1.00 | 0.71 | 0.90 | 1.00 | 0.79 | 1.00 | 0.91 |
| Composite Reliability | 1.00 | 0.73 | 0.91 | 1.00 | 0.84 | 1.00 | 0.93 |
| Average | 1.00 | 0.49 | 0.53 | 1.00 | 0.51 | 1.00 | 0.57 |
| Variance Extracted (AVE) | |||||||
| Fornell-Lacker Criterion | |||||||
| Age | 1.00 | ||||||
| DP | −0.06 | 0.70 | |||||
| EE | −0.09 | 0.58 | 0.73 | ||||
| Gender | −0.12 | −0.02 | 0.24 | 1.00 | |||
| PA | 0.03 | −0.24 | −0.20 | −0.14 | 0.64 | ||
| Profession | −0.08 | 0.06 | 0.11 | 0.42 | −0.19 | 1.00 | |
| Resilience | −0.10 | −0.17 | −0.17 | −0.15 | 0.50 | −0.18 | 0.75 |
| % | |
|---|---|
| Gender | |
| Female | 77.0 |
| Male | 23.0 |
| Age (years) | |
| <30 | 31.7 |
| 31–40 | 31.6 |
| 41–50 | 17.3 |
| 51–60 | 17.9 |
| >60 | 1.50 |
| Profession | |
| Healthcare Assistants | 2.6 |
| Nurses | 73.0 |
| Physicians | 24.5 |
| Have children | |
| No | 46.9 |
| Yes | 53.1 |
| Work Experience (years) | |
| <5 | 31.1 |
| 6–10 | 27.0 |
| 11–20 | 13.3 |
| >20 | 28.6 |
| Weekly working hours (in the last 6 months) (mean) | 47.6 |
| Participants (n) | 196 |
| Burnout Dimensions | Mean ± SD, f (%) |
|---|---|
| Emotional Exhaustion (EE) | 28.44 ± 8.83 |
| Low (0–16) | 21 (10.7%) |
| Moderate (17–26) | 61 (31.1%) |
| High (27–54) | 114 (58.2%) |
| Depersonalization (DP) | 11.11 ± 4.78 |
| Low (0–6) | 32 (16.3%) |
| Moderate (7–12) | 98 (50%) |
| High (13–30) | 66 (33.7%) |
| Reduced personal accomplishment (PA) | 30.32 ± 6.36 |
| Low (>39) | 17 (8.7%) |
| Moderate (32–38) | 72 (36.7%) |
| High (0–31) | 107 (54.6%) |
| Original Sample (O) | Sample Mean (M) | Standard Deviation (STDEV) | T Statistics (|O/STDEV|) | 95% Confidence Interval (CI) | p Values | |
|---|---|---|---|---|---|---|
| Age -> Resilience | −0.12 | −0.12 | 0.07 | 1.75 | (−0.25, 0.01) | 0.08 * |
| Gender -> Resilience | −0.09 | −0.10 | 0.08 | 1.25 | (−0.24, 0.04) | 0.21 |
| Profession -> Resilience | −0.15 | −0.15 | 0.07 | 2.23 | (−0.27, −0.03) | 0.03 ** |
| Resilience -> DP | −0.17 | −0.19 | 0.07 | 2.34 | (−0.31, −0.03) | 0.02 ** |
| Resilience -> EE | −0.17 | −0.20 | 0.10 | 1.67 | (−0.38, 0.04) | 0.09 * |
| Resilience -> PA | 0.50 | 0.52 | 0.06 | 8.76 | (0.40, 0.61) | 0.00 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira, P.; Gomes, S. The Role of Resilience in Reducing Burnout: A Study with Healthcare Workers during the COVID-19 Pandemic. Soc. Sci. 2021, 10, 317. https://doi.org/10.3390/socsci10090317
Ferreira P, Gomes S. The Role of Resilience in Reducing Burnout: A Study with Healthcare Workers during the COVID-19 Pandemic. Social Sciences. 2021; 10(9):317. https://doi.org/10.3390/socsci10090317
Chicago/Turabian StyleFerreira, Pedro, and Sofia Gomes. 2021. "The Role of Resilience in Reducing Burnout: A Study with Healthcare Workers during the COVID-19 Pandemic" Social Sciences 10, no. 9: 317. https://doi.org/10.3390/socsci10090317
APA StyleFerreira, P., & Gomes, S. (2021). The Role of Resilience in Reducing Burnout: A Study with Healthcare Workers during the COVID-19 Pandemic. Social Sciences, 10(9), 317. https://doi.org/10.3390/socsci10090317







