Abstract
This study aimed to assess health literacy (HL), preventive behaviors (PBs), and the factors associated with PBs toward COVID-19 among village health volunteers (VHVs) and residents in urban and rural areas in the upper south of Thailand. A cross-sectional study was conducted using valid questionnaires administered using an online platform. Data were analyzed using descriptive statistics, t-tests, and binary logistic regression analysis. A total of 846 people participated in this study, and 62.8% of participants had an adequate level of HL. Furthermore, 55.0% of participants had an adequate level of PBs. Among VHVs, PB levels were adequate, whereas among residents, they were inadequate. Moreover, among VHVs, underlying diseases (adjusted odds ratio (OR): 1.77, 95% CI: 1.13–2.76), access to HL (adjusted OR: 4.28, 95% CI: 1.42–12.88), appraisal of HL (adjusted OR: 3.09, 95% CI: 1.90–5.02), and application of HL (adjusted OR: 2.51, 95% CI: 1.52–4.12) were associated with COVID-19 PB. Additionally, among residents, only marital status (adjusted OR: 1.59, 95% CI: 1.04–2.44), appraisal of HL (adjusted OR: 1.78, 95% CI: 1.18–2.84), and application of HL (adjusted OR: 3.85, 95% CI: 2.39–6.20) were associated with PBs towards COVID-19. Furthermore, individuals with inadequate HL demonstrated noteworthy significance in all dimensions of PBs. To prioritize and optimize preventive programs aimed at enhancing PBs, the government must take proactive initiatives in implementing robust health communication strategies across diverse media platforms, both in the present and future.
1. Introduction
The novel coronavirus disease (COVID-19) emerged in Wuhan, China’s Hubei Province in December 2019 (Wang et al. 2020) and rapidly spread worldwide. It is a highly contagious disease primarily transmitted through saliva droplets or nasal discharge when infected individuals cough or sneeze. The World Health Organization (WHO) declared COVID-19 an international public health emergency (Eurosurveillance Editorial Team 2020). In Thailand, the first wave occurred in late March 2020, with nightclubs and boxing arenas serving as primary sources of infection (United Nations 2020). The second wave lasted from mid-December 2020 to late February 2021, mainly affecting Myanmar migrant workers in Samut Sakhon province near Bangkok, some of whom had crossed the border without undergoing quarantine. Subsequent waves, caused by the Alpha and Delta variants, led to significant transmission and the implementation of lockdown policies and vaccination campaigns (Uansri et al. 2021; Reuters 2021). The fifth wave emerged in December 2021 with the Omicron variant, posing concerns for the Thai healthcare system (Tangcharoensathien et al. 2022). From the records, COVID-19 in Thailand was mainly found in the southern part (World Health Organization (WHO) 2021), which was the source of its spread. South Thailand serves as the focal point for numerous facets of this nation and is one of the world’s most popular tourist destinations for foreign visitors to Thailand. Moreover, foreigners typically visit the south of Thailand because of the available tourist attractions. Moreover, a wide array of international and local flights is provided to accessible and pleasant locations (Vicerra 2021; Tantrakarnapa et al. 2020). In this study conducted during the 4th and 5th waves of COVID-19 in Thailand (November to December 2021), we examined the impact of health information and behavior adaptation during a pandemic. While the rapid spread of misinformation through social media platforms poses a serious challenge to public health (Zarocostas 2020), strict measures were enforced by central and local governments, as well as community partnerships, to control the spread of the disease (Prem et al. 2020).
Amidst the rapid evolution of COVID-19 and the urgent need for individuals to adopt healthy practices and make informed decisions, health literacy (HL) emerges as a critical factor. HL encompasses the essential abilities to access, understand, evaluate, and utilize health-related information, enabling individuals to effectively navigate the complexities of their health conditions (Nutbeam and Lloyd 2021). With the ongoing COVID-19 pandemic exposing the prevalence of false and misleading information, the significance of HL becomes even more pronounced. Distinguishing between accurate and deceptive information about COVID-19 is crucial for individuals to protect their health and that of others. Furthermore, HL serves as a valuable tool for navigating the vast array of medical data and services. The recognition of the dynamic nature of COVID-19 has highlighted two notable trends: the crucial involvement of HL in preventing both infectious and noncommunicable diseases, and the essential need for individuals and systems to be prepared in dealing with complex real-world challenges (Paakkari and Okan 2020). To conduct a comprehensive study on HL, it is crucial to acknowledge and incorporate the specific definition being utilized, taking a holistic perspective that encompasses various dimensions and instruments of HL (Bergman et al. 2023). However, the emergence of biased data, deceptive information, and false claims during the COVID-19 pandemic highlights the susceptibility to misinformation and the need for careful assessment (Capodici et al. 2022; Zhang et al. 2022).
This research is driven by the urgent needs and unique challenges faced by village health volunteers (VHVs) and residents in urban and rural areas. VHVs have played a significant role in Thailand’s healthcare system for the past two decades, providing nationwide coverage. They are recruited and trained to support health workers in delivering essential healthcare services and education within their communities. Currently, there are 1.05 million VHVs across the country (Sirilak et al. 2020). Their efforts align with Thailand’s National Primary Healthcare program, which aims to extend healthcare access at reduced costs (Bhutta et al. 2010). During the COVID-19 pandemic, VHVs made pivotal contributions in containing infections through door-to-door educational campaigns on COVID-19 symptoms and screenings of residents. They also shared COVID-19-related information with the provincial health office and mobilized to prevent and control the epidemic (Marome and Shaw 2021; United Nations 2020).
Moreover, understanding the HL needs of residents in urban and rural areas is crucial for addressing the challenges faced by these communities. Urban areas offer many unique opportunities, although densely populated areas increase health risks. By 2050, more than two-thirds of the world’s population will live in urban areas (Ritchie and Roser 2018). While rural residents benefited from a network of VHVs serving as a community resource for information throughout the COVID-19 pandemic, they also faced challenges accessing more modern media sources, particularly the internet, for the most recent COVID-19 developments (Vicerra 2021). In addition, regarding rural–urban health disparities, living in an urban area is not a risk factor for lower HL, which has important implications (Aljassim and Ostini 2020). Enhancing their HL is of utmost importance as it equips VHVs with the necessary knowledge and skills to effectively disseminate accurate information and promote healthy practices, thus safeguarding the overall wellbeing of community members. Empowering VHVs with HL competencies and promoting HL among residents are fundamental steps towards fostering the development of proactive, healthier, and more resilient communities.
Nevertheless, little is known about the association between health literacy and preventive behavior. Furthermore, research on VHVs’ and their residents’ health literacy and preventive behaviors, especially in urban and rural areas, is limited. This research aimed to (1) evaluate the health literacy and preventive behaviors of VHVs and residents and (2) investigate the factors associated with preventive behaviors towards COVID-19 among VHVs and residents in urban and rural areas in upper south Thailand.
2. Materials and Methods
2.1. Study Design and Setting
A cross-sectional study was conducted in upper south Thailand after obtaining approval from the Institutional Review Board of the Human Research Ethics Committee of Walailak University. Data were collected from November to December 2021 during the fourth wave (the Delta variant) and the fifth wave in December (the Omicron variant) of the COVID-19 outbreak. An internet-based data collection mode utilizing the Google platform was employed, as per governmental directives, due to the continued emphasis on safety protocols. The participants were VHVs and residents in upper southern Thailand, including Nakhon Si Thammarat (NST) and Surat Thani (SRT) provinces. To be eligible for this study, VHVs had to (1) be 18 years or older, have been VHVs for at least 6 months, have been living in a rural or urban area for more than 6 months, and be literate in the Thai language while residents had to (2) be 18 years or older, have lived in the rural or urban area more than 6 months, and be literate in the Thai language.
Rural–Urban residence—Rural–urban residence was defined based on the population size. Urban areas are defined as all areas with at least 10,000 persons (Town–City Municipal). Rural areas: all areas not defined as urban (Subdistrict–Municipal or Tambon (in Thai)).
2.2. Sample Size Determination and Sampling
The data were obtained from the VHVs and residents. The sample size was calculated according to Thrusfield (Thrusfield 2007) by considering 50% (P) as the proportion of people with high health literacy, 95% confidence interval (CI) (Z = 1.96), and 5% absolute error (d). The estimated sample size was 384 participants in each group (we used a 1:1 ratio of VHVs to residents), and we added an extra 10% to account for potential attrition, yielding a minimum sample size of 423 in each group. The total number of participants was 846.
A cluster sampling method was used, and randomly selected communities were asked to complete the collection form. Of the seven provinces in upper south Thailand, two provinces were randomly selected for first-stage sampling (Nakhon Si Thammarat; NST and Surat Thani; SRT). A total of 846 participants from one urban area and 1 rural area of 3 selected districts in each province, thus totaling 6 urban and 6 rural areas, were chosen randomly for 2nd-stage sampling.
The participants for this study were selected using a random sampling process. In the initial stage, a total of six urban and six rural areas were chosen, totaling twelve health-promoting hospitals’ (HPHs’) representation from every subdistrict or Tambon (in Thai), where HPHs are located. Within each HPH, a random draw method was utilized, ensuring that VHVs were selected without replacement. Approximately 35–36 participants were chosen from the list of VHVs in each HPH, representing the VHVs involved in the study. Moving on to the 2nd stage, VHVs randomly selected 1–2 residents from the households they were responsible for. However, it is important to note that in some areas, VHVs did not select residents from the households they were assigned to (Figure 1).
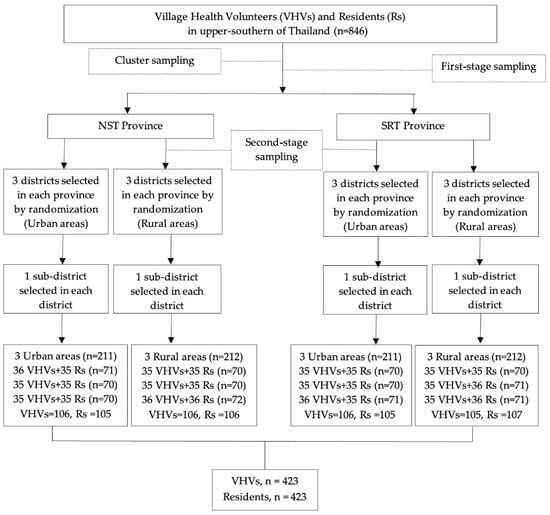
Figure 1.
Flowchart of included study participants.
2.3. Data Collection and Measurements
Research Measurements
Data were collected using self-reported online questionnaires administered to VHVs and residents in upper southern Thailand. The participants are typically contacted, and data is collected from online questionnaires through collaboration with community health center or officers from health-promoting hospitals (HPHs) in each area, who can help reach the target groups. Once participants are contacted using these methods, they are directed to an online questionnaire platform (Google Forms) where they can provide their responses. A panel of 5 experts rated the overall content validity of all instruments, and the index of item objective congruence (IOC) yielded a value of 0.91 for content validity.
The structured questionnaires comprised the three parts described below:
(1) Ten items measured the sociodemographic characteristics, including current province, area of residence (urban or rural), gender, age, religion, education, marital status, employment, income, and underlying diseases of community residents. VHVs answered the same ten items plus additional items assessing the duration of volunteering, COVID-19 training in the last six months, and the number of households served.
(2) The Office of the Honorable Commission, Department of Disease Control, Ministry of Public Health, Thailand, developed health literacy (HL). This instrument is a validated tool that has been used in other studies focusing on health literacy (Ministry of Public Health of Thailand 2021), and we applied this tool by incorporating key message and skills related to preventive measures against COVID-19. Specifically, we focused on D-M-H-T-T, which stands for the following measures: D for social distancing; M for mask wearing; H for hand washing; T for temperature check; and T for the Thai Chana contact tracing application. The aim was to prevent the spread of COVID-19 in Thailand (Department of Disease Control of Thailand 2021). It comprises 36 items assessing the following 4 elements: access, understanding, appraisal, and application. The access dimension includes 10 items, with the ‘can access information’ response being assigned 1 point and the ‘cannot access information’ response assigned 0 points. The understanding dimension contains nine items, appraisal dimension contains seven items, and the applied dimension comprises ten items. The responses were measured on a 4-point Likert scale: very low = 1, low = 2, more = 3, and most = 4. The maximum score of health literacy was 114 points, with a cutoff score of 80% of the maximum score (≥92 points), meaning the subjects had adequate health literacy. The Cronbach’s alpha was 0.89.
(3) Preventive behavior towards COVID-19 refers to preventive practice guidelines that the WHO and the Ministry of Public Health of Thailand (MOPH) recommended to reduce the spread of COVID-19. The questionnaire consisted of 2 sections comprising 29 items. The first part assessed risk preventive behavior with nine items. The 2nd part assessed preventive behavior with 20 items (indoor and outdoor preventive behavior, 14 and 6 items, respectively). Each item was measured on a 5-point rating scale ranging from 0 to 4 points (never, rarely, sometimes, often, and always). The total score ranged from 0 to 116 points. The maximum score of preventive behavior was 116 points, with a cutoff score of 80% of the maximum score (≥93 points), meaning the subjects had adequate preventive behavior. The Cronbach’s alpha was 0.93.
2.4. Data Analysis
Data were analyzed using the Statistical Package for the Social Sciences version 28.0 (SPSS Inc., Chicago, IL, USA). The data are presented as the frequency, percentage, mean, and standard deviation (SD). Binary logistic regression analysis was performed to examine the association between dependent and independent variables. Preventive behavior, respondent characteristics, and health literacy were coded as 1 and 0. All factors were entered into multiple logistic regression analyses. Adjusted odds ratios with 95% confidence intervals (CI) were calculated to show the strength of the association. Statistical significance was set at p-value < 0.05.
3. Results
3.1. Sociodemographic Characteristics of Study Participants
The online survey conducted with 846 participants, including 423 VHVs and 423 residents from rural and urban areas of upper southern Thailand, revealed significant differences. For VHVs, the average age of the VHVs in urban and rural areas was found to be significantly different, with the average age in the former being 51.36 (SD = 13.09) and the latter 47.75 (SD = 10.37). The majority of the VHVs in urban areas engaged in Buddhism (95.8%), whereas the majority of those in rural areas worked in agriculture (49.8%). Over the previous six months, the COVID-19 training score averaged 2.21 (SD = 1.95) while in urban areas it was 1.64 (SD = 1.87). For residents, Residents from urban and rural areas differed significantly in terms of gender, with the majority of participants in rural areas being female (50.8%), while most of participants in urban areas had a bachelor’s degree or higher (35.7%), were business owners (42.4%), and had no underlying diseases (74.8%) (Table 1).

Table 1.
Demographic characteristics of study participants (n = 846).
3.2. Health Literacy on COVID-19
For each health literacy dimension, namely access, application, appraisal, and understanding, VHVs and residents scored relatively high on HL. VHVs achieved a higher mean score of 96.35, while residents scored 94.65. These scores indicate adequate HL levels for both groups, which included individuals living in both urban and rural areas. In addition, VHVs and residents differed significantly in the dimensions of access, application, and overall HL (Table 2). Furthermore, VHV groups had the most favorable scores, scoring the highest on the access dimension among the four dimensions assessed and lowest on the understanding dimension [Figure 2a].

Table 2.
The mean and standard deviation of health literacy among the participants.
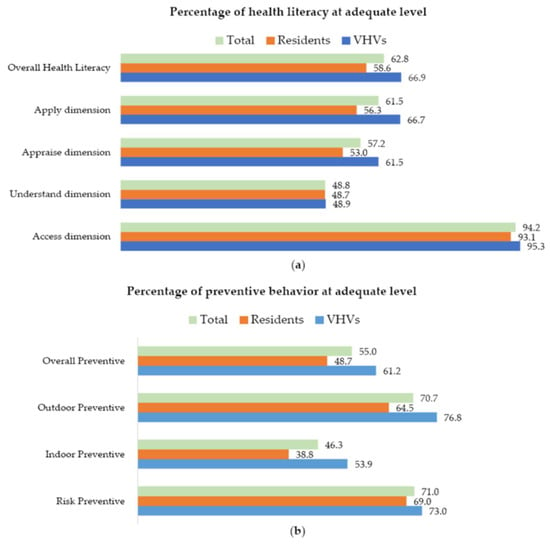
Figure 2.
(a) Percentage of health literacy at adequate level. (b) Percentage of preventive behavior at adequate level.
3.3. Preventive Behaviors Regarding COVID-19
For each preventative dimension, namely outdoor PBs, risk PBs, and indoor PBs, scores were relatively high for both VHVs and residents. Notably, there was a significant difference in risk PBs between VHVs from urban and rural areas. Additionally, for residents, significant differences were observed in indoor PBs and overall PBs between urban and rural areas. Overall, the PB scores obtained for both VHVs and residents were deemed inadequate, with a mean score of 91.06, VHVs scoring a higher mean score of 94.08, while residents scored lower with a mean score of 88.04. These findings suggest that VHVs demonstrated adequate levels of health literacy in relation to PB, encompassing both urban and rural areas. However, residents, including those residing in urban and rural areas, exhibited inadequate PB levels (Table 3). Furthermore, among the three dimensions evaluated, the outdoor PBs dimension garnered the highest scores. Conversely, the indoor PBs dimension received comparatively lower scores [Figure 2b].

Table 3.
The mean and standard deviation of preventive behaviors among the participants.
3.4. Factors Related to Preventive Behaviors Regarding COVID-19
The bivariate and multivariate logistic regression analysis results for VHVs, preventive behaviors (PBs) related to the duration of volunteering of VHVs, VHVs who had adequate PBs (≥93 points) were adequate scores, 10 years or more of volunteering than those who had less than ≤10 years. Also, VHVs who had adequate PBs were more likely to have higher scores and be responsible for more than 10 households, in contrast to those who were responsible for 10 households or fewer. Moreover, PBs affected all dimension of HL; VHVs who had adequate PBs were more likely to have an adequate score of access HL than those who had an inadequate score of access HL. VHVs who had PBs were more likely to have adequate scores on understanding HL than those who had inadequate scores on understanding HL. VHVs who had adequate PBs were more likely to have adequate scores on appraisal HL than those who had inadequate scores on appraisal HL. VHVs who had adequate PBs were more likely to have adequate scores on application HL than those who had inadequate scores on application HL. Nevertheless, PBs did not show the relationship to gender, age, religion, education, marital status, employment, income, underlying diseases, and training in COVID-19 (Table 4).

Table 4.
Relationship between sociodemographic and health and with the levels of preventive behavior regarding the COVID-19 situation among VHVs.
For residents, preventive behaviors (PBs) affected three dimensions of HL; people who had adequate PBs were more likely to have adequate scores on understanding HL than those who had inadequate scores on understanding HL. People who had adequate PBs were more likely to have adequate scores on appraise HL than those who had inadequate scores on appraise HL. People who had adequate PBs were more likely to have adequate scores on apply HL than those who had inadequate scores on apply HL. Nevertheless, PBs did not show a relationship to all demographic characteristics and access dimensions of HL (Table 5).

Table 5.
Relationship between sociodemographic and health literacy and the levels of preventive behavior regarding the COVID-19 situation among residents.
3.5. Factors Associated with Preventive Behaviors Regarding COVID-19
Table 4 and Table 5 show the logistic regression analysis results for PBs during the COVID-19 pandemic. For VHVs, participants with underlying diseases were almost two times more likely to have adequate PBs than those without the disease (adjusted OR: 1.77, 95% CI: 1.13–2.76). Those with adequate access to HL were more than four times as likely to have adequate PBs as those with inadequate access (adjusted OR: 4.28, 95% CI: 1.42–12.88). Moreover, more than three times as many VHVs with adequate HL appraisal (adjusted OR: 3.09, 95% CI: 1.90–5.02) had adequate PBs. In addition, those who adequately applied HL were more than twice as likely to have adequate PBs (adjusted OR: 2.51, 95% CI: 1.52–4.12).
Among residents, those who were married were 1.59 times more likely to have adequate PBs than those who were unmarried (adjusted OR: 1.59, 95% CI: 1.04–2.44). Furthermore, those who adequately appraised their health literacy were 2.78 times more likely to possess the adequate PBs compared to those who had inadequate health literacy (adjusted OR: 2.78, 95% CI: 1.75–4.47). Moreover, participants who adequately applied HL were almost four times more likely to have adequate PBs than those who applied HL inadequately (adjusted OR: 3.85, 95% CI: 2.39–6.20).
4. Discussion
This study was conducted to evaluate HL, PBs, and the factors associated with PBs toward COVID-19 among VHVs and residents in urban and rural areas in the upper south of Thailand. The analysis revealed noteworthy results regarding overall HL in both VHVs, and residents in urban and rural areas, indicating that they had adequate overall HL scores. Furthermore, VHVs in both urban and rural areas demonstrated adequate PB scores. In contrast, residents, including those residing in urban and rural areas, displayed inadequate levels of PBs, particularly in indoor PBs. The outcomes highlighted significant contributing factors to adequate PBs of underlying diseases, access to HL, appraisal of HL, and application of HL, among VHVs. For residents, marital status, appraisal of HL, and application of HL were found to be associated with adequate PBs towards COVID-19.
4.1. Health Literacy Regarding COVID-19
Based on our findings, 62.8% of participants had adequate overall HL scores (66.9% in VHVs and 58.6% in residents), indicating that HL was adequate in both urban and rural areas of upper southern Thailand. Silva and Santos’ study in Portugal and Jiang’s cross-sectional investigation in China reported similar conclusions (Silva and Santos 2021; Jiang 2020). However, using different instruments (HLS-COVID-Q22) and cutoff scores (Okan’s cutoff scale was 66% for adequate HL, whereas our cutoff scale was 80%), Okan et al. (2020) showed that 50% of adult Germans had inadequate levels of HL. The results of our study also indicated that a significant portion of individuals, specifically 37.2%, had inadequate total HL scores. This study emphasizes the urgent need for greater HL levels in urban and rural regions of upper southern Thailand. It is imperative to address this issue to help individuals understand health-related information, enabling them to make informed decisions and ultimately improve health outcomes.
VHVs and residents in this study demonstrated a considerable gap in their ability to access and use HL. Compared to the residents, VHVs were more likely to seek information about COVID-19. Although VHVs tend to have higher HL than the general population, Visanuyothin et al. (2015) underlined the importance of advocating for laws that would improve the HL of VHVs.
4.2. Preventive Behaviors Regarding COVID-19
Based on our results, 55.0% of participants had adequate overall PB scores (61.2% in VHVs and 48.7% in residents), indicating that VHVs exhibited adequate while residents exhibited inadequate PBs. Experiencing the three waves, along with several government policies, such as work from home and lockdown policy, and the WHO’s and local government’s efforts, increased awareness of the COVID-19 outbreak in Thailand and health literacy. Especially in the first wave, VHVs in Thailand responded effectively to the COVID-19 pandemic, focusing on primary health care and multisectoral collaboration. The transmission of impactful health messages was facilitated using the key success factors of primary healthcare, resulting in active collaboration between both health and non-health sectors at the local level that helped individuals and community members live under a ‘new normal’. Passive collaboration involved screening, treatment, and follow-up of patients, whereas active collaboration encompassed health promotion activities (Tejativaddhana et al. 2020).
According to our results, indoor PBs (when you are together with others in the house, always wear a mask, open the windows and doors of the house for ventilation, and socially distance from a family member) (46.3%) were lower than outdoor PBs (70.7%). These results are similar to those reported in a previous study conducted in China (Ye et al. 2021). Indoor preventive behaviors could have been easily overlooked for various reasons. More attention was paid to boosting immunity through exercise and nutritional intake, but the effects of these efforts were not immediately noticeable (Moghadam et al. 2021). Additionally, VHVs and residents differed significantly in indoor and outdoor PBs. Specifically, residents engaged in fewer adequate indoor and outdoor PBs (38.8% and 64.5%, respectively) compared to VHVs (53.9% and 76.8%, respectively). The results also showed that VHVs had higher HL overall; therefore, they could promote the adoption of PBs among residents. Visanuyothin et al. reported similar findings in their study conducted in Thailand (Visanuyothin et al. 2015). Furthermore, the cross-sectional investigation conducted by Qian et al. in China revealed that COVID-19 transmission occurred predominantly indoors in almost all of the outbreaks, except for one, where three or more cases were reported to have been transmitted within an enclosed environment. Additionally, the study revealed a considerable likelihood of subsequent infections among the family members of symptomatic patients, with an approximate rate of 25% (Qian et al. 2021). In addition, VHVs should help the public identify PBs to promote residents’ daily hand washing, social distancing, mask wearing, and preventive measures in the wake of the COVID-19 pandemic.
Comparing the urban and rural areas, they did not differ in dimensions of HL, although we found a significant difference in risk PBs between urban and rural areas among VHVs, with rural VHVs reporting lower risk PB scores compared to their urban counterparts. One explanation could be that most COVID-19 prevention-related media have focused on densely populated, large metropolitan areas rather than the specific requirements of rural VHVs. Additionally, we found a significant difference in residents’ indoor and overall PB scores between urban and rural areas among residents, with urban residents reporting lower risk PB scores than their rural counterparts. One explanation for this difference could be that rural community members have stronger relations with local VHVs than urban residents. Furthermore, VHVs provided information during the outbreak to the community network that benefited rural residents, which was consistent with the finding of a previous study (Capodici et al. 2022). However, the PB difference in the area of residency between rural and urban did not affect PBs towards COVID-19, which is consistent with Chen’s cross-sectional study in China, which produced comparable findings (Chen and Chen 2020).
4.3. Factors Associated with Preventive Behaviors Regarding COVID-19
According to these results, the duration of volunteering and the number of households served influenced COVID-19 preventive behaviors among VHVs. HL and dimensions of access, understanding, appraisal, and application, significantly influenced COVID-19 PBs among VHVs and residents (except for access to HL). A higher HL level was associated with a higher COVID-19 PB score level, consistent with previous studies’ findings (Silva and Santos 2021; Uchibori et al. 2022). This might be because, in our study, 65.5% of VHVs had greater experience of more than 10 years, and 62.9% of the VHVs who served more than 10 households had adequate PBs. Moreover, 72.8% and 61.7% of VHVs and residents, respectively, had an adequate overall HL. This study indicated that VHVs might adopt PBs to reduce the spread of COVID-19 to their residents in the living areas (urban and rural) they served. Overall, participants had positive odds ratios, and this might be because, in our study, 65.5% of VHVs had more than 10 years of experience in adequate PBs compared to inadequate preventive behaviors. In addition, the experience of VHVs was the most significant influence on preventive behaviors. A higher duration of volunteering was associated with higher COVID-19 preventive behaviors, which is aligned with the previous study’s finding (Nakayama et al. 2022).
Our analysis discovered significant connections between underlying diseases and the dimensions of access, appraisal, and application of HL. These associations were observed in relation to individuals’ active participation in proactive risk-taking and their adherence to PBs indoors and outdoors. These findings were observed among both urban and rural VHVs. It should be noted that people with underlying medical conditions were more likely to seek information and medical advice because they might be at higher risk for severe illness from COVID-19 than those with no disease if they risk exposure to the virus or suspect infection (CDC COVID-19 Response Team 2020). Furthermore, marital status was an important social factor. Appraisal and application HL dimensions were associated with positive prevention in urban and rural residents. Our findings suggest that marriage had a protective effect because married people have greater family and health behavior support (Mao et al. 2021).
Furthermore, married participants who engaged in indoor PBs generally had greater levels of PB than unmarried people. Some married participants with children may spend much time at home or engage less in leisure activities due to obligations associated with working from home, housekeeping, and family activities. They were cautious about engaging in activities as inadequate indoor ventilation may heighten the chances of being infected by COVID-19, which would increase the health risk for their families. Our findings confirmed that marriage positively affected the adoption of preventive behaviors during the COVID-19 pandemic.
It is worth noting that both VHVs and residents with adequate appraisal and application HL dimensions were more likely to prevent and control COVID-19 than people with inadequate HL, consistent with a previous study that reported better HL is associated with better preventive strategies against COVID-19 (Naveed and Shaukat 2022). A Greater understanding, appreciation, and application of HL can support policy action at all levels, individual, community, and population, during a pandemic (Silva and Santos 2021; Sentell et al. 2020).
Additionally, Taiwan demonstrated strong, effective state–society relations characterized by transparency, communication, and collaboration (Yen 2020). In addition, at the onset of the most transmissible Delta variant and the fourth wave in June 2021, lockdown measures were implemented in Greater Bangkok (Bangkok and five affiliated provinces) and other regions with an increased number of incidents (also in the southern area, including areas in this study). The Thai government declared that termination of the action (DMHTT—distancing, mask wearing, hand washing, temperature testing—was implemented for prevention, whereas the Thai Cha Na mobile application was for tracing people at risk of the disease) relied on continually evaluating the situation since the city lockdown had no specific time limit. This may have increased VHVs’ and residents’ willingness to adopt preventive behaviors against COVID-19.
4.4. Study Strengths and Limitations
To our knowledge, this study is the first to examine related factors and dimensions of HL associated with behavior prevention from the perspectives of VHVs and residents in both urban and rural areas. Despite this strength, it had some limitations. First, the study used self-reported instruments to measure HL and PB variables. Some participants likely exaggerated or understated their status. This may have led to information bias. Second, no causal inferences or conclusions can be drawn from the results because the analyses were based on cross-sectional data. Third, this study was only conducted in the upper south of Thailand, and the results may not be generalizable to other parts of Thailand. Fourth, respondents who regularly used all preventive behavioral activities were classified as adequate if they scored 80% and above and inadequate if they scored less than 80%. However, this classification did not mean that respondents with adequate scores in this study were at lower risk, as COVID-19 requires full and regular implementation of preventive activities. Fifth, we used the same proportion of VHVs and residents in our sampling, so the lack of sample weighting may have introduced bias in our analysis. Finally, this study did not determine the extent of contact or the quantity of information that residents received from VHVs. Comparing residents who had extensive access to information and those who did not would have been highly valuable in elucidating the effect of VHVs on residents’ HL. Therefore, future research should examine the influence of VHVs and the variations in scores based on inadequate residents’ information exposure to provide valuable insights in this regard.
5. Conclusions
Our study examined the adequate level of HL and PBs among both VHVs and residents; however, only residents’ PB levels were inadequate. As VHVs are an important mechanism of the primary care system, preventive behavior for residents should be expedited via VHVs or directly to residents. Additionally, this study showed that better health literacy is associated with better PBs towards COVID-19. These results help raise the general awareness of citizens and decision-makers about HL and empower the entire population to have more control over the prevention of COVID-19 and its spread, leading to better health outcomes. From a community and public health standpoint, it is crucial to prioritize preventive programs aimed at enhancing HL. Additionally, the government should take the initiative to establish health communication strategies to efficiently communicate information on public health through diverse media channels. Consequently, understanding the effects of information sources on PB becomes vital for managing new outbreaks of infectious diseases in the future. Further research should be undertaken to understand HL dimensions and social media’s effects on preventative actions.
Author Contributions
W.S.N.A. designed and planned the study, collected the data, analyzed and interpreted the data, drafted and approved the final version of the manuscript; C.T. and P.W. planned the study, collected the data, analyzed and interpreted the data, supervised the research, drafted and approved the final version of the manuscript; S.L., P.L. and R.F. collected the data, analyzed and interpreted the data, drafted and approved the final version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Research Institute for Health Sciences at Walailak University grant number WU-IRG-64-061.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved from Review Board of the Human Research Ethics Committee of Walailak University (WUEC-21-225-01; 19 December 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Data available on request from the authors.
Acknowledgments
The authors would like to thank Walailak University’s School of Public Health for their generous assistance. We express our gratitude to the Committees of the Excellent Centre for Dengue and Community Public Health (E.C. for DACH) for their support. Thank you also to the officers at the health-promoting hospitals, to all who participated in this study in upper southern Thailand for assisting with data collection, and to the Research Institute for Health Sciences at Walailak University for funding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CI | Confidence intervals. |
| COVID-19 | Coronavirus disease 2019. |
| HPHs | Health-promoting hospitals. |
| HL | Health literacy. |
| PBs | Preventive behaviors. |
| SD | Standard deviation. |
| VHVs | Village health volunteers. |
References
- Aljassim, Noor, and Remo Ostini. 2020. Health literacy in rural and urban populations: A systematic review. Patient Education and Counseling 103: 2142–54. [Google Scholar] [CrossRef] [PubMed]
- Bergman, Lina, Ulrica Nilsson, Karuna Dahlberg, Maria Jaensson, and Josefin Wångdahl. 2023. Validity and reliability of the arabic version of the HLS-EU-Q16 and HLS-EU-Q6 questionnaires. BMC Public Health 23: 304. [Google Scholar] [CrossRef] [PubMed]
- Bhutta, Zulfiqar A., Zohra S. Lassi, George Pariyo, and Luis Huicho. 2010. Global experience of community health workers for delivery of health related millennium development goals: A systematic review, country case studies, and recommendations for integration into national health systems. Global Health Workforce Alliance 1: 61. [Google Scholar]
- Capodici, Angelo, Aurelia Salussolia, Francesco Sanmarchi, Davide Gori, and Davide Golinelli. 2022. Biased, wrong and counterfeited evidences published during the COVID-19 pandemic, a systematic review of retracted COVID-19 papers. Qual Quant, 1–33. [Google Scholar] [CrossRef] [PubMed]
- CDC COVID-19 Response Team. 2020. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, 12 February–16 March 2020. Morbidity and Mortality Weekly Report 69: 343–46. [Google Scholar] [CrossRef]
- Chen, Xuewei, and Hongliang Chen. 2020. Differences in Preventive Behaviors of COVID-19 between Urban and Rural Residents: Lessons Learned from A Cross-Sectional Study in China. International Journal of Environmental Research and Public Health 17: 4437. [Google Scholar] [CrossRef]
- Department of Disease Control of Thailand. 2021. Measures of D-M-H-T-T. Available online: https://ddc.moph.go.th/brc/news.php?news=16434&deptcode=brc (accessed on 7 June 2023). (In Thai).
- Eurosurveillance Editorial Team. 2020. Note from the editors: World Health Organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveillance: Bulletin Europeen sur les Maladies Transmissibles = European Communicable Disease Bulletin 25: 200131e. [Google Scholar] [CrossRef]
- Jiang, Ruichen. 2020. Knowledge, attitudes and mental health of university students during the COVID-19 pandemic in China. Children and Youth Services Review 119: 105494. [Google Scholar] [CrossRef]
- Mao, Yimeng, Hao Chen, Yi Wang, Suhong Chen, Junling Gao, Junming Dai, Yingnan Jia, Qianyi Xiao, Pinpin Zheng, and Hua Fu. 2021. How can the uptake of preventive behaviour during the COVID-19 outbreak be improved? An online survey of 4827 Chinese residents. BMJ Open 11: e042954. [Google Scholar] [CrossRef]
- Marome, Wijitbusaba, and Rajib Shaw. 2021. COVID-19 response in Thailand and its implications on future preparedness. International Journal of Environmental Research and Public Health 18: 1089. [Google Scholar] [CrossRef]
- Ministry of Public Health of Thailand. 2021. Developing Health Literacy Assessment Guidelines and Measures for Disease Prevention and Control. Available online: https://ddc.moph.go.th/uploads/files/1706220210215050906.pdf (accessed on 5 June 2023). (In Thai).
- Moghadam, Majid Taati, Behzad Taati, Seyed Mojtaba Paydar Ardakani, and Katsuhiko Suzuki. 2021. Ramadan fasting during the COVID-19 pandemic; observance of health, nutrition and exercise criteria for improving the immune system. Frontiers in Nutrition 7: 570235. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, Kazuhiro, Yuki Yonekura, Hitomi Danya, and Kanako Hagiwara. 2022. COVID-19 Preventive Behaviors and Health Literacy, Information Evaluation, and Decision-making Skills in Japanese Adults: Cross-sectional Survey Study. JMIR Formative Research 6: e34966. [Google Scholar] [CrossRef] [PubMed]
- Naveed, Muhammad Asif, and Rozeen Shaukat. 2022. Health literacy predicts COVID-19 awareness and protective behaviours of university students. Health Information & Libraries Journal 39: 46–58. [Google Scholar] [CrossRef]
- Nutbeam, Don, and Jane E. Lloyd. 2021. Understanding and Responding to Health Literacy as a Social Determinant of Health. Annual Review of Public Health 42: 159–73. [Google Scholar] [CrossRef] [PubMed]
- Okan, Orkan, Torsten Michael Bollweg, Eva-Maria Berens, Klaus Hurrelmann, Ullrich Bauer, and Doris Schaeffer. 2020. Coronavirus-Related Health Literacy: A Cross-Sectional Study in Adults during the COVID-19 Infodemic in Germany. International Journal of Environmental Research and Public Health 17: 5503. [Google Scholar] [CrossRef]
- Paakkari, Leena, and Orkan Okan. 2020. COVID-19: Health literacy is an underestimated problem. The Lancet Public Health 5: e249–e250. [Google Scholar] [CrossRef]
- Prem, Kiesha, Yang Liu, Timothy W. Russell, Adam J. Kucharski, Rosalind M. Eggo, Nicholas Davies, Stefan Flasche, Samuel Clifford, Carl A. B. Pearson, and James D. Munday. 2020. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. The Lancet Public Health 5: e261–e270. [Google Scholar] [CrossRef]
- Qian, Hua, Te Miao, Li Liu, Xiaohong Zheng, Danting Luo, and Yuguo Li. 2021. Indoor transmission of SARS-CoV-2. Indoor Air 31: 639–45. [Google Scholar] [CrossRef]
- Reuters. 2021. Reuters, Thailand Aims to Vaccinate 70% of People by September. Bangkok, Thailand. Available online: https://www.reuters.com/business/healthcare-pharmaceuticals/thailand-aims-vaccinate-70-people-by-september-2021-05-19/ (accessed on 24 August 2022).
- Ritchie, Hannah, and Max Roser. 2018. Urbanization. Available online: https://ourworldindata.org/urbanization (accessed on 13 January 2023).
- Sentell, Tetine, Sandra Vamos, and Orkan Okan. 2020. Interdisciplinary Perspectives on Health Literacy Research Around the World: More Important Than Ever in a Time of COVID-19. International Journal of Environmental Research and Public Health 17: 3010. [Google Scholar] [CrossRef]
- Silva, Maria João, and Paulo Santos. 2021. The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: A cross-sectional study. International Journal of Environmental Research and Public Health 18: 5421. [Google Scholar] [CrossRef]
- Sirilak, Supakit, Sopon Iamsirithaworn, Soawapak Hinjoy, Noppavan Janejai, Suriwan Thaiprayoon, and Ratchakorn Keawpramkusol. 2020. Thailand’s Experience in the COVID-19 Response. Bangkok: Ministry of Public Health of Thailand. Available online: https://ddc.moph.go.th/viralpneumonia/eng/file/pub_doc/LDoc9.pdf (accessed on 24 August 2022).
- Tangcharoensathien, Viroj, Saranya Sachdev, Shaheda Viriyathorn, Kriddhiya Sriprasert, Lalitaya Kongkam, Kanchana Srichomphu, and Walaiporn Patcharanarumol. 2022. Universal access to comprehensive COVID-19 services for everyone in Thailand. BMJ Global Health 7: e009281. [Google Scholar] [CrossRef] [PubMed]
- Tantrakarnapa, Kraichat, Bhophkrit Bhopdhornangkul, and Kanchana Nakhaapakorn. 2020. Influencing factors of COVID-19 spreading: A case study of Thailand. Journal of Public Health 30: 621–27. [Google Scholar] [CrossRef] [PubMed]
- Tejativaddhana, Phudit, Wichukorn Suriyawongpaisal, Vijj Kasemsup, and Thunwadee Suksaroj. 2020. The roles of village health volunteers: COVID-19 prevention and control in Thailand. Asia Pacific Journal of Health Management 15: 18–22. [Google Scholar] [CrossRef]
- Thrusfield, Michael. 2007. Veterinary Epidemiology. Oxford: Blackwell Science Ltd. [Google Scholar]
- Uansri, Sonvanee, Titiporn Tuangratananon, Mathudara Phaiyarom, Nattadhanai Rajatanavin, Rapeepong Suphanchaimat, and Warisara Jaruwanno. 2021. Predicted Impact of the Lockdown Measure in Response to Coronavirus Disease 2019 (COVID-19) in Greater Bangkok, Thailand, 2021. International Journal of Environmental Research and Public Health 18: 12816. [Google Scholar] [CrossRef]
- Uchibori, Manae, Cyrus Ghaznavi, Michio Murakami, Akifumi Eguchi, Hiroyuki Kunishima, Satoshi Kaneko, Keiko Maruyama-Sakurai, Hiroaki Miyata, and Shuhei Nomura. 2022. Preventive Behaviors and Information Sources during COVID-19 Pandemic: A Cross-Sectional Study in Japan. International Journal of Environmental Research and Public Health 19: 14511. [Google Scholar] [CrossRef]
- United Nations. 2020. Social Impact Assessment of COVID-19 in Thailand. Oxford Policy Management Limited Oxford, UK. Available online: https://thailand.un.org/index.php/en/91973-social-impact-assessment-COVID-19-thailand (accessed on 14 January 2023).
- Vicerra, Paolo Miguel Manalang. 2021. Knowledge-Behavior gap on COVID-19 among older people in rural Thailand. Gerontology and Geriatric Medicine 7: 2333721421997207. [Google Scholar] [CrossRef]
- Visanuyothin, Sawitree, Chanudda Chatanuluk, Sureeporn Saengsuwan, Amorn Rojanavarapong, and Pinyada Pornchanya. 2015. Health literacy of village health volunteer in Municipalitiy, Nakhonratchasima, Thailand. Journal of Public Health and Development 13: 37–54. [Google Scholar]
- Wang, Chen, Peter W. Horby, Frederick G. Hayden, and George F. Gao. 2020. A novel coronavirus outbreak of global health concern. The Lancet 395: 470–73. [Google Scholar] [CrossRef]
- World Health Organization (WHO). 2021. COVID-19 Situation. Thailand: WHO, WHO Thailand Weekly Situation Update No. 214. Available online: https://cdn.who.int/media/docs/default-source/searo/thailand/2021_12_17_tha-sitrep-214-COVID-19.pdf?sfvrsn=dd37e4f6_5 (accessed on 31 May 2023).
- Ye, Yisheng, Ruijun Wu, Yao Ge, Tao Wang, Xin Yao, Yao Yang, Chengxu Long, Fangfei Chen, Shangfeng Tang, and Rui Huang. 2021. Preventive behaviours and family inequalities during the COVID-19 pandemic: A cross-sectional study in China. Infectious Diseases of Poverty 10: 1–14. [Google Scholar] [CrossRef]
- Yen, Wei-Ting. 2020. Taiwan’s COVID-19 Management: Developmental State, Digital Governance, and State-Society Synergy. Asian Politics & Policy 12: 455–68. [Google Scholar] [CrossRef]
- Zarocostas, John. 2020. How to fight an infodemic. The Lancet 395: 676. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Yun, Qun Wu, Ting Zhang, and Lingxiao Yang. 2022. Vulnerability and fraud: Evidence from the COVID-19 pandemic. Humanities and Social Sciences Communications 9: 424. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).