Abstract
This study draws on a general theoretical framework comprising of a decision maker (a doctor), perceived moral intensity of the issue (breastfeeding substitute prescription), and the situational environment (hospital policy, pharma company promotions, and mother’s beliefs regarding breastfeeding) to explain the physician’s role and influence on mothers’ infant feeding choices when prescribing infant formula in Kuwait, Middle East. Moral intensity is an issue-contingent model that suggests ethical decisions vary in terms of how much a moral imperative is present in a situation. The moral intensity of the issue is assessed using six components. Path Least Squares results indicate the following moral intensity components have significant impact on prescription behavior: magnitude of consequences, probability of effect, and temporal immediacy. Company promotion and hospital policy also significantly influence doctor’s prescription of infant formula. Doctors appear to disengage from the consequences of over prescribing infant formula.
1. Introduction
Over prescribing or advising breast-milk substitutes is a major issue in healthcare because of its implications for a child’s early development. Empirical evidence from the Philippines suggests that mothers, who receive a prescription from a doctor for formula, were 3.25 times more likely to use formula, and infants given formula were 6.4 times more likely to stop breastfeeding before 12 months of age [1]. According to the WHO, there are few reasons for mothers to complement breastmilk or substitute it with infant formula [2]. A lack of breastfeeding has been linked to a number of harmful consequences such as higher death rates [3], higher rates of infections, lower school test scores [4], rising weight gain trajectory [5], and a number of chronic diseases [6]. The WHO is thus working towards increasing the rate of exclusive breastfeeding (i.e., no reliance on infant formula and/or solid food) for children under six months to at least 50% by 2025 [7], from a low global rate of 38% [8].
Several research articles and letters in the Lancet’s Series on breastfeeding [9,10], emphasize the benefits of global breastfeeding [11], and acknowledge more is needed to achieve the target of 50% exclusive breastfeeding. Some suggestions include for instance, strengthening legal protection to effectively implement, enforce and monitor existing laws supporting the International Code of Marketing of Breastmilk Substitutes1 [13], providing financial incentives [14], and supporting mothers in early breastfeeding [15]. Despite efforts, little progress has been made to combat the low exclusive breastfeeding rate. Various factors have been proposed and empirically tested [16,17,18] and this study offers an additional perspective by investigating, in Kuwait, doctors’ prescription of infant formula to mothers who can breastfeed2. More importantly, it aims to investigate if this practice is perceived as morally intense (i.e., as an ethical one) and if so, its impact on the prescription rate. The suggestion that doctors’ prescription or advice to mothers to complement or substitute breastmilk for infant formula can be seen as a moral issue is not far-fetched. For example, during the implementation of the breastfeeding policy in Nova Scotia, Canada, physicians were reported to be particularly challenging in sessions to educate them on the International Code of Marketing of Breast-milk substitute (referred to as the Code), and still accepted free formula and family care items with formula company advertisements on them ([19], p. 1314). Recent statistics show a 41% decline in the distribution of infant formula discharge packs in general hospitals and 91% in teaching hospitals in the US. Some attribute this trend to “ethical conflicts of interest”, and to a period “when the medical profession was critically evaluating the impact of commercial influences on professionalism and scientific integrity” ([20], p. 1064). That is, doctors and nurses in the United States were influencing mothers’ infant feeding choices. Ultimately, health care providers were doing the work of the medical representatives, by handing out samples to mothers, thus ‘helping dismantle breastfeeding as the cultural norm in the United States’ ([21], p. 345).
In light of this preliminary evidence and acknowledging that medical actions have a moral dimension in their commitment to improving patients’ health, it is posited that over prescribing infant formula constitutes a moral issue. The research questions guiding this study are: What are the factors influencing the prescription of breast milk substitutes to mothers who can breastfeed their babies? With what moral intensity do doctors perceive the situation under study, if any? Does the perception of moral intensity influence the decision to prescribe breastmilk substitutes?
This study offers the following potential contributions to the current understanding of factors that affect breastfeeding. First, it addresses a neglected and important topic, that is, the perception of breastfeeding prescription as a moral issue. Second, this study examines the moral issue of breastfeeding in a country that offers an interesting context. For example, religious laws imparted in the Koran suggest a two-year period of breastfeeding [22] and Kuwait requires a prescription to obtain a government subsidized infant formula. Third, this study explicitly acknowledges, in the model, the role of hospitals’ policy regarding the consent and attitude towards infant promotions. Finally, this study examines the influence of mothers’ beliefs and attitudes (as reported by doctors) on doctors’ prescription of infant formula.
Theoretical Framework
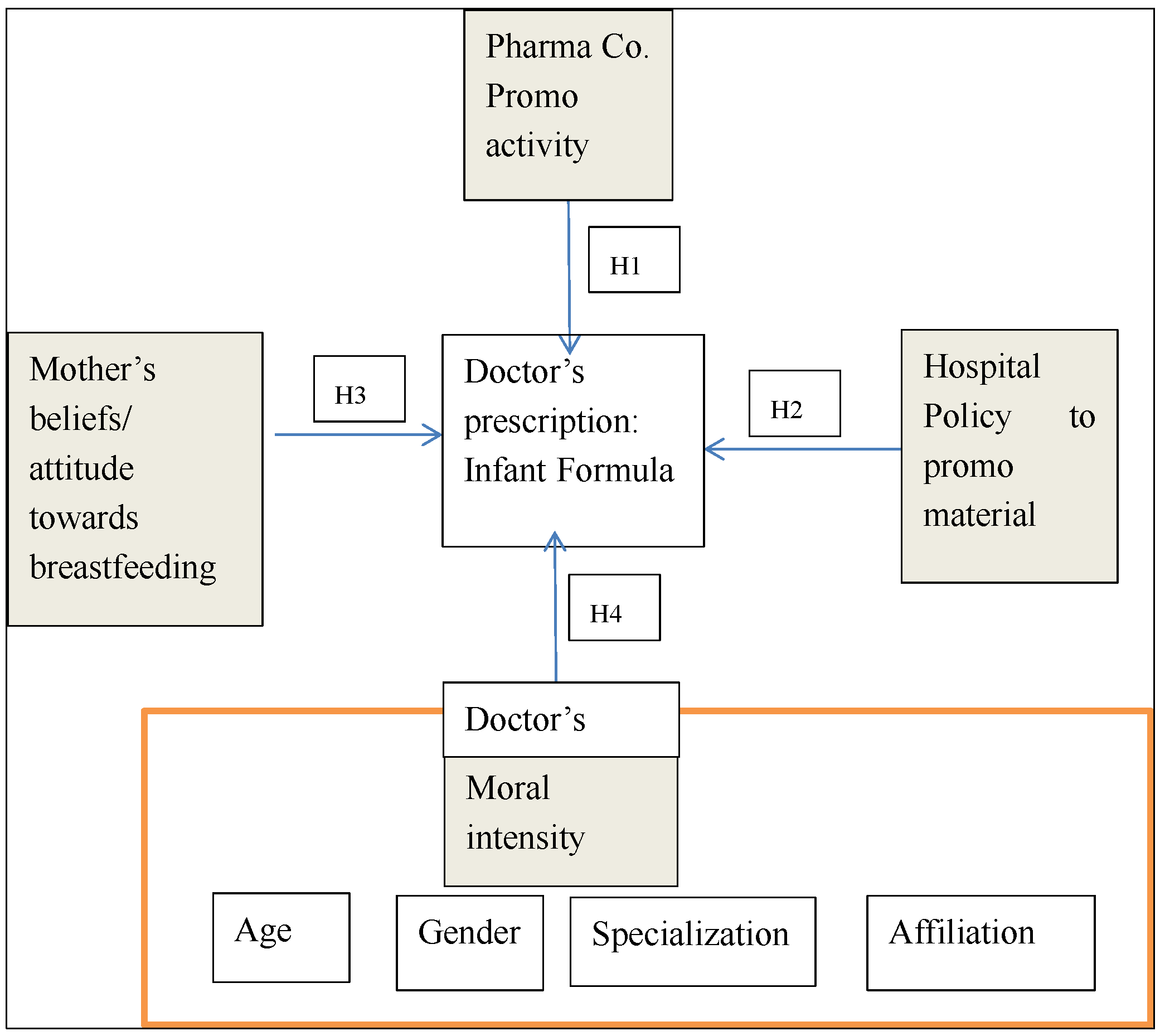
The following section describes briefly the existing evidence to support each of the proposed hypotheses depicted by an arrow in Figure 1. It begins by referring to the situational environment that influences doctors’ prescription. Three factors are considered, namely, the pharmaceutical efforts in promoting infant formula, the hospital policy towards such activities, and the mother’s beliefs and attitudes towards breastfeeding as reported by doctors. A fourth factor relates to the doctor: his/her perception of moral intensity of breastfeeding prescription. The hypothesized predictors are illustrated in the grey boxes and the doctors’ characteristics, illustrated in the unshaded boxes, are control variables.
Figure 1.
Model of prescription of Infant Formula.
The relationship between clinicians and the pharmaceutical industry has been under scrutiny for some years now given potential conflicts of interest and the impact on the cost, quality, and safety of health care [23]. Pharmaceutical companies’ expenditures on direct-to-consumer advertisement correlate strongly with what drugs patients request from physicians [24]. More specifically, the impact of commercial influences (e.g., trips to conferences) has also been linked to the prescription of drugs [25]. In a German sample, doctors attending these functions, and who were “educated” by pharmaceutical companies, increased their prescriptions for the targeted drugs following the attendance of “teach-ins” [26]. Interestingly, only a small percentage of doctors surveyed perceived themselves influenced by pharmaceutical company promotions, however, they thought the benefits others received had affected their professional ethics [27]. More evidence from the social sciences suggests that even gifts of negligible value can influence the behavior of the recipient in ways the recipient does not always realize [28].
Additional evidence related to infant formula manufacturers indicates some of these companies paid hospital staff across several nations to feed newborns with infant formula before their mothers had an opportunity to breastfeed them [29]. This is a more serious problem in countries with relaxed regulations and laws such as Kuwait [30], Pakistan [31] Philippines [32] China or India [33]. A recent report describes evidence of 813 Code violations from 81 countries [29]. For example, Dumex, a company owned by Danone, was heavily criticized for the briberies its medical representatives provided to healthcare providers in China [34]. Although the US exhibits a significant downward trend in infant formula pack distribution among hospitals [20], from a 72.6% in the year 2007 to 31.6% in 2013, a considerable percentage still remains. Since infant formula does not need a prescription in most countries, there is little evidence of its effect on infant formula consumption. Early evidence in the 90s found that physician’s recommendation was among the primary influencers of the choice of infant formula, along with recommendations from friends and family, advertisements, and infant formula the mother may have been given while in hospital [35]. A study in the Philippines of 5219 households and 345 respondents with children under 24 months corroborate the importance of advertising messages and doctors’ prescription. Those that received a doctor’s prescription for formula were 3.25 time more likely to use formula [1]. For the above reasons, we hypothesize that (H1) a pharmaceutical company promotional activity of infant formula influences the doctor’s decision to prescribe breastmilk substitutes.
Similarly, it is expected (H2) hospital policies permitting promotions of infant formula within hospitals (“baby unfriendly” hospitals [36]), will positively correlate with the prescription of breastmilk substitute. Evidence of a positive relation between institutional changes in maternity care practices (e.g., maternity ward practices that promote mother-infant contact and autonomy (rooming-in), and breastfeeding is noted in the Cochrane review [37]. Further, other studies have examined the impact of distribution of infant formula within hospitals on breast feeding rates, and find a negative effect [38,39,40]. More recently, a study in the US found no significant differences in breastfeeding initiation rates between accredited BFHI and non-Baby-Friendly facilities [41]. However, when taking into consideration education, breast-feeding initiation increased by 3.8 percentage points among mothers with lower education who delivered in Baby-Friendly facilities, but not among mothers with higher education.
A hospital that has implemented baby friendly practices mentioned that a major challenge was to change the attitude among staff [42]; hence, it is plausible to think hospital practices promoting unfriendly practices will affect doctors’ prescription toward baby formula. Specifically, doctors working in these facilities will perceive prescribing infant formula as an acceptable practice.
Finally, within the situational environment, mothers’ perceptions and attitudes towards breastfeeding are expected to have an important influence on the doctor’s decision to prescribe breastmilk substitute. A study in Belfast indicates breastfeeding mothers have a more positive attitude towards breastfeeding than bottle-feeding mothers [16], and that such an attitude will influence her individual commitment to breastfeeding [43]. We suggest in this study that this positive attitude will influence the doctor’s recommendation. Evidence shows that when patients made at least one request to their doctors, four-fifths of patients were granted their request [44,45]. Moreover, a survey of pediatricians in the United States found that doctors do not recommend breastfeeding to mothers who oppose breastfeeding [46]. It should be noted however that doctors may be influenced by their patients for other reasons. For example, it has been found general practitioners prescribe antibiotics for children to satisfy parents and shorten consultations [47]. In this study, we expect a relationship between mothers’ attitude towards breastfeeding and rate of formula prescription, such that, the more negative the attitude towards breastfeeding, the higher the rate of formula prescription (H3).
The fourth major antecedent of infant formula over prescription is the perception of breastmilk substitute as a moral issue itself. In this study, it is hypothesized that the moral intensity of an issue is negatively related to prescription of breastmilk substitutes. In other words, the more doctors consider breastfeeding a moral issue, the less likely they are to prescribe a breastmilk substitute (H4).
According to Jones [48], researchers examining moral or ethical behavior, have only considered the characteristics of the decision maker and the organization, but omitted the issue itself. Jones suggests that the moral intensity of the issue under study will have an impact on ethical behavior, since the more the matter is perceived as morally intense the more likely it is to “catch the attention of the moral decision maker” ([48], p. 381).
Six components of moral intensity are proposed to influence a person’s recognition of an issue as a moral problem, namely, the magnitude of consequences (an issue will be more intense if the consequences are more, rather than less, serious), social consensus (an issue will be more intense if society agrees on the morality (or immorality) of the issue), probability of the effect (an issue will be perceived more intense if the consequences are likely, rather than unlikely), temporal immediacy (an issue will be perceived more moral intense if the consequences occur sooner, rather than later), proximity of effect (an issue is more intense morally if the consequences affect those close or similar to the decision maker), and concentration of the effect (an issue will be more intense if fewer individuals bear the brunt of the consequences) [49].
According to moral intensity theory, as any one of the element above increases, the overall moral intensity of the situation or issue increases, and each component is likely to reduce the influence of unethical behavior [50]. The evidence regarding the impact of each component of moral intensity, however, remains an open question. Some studies have found social consensus has a significant effect on ethical behavior, and that neither the magnitude of consequences nor proximity play a meaningful role [51]. Still, others have concluded the magnitude of consequences is one of the most significant components influencing moral decisions [49] along with social consensus [52]. Methodological problems have been suggested to account for differences in findings, for instance, differences in research experiments (within and between subjects), manipulation of scenarios and salience of content within scenarios, and statements used to test moral intensity components [53].
There is no research suggesting a relationship between doctors’ individual characteristics (gender, age, specialization, and affiliation) and the prescription of breastmilk substitute. However, some relationships, albeit inconsistent, have been found between these characteristics and on other medical prescriptions. For instance, in relation to decisions on ethical issues, some argue that females and males reason differently and that the former possess more ethical attitude and judgments than the latter [54]. However, others have reported trivial or non-significant differences in ethical reasoning [55]. Some evidence suggests female physicians tend to communicate higher degrees of empathy in response to the empathic opportunities created by patients [56]. Thus, female doctors appear to relate more to mothers than male doctors. In addition, personal breastfeeding experience is associated with more optimal breastfeeding management among pediatricians [46].
Age of the doctor is considered a control variable since the rate of prescription of antibiotics has been found to decrease as the age of the doctor increases [57]. The prevailing literature also suggests the older an individual becomes, the more discerning and the higher the level of moral reasoning s/he operates [58]. Thus, it is inferred the older the person is, the less likely s/he will prescribe breast milk substitutes.
Medical specialization may also be related to breastmilk-substitute prescription. First, pediatric doctors are expected to be more knowledgeable and current about babies’ matters than GPs or Gynecologists, for example. Secondly, a primary goal of the American Academy of Pediatrics is to encourage optimal infant nutrition through the promotion of breastfeeding and “any routine professional, institutional, or commercial practices that tend to discourage breast-feeding should be opposed” ([59], p. 661). Although there is no evidence in relation to breastfeeding prescription, over-prescription of antibiotics in Korea was positively correlated with specialization: the higher the ratio of specialist to GPs, the higher the over prescription [60].
The characteristic of the hospital (government or private) where doctors operate may also have an effect on prescribing more breastmilk substitute than necessary, particularly in countries where regulations regarding the implementation of the Code are weak. A study conducted in Cambodia found women delivering in a private clinic were five times more likely to provide their child with breastmilk substitute than women delivering in public sector hospitals [61]. For this reason, the doctor’s affiliation to a hospital namely private, public, or both is also considered a control variable for the purposes of this study.
2. Materials and Methods
2.1. Design
A theoretical model comprising of a decision maker [the doctor], the perception of moral intensity, and the situational environment is used as a framework for collecting data. This study employs a quantitative, descriptive, and cross-sectional design from a sample of doctors in Kuwait.
2.2. Setting
This study took place in Kuwait. According to the 2015 World Breastfeeding Trend initiative report [30] the exclusive breastfeeding rate for 6 months is only 20% in Kuwait. The same report indicates that infant formula is subsidized by the government. The Ministry of Health General Store accepts donated ready to feed formula from milk companies. Penalties and sanctions are not yet established against violators of the Code. Finally, there are only two hospitals that have been designated as Baby Friendly out of fourteen that offer maternity services: one is a private hospital and the other is public. Only 14% of babies were delivered in a baby friendly facility.
2.3. Sample
Salesforce.com [62] was used to draw a sample from a population of 1570 health care providers in Kuwait. All 1570 healthcare providers were solicited to participate in an online survey to explain the physician’s role and influence on a mother’s infant feeding choices when prescribing breast milk substitute in Kuwait. This study includes 363 respondents who completed all questions in the survey (equivalent to a response rate of 23%). The sample is non-probabilistic but self-selected. The descriptive statistics of the sample are as follows: 169 (46.56%) were male participants, 56% were pediatricians, 9% were gynecologists, and the remaining consisted of general practitioners. Ages of respondents were divided into 3 age groups: less than 40 years, between 40 and 50, and over 50. 116 (31.96% of the sample) doctors were less than 40 years of age, 159 (43.8%) were between 40 and 50 years, while the remaining 88 (24.24%) doctors in our sample were more than 50 years old. Almost half of respondents, 186 (51.2%), work in government facilities, 268 (73.8%) practice in hospitals, 77 (21.2) practice in clinics, 9 (2.5%) practice in pharmacies, and 9 (2.5%) practice in both clinics and hospitals.
2.4. Measures
The breastmilk substitute prescription of the doctor was evaluated through two questions: “In your practice, what is the percentage (more or less) of exclusive bottle-fed infants among all infants aged from 0 to 6 months?” and “what is the percentage (more or less) of infant formula prescribed among all infants aged from 0 to 6 months?” An over prescription rate of infant formula was considered if the doctor prescribed breast milk substitute above the WHO target (50% of mothers who breastfeed). This criterion is based on the global target set by the WHO highlighted earlier in this article.
To measure a hospital’s acceptance of infant formula promotion and companies’ promotional practices towards breastfeeding substitutes, three statements were furnished to respondents. Examples of statements read by respondents are: ”In the facility you work in, healthcare providers may prescribe infant formulas to mothers who can breastfeed their babies”, “In the premises where you practice, the infant formula companies offer seminars and conferences to healthcare providers”, and “Infant formula companies offer free gifts and product reminders to healthcare providers in the facility you work in”.
The doctor’s perception of mothers’ attitude towards breastfeeding was measured using three statements (“From your practice, mothers do not see the importance of providing their babies with breast milk from the very beginning”, “working mothers almost always breastfeed their babies if their medical conditions permit to, while they are in the maternity leave” [reverse code]). “From your practice, mothers believe breastfeeding may damage their physical appearance”. These statements were measured on a scale from 1 to 7 where 1 = strongly agree, 7 = strongly disagree.
Respondents were given two marketing ethic scenarios to evaluate in conjunction with each statement. Scenarios have been commonly employed in the prevailing literature to gather information relating to perceived moral intensity [49], and the scenarios we use are adapted from Reidenbach et al. [63]. The scenarios read as follow:
- Scenario 1:
- A healthcare provider (doctor) is told by a mother that she is planning to bottle-feed her baby. However, because of his intention to prescribe an infant formula, the healthcare provider does not inform her about the benefits of breastfeeding and prescribed an infant formula instead.
- Scenario 2:
- An infant formula company sponsors a hospital’s advertisement campaign, and in return, the hospital allows the company to distribute and promote its branded ready to feed milk formula and branded maternity goody bags to mothers.
Further, we borrow the moral intensity measures found in Singhapakdi, Vitell and Kraft [64] to test our hypotheses. Moral intensity was measured using one statement for each of moral intensity’s six dimensions. The statement used to measure the Magnitude of Consequence is read as follows: ‘The overall harm (if any) done as a result of the healthcare provider’s action would be very small’. To measure Social Consensus the following statement was used: “Most people would agree that the healthcare provider’s action is wrong” [reverse code]. To measure Probability of Effect: “There is a very small likelihood that the [healthcare provider]’s action will actually cause any harm”. To measure Temporal Immediacy: “The [healthcare provider]’s action will not cause any harm in an immediate future”. The measure of Proximity read: “If the [healthcare provider] is a personal friend of the [mother], the action is wrong”. Finally, Concentration of Effect was measured by: “The [healthcare provider]’s action will harm very few people (if any)”. These statements were measured on a scale from 1 to 7 where 1 = strongly agree, 7 = strongly disagree, and higher values indicate higher degrees of perceived moral intensity.
Given the sensitive nature of this study, respondents may respond differently if they—or others—are the focus of inquiry [65]. To mitigate this bias, self-administered questionnaires [66] are used, and the scenario settings provided refer to a health care provider, and the word, doctor, in brackets. Note however, that each statement read by the respondent does not include the word doctor.
2.5. Analysis Plan
This article utilizes Path Least Squares Structural Equation Modeling (PLS-SEM) to test the predicting model of prescription of infant formula, and calculates statistical parameters such as Cronbach alpha (CA) and composite reliability (CR). A Cronbach alpha of 0.70 has been employed throughout this study as suggested by the extant literature [67]. PLS-SEM emphasizes the use of the Composite Reliability (CR) parameter and not Cronbach alpha since it is generally regarded as a more appropriate criterion of internal consistency reliability. Cronbach alpha assumes equal weighting of a construct’s items whereas CR considers the loadings of each item obtained from the full model [68]. PLS-SEM is advantageous for small samples (such as the case of this study) and non-normal data (within a reasonable range), and it is used predominantly to test predictions rather than theory [68].
To test the influence of the demographic variables on percentage of prescription of breastmilk substitute (dependent variable), t-tests were conducted for gender, and Analysis of Variance was performed for age and medical specialization. Further, significance levels of 5% are used where appropriate. Given previous studies have acknowledged the presence of two dimensions within the moral intensity construct [69], Exploratory Factor Analysis (EFA) was undertaken to further explore the dimensionality of moral intensity.
3. Results
On average, prescription of infant formula in a doctor’s practice was 71.6%, which is consistent with the low rates of exclusive breastfeeding reported earlier. It should be noted that these results also provide evidence of over prescription of infant formula in Kuwait. If the WHO target for 2025 of 50% is taken as a reasonable point of reference, 71.6% is markedly above this level (z = 8.231; p < 0.0001). An obvious concern in social research studies is the presence of a social desirability bias. The high self-reported infant formula prescription suggests however, that this is not a major issue. Indeed, a bias is more likely to exist if the reported prescription of infant formula in our sample is low (e.g., below the WHO recommended target), if, of course, it is assumed breast-feeding is considered socially desirable.
To achieve the research objective posed at the beginning of this study that is, to determine if the prescription of infant formula to mothers that can breastfeed is perceived as a moral issue, each of the components of moral intensity were summed and a mean value was calculated. Table 1 reports the descriptive statistics for the scenarios. Overall, the results indicate that doctors perceive the situations in scenarios 1 and 2 as having relatively high moral intensity (Mean value = 5.08 and 4.86 respectively and statistically significant t (df =362) = 76.66; two-tailed p < 0.001 and t (df =362) = 90.18; two-tailed p < 0.001). Recall, both scenarios provide instances of morally unacceptable behavior. Thus, in both scenarios, respondents judged the actors’ actions as morally incorrect.

Table 1.
Descriptive Statistics of Scenarios.
Cronbach reliability measures range from 0.70 (doctor’s moral intensity) to company promotional practice Cronbach alpha (α) = 0.94. All composite reliabilities are high and beyond the minimum acceptable cut off, i.e., 0.70 [67].
Moral intensity statements were subjected to EFA and two dimensions were found. Dimension one is comprised of the components Magnitude of consequences, Probability of effects and Temporal immediacy and is coined for the purposes of this article, ‘perceived potential harm’. The second dimension comprises of two components namely, Social consensus and Concentration of effects. Proximity of effects was found to be an inadequate discriminator of either dimension and has been discarded for subsequent analysis. Scores obtained from the factor analysis were saved and later used in the prediction model of breastmilk substitute prescription.
Next, the hypothesized factors were regressed using Path Least Squares. Table 2 shows the standardized coefficients of each of the paths (underlying the hypotheses) and their effect on the dependent variable. All hypotheses are statistically significant except for one of the dimensions of moral intensity, namely, the concentration of effects (Dimension 2). Importantly, however, Dimension 1 (perceived potential harm) influences prescription of breastmilk substitutes (B = –0.14; p = 0.003) Together, company promotion, hospital policy toward company infant formula promotion, mother’s attitude and beliefs, and perceived potential harm predict (R2) 52% of the variability of the prescription behavior.

Table 2.
Reliability and Path coefficients of infant formula prescription model.
A doctor’s individual characteristics, treated as control variables, such as gender (t df 361 = 1.23; p = 0.216), age (F df 2 = 0.27; p = 0.761), or medical specialization (F df 4 = 1.08; p = 0.363) did not contribute to predicting prescription of infant formula. There is a statistically significant difference between doctors who work in private or public hospitals, or both, in relation to prescription of infant formula (F df 2 = 15.63; p = 0.000). This suggests that doctors who work in private hospitals are less reluctant to prescribe infant formula than those who work only in public hospitals. Private hospitals in Kuwait treat mothers in maternity wards like clients, and are given sedative to rest. Thus, hospital staff feed the mother’s baby with infant formula, and do not exert effort to convince her to breastfeed for fear of annoying her [70].
4. Discussion
This study can be broken into two parts. First, it investigates whether or not doctors perceive breastfeeding as a morally intense issue. Second, this article seeks to understand the factors contributing to the prescription of infant formula. In relation to the latter, the data reveal prescription of infant formula is significantly associated with company promotions, hospital policies that allow for such company practices, mothers’ attitudes towards breastfeeding, and importantly, the perceived moral intensity of breastfeeding. Of the contextual variables, it was hypothesized that promotion of infant formula by a pharmaceutical company influences doctors’ prescription of a breastmilk substitute (H1). The data is largely in support of this hypothesis, that is, the more pharmaceutical companies promote breastmilk substitutes in hospitals the higher is the prescription of infant formula. While this study does not specifically investigate breastfeeding rates, this result is consistent with previous studies that report a negative correlation between the promotion and distribution of infant formula (within and outside hospitals) and breastfeeding rates. Given the reasonable assumption that infant formula is a breastmilk substitute, our findings imply that the more doctors prescribe infant formula, the higher is the disincentive to breastfeed. This is in accordance with a paper that found mothers were 3.25 times more likely to use a breast milk substitute to halt breastfeeding when they received a prescription from a doctor for formula [1]. Recall, it is posited that hospital policy permitting promotions of infant formula will influence doctor’s prescription of infant formula (H2). Indeed, it is the second most important predictor of infant formula prescription, and this finding is largely in line with studies that relate hospital support of breastfeeding to breastfeeding rates [40]. Particularly in countries like Kuwait where regulations are relaxed on the implementation of the Code, the lack of hospital support toward breastfeeding may compound the influence on doctors to prescribe infant formula since it reinforces the perception that breastfeeding is the social norm. Interestingly, however, the literature finds that even in cases of developed countries where hospitals adopted a policy supporting the international Code on breastfeeding, the exclusive breastfeeding remains low. For example, Australia has an average of approximately 15% [43].
Mothers’ attitude towards breastfeeding, as reported by doctors, is also important in influencing a doctor to prescribe a breast-milk substitute. The more mothers perceive breastfeeding as unimportant and inconvenient, the more likely doctors are to prescribe a breastmilk substitute (H3). Our findings here contribute to the literature on the influence patients have on prescription by extending the evidence to infant formula prescription. The extant literature provides evidence to suggest doctors are not reluctant to respond to patient’s requests [44]. Our results may also offer insights into why some pediatricians in the U.S. are less likely to believe the benefits of breastfeeding outweigh its difficulties or inconvenience [46], and why difficulties—and perceived difficulties—faced by mothers as a result of breastfeeding may prompt requests to doctors.
Findings from this study indicate that doctors are influenced by only one dimension (out of two) of moral intensity. The data is therefore in partial support of H4. Our findings are also consistent with other studies that have found only some of the moral intensity variables are influential in ethical decisions [71].
Responses to the scenarios presented appear to reflect doctors’ consequentialist views towards prescribing infant formula. That is, their views are driven by the consequences of prescribing infant formula (Magnitude of consequences, Probability of effect and Temporal immediacy). One explanation for the insufficient support of the total moral intensity dimensions is that doctors may just accept that exclusive breastfeeding is not the norm in Kuwait (circa 20% among Kuwaiti mothers [30]. It is well established that what others accept, expect, and do affect behavior [72]. It is also known in the relevant literature that people tend to rely on ethical norms—and less on perceived consequences—in forming ethical judgments [73]. Doctors may be acting in the same way when over prescribing infant formula. They may hold a relativistic moral stance, that is, the belief that the moral decision is driven by the circumstances of the particular situation or context [74]. The circumstances indicate that the majority of mothers in Kuwait are not initiating and sustaining breastfeeding exclusively for the baby’s first six months of age. Further, according to the doctors in our study, mothers do not have a positive attitude towards breastfeeding for a long period, which reinforces the perception of doctors that the best course of action is to prescribe infant formula. Caution must be exercised here since doctors may simply be displacing their responsibility (a mechanism of moral disengagement [75]) and this study does not investigate directly the attitude and beliefs of mothers.
Perhaps we do not find a stronger influential effect of the moral intensity factor because doctors perceive the risks of not breastfeeding are outweighed by any concerns about the sustainability of breastfeeding, as found among some pediatricians in the U.S. [46].
Another plausible explanation is that doctors, even when they perceive breastfeeding as a moral issue, they disengage morally by decoupling [76], or minimize the importance of the issue, even when acknowledging it as an issue, to rid of the feeling of guilt and shame [77]. For example, there is evidence to suggest that doctors believe the acceptance of gifts and lunches is not unreasonable and that the pharmaceutical company’s practices have no influence on their behavior, but they do on others. The results in this study suggest that to reduce over prescription of breastmilk substitute in a country like Kuwait, a concerted effort to alter the four predictors of over prescription behavior is required. Hospitals can play an important role in providing disincentives to over-prescribe by implementing the BFHI. Hospitals that do not subscribe to the BFHI should have a written policy to deter pharmaceutical companies to promote their products within and outside the hospital, and to sanction health-care providers that accept any kinds of gifts or lunches associated with infant formula companies.
Since infant formula manufacturers’ promotional activities have a great impact on the over-prescription of infant formula, pharmaceutical companies, if they want to be perceived as socially responsible, should abstain from distributing free maternity bounties with infant formula bottles. Pharmaceutical companies should develop a code of ethics in relation to promoting breastmilk substitutes (if they do not have them), support and implement this code to ensure employees can focus their attention on the code when dealing with governments, hospitals and other institutions, or individuals. Companies should educate their employees with respect to this code of ethics and sanction employees if it is not adhered to. We find that doctors perceive breastfeeding with some degree of moral intensity however they seem to disengage from the consequences of prescribing infant formula. Perhaps doctors can be made more aware of the trend towards greater support of the Code and that local norms should not be used as a guide.
This is not without its limitations. For instance, we have not considered the cultural backgrounds or ethnicity of the mothers. It is possible that doctors in the Middle East exercise an undue influence on women who do not assert themselves against the quick advice to bottle-feed their babies, because of their cultural backgrounds. This poses an interesting new avenue to explore in further studies. A note of caution is in order here. Since there was no direct measure of mothers’ beliefs and attitudes towards breastfeeding (but the doctors’ report), future research may obtain a sample of mothers and learn directly about their attitudes and beliefs in the Middle East culture.
Another potential limitation is the non-response bias, which may be impacting the statistical significance of our findings. The response rate in our sample is 23%. Perhaps the most important variable linked to the non-response bias is the doctor’s time. If this is the case, correction for non-response bias would not significantly impact the unconditional mean of the dependent variable (prescription of infant formula) since it is already quite large (70.1%). A correction would impact [something] by 5% based on the information obtained from a meta-analytic study on the effect of the non-response bias [78].
5. Conclusions
The results gleaned from this study contribute to a better understanding of the factors influencing a doctor’s prescription of infant formula. Although this study does not measure breastfeeding rates specifically, our results suggest that if doctors are quick to prescribe a breast-milk substitute, such a practice will have an impact on breastfeeding, and perhaps explain the low exclusive breast-feeding rates in Kuwait. Secondary data from Kuwait regarding low exclusive breastfeeding rates during the baby’s first six months of age is consistent with other studies conducted in developed countries where exclusive breastfeeding rates are very low also. The novelty of this research is the inclusion of the perception of moral intensity in a model that explains the prescription and over prescription of breast feeding substitutes by physicians. We have learned that doctors perceive breastfeeding infant prescription with some moral intensity, but they disengage perhaps because doctors perceive such prescription as the norm.
Author Contributions
Sharif El Beshlawy conceived the thesis for the research, collected data, and conducted preliminary data analysis. Rosa Rios collected and analyzed literature, wrote drafts of the literature and results, and performed data analysis. Hernan Riquelme contributed in designing the survey, collected literature, performed data analysis and interpretation, revised drafts, and wrote the final paper.
Conflicts of Interest
The authors declare no conflict of interest. The College under which the study was conducted does not have an institutional review board therefore the study was not submitted for an approval. However, the study complies with ethical standards in the treatment of all participants in the survey.
References
- Howard L. Sobel, Alessandro Iellamo, René R. Raya, Alexander A. Padilla, Jean-Marc Olivé, and Soe Nyunt-U. “Is unimpeded marketing for breast milk substitutes responsible for the decline in breastfeeding in the Philippines? An exploratory survey and focus group analysis.” Social Science & Medicine 73 (2011): 1445–48. [Google Scholar] [CrossRef] [PubMed]
- WHO/UNICEF. Acceptable Medical Reasons for Use of Breast-Milk Substitutes. Geneva: World Health Organization, 2009. [Google Scholar]
- Mari Jeeva Sankar, Bireshwar Sinha, Ranadip Chowdhury, Nita Bhandari, Sunita Taneja, Jose Martines, and Rajiv Bahl. “Optimal breastfeeding practices and infant and child mortality: A systematic review and meta-analysis.” Acta Paediatrica 104 (2015): 3–13. [Google Scholar] [CrossRef] [PubMed]
- Cathal McCrory, and Richard Layte. “The effect of breastfeeding on children’s educational test scores at nine years of age: Results of an Irish cohort study.” Social Science & Medicine 72 (2011): 1515–21. [Google Scholar] [CrossRef] [PubMed]
- Stacy J. Carling, Margaret M. Demment, Chris L. Kjolhede, and Christine M. Olson. “Breastfeeding duration and weight gain trajectory in infancy.” Pediatrics 135 (2015): 111–19. [Google Scholar] [CrossRef] [PubMed]
- Colin W. Binns, Mi Kyung Lee, Li Tang, Chuan Yu, Tomiko Hokama, and Andy Lee. “Ethical issues in infant feeding after disasters.” Asia-Pacific Journal of Public Health 24 (2012): 672–80. [Google Scholar] [CrossRef] [PubMed]
- Flavia Bustreo. “Understanding the past—Planning the future: Celebrating 10 years of WHO/UNICEF’s Global Strategy for Infant and Young Child Feeding. Maternal, newborn, child and adolescent health.” 2012. Available online: http://www.who.int/maternal_child_adolescent/news_events/news/2012/30_07_2012/en/# (accessed on 5 July 2015).
- WHO. “European Region has lowest global breastfeeding rates.” 5 August 2015. Available online: http://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/news/news/2015/08/who-european-region-has-lowest-global-breastfeeding-rates (accessed on 1 December 2015).
- Cesar G. Victora, Rajiv Bahl, Aluísio J. D. Barros, Giovanny V. A. França, Susan Horton, Julia Krasevec, Simon Murch, Mari Sankar, Neff Walker, and Nigel Rollins. “Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect.” The Lancet 387 (2016): 475–90. [Google Scholar] [CrossRef]
- Ranadip Chowdhury, Bireshwar Sinha, Mari Jeeva Sankar, Sunita Taneja, Nita Bhandari, Nigel Rollins, Rajiv Bahl, and Jose Martines. “Breastfeeding and maternal health outcomes: A systematic review and meta-analysis.” Acta Paediatrica 104 (2015): 96–113. [Google Scholar] [CrossRef] [PubMed]
- The Lancet. “Breastfeedindg: Achieving the new normal.” 30 January 2016. Available online: http://thelancet.com/journals/lancet/article/PIIS0140-6736%2816%2900210-5/fulltext (accessed on 29 May 2016).
- World Health Organization (WHO). International Code of Marketing of Breast-Milk Substitutes. Geneva: WHO, 1981, p. 24. [Google Scholar]
- The Lancet. “No ifs, no buts, no follow-on milk.” 21 May 2016. Available online: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2816%2930599-2/fulltext?rss=yes (accessed on 27 July 2016).
- Clare Relton, Barbara Whelan, Mark Strong, Kate Thomas, Heather Whitford, Elaine Scott, and Patrice van Cleemput. “Are financial incentives for breastfeeding feasible in the UK? A mixed methods field study.” The Lancet 384 (2014): S5. [Google Scholar] [CrossRef]
- Dylan Walters, Jakub Kakietek, Julia Eberwein, Thomas Pullum, and Meera Shekar. “Breastfeeding in the 21st century.” 2016. Available online: http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736%2816%2930546-3.pdf (accessed on 27 July 2016).
- Hilary Bishop, Wendy Cousins, Karen Casson, and Ann Moore. “Culture and caregivers: Factors influencing breastfeeding among mothers in west Belfast, Northern Ireland.” Child Care in Practice 14 (2008): 165–79. [Google Scholar] [CrossRef]
- Helen Skouteris, Cate Nagle, Michelle Fowler, Bridie Kent, Pinki Sahota, and Heather Morris. “Interventions designed to promote exclusive breastfeeding in high-income countries: A systematic review.” Breastfeeding Medicine 9 (2014): 113–27. [Google Scholar] [CrossRef] [PubMed]
- Ke Zhang, Li Tang, Hong Wang, Li-Qian Qiu, Colin W. Binns, and Andy H. Lee. “Why do mothers of young infants choose to formula feed in china? Perceptions of mothers and hospital staff.” International Journal of Environmental Research and Public Health 12 (2015): 4520–32. [Google Scholar] [CrossRef] [PubMed]
- Sara F. L. Kirk, Sarah Meaghan Sim, Erin Hemmens, and Sheri L. Price. “Lessons learned from the implementation of a provincial breastfeeding policy in Nova Scotia, Canada and the implications for childhood obesity prevention.” International Journal of Environmental Research and Public Health 9 (2012): 1308–18. [Google Scholar] [CrossRef] [PubMed]
- Jennifer M. Nelson, Ruowei Li, and Cria G. Perrine. “Trends of US hospitals distributing infant formula packs to breastfeeding mothers, 2007 to 2013.” Pediatrics 135 (2015): 1051–56. [Google Scholar] [CrossRef] [PubMed]
- Todd Wolynn. “Breastfeeding—So easy even a doctor can support it.” Breastfeeding Medicine 6 (2011): 345–47. [Google Scholar] [CrossRef] [PubMed]
- Huda. “Breastfeeding in Islam.” 11 March 2016. Available online: http://islam.about.com/od/parenting/a/breastfeeding.htm (accessed on 8 August 2016).
- Quinn Grundy, Lisa Bero, and Ruth Malone. “Interactions between non-physician clinicians and industry: A systematic review.” PLOS Medicine 10 (2013): e1001561. [Google Scholar] [CrossRef] [PubMed]
- Worst Pills, and Best Pills. “Misprescribing and overprescribing of drugs.” Available online: http://www.worstpills.org/public/page.cfm?op_id=3 (accessed on 1 December 2015).
- Marc A. Rodwin. Medicine, Money, and Morals: Physicians’ Conflicts of Interest. New York: Oxford University Press, 1993. [Google Scholar]
- Charlotte M. Wright, and Tony Waterston. “Relationships between paediatricians and infant formula milk companies.” Archives of Disease in Childhood 91 (2006): 383–85. [Google Scholar] [CrossRef] [PubMed]
- Klaus Lieb, and Simone Brandtönies. “A survey of German physicians in private practice about contacts with pharmaceutical sales representatives.” Deutsches Ärzteblatt International 107 (2010): 392–98. [Google Scholar] [PubMed]
- Dana Katz, Arthur Caplan, and Jon Merz. “All gifts large and small. Toward an understanding of the ethics of pharmaceutical industry gift-giving.” The American Journal of Bioethics 3 (2003): 39–46. [Google Scholar] [CrossRef] [PubMed]
- IBFAN. Breaking the Rules, Stretching the Rules 2014. Edited by Annelies Allain. Penang: International Baby Food Action Network, 2014, p. 40. Available online: http://www.babymilkaction.org/wp-content/uploads/2014/05/BTR14inbrief.pdf (accessed on 25 July 2016).
- Kuwait-WBTi. “Kuwait WBTi Assessment report.” In The Worldbreastfeeding Trends Initiative (WBTi). Kuwait: Kuwait MOH, 2015. [Google Scholar]
- Rizwan Raheem Ahmed, and Ahmad Saeed. “Pharmaceutical drug promotion in Pakistan: Issues in ethical and non-ethical practices.” Interdisciplinary Journal of Contemporary Research in Business 4 (2012): 149–64. [Google Scholar]
- Barbara Mintzes. “Regulation of formula advertising in the Philippines and promotion and protection of breastfeeding: A commentary on Sobel, Iellamo, Raya, Padilla, Olivé and Nyunt-U.” Social Science & Medicine 73 (2011): 1449–51. [Google Scholar] [CrossRef] [PubMed]
- June P. Brady, and Leila Srour. “India, Laos and South Africa reject sponsorship and gifts from formula companies.” African Health Sciences 14 (2014): 211–15. [Google Scholar] [CrossRef] [PubMed]
- BBC News. “Danone in management shuffle amid China bribery claims.” 15 October 2013. Available online: http://www.bbc.com/news/business-24530034 (accessed on 5 July 2015).
- Bob D. Cutler, and Robert F. Wright. “The US infant formula industry: Is direct-to-consumer advertising unethical or inevitable? ” Health Marketing Quarterly 19 (2002): 39–55. [Google Scholar] [CrossRef] [PubMed]
- WHO. “Baby-friendly hospital initiative.” Available online: http://www.who.int/nutrition/topics/bfhi/en/ (accessed on 5 July 2015).
- Fairbank Lisa, Susan O’Meara, Mary Renfrew, Mike Woolridge, and Amanda Sowden. “A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding.” Health Technology Assessment 4 (2000): 1–171. [Google Scholar]
- Angela Donnelly, Helen Snowden, Mary Renfrew, and Mike Woolridge. “Commercial hospital discharge packs for breastfeeding women.” In The Cochrane Library. Chichester: John Wiley & Sons, Ltd., 2004. [Google Scholar]
- Barbara L. Philipp, Anne Merewood, Lisa W. Miller, Neetu Chawla, Melissa M. Murphy-Smith, Jenifer S. Gomes, Sabrina Cimo, and John T. Cook. “Baby-friendly hospital initiative improves breastfeeding initiation rates in a US hospital setting.” Pediatrics 108 (2001): 677–81. [Google Scholar] [CrossRef] [PubMed]
- June Pauline Brady. “Marketing breast milk substitutes: Problems and perils throughout the world.” Archives of Disease in Childhood 97 (2012): 529–32. [Google Scholar] [CrossRef] [PubMed]
- Summer Sherburne Hawkins, Ariel Dora Stern, Christopher F. Baum, and Matthew W. Gillman. “Evaluating the impact of the Baby-Friendly Hospital Initiative on breast-feeding rates: A multi-state analysis.” Public Health Nutrition 18 (2015): 189–97. [Google Scholar] [CrossRef] [PubMed]
- Joy Heads. “The baby friendly hospital initiative: A case study from NSW.” New South Wales Public Health Bulletin 16 (2005): 63–66. [Google Scholar] [PubMed]
- Australian Health Ministers’ Conference. The Australian National Breastfeeding Strategy 2010–2015; Canberra: Australian Government Department of Health and Ageing, 2009.
- Richard L. Kravitz, Robert A. Bell, Rahman Azari, Edward Krupat, Steven Kelly-Reif, and David Thom. “Request fulfillment in office practice: Antecedents and relationship to outcomes.” Medical Care 40 (2002): 38–51. [Google Scholar] [CrossRef] [PubMed]
- Richard L. Kravitz, Robert A. Bell, Carol E. Franz, Richard L. Kravitz, Marc N. Elliott, Ezra Amsterdam, Carrie Willis, and Lisa Silverio. “Characterising patient requests and physician responses in office practice.” Health Services Research 37 (2002): 217–38. [Google Scholar] [PubMed]
- Lori B. Feldman-Winter, Richard J. Schanler, Karen G. O’Connor, and Ruth A. Lawrence. “Pediatricians and the promotion and support of breastfeeding.” Archives of Pediatrics & Adolescent Medicine 162 (2008): 1142–49. [Google Scholar] [CrossRef] [PubMed]
- Patricia J. Lucas, Christie Cabral, Alastair D. Hay, and Jeremy Horwood. “A systematic review of parent and clinician views and perceptions that influence prescribing decisions in relation to acute childhood infections in primary care.” Scandinavian Journal of Primary Health Care 33 (2015): 11–20. [Google Scholar] [CrossRef] [PubMed]
- Thomas M. Jones. “Ethical decision making by individuals in organizations: An issue-contingent model.” Academy of Management Review 16 (1991): 366–95. [Google Scholar]
- Loy D. Watley, and Douglas R. May. “Enhancing moral intensity: The roles of personal and consequential information in ethical decision-making.” Journal of Business Ethics 50 (2004): 105–26. [Google Scholar] [CrossRef]
- Douglas R. May, and Kevin P. Pauli. “The role of moral intensity in ethical decision making a review and investigation of moral recognition, evaluation, and intention.” Business & Society 41 (2002): 84–117. [Google Scholar] [CrossRef]
- Mark A. Davis, Nancy Brown Johnson, and Douglas G. Ohmer. “Issue-contingent effects on ethical decision making: A cross-cultural comparison.” Journal of Business Ethics 17 (1998): 373–89. [Google Scholar] [CrossRef]
- Tim Barnett. “Dimensions of moral intensity and ethical decision making: An empirical study.” Journal of Applied Social Psychology 31 (2001): 1038–57. [Google Scholar] [CrossRef]
- Joan Marie McMahon, and Robert J. Harvey. “The effect of moral intensity on ethical judgment.” Journal of Business Ethics 72 (2007): 335–57. [Google Scholar] [CrossRef]
- Susan C. Borkowski, and Yusuf J. Ugras. “Business students and ethics: A meta-analysis.” Journal of Business Ethics 17 (1998): 1117–27. [Google Scholar] [CrossRef]
- Stephen Thomas, and James Rest. “Moral judgement, behavior, decision making, and attitudes.” In Moral Development: Advances in Research and Theory. Edited by James Rest. New York: Praeger, 1986, pp. 133–75. [Google Scholar]
- Carma L. Bylund, and Gregory Makoul. “Empathic communication and gender in the physician-patient encounter.” Patient Education and Counseling 48 (2002): 207–16. [Google Scholar] [CrossRef]
- Letizia Orzella, Francesco Chini, Patrizzio Pezzotti, and Marco Nardelli. “Antibiotic prescriptions in the paediatric population in the Lazio Region of Italy: Association with children’s and physician’s characteristics.” Annali di Igiene: Medicina Preventiva e di Comunita 26 (2013): 507–17. [Google Scholar]
- Lawrence Kohlberg. “Moral Stages and Moralization: The Cognitive-Developmental.” In Moral Development and Behavior: Theory, Research, and Social Issues. Edited by Thomas Lickona. New York: Rinehart and Winston, 1976. [Google Scholar]
- American Academy of Pediatrics (AAP). “The promotion of breast-feeding.” Pediatrics 69 (1981): 654–61. [Google Scholar]
- Kyung-Hyun Choi, Sang-Min Park, Ju-Hyun Lee, and Soonman Kwon. “Factors affecting the prescribing patterns of antibiotics and injections.” Journal of Korean Medical Science 27 (2012): 120–27. [Google Scholar] [CrossRef] [PubMed]
- Sophonneary Prak, Miriam Iuell Dahl, Sam Oeurn, Joel Conkle, Aaron Wise, and Arnaud Laillou. “Breastfeeding Trends in Cambodia, and the Increased Use of Breast-Milk Substitute—Why Is It a Danger? ” Nutrients 6 (2014): 2920–30. [Google Scholar] [CrossRef] [PubMed]
- “salesforce.com.” Available online: https://www.salesforce.com/ (accessed on 25 September 2015).
- R. Eric Reidenbach, Donald P. Robin, and Lyndon Dawson. “An application and extension of a multidimensional ethics scale to selected marketing practices and marketing groups.” Journal of the Academy of Marketing Science 19 (1991): 83–92. [Google Scholar] [CrossRef]
- Anusorn Singhapakdi, Scott J. Vitell, and Kenneth L. Kraft. “Moral intensity and ethical decision-making of marketing professionals.” Journal of Business Research 36 (1996): 245–55. [Google Scholar] [CrossRef]
- David Glen Mick. “Are studies of dark side variables confounded by socially desirable responding? The case of materialism.” Journal of Consumer Research 23 (1996): 106–19. [Google Scholar] [CrossRef]
- Delroy Paulhus. “Two-Component Models of Socially Desirable Responding.” Journal of Personality and Social Psychology 46 (1984): 598–609. [Google Scholar] [CrossRef]
- David Streiner, Geoffrey Norman, and John Cairney. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed. New York: Oxford University Press, 2014. [Google Scholar]
- Joseph F. Hair, Marko Sarstedt, Torsten M. Pieper, and Christian M. Ringle. “The use of partial least squares structural equation modeling in strategic management research: A review of past practices and recommendations for future applications.” Long Range Planning 45 (2012): 320–40. [Google Scholar] [CrossRef]
- Joan M. McMahon, and Robert J. Harvey. “An analysis of the factor structure of Jones’ moral intensity construct.” Journal of Business Ethics 64 (2006): 381–404. [Google Scholar] [CrossRef]
- Hussain Al-Qatari. “Milking Health for All Its Worth.” Kuwait Times, 22 July 2011. [Google Scholar]
- Jennifer Kish-Gephart, David Harrison, and Linda Trevino. “Bad apples, bad cases, and bad barrels: Meta-analytic evidence about sources of unethical decision work.” Journal of Applied Psychology 95 (2010): 1–31. [Google Scholar] [CrossRef] [PubMed]
- Alan Berkowitz. “The social norms approach: Theory, research, and annotated bibliography.” 2004. Available online: alanberkowitz.com/articles/social_norms.pdf (accessed on 24 August 2015).
- Scott J. Vitell, Anusorn Singhapakdi, and James Thomas. “Consumer ethics: An application and empirical testing of the Hunt-Vitell theory of ethics.” Journal of Consumer Marketing 18 (2001): 153–78. [Google Scholar] [CrossRef]
- Donelson R. Forsyth. “Judging the morality of business practices: The influence of personal moral philosophies.” Journal of Business Ethics 11 (1992): 461–70. [Google Scholar] [CrossRef]
- Albert Bandura, Claudio Barbaranelli, Gian Caprara, and Concetta Pastorelli. “Mechanisms of moral disengagement in the exercise of moral agency.” Journal of Personality and Social Psychology 71 (1996): 364–74. [Google Scholar] [CrossRef]
- Amit Bhattacharjee, Jonathan Berman, and Americus Reed II. “Moral decoupling enables consumers to admire and admonish.” Journal of Consumer Research 39 (2013): 1167–84. [Google Scholar] [CrossRef]
- Albert Bandura. “Social cognitive theory: An agentic perspective.” Asian Journal of Social Psychology 2 (1999): 21–41. [Google Scholar] [CrossRef]
- Robert M. Groves. “Nonresponse rates and nonresponse bias in household surveys.” Public Opinion Quarterly 70 (2006): 646–75. [Google Scholar] [CrossRef]
- 1The aim of this Code is “to contribute to the provision of safe and adequate nutrition for infants, by the protection and promotion of breast-feeding, and by ensuring the proper use of breast-milk substitutes, when these are necessary, on the basis of adequate information and through appropriate marketing and distribution.” [12]. It also aims to promote breast-feeding, to take legislative and social action to facilitate breast-feeding by working mothers, and to regulate inappropriate sales promotion of infant foods that can be used to replace breast milk.
- 2A doctor prescription is needed only for special formula that pharmacies dispense under the request of a doctor (personal communication with Dr. Mona Alsumaie, Kuwait Breastfeeding Promotion & Baby Friendly Hospital Initiative (BFHI) Implementation Program Coordinator).
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).