Diagnostic Practices and Treatment for P. vivax in the InterEthnic Therapeutic Encounter of South-Central Vietnam: A Mixed-Methods Study
Abstract
:1. Introduction
2. Materials and Methods
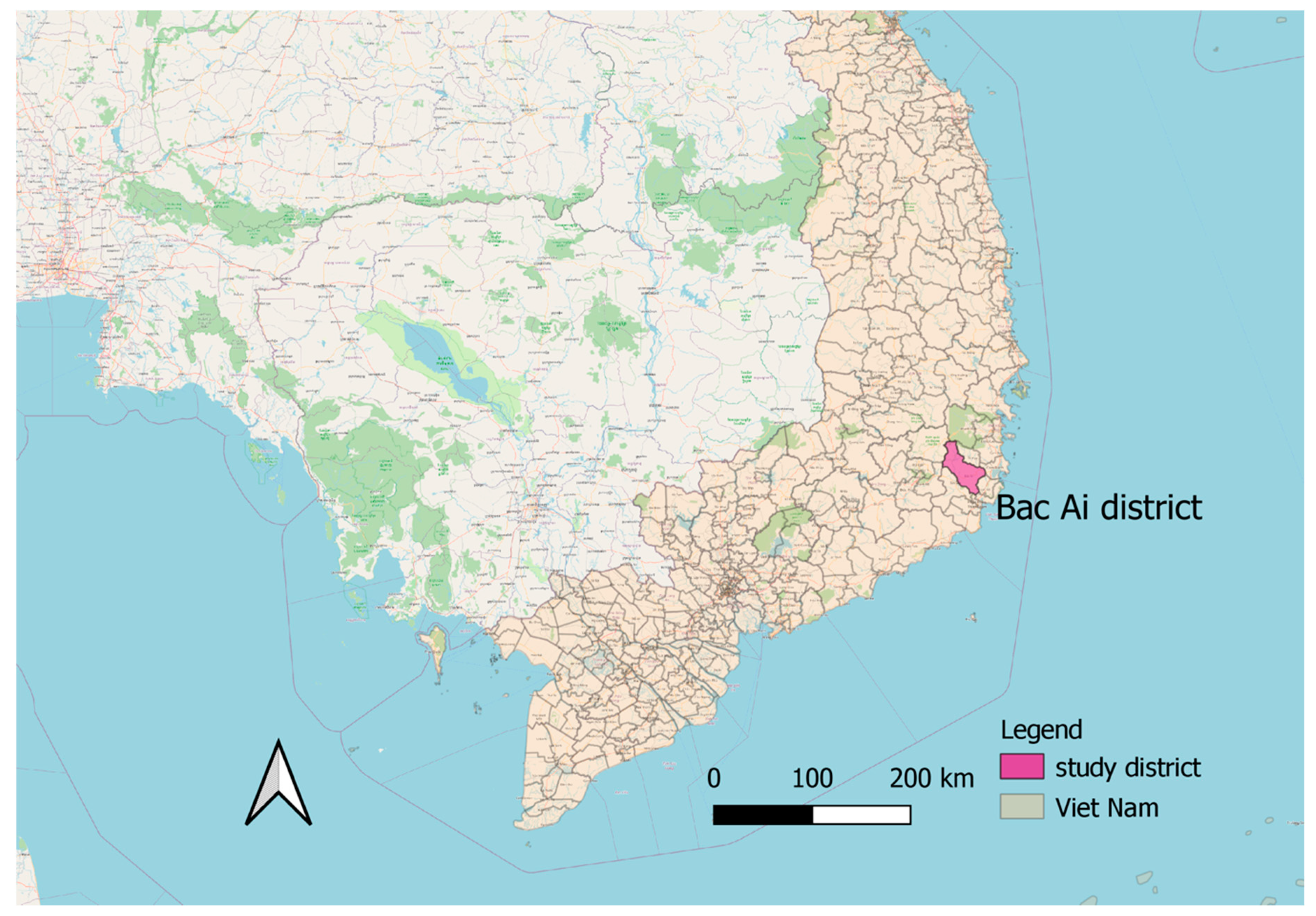
2.1. Study Site and Population
2.2. Study Design
2.2.1. Qualitative Strands
2.2.2. Quantitative Strand
2.3. Ethical Considerations
3. Results
3.1. Respondent Characteristics
3.2. Community Perceptions of P. vivax Malaria and Its Treatment
3.2.1. Perceived Malaria Types
3.2.2. Perceived Malaria Aetiology
3.2.3. Perceptions of Appropriate Malaria Treatment
3.3. G6PD Testing and Malaria Diagnostics
3.3.1. Healthcare Staff Perceptions of G6PD Testing
3.3.2. Healthcare Staff Diagnostic Practices for Malaria
3.3.3. Patient Perceptions of Malaria Diagnostics
3.4. Factors Determining the Use of Appropriate Malaria Treatment
3.4.1. Provider Challenges with Radical Cure
3.4.2. Trust in Healthcare Providers
3.4.3. Inter-Ethnic Health Encounters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. World Malaria Report Geneva. Available online: https://www.who.int/publications-detail/world-malaria-report-2019 (accessed on 31 December 2020).
- Mendis, K.; Marchesini, P.; Carter, R.; Sina, B.J. The neglected burden of Plasmodium vivax malaria. Am. J. Trop. Med. Hyg. 2001, 64, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Baird, J.K. Asia-Pacific malaria is singular, pervasive, diverse and invisible. Int. J. Parasitol. 2017, 47, 371–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, N.; Shukla, M.M.; Sharma, V.P. Epidemiology of malaria in pregnancy in central India. Bull. World Health Organ. 1999, 77, 567–572. [Google Scholar] [PubMed]
- Nosten, F.H.; Mcgready, R.; Simpson, J.A.; Thwai, K.L.; Balkan, S.; Cho, T.; Hkirijaroen, L.; Looareesuwan, S.; White, N.J. Effects of Plasmodium vivax malaria in pregnancy. Lancet 1999, 354, 546–549. [Google Scholar] [CrossRef]
- Price, R.N.; Anstey, N.M.; Guerra, C.A.; Yeung, S.; Tjitra, E.; White, N.J. Vivax Malaria: Neglected and Not Benign. Am. J. Trop. Med. Hyg. 2007, 77, 79–87. [Google Scholar] [CrossRef]
- Naing, C.; Whittaker, M.A.; Wai, V.N.; Mak, J.W. Is Plasmodium vivax Malaria a Severe Malaria?: A Systematic Review and Meta-Analysis. PLoS Negl. Trop. Dis. 2014, 8, e3071. [Google Scholar] [CrossRef]
- WHO. Strategy for Malaria Elimination in the Greater Mekong Subregion (2015–2030). 2015. Available online: https://iris.wpro.who.int/bitstream/handle/10665.1/10945/9789290617181_eng.pdf (accessed on 31 December 2020).
- MOH Vietnam. National Strategy for Malaria Control and Elimination from 2011 to 2020 with direction to 2030. 2011. Available online: http://www2.chinhphu.vn/portal/page/portal/chinhphu/noidungchienluocphattrienkinhtexahoi?_piref33_14725_33_14721_14721.strutsAction=ViewDetailAction.do&_piref33_14725_33_14721_14721.docid=1160&_piref33_14725_33_14721_14721.substract= (accessed on 31 December 2020).
- Price, R.N.; Commons, R.J.; Battle, K.E.; Thriemer, K.; Mendis, K. Plasmodium vivax in the Era of the Shrinking, P. falciparum Map. Trends Parasitol. 2020, 36, 560–570. [Google Scholar] [CrossRef]
- Geng, J.; Malla, P.; Zhang, J.; Xu, S.; Li, C.; Zhao, Y. Increasing trends of malaria in a border area of the Greater Mekong Sub-region. Malar. J. BioMed Cent. Ltd. 2019, 18, 309. [Google Scholar]
- Sattabongkot, J.; Tsuboi, T.; Zollner, G.E.; Sirichaisinthop, J.; Cui, L. Plasmodium vivax transmission: Chances for control? Trends Parasitol. 2004, 20, 192–198. [Google Scholar] [CrossRef]
- Vietnamese National Institute of Malaria, Parasitology and Entomology in Hanoi. Annual Report 2010. 2010; (Internal report). [Google Scholar]
- Vietnamese National Institute of Malaria, Parasitology and Entomology in Hanoi. Annual Report 2019. 2019; (Internal report). [Google Scholar]
- Baird, J.K.; Maguire, J.D.; Price, R.N. Diagnosis and Treatment of Plasmodium vivax Malaria. Haemonchus Contortus Haemonchosis Past Present Future Trends 2012, 80, 203–270. [Google Scholar] [CrossRef] [Green Version]
- Chen, N.; Auliff, A.; Rieckmann, K.; Gatton, M.L.; Cheng, Q. Relapses ofPlasmodium vivaxInfection Result from Clonal Hypnozoites Activated at Predetermined Intervals. J. Infect. Dis. 2007, 195, 934–941. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imwong, M.; Snounou, G.; Pukrittayakamee, S.; Tanomsing, N.; Kim, J.R.; Nandy, A.; Guthmann, J.; Nosten, F.; Carlton, J.; Looareesuwan, S.; et al. Relapses of Plasmodium vivax Infection Usually Result from Activation of Heterologous Hypnozoites. J. Infect. Dis. 2007, 195, 927–933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, N.J. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar. J. 2011, 10, 297. [Google Scholar] [CrossRef] [Green Version]
- Silachamroon, U.; Krudsood, S.; Treeprasertsuk, S.; Wilairatana, P.; Chalearmrult, K.; Mint, H.Y.; Maneekan, P.; White, N.J.; Gourdeuk, V.R.; Brittenham, G.M.; et al. Clinical Trial of Oral Artesunate With or Without High-Dose Primaquine for the Treatment of Vivax Malaria in Thailand. Am. J. Trop. Med. Hyg. 2003, 69, 14–18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Llanos-Cuentas, A.; Lacerda, M.V.; Hien, T.T.; Vélez, I.D.; Namaik-Larp, C.; Chu, C.S.; Villegas, M.F.; Val, F.; Monteiro, W.M.; Brito, M.A.; et al. Tafenoquine versus Primaquine to Prevent Relapse of Plasmodium vivax Malaria. N. Engl. J. Med. 2019, 380, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Galappaththy, G.N.L.; Tharyan, P.; Kirubakaran, R. Primaquine for preventing relapse in people with Plasmodium vivax malaria treated with chloroquine. Cochrane Database Syst. Rev. 2013, 10, CD004389. [Google Scholar] [CrossRef]
- Khantikul, N.; Butraporn, P.; Kim, H.S.; Leemingsawat, S.; Tempongko, M.S.B.; Suwonkerd, W. Adherence to Antimalarial Drug Therapy among Vivax Malaria Patients in Northern Thailand. J. Heal Popul. Nutr. 2009, 27, 4–13. [Google Scholar] [CrossRef] [Green Version]
- Douglas, N.M.; Poespoprodjo, J.R.; Patriani, D.; Malloy, M.J.; Kenangalem, E.; Sugiarto, P.; Simpson, J.A.; Soenarto, Y.; Anstey, N.M.; Price, R.N. Unsupervised primaquine for the treatment of Plasmodium vivax malaria relapses in southern Papua: A hospital-based cohort study. PLoS Med. 2017, 14, e1002379. [Google Scholar] [CrossRef] [Green Version]
- Baird, J.K. Real-world therapies and the problem of vivax malaria. N. Engl. J. Med. 2008, 359, 2601–2603. [Google Scholar] [CrossRef] [Green Version]
- Rollinson, D.; Hay, S.I. Advances in Parasitology; Academic Press: New York, NY, USA, 2012. [Google Scholar]
- Ley, B.; Luter, N.; Espino, F.E.; Devine, A.; Kalnoky, M.; Lubell, Y.; Thriemer, K.; Baird, J.K.; Poirot, E.; Conan, N.; et al. The challenges of introducing routine G6PD testing into radical cure: A workshop report. Malar. J. 2015, 14, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Chu, C.S.; Freedman, O.; Tafenoquine, D. G6PD: A Primer for Clinicians. J. Travel Med. 2019, 26. [Google Scholar] [CrossRef] [Green Version]
- Commons, R.J.; McCarthy, J.S.; Price, R.N. Tafenoquine for the radical cure and prevention of malaria: The importance of testing for G6PD deficiency. Med. J. Aust. 2020, 212, 152–153.e1. [Google Scholar] [CrossRef] [PubMed]
- WHO. Guidelines for the Treament of Malaria, 3rd ed.; Olumese, P., Ed.; WHO: Geneva, Switzerland, 2015; Available online: http://apps.who.int/iris/bitstream/10665/162441/1/9789241549127_eng.pdf (accessed on 28 April 2020).
- Domingo, G.J.; Satyagraha, A.W.; Anvikar, A.R.; Baird, J.K.; Bancone, G.; Bansil, P.; Carter, N.; Cheng, Q.; Culpepper, J.; Eziefula, A.C.; et al. G6PD testing in support of treatment and elimination of malaria: Recommendations for evaluation of G6PD tests. Malar. J. 2013, 12, 391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LaRue, N.; Kahn, M.; Murray, M.; Leader, B.T.; Bansil, P.; McGray, S.; Kalnoky, M.; Zhang, H.; Huang, H.; Jiang, H.; et al. Comparison of quantitative and qualitative tests for glu-cose-6-phosphate dehydrogenase deficiency. Am. J. Trop. Med. Hyg. 2014, 91, 854–861. [Google Scholar] [CrossRef]
- Ley, B.; Bancone, G.; Von Seidlein, L.; Thriemer, K.; Richards, J.S.; Domingo, G.J.; Price, R.N. Methods for the field evaluation of quantitative G6PD diagnostics: A review. Malar. J. 2017, 16, 1–9. [Google Scholar] [CrossRef]
- Vietnamese Ministry of Health. Guidelines on Diagnosis, Treatment for Malaria. 2016. Available online: https://thuvienphapluat.vn/van-ban/The-thao-Y-te/Quyet-dinh-4845-QD-BYT-Huong-dan-chan-doan-dieu-tri-benh-Sot-ret-2016-321533.aspx (accessed on 31 December 2020).
- Thriemer, K.; Ley, B.; Bobogare, A.; Lek, S.; Alam, M.S.; Pasaribu, A.P.; Sattabongkot, J.; Jambert, E.; Domingo, G.J.; Commons, R.J.; et al. Challenges for achieving safe and effective radical cure of Plasmodium vivax: A round table discussion of the APMEN Vivax Working Group. Malar. J. 2017, 16, 141. [Google Scholar] [CrossRef] [Green Version]
- Gryseels, C.; Uk, S.; Erhart, A.; Gerrets, R.; Sluydts, V.; Durnez, L.; Ribera, J.M.; Muela, S.H.; Menard, D.; Heng, S.; et al. Injections, Cocktails and Diviners: Therapeutic Flexibility in the Context of Malaria Elimination and Drug Resistance in Northeast Cambodia. PLoS ONE 2013, 8, e80343. [Google Scholar] [CrossRef]
- Grietens, K.P.; Xuan, X.N.; Ribera, J.M.; Duc, T.N.; Van Bortel, W.; Ba, N.T.; Van, K.P.; le Xuan, H.; D’Alessandro, U.; Erhart, A. Social determinants of long lasting insecticidal ham-mock-use among the Ra-Glai ethnic minority in Vietnam: Implications for forest malaria control. PLoS ONE 2012, 7, e29991. [Google Scholar]
- Gryseels, C.; Grietens, K.P.; Dierickx, S.; Xuan, X.N.; Uk, S.; Bannister-Tyrrell, M.; Trienekens, S.; Ribera, J.M.; Hausmann-Muela, S.; Gerrets, R.; et al. High Mobility and Low Use of Malaria Preventive Measures among the Jarai Male Youth along the Cambodia-Vietnam Border. Am. J. Trop. Med. Hyg. 2015, 93, 810–818. [Google Scholar] [CrossRef] [Green Version]
- Grietens, K.P.; Gryseels, C.; Dierickx, S.; Bannister-Tyrrell, M.; Trienekens, S.; Uk, S.; Phoeuk, P.; Suon, S.; Set, S.; Gerrets, R.; et al. Characterizing Types of Human Mobility to Inform Differential and Targeted Malaria Elimination Strategies in Northeast Cambodia. Sci. Rep. 2015, 5, 16837. [Google Scholar] [CrossRef] [Green Version]
- Bannister-Tyrrell, M.; Gryseels, C.; Suon, S.; Dara, L.; Sereiboth, N.; James, N.; Thavrin, B.; Ly, P.; Ty, K.S.; Grietens, K.P.; et al. Forest Goers and Multidrug-Resistant Malaria in Cambodia: An Ethnographic Study. Am. J. Trop. Med. Hyg. 2019, 100, 1170–1178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peeters, G.K.; Xuan, X.N.; Van Bortel, W.; Duc, T.N.; Ribera, J.M.; Nhat, T.B.; Van, K.P.; Le Xuan, H.; D’Alessandro, U.; Erhart, A. Low perception of malaria risk among the Ra-glai ethnic minority in south-central Vietnam: Implications for forest malaria control. Malar. J. BioMed Central 2010, 9, 23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morel, C.M.; Thang, N.D.; Erhart, A.; Xa, N.X.; Peeters Grietens, K.; Hung, L.X.; Thuan, L.K.; van Ky, P.; Hung, N.M.; Coosemans, M.; et al. Cost-Effectiveness of Long-Lasting Insecti-cide-Treated Hammocks in Preventing Malaria in South-Central Vietnam. PLoS ONE 2013, 8, e58205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koen, P.G.; Charlotte, G.G.V. Misdirection in the margins of malaria elimination methods. Crit. Public Health 2019, 29, 390–400. [Google Scholar]
- Thuan Thi Nguyen (National Institute of Malariology, Parasitology and Entomology, Hanoi, Vietnam and Institute of Tropi-cal Medicine, Antwerp, Belgium). Unpublished work. 2020.
- Quy Nhon Institute of Malaria Parasitology and Entomology. Malaria Situation Report, Central Highlands Region. 2019; (Internal Report). [Google Scholar]
- Quy Nhon Institute of Malariology Parasitology and Entomology. Annual Report on Malaria in Central Region of Vietnam 2009–2019. 2019; (Internal Report). [Google Scholar]
- Bancone, G.; Menard, D.; Khim, N.; Kim, S.; Canier, L.; Chea, N.; Phommasone, K.; Mayxay, M.; Dittrich, S.; Vongsouvath, M.; et al. Molecular characterization and mapping of glucose-6-phosphate dehydrogenase (G6PD) mutations in the Greater Mekong Subregion. Malar. J. 2019, 18, 20. [Google Scholar] [CrossRef]
- Ngo, T.D.; Erhart, A.; Speybroeck, N.; Hung, L.X.; Thuan, L.K.; Hung, C.T.; Van Ky, P.; Coosemans, M.; D’Alessandro, U. Malaria in central Vietnam: Analysis of risk factors by multivariate analysis and classification tree models. Malar. J. 2008, 7, 28. [Google Scholar] [CrossRef] [Green Version]
- Ngo, T.D.; Erhart, A.; Speybroeck, N.; Xa, N.X.; Thanh, N.N.; Van Ky, P.; Hung, L.X.; Thuan, L.K.; Coosemans, M.; D’Alessandro, U. Long-Lasting Insecticidal Hammocks for Controlling Forest Malaria: A Community-Based Trial in a Rural Area of Central Vietnam. PLoS ONE 2009, 4, e7369. [Google Scholar] [CrossRef] [Green Version]
- Statistical Publishing House. Ninh Thuan Statistical Yearbook 2018 (Nien giam thong ke tinh Ninh Thuan 2018). 2018; (Internal Publication, in Vietnamese language). [Google Scholar]
- Ninh Thuan Provincial People’s Committee. Decision on resettlement of ethnic minority groups living in Ninh Thuan province from 2006–2010. 2007; (Internal report, in Vietnamese). [Google Scholar]
- Maya Ronse (Institute of Tropical Medicine, Antwerp, Belgium). Unpublished work. 2020.
- OCHA. Vietnam Subnational Administrative Boundaries. 2020. Available online: https://data.humdata.org/dataset/viet-nam-administrative-boundaries-polygon-polyline (accessed on 31 December 2020).
- Morse, J.M. Janice Example of Methods. Nurs. Res. 1991, 40, 120–123. [Google Scholar]
- Ivankova, N.V.; Creswell, J.W.; Stick, S.L. Using mixed-methods sequential explanatory design: From theory to practice. Field Methods 2006, 18, 3–20. [Google Scholar] [CrossRef]
- Jaccard, J.; Jacoby, J. Theory Construction and Model-Building; The Guilford Press: New York, NY, USA, 2010; pp. 256–283. [Google Scholar]
- Code of Ethics of the American Anthropological Association. 1998. Available online: http://s3.amazonaws.com/rdcms-aaa/files/production/public/FileDownloads/pdfs/issues/policy-advocacy/upload/ethicscode.pdf (accessed on 31 December 2020).
- Ley, B.; Satyagraha, A.W.; Rahmat, H.; Von Fricken, M.E.; Douglas, N.M.; Pfeffer, D.A.; Espino, F.; von Seidlein, L.; Henriques, G.; Oo, N.N.; et al. Performance of the Access Bio/CareStart rapid diagnostic test for the detection of glucose-6-phosphate dehydrogenase deficiency: A systematic review and meta-analysis. PLoS Med. 2019, 13, e1002992. Available online: https://pubmed.ncbi.nlm.nih.gov/31834890/ (accessed on 31 December 2020). [CrossRef] [PubMed] [Green Version]
- Erhart, A.; Ngo, T.D.; Van Ky, P.; Tinh, T.T.; Van Overmeir, C.; Speybroeck, N.; Obsomer, V.; Hung, L.X.; Thuan, L.K.; Coosemans, M.; et al. Epidemiology of forest malaria in central Vietnam: A large scale cross-sectional survey. Malar. J. 2005, 4, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thanh, D.T.; Van Hong, N.; Van Nguyen, V.; Van Malderen, C.; Obsomer, V.; Rosanas-Urgell, A.; Grietens, K.P.; Xa, N.X.; Bancone, G.; Chowwiwat, N.; et al. Epidemiology of forest malaria in Central Vietnam: The hidden parasite reservoir. Malar. J. 2015, 14, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Cheng, Q.; Cunningham, J.; Gatton, M.L. Systematic Review of Sub-microscopic P. vivax Infections: Prevalence and Determining Factors. PLoS Neglected Trop. Dis. 2015, 9, e3413. [Google Scholar] [CrossRef] [Green Version]
- Bell, D.L.; Peeling, R.W. Evaluation of rapid diagnostic tests: Malaria. Nat. Rev. Genet. 2006, 4, S34–S38. [Google Scholar] [CrossRef]
- Coleman, R.E.; Thimasarn, K.; Kumpitak, C.; Soyseng, V.; Maneechai, N.; Sattabongkot, J.; Miller, R.S.; Rachapaew, N. Field evaluation of the ICT Malaria Pf/Pv immunochromatographic test for the detection of asymptomatic malaria in a Plasmodium falciparum/vivax endemic area in Thailand. Am. J. Trop. Med. Hyg. 2002, 66, 379–383. [Google Scholar] [CrossRef] [Green Version]
- Feenberg, A. The Handbook of Science and Technology Studies, 4th ed.; Felt, U., Fouché, R., Miller, C.A., Smith-Doerr, L., Eds.; The MIT Press: Chicago, IL, USA, 2017. [Google Scholar]
- Commons, R.J.; Simpson, J.; Thriemer, K.; Hossain, M.S.; Douglas, N.M.; Humphreys, G.S.; Sibley, C.H.; Guerin, P.J.; Price, R.N. Risk of Plasmodium vivax parasitaemia after Plasmodium falciparum infection: A systematic review and meta-analysis. Lancet Infect. Dis. 2019, 19, 91–101. [Google Scholar] [CrossRef] [Green Version]
- Forsyth, T.; Michaud, J. Rethinking the Relationships between Livelihoods and Ethnicity in Highland China, Vietnam, and Laos. In Moving mountains: Ethnicity and livelihoods in highland China, Vietnam, and Laos; UBC Press: Vancouver, BC, Canada, 2011; pp. 1–27. [Google Scholar]
- McKinnon, K. Southeast Asia. Civilizing the margins: Southeast Asian government policies for the development of minorities. Edited by Christopher R. Duncan. Singapore: NUS Press, 2008. Pp. 284. Index. J. Southeast Asian Stud. 2012, 43, 186. Available online: http://www.journals.cambridge.org/abstract_S0022463411000737 (accessed on 31 December 2020).
- Vigh, H. Motion squared. Anthr. Theory 2009, 9, 419–438. [Google Scholar] [CrossRef]
- Castel, P. Vietnam Health insurance Use of health care services by the poor efficiency and equity issues in the province of Kon Tum. SSRN Electron. J. 2011. Available online: http://ssrn.com/abstract=1461327 (accessed on 31 December 2020). [CrossRef] [Green Version]
- Ekman, B.; Liem, N.T.; Duc, H.A.; Axelson, H. Health insurance reform in Vietnam: A review of recent developments and future challenges. Health Policy Plan. 2008, 23, 252–263. [Google Scholar] [CrossRef] [Green Version]
- Wagstaff, A. Health Insurance for the Poor: Initial Impacts of Vietnam’s Health Care Fund for the Poor. The World Bank. 2007. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=961760 (accessed on 28 April 2020).
- Palmer, M. Inequalities in Universal Health Coverage: Evidence from Vietnam. SSRN Electron. J. 2014, 64, 384–394. [Google Scholar] [CrossRef]
| Frequency (n) | Proportion (%) | |
|---|---|---|
| Household representatives included in the cross-sectional survey (N = 202) | ||
| Sex | ||
| - Male | 91 | 45.1 |
| - Female | 111 | 54.9 |
| Median of age (range), IQR | 40 (14; 73); IQR (18; 68) | |
| Ethnicity | ||
| - Ra-glai | 199 | 98.5 |
| - Kinh | 3 | 1.5 |
| Religion | ||
| - Christianity | 5 | 2.5 |
| - Animism | 196 | 97.0 |
| - Buddhism | 1 | 0.5 |
| Occupations (multiple replies possible) | ||
| - Sedentary farming | 149 | 73.8 |
| - Rotational farming | 174 | 86.1 |
| - Seasonal plantation work | 137 | 67.8 |
| Median of days being away from home for work (n = 180) | 6 (min = 1; max = 90); IQR (1; 60) | |
| Patients enrolled in the health-facility based survey (N = 176) | ||
| Sex | ||
| - Male | 62 | 35.2 |
| - Female | 114 | 64.8 |
| Ra-glai ethnicity | 176 | 100 |
| Median of age (range, IQR) | 30 (2; 77), IQR (5; 64) | |
| n | % | |
|---|---|---|
| Household representatives included in the cross-sectional survey (N = 202) | ||
| Has not heard about different types of malaria | 153 | 75.7 |
| Knows about ‘hidden’ (asymptomatic) malaria | 44 | 21.8 |
| Knows about the possibility of relapses | 60 | 29.7 |
| Did not think a person could have malaria without having symptoms | 105 | 52.0 |
| Perceived causes of relapse (n = 60) | ||
| - Did not complete medicine | 4 | 6.7 |
| - Incorrect treatment | 2 | 3.3 |
| - Drinking dirty water | 1 | 1.7 |
| - Going/sleeping in the forest | 22 | 36.7 |
| - Staying in the old village | 10 | 16.7 |
| - Polluted environment | 1 | 1.7 |
| - Mosquito bites | 21 | 35.0 |
| - Parasites (“ký sinh trùng”, “ana hula”, “sâu”) | 29 | 48.3 |
| - Weak body | 1 | 1.7 |
| - Do not know | 12 | 20.0 |
| Patients enrolled in the health-facility based survey (N = 176) | ||
| Positive malaria results (using conventional RDT) | 8 | 4.6 |
| Positive for P. vivax (using microscopy) | 2 | 1.1 |
| Has heard about the two common types of malaria (vivax and falciparum) | 10 | 5.7 |
| Thinks that each type of malaria has different symptoms | 7 | 4.0 |
| Thinks that falciparum causes more severe symptoms | 3 | 1.7 |
| Suspects their fever was caused by malaria | 21 | 11.9 |
| Patients who report to have been infected with malaria in the past | 7 | 4.0 |
| Patients who suspected their current fever was caused by a relapse of that past malaria episode (n = 7) | 1 | 14.3 |
| Free Response | Prompted Response | |||
|---|---|---|---|---|
| n | % | n | % | |
| Reported common fevers | ||||
| - Viral fever | 3 | 1.5 | 18 | 8.9 |
| - Influenza | 122 | 60.4 | 195 | 96.5 |
| - Malaria | 64 | 31.7 | 168 | 83.2 |
| - Fever caused by pollution | 1 | 0.5 | 173 | 85.6 |
| - Fever caused by the weather | 0 | 0 | 7 | 3.5 |
| - Fever caused by contaminated food | 0 | 0 | 32 | 15.8 |
| - Dengue fever | 7 | 3.5 | 1 | 0.5 |
| - Other (diarrhoea, fatigue, stomach pain) | 5 | 2.5 | 37 | 18.3 |
| - Do not know | 48 | 23.8 | 7 | 3.5 |
| - No answer | 1 | 0.5 | 9 | 4.5 |
| Perceived causes of malaria (multiple choice) | ||||
| - Drinking dirty water | 1 | 0.5 | 33 | 16.3 |
| - Going/sleeping in the forest | 91 | 45.1 | 180 | 89.1 |
| - Being in the rain | 4 | 2.0 | 14 | 6.9 |
| - Staying in the old village | 44 | 21.8 | 157 | 77.7 |
| - Hot weather | 0 | 0 | 0 | 0 |
| - Polluted environment | 2 | 1.0 | 37 | 18.3 |
| - Poor personal hygiene | 0 | 0 | 14 | 6.9 |
| - Dirty house | 0 | 0 | 3 | 1.5 |
| - Virus/viruses | 1 | 0.5 | 1 | 0.04 |
| - Mosquito bites | 148 | 73.3 | 181 | 89.6 |
| - Parasites (“ký sinh trùng”, “ana hula”, “sâu”) | 1 | 0.5 | 43 | 21.3 |
| - Insects in the forest/water | 4 | 1.2 | 59 | 28.2 |
| - Other (working away from home, not sleeping under a net, climate change) | 3 | 1.5 | 3 | 1.5 |
| - Do not know | 32 | 15.8 | 26 | 12.9 |
| - No answer | 1 | 0.5 | 1 | 0.5 |
| Perceived symptoms of malaria (multiple choice) | ||||
| - Fever | 146 | 72.6 | 192 | 95.5 |
| - Dizzy | 3 | 1.5 | 100 | 49.8 |
| - Chills | 130 | 64.7 | 189 | 94.0 |
| - Headache | 26 | 12.9 | 171 | 85.1 |
| - Body pain | 5 | 2.5 | 58 | 28.9 |
| - Insomnia | 3 | 1.5 | 27 | 13.4 |
| - Vomit | 1 | 0.5 | 20 | 10.0 |
| - Stiffness | 2 | 1.0 | 13 | 6.5 |
| - Lack of appetite | 0 | 0 | 10 | 5.0 |
| - Nausea | 0 | 0 | 19 | 9.5 |
| - Fatigue | 20 | 10.0 | 128 | 63.7 |
| - Unable to work | 0 | 0 | 1 | 0.5 |
| - Diarrhoea | 0 | 0 | 1 | 0.5 |
| - Hot body | 9 | 4.5 | 26 | 13.0 |
| - Difficult indigestion | 0 | 0 | 1 | 0.5 |
| - Cold body | 8 | 4.0 | 27 | 13.4 |
| - Other (coughing, sweat, yellow skin) | 0 | 4 | 2.0 | |
| - Do not know | 40 | 19.9 | 13 | 6.5 |
| - No answer | 1 | 0.5 | 0 | 0 |
| n | % | |
|---|---|---|
| Thinks a person can be infected with malaria whilst showing no symptoms (asymptomatic infection) | ||
| - No | 105 | 52.0 |
| - Yes | 44 | 21.8 |
| - Do not know | 52 | 25.7 |
| - No answer | 1 | 0.5 |
| Perceived the necessity of treatment for asymptomatic infection (given being prescribed by a health worker) | ||
| - Not necessary | 2 | 1.0 |
| - Necessary | 190 | 94.1 |
| - Do not know | 9 | 4.5 |
| - No answer | 1 | 0.5 |
| Reported importance of adherence to treatment (N = 202) | ||
| - Patients should continue taking all medicine even when better | 185 | 91.5 |
| - Patients should stop taking medicine when feeling better | 10 | 5.0 |
| - Do not know | 6 | 3.0 |
| - No answer | 1 | 0.5 |
| Use of malaria treatment during last self-reported malaria episode (N = 21) | ||
| Sought treatment from CHC first | 21 | 100 |
| Received treatment from CHC during last malaria episode | 19 | 90.5 |
| Received different types of pills during last malaria episode | 3 | 14.3 |
| Reported treatment regime | ||
| Do not remember | 10 | 47.6 |
| 1 day | 4 | 19.0 |
| 3 days | 3 | 14.3 |
| 5 days | 3 | 14.3 |
| 10 day | 1 | 4.8 |
| Received supplements to malaria treatment | 14 | 66.7 |
| Types of supplement (n = 14, multiple responses) | ||
| - Injection | 1 | 7.1 |
| - IV drips | 13 | 92.9 |
| - Spiritual sacrifice | 2 | 14.3 |
| n | % | |
|---|---|---|
| Self-reported past malaria infection | 21 | 10.4 |
| Malaria diagnosis at health facility during last malaria episode (n = 21) (multiple choice) | ||
| RDT | 21 | 100 |
| RDT, then microscopy | 12 | 57.1 |
| RDT, then unknown | 4 | 19.0 |
| Median days from onset malaria symptoms to seeking diagnosis and treatment | 3 (min = 1; max = 4), IQR (2; 4) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, T.T.; Nguyen, X.X.; Ronse, M.; Nguyen, Q.T.; Ho, P.Q.; Tran, D.T.; Gerrets, R.; Thriemer, K.; Ley, B.; Marfurt, J.; et al. Diagnostic Practices and Treatment for P. vivax in the InterEthnic Therapeutic Encounter of South-Central Vietnam: A Mixed-Methods Study. Pathogens 2021, 10, 26. https://doi.org/10.3390/pathogens10010026
Nguyen TT, Nguyen XX, Ronse M, Nguyen QT, Ho PQ, Tran DT, Gerrets R, Thriemer K, Ley B, Marfurt J, et al. Diagnostic Practices and Treatment for P. vivax in the InterEthnic Therapeutic Encounter of South-Central Vietnam: A Mixed-Methods Study. Pathogens. 2021; 10(1):26. https://doi.org/10.3390/pathogens10010026
Chicago/Turabian StyleNguyen, Thuan Thi, Xa Xuan Nguyen, Maya Ronse, Quynh Truc Nguyen, Phuc Quang Ho, Duong Thanh Tran, Rene Gerrets, Kamala Thriemer, Benedikt Ley, Jutta Marfurt, and et al. 2021. "Diagnostic Practices and Treatment for P. vivax in the InterEthnic Therapeutic Encounter of South-Central Vietnam: A Mixed-Methods Study" Pathogens 10, no. 1: 26. https://doi.org/10.3390/pathogens10010026






