Molecular Characterization of Fluoroquinolone-Resistant Bartonella bacilliformis
Abstract
1. Introduction
2. Results
2.1. Classification of the Isolates
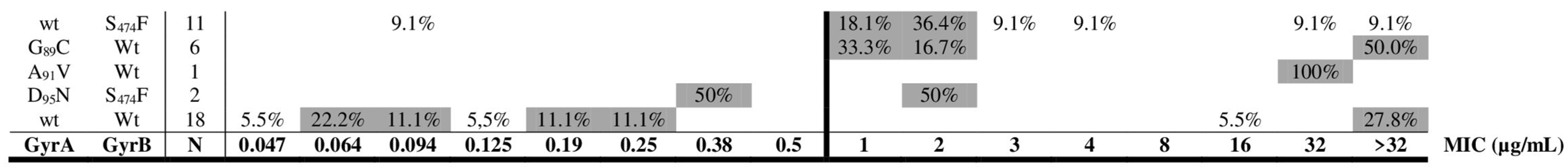
2.2. Mechanisms of Resistance to Quinolones and Chloramphenicol
3. Discussion
4. Materials and Methods
4.1. Microorganisms
4.2. Antibiotic Susceptibility
4.3. DNA Extraction
4.4. Molecular Analysis of Antibiotic Targets
4.5. DNA Sequencing
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gomes:, C.; Ruiz, J. Carrion’s disease. The sound of silence. Clin. Microb. Rev. 2018, 31, e00056-17. [Google Scholar] [CrossRef]
- Chamberlin, J.; Laughlin, L.W.; Romero, S.; Solórzano, N.; Gordon, S.; Andre, R.G.; Pachas, P.; Friedman, H.; Ponce, C.; Watts, D. Epidemiology of endemic Bartonella bacilliformis: A prospective cohort study in a Peruvian mountain valley community. J. Infect. Dis. 2002, 186, 983–990. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.; Palma, N.; Pons, M.J.; Magallón-Tejada, A.; Sandoval, I.; Tinco-Valdez, C.; Gutarra, C.; del Valle-Mendoza, J.; Ruiz, J.; Matsuoka, M. Succinyl-CoA synthetase: New antigen candidate of Bartonella bacilliformis. PLoS Negl. Trop. Dis. 2016, 10, e0004989. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.; Pons, M.J. Revisiting Bartonella bacilliformis MLST. Infect. Genet. Evol. 2018, 63, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.; Minnick, M.F.; Chattopadhyay, S. Mutation-driven divergence and convergence indicate adaptive evolution of the intracellular human-restricted pathogen, Bartonella bacilliformis. PLoS Negl. Trop. Dis. 2016, 10, e0004712. [Google Scholar] [CrossRef] [PubMed]
- Loparev, V.N.; Dasch, G.A.; Knipe, K.M.; Rowe, L.A.; Lydy, S.L. Optical mapping and genome sequences of isolates of Bartonella bacilliformis. In Proceedings of the Program and Abstracts Book of International Conference on Emerging Infectious Diseases, Atlanta, GA, USA, 24–26 August 2015; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015; p. 6. [Google Scholar]
- Amano, Y.; Rumbea, J.; Knobloch, J.; Olson, J.; Kron, M. Bartonellosis in Ecuador: Serosurvey and current status of cutaneous verrucous disease. Am. J. Trop Med. Hyg. 1997, 57, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.; Pons, M.J.; del Valle, M.J.; Ruiz, J. Carrion’s disease: An eradicable illness? Infect. Dis Poverty 2016, 5, 105. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ellis, B.A.; Rotz, L.D.; Leake, J.A.; Samalvides, F.; Bernable, J.; Ventura, G.; Padilla, C.; Villaseca, P.; Beati, L.; Regnery, R.; et al. An outbreak of acute bartonellosis (Oroya fever) in the Urubamba region of Peru, 1998. Am. J. Trop. Med. Hyg. 1999, 61, 344–349. [Google Scholar] [CrossRef]
- Patiño-Camargo, L. Fiebre verrucosa del Guaitara en Colombia. Rev. Fac. Med. 1952, 20, 657–705. [Google Scholar]
- Ticona, E.; Huaroto, L.; Garcia, Y.; Vargas, L.; Madariaga, M.G. The pathophysiology of the acute phase of human bartonellosis resembles AIDS. Med. Hypotheses 2010, 74, 45–49. [Google Scholar] [CrossRef]
- Maguiña, C.; García, P.J.; Gotuzzo, E.; Cordero, L.; Spach, D.H. Bartonellosis (Carrión’s disease) in the modern era. Clin. Infect. Dis. 2001, 33, 772–779. [Google Scholar] [CrossRef]
- Pachas, P.; Rojas, Y.; Solorzano, N.; Chiroque, J.; Chancafe, J.A.; Canal, E.; Suarez-Ognio, L.; Maguiña, M.; Tarazona, A.; Salazar, J.; et al. Persistence of bacteremia by Bartonella bacilliformis post treatment with cloranfenicol, Ancash, Peru. In Proceedings of the Abstracts of the 55th ASTMH Annual Meeting, Atlanta, GA, USA, 12–16 November 2006; p. 229. [Google Scholar]
- Mendoza-Mujica, G.; Flores-León, D. Resistencia antimicrobiana de cepas de Bartonella bacilliformis procedentes de regiones endémicas de la enfermedad de Carrión en el Perú. Rev. Peru. Med. Exp. Salud Publica 2015, 32, 659–666. [Google Scholar] [CrossRef][Green Version]
- Silva-Caso, W.; Pons, M.J.; Tinco, C.; Ruiz, J.; del Valle, J. Antibiotic resistance in Bartonella bacilliformis clinical isolates from an endemic area of Peru. J. Glob. Antimicrob. Resist. 2015, 3, 222–223. [Google Scholar] [CrossRef][Green Version]
- Sobraquès, M.; Maurin, M.; Birtles, R.J.; Raoult, D. In vitro susceptibilities of four Bartonella bacilliformis strains to 30 antibiotic compounds. Antimicrob. Agents Chemother. 1999, 43, 2090–2092. [Google Scholar] [CrossRef]
- Biswas, S.; Raoult, D.; Rolain, J.M. Molecular mechanisms of resistance to antibiotics in Bartonella bacilliformis. J. Antimicrob. Chemother. 2007, 59, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Del Valle, L.J.; Flores, L.; Vargas, M.; de la-Guarda, R.G.; Quispe, R.L.; Ibañez, Z.B.; Alvarado, D.; Ramírez, P.; Ruiz, J. Bartonella bacilliformis, endemic pathogen of the Andean region, is intrinsically resistant to quinolones. Int. J. Infect. Dis. 2010, 14, 506–510. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gomes, C.; Martínez-Puchol, S.; Ruiz-Roldán, L.; Pons, M.J.; del Valle, J.; Ruiz, J. Development and characterisation of highly antibiotic resistant Bartonella bacilliformis mutants. Sci. Rep. 2016, 6, 33584. [Google Scholar] [CrossRef] [PubMed]
- Minnick, M.F.; Wilson, Z.R.; Smitherman, L.S.; Samuels, D.S. gyrA mutations in ciprofloxacin-resistant Bartonella bacilliformis strains obtained in vitro. Antimicrob. Agents Chemother. 2003, 47, 383–386. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J. Mechanisms of resistance to quinolones: Target alterations, decreased accumulation and DNA gyrase protection. J. Antimicrob. Chemother. 2003, 51, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Vila, J.; Vargas, M.; Ruiz, J.; Corachan, M.; de Anta, M.T.J.; Gascón, J. Quinolone resistance in enterotoxigenic Escherichia coli causing diarrhea in travelers to India in comparison with other geographical areas. Antimicrob. Agents Chemother. 2000, 44, 1731–1733. [Google Scholar] [CrossRef]
- Angelakis, E.; Biswas, S.; Taylor, C.; Raoult, D.; Rolain, J.M. Heterogeneity of susceptibility to fluoroquinolones in Bartonella isolates from Australia reveals a natural mutation in gyrA. J. Antimicrob. Chemother. 2008, 61, 1252–1255. [Google Scholar] [CrossRef] [PubMed]
- Almahmoud, I.; Kay, E.; Schneider, D.; Maurin, M. Mutational paths towards increased fluoroquinolone resistance in Legionella pneumophila. J. Antimicrob. Chemother. 2009, 64, 284–293. [Google Scholar] [CrossRef] [PubMed]
- Bhatnagar, K.; Wong, A. The mutational landscape of quinolone resistance in Escherichia coli. PLoS ONE 2019, 14, e0224650. [Google Scholar] [CrossRef] [PubMed]
- Mouneimné, H.; Robert, J.; Jarlier, V.; Cambau, E. Type II topoisomerase mutations in ciprofloxacin-resistant strains of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 1999, 43, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Tanmoy, A.M.; Westeel, E.; De Bruyne, K.; Goris, J.; Rajoharison, A.; Sajib, M.S.I.; van Belkum, A.; Saha, S.K.; Komurian-Pradel, F.; Endtz, H.P. Salmonella enterica serovar Typhi in Bangladesh: Exploration of genomic diversity and antimicrobial resistance. mBio 2018, 9, e02112-18. [Google Scholar] [CrossRef] [PubMed]
- Weigel, L.M.; Anderson, G.J.; Tenover, F.C. DNA gyrase and topoisomerase IV mutations associated with fluoroquinolone resistance in Proteus mirabilis. Antimicrob. Agents Chemother. 2002, 46, 2582–2587. [Google Scholar] [CrossRef] [PubMed]
- Matrat, S.; Cambau, E.; Jarlier, V.; Aubry, A. Are all the DNA gyrase mutations found in Mycobacterium leprae clinical strains involved in resistance to fluoroquinolones? Antimicrob. Agents Chemother. 2008, 52, 745–747. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Romero, M.A.; Casadesús, J. Contribution of phenotypic heterogeneity to adaptive antibiotic resistance. Proc. Natl. Acad. Sci. USA 2014, 111, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Bogaki, M.; Nakamura, M.; Nakamura, S. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob. Agents Chemother. 1990, 34, 1271–1272. [Google Scholar] [CrossRef] [PubMed]
- Oppegard, L.M.; Streck, K.R.; Rosen, J.D.; Schwanz, H.A.; Drlica, K.; Kerns, R.J.; Hiasa, H. Comparison of in vitro activities of fluoroquinolone-like 2, 4- and 1, 3-diones. Antimicrob. Agents Chemother. 2010, 54, 3011–3014. [Google Scholar] [CrossRef] [PubMed]
- Lluque, A.; Riveros, M.; Prada, A.; Ochoa, T.J.; Ruiz, J. Virulence and antimicrobial resistance in Campylobacter spp. from a Peruvian pediatric cohort. Scientifica 2017, 2017, 7848926. [Google Scholar] [CrossRef]
- Pons, M.J.; Silva-Caso, W.; del Valle-Mendoza, J.; Ruiz, J. Multi-locus sequence typing of Bartonella bacilliformis DNA performed directly from blood of patients with Oroya’s fever during a Peruvian outbreak. PLoS Negl. Trop. Dis. 2016, 10, e0004391. [Google Scholar] [CrossRef] [PubMed]
- Gomes, C.; Martinez-Puchol, S.; Pons, M.J.; Bazán, J.; Tinco, C.; del Valle, J.; Ruiz, J. Evaluation of PCR approaches for detection of Bartonella bacilliformis in blood samples. PLoS Negl. Trop. Dis. 2016, 10, e0004529. [Google Scholar] [CrossRef] [PubMed]
- Smit, P.W.; Peeling, R.W.; Garcia, P.J.; Torres, L.L.; Pérez-Lu, J.E.; Moore, D.; Mabey, D. Dried blood spots for qPCR diagnosis of acute Bartonella bacilliformis infection. Am. J. Trop. Med. Hyg. 2013, 89, 988–990. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Flores, A.L.E. Estudios Moleculares en Bartonella bacilliformis Para el Control de la Enfermedad de Carrión. Master’s Thesis, Universidad Nacional Mayor de San Marcos, Lima, Peru, 2008. [Google Scholar]
- Espinoza-Culupú, A. Caracterización de las Regiones Determinantes de Resistencia a Antimicrobianos de Cepas de Bartonella bacilliformis de Zonas Endémicas del Perú. Master’s Thesis, Universidad Nacional Mayor de San Marcos, Lima, Peru, 2014. [Google Scholar]
- Hall, T.A. BioEdit: A user-friendly biological sequence alignment editor and analysis program for Windows 95/98/NT. Nucleic Acids Symp. Ser. 1999, 41, 95–98. [Google Scholar]
- Tamura, K.; Peterson, D.; Peterson, N.; Stecher, G.; Nei, M.; Kumar, S. MEGA5: Molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol. Biol. Evol. 2011, 28, 2731–2739. [Google Scholar] [CrossRef] [PubMed]

| subsp. 1 1 | subsp. 2 1 | |||||
|---|---|---|---|---|---|---|
| Cond044 2 | Peru18 3 | Other 4 | Ver097 | Other 4 | ||
| Ancash | Center | 1 | 1 | 1 5 | 6 | 4 6 |
| Cajamarca | North | 1 | 3 | |||
| Cusco | South | 19 | 1 7 | |||
| Piura | North | 1 | ||||
| GyrA | GyrB | |||||||
|---|---|---|---|---|---|---|---|---|
| N | MIC | 89 | 91 | 95 | 474 | Identity 1 | Region | |
| wt | --- | --- | G | A | D | S | ||
| 1 | 0.047 | --- | --- | --- | --- | V97 | A | |
| 4 | 0.064 | --- | --- | --- | --- | V97 (3), M1 (1) | A | |
| 2 | 0.094 | --- | --- | --- | --- | V97 (1), P18 (1) | A, Cu | |
| 1 | 0.094 | --- | --- | --- | F | P18 | Cu | |
| 1 | 0.125 | --- | --- | --- | --- | C044 | Cj | |
| 2 | 0.19 | --- | --- | --- | --- | V97 | A | |
| 2 | 0.25 | --- | --- | --- | --- | V97 (1), C044 (1) | A, P | |
| 1 | 0.38 | --- | --- | N | F | P18 | Cj | |
| 2 | 1 | C | --- | --- | --- | P18 | Cu | |
| 2 | 1 | --- | --- | --- | F | P18 | Cu | |
| 1 | 2 | C | --- | --- | --- | P18 | A | |
| 4 | 2 | --- | --- | --- | F | P18 | Cu | |
| 1 | 2 | --- | --- | N | F | P18 | Cu | |
| 1 | 3 | --- | --- | --- | F | P18 | Cu | |
| 1 | 4 | --- | --- | --- | F | P18 | Cu | |
| 1 | 16 | --- | --- | --- | --- | V97 | A | |
| 1 | 32 | --- | V | --- | --- | P18 | Cu | |
| 1 | 32 | --- | --- | --- | F | P18 | Cu | |
| 5 | >32 | --- | --- | --- | --- | V97 (1), C044 (1), P18 (2), M2 (1) | A, Cj, Cu | |
| 3 | >32 | C | --- | --- | --- | P18 | Cu | |
| 1 | >32 | --- | --- | --- | F | P18 | Cu | |
| Annealing | ||||||
|---|---|---|---|---|---|---|
| Primer | Sequence 5′-3′ | Target | Size 1 | °C | Sec | Ref |
| gyrA-F | GACCGATCTTACTCGACTACC | gyrA | 701 | 57 | 30 | [38] |
| gyrA-R | ATAAGCAGAACGGACACCAGA | |||||
| gyrB-F | ATGAAGGACTTTCAGCATGGC | gyrB | 766 | 59 | 30 | TS |
| gyrB-R | ATTGAAAGCACCAGCGATTG | |||||
| parC-F | AGAACTACGTTCTGCTTTGC | parC | 621 | 55 | 30 | TS |
| parC-R | AACCAAAATGCCACCTGTTG | |||||
| parE-F | AATAGGAAATAAGCGTGCCTCG | parE | 750 | 59 | 30 | TS |
| parE-R | TCTTTATGAGAATCGTCGCGT | |||||
| 23S rRNA-F | CAAGCATTGAATTGAAGCCCC | 23S rRNA | 1020 | 58 | 30 | TS |
| 23S rRNA-R | AATGAGAACGATCAAGCCAATC | |||||
| CAT-F | ATTGAGAGTATGGGAATGGTTTT | WP_005767400 2 | 796 | 54 | 30 | TS |
| CAT-R | CGTGTTCTCGACAATTTTGTTA | |||||
| ialB-F | ATGAAAAAAATATTAAATTTAATTTG | ialB | 558 | 58 | 60 | [37] |
| ialB-R | TTTTTGCAAAGAAGTTAAACGCTTAAG | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendoza-Mujica, G.; Flores-León, D.; Ruiz, J. Molecular Characterization of Fluoroquinolone-Resistant Bartonella bacilliformis. Pathogens 2021, 10, 876. https://doi.org/10.3390/pathogens10070876
Mendoza-Mujica G, Flores-León D, Ruiz J. Molecular Characterization of Fluoroquinolone-Resistant Bartonella bacilliformis. Pathogens. 2021; 10(7):876. https://doi.org/10.3390/pathogens10070876
Chicago/Turabian StyleMendoza-Mujica, Giovanna, Diana Flores-León, and Joaquim Ruiz. 2021. "Molecular Characterization of Fluoroquinolone-Resistant Bartonella bacilliformis" Pathogens 10, no. 7: 876. https://doi.org/10.3390/pathogens10070876
APA StyleMendoza-Mujica, G., Flores-León, D., & Ruiz, J. (2021). Molecular Characterization of Fluoroquinolone-Resistant Bartonella bacilliformis. Pathogens, 10(7), 876. https://doi.org/10.3390/pathogens10070876







