Current Knowledge of Hepatitis E Virus (HEV) Epidemiology in Ruminants
Abstract
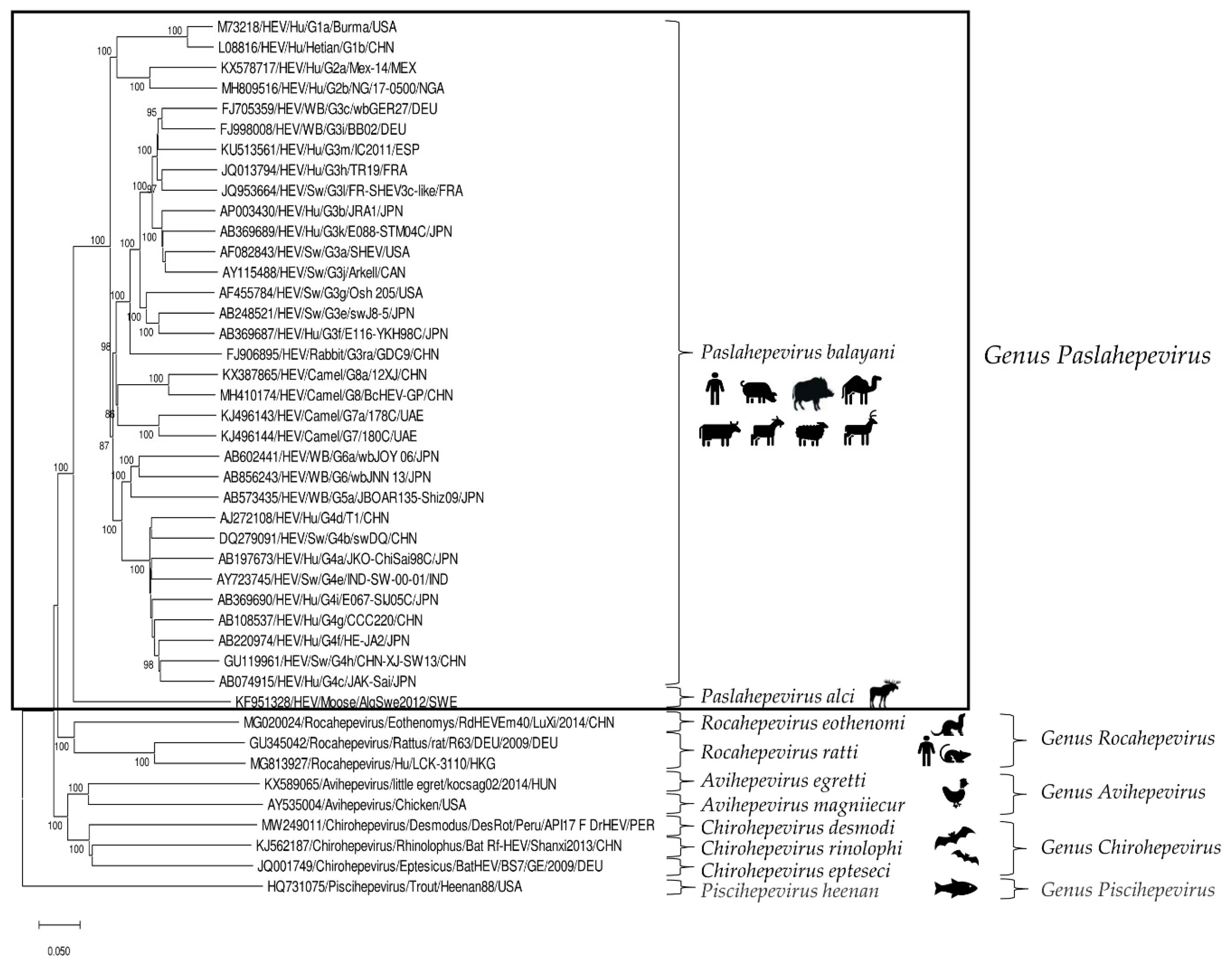
:1. Introduction
2. Domestic Ruminants
2.1. Bovids
2.2. Goats
2.3. Sheep
3. Wild Ruminants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kamar, N.; Izopet, J.; Pavio, N.; Aggarwal, R.; Labrique, A.; Wedemeyer, H.; Dalton, H.R. Hepatitis E virus infection. Nat. Rev. Dis. Prim. 2017, 3, 17086. [Google Scholar] [CrossRef] [PubMed]
- Kamar, N.; Dalton, H.R.; Abravanel, F.; Izopet, J. Hepatitis E virus infection. Clin. Microbiol. Rev. 2014, 27, 116–138. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Yamada, K.; Hoshino, Y.; Takahashi, H.; Ichiyama, K.; Tanaka, T.; Okamoto, H. Monoclonal antibodies raised against the ORF3 protein of hepatitis E virus (HEV) can capture HEV particles in culture supernatant and serum but not those in feces. Arch. Virol. 2008, 153, 1703–1713. [Google Scholar] [CrossRef] [PubMed]
- Nagashima, S.; Takahashi, M.; Kobayashi, T.; Nishizawa, T.; Nishiyama, T.; Primadharsini, P.P.; Okamoto, H. Characterization of the quasi-enveloped hepatitis E virus particles released by the cellular exosomal pathway. J. Virol. 2017, 91, e00822-17. [Google Scholar] [CrossRef]
- Wang, B.; Meng, X.J. Structural and molecular biology of hepatitis E virus. Comput. Struct. Biotechnol. J. 2021, 19, 1907–1916. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://talk.ictvonline.org/taxonomy/ (accessed on 23 August 2022).
- Smith, D.B.; Izopet, J.; Nicot, F.; Simmonds, P.; Jameel, S.; Meng, X.J.; Norder, H.; Okamoto, H.; van der Poel, W.; Reuter, G.; et al. Update: Proposed reference sequences for subtypes of hepatitis E virus (species Orthohepevirus A). J. Gen. Virol. 2020, 101, 692–698. [Google Scholar] [CrossRef]
- Wang, B.; Meng, X.J. Hepatitis E virus: Host tropism and zoonotic infection. Curr. Opin. Microbiol. 2021, 59, 8–15. [Google Scholar] [CrossRef]
- Pavio, N.; Doceul, V.; Bagdassarian, E.; Johne, R. Recent knowledge on hepatitis E virus in Suidae reservoirs and transmission routes to human. Vet. Res. 2017, 48, 78. [Google Scholar] [CrossRef]
- Dalton, H.R.; Izopet, J. Transmission and Epidemiology of Hepatitis E Virus Genotype 3 and 4 Infections. Cold Spring Harb. Perspect. Med. 2018, 8, a032144. [Google Scholar] [CrossRef]
- Takahashi, M.; Nishizawa, T.; Sato, H.; Sato, Y.; Jirintai; Nagashima, S.; Okamoto, H. Analysis of the full-length genome of a hepatitis E virus isolate obtained from a wild boar in Japan that is classifiable into a novel genotype. J. Gen. Virol. 2011, 92, 902–908. [Google Scholar] [CrossRef]
- Woo, P.C.; Lau, S.K.; Teng, J.L.; Tsang, A.K.; Joseph, M.; Wong, E.Y.; Tang, Y.; Sivakumar, S.; Xie, J.; Bai, R.; et al. New hepatitis E virus genotype in camels, the Middle East. Emerg. Infect. Dis. 2014, 20, 1044–1048. [Google Scholar] [CrossRef] [PubMed]
- Woo, P.C.; Lau, S.K.; Teng, J.L.; Cao, K.Y.; Wernery, U.; Schountz, T.; Chiu, T.H.; Tsang, A.K.; Wong, P.C.; Wong, E.Y.; et al. New Hepatitis E Virus Genotype in Bactrian Camels, Xinjiang, China. Emerg. Infect. Dis. 2016, 22, 2219–2221. [Google Scholar] [CrossRef] [PubMed]
- Li, T.C.; Bai, H.; Yoshizaki, S.; Ami, Y.; Suzaki, Y.; Doan, Y.H.; Takahashi, K.; Mishiro, S.; Takeda, N.; Wakita, T. Genotype 5 Hepatitis E Virus Produced by a Reverse Genetics System Has the Potential for Zoonotic Infection. Hepatol. Commun. 2018, 3, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Teng, J.; Lau, S.; Sridhar, S.; Fu, H.; Gong, W.; Li, M.; Xu, Q.; He, Y.; Zhuang, H.; et al. Transmission of a Novel Genotype of Hepatitis E Virus from Bactrian Camels to Cynomolgus Macaques. J. Virol. 2019, 93, e02014-18. [Google Scholar] [CrossRef]
- Sridhar, S.; Yip, C.C.Y.; Wu, S.; Cai, J.; Zhang, A.J.X.; Leung, K.H.; Chung, T.W.H.; Chan, J.F.W.; Chan, W.M.; Teng, J.L.L.; et al. Rat Hepatitis E Virus as Cause of Persistent Hepatitis after Liver Transplant. Emerg. Infect. Dis. 2018, 24, 2241–2250. [Google Scholar] [CrossRef]
- Andonov, A.; Robbins, M.; Borlang, J.; Cao, J.; Hatchette, T.; Stueck, A.; Deschambault, Y.; Murnaghan, K.; Varga, J.; Johnston, L. Rat Hepatitis E Virus Linked to Severe Acute Hepatitis in an Immunocompetent Patient. J. Infect. Dis. 2019, 220, 951–955. [Google Scholar] [CrossRef]
- Sridhar, S.; Yip, C.C.; Wu, S.; Chew, N.F.; Leung, K.H.; Chan, J.F.; Zhao, P.S.; Chan, W.M.; Poon, R.W.; Tsoi, H.W.; et al. Transmission of Rat Hepatitis E Virus Infection to Humans in Hong Kong: A Clinical and Epidemiological Analysis. Hepatology 2021, 73, 10–22. [Google Scholar] [CrossRef]
- Rivero-Juarez, A.; Frias, M.; Perez, A.B.; Pineda, J.A.; Reina, G.; Fuentes-Lopez, A.; Freyre-Carrillo, C.; Ramirez-Arellano, E.; Alados, J.C.; Rivero, A.; et al. Orthohepevirus C infection as an emerging cause of acute hepatitis in Spain: First report in Europe. J. Hepatol. 2022, 77, 326–331. [Google Scholar] [CrossRef]
- Lee, G.H.; Tan, B.H.; Teo, E.C.; Lim, S.G.; Dan, Y.Y.; Wee, A.; Aw, P.P.; Zhu, Y.; Hibberd, M.L.; Tan, C.K.; et al. Chronic Infection with Camelid Hepatitis E Virus in a Liver Transplant Recipient Who Regularly Consumes Camel Meat and Milk. Gastroenterology 2016, 150, 355–357. [Google Scholar] [CrossRef]
- Kumar, S.; Stecher, G.; Li, M.; Knyaz, C.; Tamura, K. MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol. Biol. Evol. 2018, 35, 1547–1549. [Google Scholar] [CrossRef]
- Kenney, S.P. The Current Host Range of Hepatitis E Viruses. Viruses 2019, 11, 452. [Google Scholar] [CrossRef] [PubMed]
- Tei, S.; Kitajima, N.; Takahashi, K.; Mishiro, S. Zoonotic transmission of hepatitis E virus from deer to human beings. Lancet 2003, 362, 371–373. [Google Scholar] [CrossRef]
- Favorov, M.O.; Nazarova, O.; Margohs, H.S. Is hepatitis E an emerging zoonotic 11 disease? Am. J. Trop. Med. Hyg. 1998, 59, 242. [Google Scholar]
- Arankalle, V.A.; Joshi, M.V.; Kulkarni, A.M.; Gandhe, S.S.; Chobe, L.P.; Rautmare, S.S.; Mishra, A.C.; Padbidri, V.S. Prevalence of anti-hepatitis E virus antibodies in different Indian animal species. J. Viral Hepat. 2001, 8, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Zhang, H.; Xia, N.; Peng, G.; Lan, H.Y.; Zhuang, H.; Zhu, Y.H.; Li, S.W.; Tian, K.G.; Gu, W.J.; et al. Prevalence, isolation, and partial sequence analysis of hepatitis E virus from domestic animals in China. J. Med. Virol. 2002, 67, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Shen, Q.; Mou, J.; Gong, G.; Yang, Z.; Cui, L.; Zhu, J.; Ju, G.; Hua, X. Hepatitis E virus infection among domestic animals in eastern China. Zoonoses Public Health 2008, 55, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Sun, J.; Liu, M.; Xia, L.; Zhao, C.; Harrison, T.J.; Wang, Y. Seroepidemiology and genetic characterization of hepatitis E virus in the northeast of China. Infect. Genet. Evol. 2009, 9, 554–561. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Wang, L.; Geng, J.; Zhu, Y.; Fu, H.; Ren, F.; Li, L.; Wang, X.; Zhuang, H. Zoonotic risk of hepatitis E virus (HEV): A study of HEV infection in animals and humans in suburbs of Beijing. Hepatol. Res. 2009, 39, 1153–1158. [Google Scholar] [CrossRef]
- Fu, H.; Li, L.; Zhu, Y.; Wang, L.; Geng, J.; Chang, Y.; Xue, C.; Du, G.; Li, Y.; Zhuang, H. Hepatitis E virus infection among animals and humans in Xinjiang, China: Possibility of swine to human transmission of sporadic hepatitis E in an endemic area. Am. J. Trop. Med. Hyg. 2010, 82, 961–966. [Google Scholar] [CrossRef]
- Geng, Y.; Wang, C.; Zhao, C.; Yu, X.; Harrison, T.J.; Tian, K.; Wang, Y. Serological prevalence of hepatitis E virus in domestic animals and diversity of genotype 4 hepatitis E virus in China. Vector-Borne Zoonotic Dis. 2010, 10, 765–770. [Google Scholar] [CrossRef]
- Geng, J.; Wang, L.; Wang, X.; Fu, H.; Bu, Q.; Liu, P.; Zhu, Y.; Wang, M.; Sui, Y.; Zhuang, H. Potential risk of zoonotic transmission from young swine to human: Seroepidemiological and genetic characterization of hepatitis E virus in human and various animals in Beijing, China. J. Viral Hepat. 2011, 18, e583–e590. [Google Scholar] [CrossRef] [PubMed]
- Yan, B.; Zhang, L.; Gong, L.; Lv, J.; Feng, Y.; Liu, J.; Song, L.; Xu, Q.; Jiang, M.; Xu, A. Hepatitis E Virus in Yellow Cattle, Shandong, Eastern China. Emerg. Infect. Dis. 2016, 22, 2211–2212. [Google Scholar] [CrossRef] [PubMed]
- Tritz, S.E.; Khounvisith, V.; Pommasichan, S.; Ninnasopha, K.; Keosengthong, A.; Phoutana, V.; Camoin, M.; Hübschen, J.M.; Black, A.P.; Muller, C.P.; et al. Evidence of increased Hepatitis E virus exposure in Lao villagers with contact to ruminants. Zoonoses Public Health 2018, 65, 690–701. [Google Scholar] [CrossRef] [PubMed]
- Obaidat, M.M.; Roess, A.A. Individual animal and herd level seroprevalence and risk factors of Hepatitis E in ruminants in Jordan. Infect. Genet. Evol. 2020, 81, 104276. [Google Scholar] [CrossRef]
- Goens, S.D.; Botero, S.; Hare, W.; Meng, X.J.; Perdue, M. Serological evidence for a hepatitis E virus of cattle. In Proceedings of the 22nd Annual Meeting of the American Society for Virology, Davis, CA, USA, 12–16 July 2003; p. 179. [Google Scholar]
- Vitral, C.L.; Pinto, M.A.; Lewis-Ximenez, L.L.; Khudyakov, Y.E.; dos Santos, D.R.; Gaspar, A.M. Serological evidence of hepatitis E virus infection in different animal species from the Southeast of Brazil. Mem. Do Inst. Oswaldo Cruz 2005, 100, 117–122. [Google Scholar] [CrossRef]
- Dong, C.; Meng, J.; Dai, X.; Liang, J.H.; Feagins, A.R.; Meng, X.J.; Belfiore, N.M.; Bradford, C.; Corn, J.L.; Cray, C.; et al. Restricted enzooticity of hepatitis E virus genotypes 1 to 4 in the United States. J. Clin. Microbiol. 2011, 49, 4164–4172. [Google Scholar] [CrossRef]
- Yugo, D.M.; Cossaboom, C.M.; Heffron, C.L.; Huang, Y.W.; Kenney, S.P.; Woolums, A.R.; Hurley, D.J.; Opriessnig, T.; Li, L.; Delwart, E.; et al. Evidence for an unknown agent antigenically related to the hepatitis E virus in dairy cows in the United States. J. Med. Virol. 2019, 91, 677–686. [Google Scholar] [CrossRef]
- El-Tras, W.F.; Tayel, A.A.; El-Kady, N.N. Seroprevalence of hepatitis E virus in humans and geographically matched food animals in Egypt. Zoonoses Public Health. 2013, 60, 244–251. [Google Scholar] [CrossRef]
- Junaid, S.A.; Agina, S.E. Haematological Changes Associated with Hepatitis E Virus Seropositivity among Human and Animal Subjects in Plateau State, Nigeria. Int. Blood Res. Rev. 2014, 2, 311–321. [Google Scholar] [CrossRef]
- Antia, R.E.; Adekola, A.A.; Jubril, A.J.; Ohore, O.G.; Emikpe, B.O. Hepatitis E Virus infection seroprevalence and the associated risk factors in animals raised in Ibadan, Nigeria. J. Immunoassay Immunochem. 2018, 39, 509–520. [Google Scholar] [CrossRef]
- Ouoba, J.B.; Traore, K.A.; Rouamba, H.; Setondji, K.V.; Minoungou, G.L.; Ouoba, B.L.; Ouedraogo, A.; Moctar, S.; M’Bengue, A.K.; Kakou, S.N.; et al. Prevalence of anti-hepatitis E virus antibodies in domestic animal from three representative provinces of Burkina Faso. Vet. Anim. Sci. 2019, 7, 100059. [Google Scholar] [CrossRef] [PubMed]
- Sayed, I.M.; Elkhawaga, A.A.; El-Mokhtar, M.A. Circulation of hepatitis E virus (HEV) and/or HEV-like agent in non-mixed dairy farms could represent a potential source of infection for Egyptian people. Int. J. Food Microbiol. 2020, 317, 108479. [Google Scholar] [CrossRef] [PubMed]
- Tialla, D.; Cissé, A.; Ouédraogo, G.A.; Hübschen, J.M.; Tarnagda, Z.; Snoeck, C.J. Prevalence of hepatitis E virus antibodies in cattle in Burkina Faso associated with swine mixed farming. J. Vet. Sci. 2022; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Shukla, P.; Chauhan, U.K.; Naik, S.; Anderson, D.; Aggarwal, R. Hepatitis E virus infection among animals in northern India: An unlikely source of human disease. J. Viral Hepat. 2007, 14, 310–317. [Google Scholar] [CrossRef]
- Peralta, B.; Casas, M.; de Deus, N.; Martín, M.; Ortuño, A.; Pérez-Martín, E.; Pina, S.; Mateu, E. Anti-HEV antibodies in domestic animal species and rodents from Spain using a genotype 3-based ELISA. Vet. Microbiol. 2009, 137, 66–73. [Google Scholar] [CrossRef]
- Reuter, G.; Fodor, D.; Forgách, P.; Kátai, A.; Szucs, G. Characterization and zoonotic potential of endemic hepatitis E virus (HEV) strains in humans and animals in Hungary. J. Clin. Virol. 2009, 44, 277–281. [Google Scholar] [CrossRef]
- Forgách, P.; Nowotny, N.; Erdélyi, K.; Boncz, A.; Zentai, J.; Szucs, G.; Reuter, G.; Bakonyi, T. Detection of hepatitis E virus in samples of animal origin collected in Hungary. Vet. Microbiol. 2010, 143, 106–116. [Google Scholar] [CrossRef]
- Hu, G.D.; Ma, X. Detection and sequences analysis of bovine hepatitis E virus RNA in Xinjiang Autonomous Region. Bing Du Xue Bao = Chin. J. Virol. 2010, 26, 27–32. [Google Scholar]
- Prpić, J.; Černi, S.; Škorić, D.; Keros, T.; Brnić, D.; Cvetnić, Ž.; Jemeršić, L. Distribution and Molecular Characterization of Hepatitis E virus in Domestic Animals and Wildlife in Croatia. Food Environ. Virol. 2015, 7, 195–205. [Google Scholar] [CrossRef]
- Huang, F.; Li, Y.; Yu, W.; Jing, S.; Wang, J.; Long, F.; He, Z.; Yang, C.; Bi, Y.; Cao, W.; et al. Excretion of infectious hepatitis E virus into milk in cows imposes high risks of zoonosis. Hepatology 2016, 64, 350–359. [Google Scholar] [CrossRef]
- Baechlein, C.; Becher, P. No evidence for zoonotic hepatitis E virus infection through dairy milk in Germany. Hepatology 2017, 65, 394–395. [Google Scholar] [CrossRef] [PubMed]
- Vercouter, A.S.; Sayed, I.M.; Lipkens, Z.; De Bleecker, K.; De Vliegher, S.; Colman, R.; Koppelman, M.; Supré, K.; Meuleman, P. Absence of zoonotic hepatitis E virus infection in Flemish dairy cows. Int. J. Food Microbiol. 2018, 281, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Geng, Y.; Zhao, C.; Huang, W.; Wang, X.; Xu, Y.; Wu, D.; Du, Y.; Liu, H.; Wang, Y. Hepatitis E virus was not detected in feces and milk of cows in Hebei province of China: No evidence for HEV prevalence in cows. Int. J. Food Microbiol. 2019, 291, 5–9. [Google Scholar] [CrossRef]
- Go, H.J.; Park, B.J.; Ahn, H.S.; Lyoo, E.L.; Kim, D.H.; Lee, J.B.; Park, S.Y.; Song, C.S.; Lee, S.W.; Choi, I.S. Identification of Hepatitis E Virus in Bovine and Porcine Raw Livers. J. Microbiol. Biotechnol. 2019, 29, 2022–2025. [Google Scholar] [CrossRef] [PubMed]
- Demirci, M.; Yiğin, A.; Ünlü, Ö.; Kılıç Altun, S. Detection of HEV RNA amounts and genotypes in raw milks obtained from different animals. Mikrobiyol. Bul. 2019, 53, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Pan, Y.; Baloch, A.R.; Tian, L.; Wang, M.; Na, W.; Ding, L.; Zeng, Q. Hepatitis E virus genotype 4 in yak, northwestern China. Emerg. Infect. Dis. 2014, 20, 2182–2184. [Google Scholar] [CrossRef] [PubMed]
- Sanford, B.J.; Emerson, S.U.; Purcell, R.H.; Engle, R.E.; Dryman, B.A.; Cecere, T.E.; Buechner-Maxwell, V.; Sponenberg, D.P.; Meng, X.J. Serological evidence for a hepatitis e virus-related agent in goats in the United States. Transbound. Emerg. Dis. 2013, 60, 538–545. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, B.; Di Profio, F.; Melegari, I.; Sarchese, V.; Robetto, S.; Marsilio, F.; Martella, V. Detection of hepatitis E virus (HEV) in goats. Virus Res. 2016, 225, 69–72. [Google Scholar] [CrossRef]
- Long, F.; Yu, W.; Yang, C.; Wang, J.; Li, Y.; Li, Y.; Huang, F. High prevalence of hepatitis E virus infection in goats. J. Med. Virol. 2017, 89, 1981–1987. [Google Scholar] [CrossRef]
- Li, S.; Liu, M.; Cong, J.; Zhou, Y.; Miao, Z. Detection and Characterization of Hepatitis E Virus in Goats at Slaughterhouse in Tai’an Region, China. BioMed Res. Int. 2017, 2017, 3723650. [Google Scholar] [CrossRef]
- El-Mokhtar, M.A.; Elkhawaga, A.A.; Sayed, I.M. Assessment of hepatitis E virus (HEV) in the edible goat products pointed out a risk for human infection in Upper Egypt. Int. J. Food Microbiol. 2020, 330, 108784. [Google Scholar] [CrossRef] [PubMed]
- Palombieri, A.; Robetto, S.; Di Profio, F.; Sarchese, V.; Fruci, P.; Bona, M.C.; Ru, G.; Orusa, R.; Marsilio, F.; Martella, V.; et al. Surveillance Study of Hepatitis E Virus (HEV) in Domestic and Wild Ruminants in Northwestern Italy. Animals 2020, 10, 2351. [Google Scholar] [CrossRef] [PubMed]
- Dziedzinska, R.; Krzyzankova, M.; Bena, M.; Vasickova, P. Evidence of Hepatitis E Virus in Goat and Sheep Milk. Viruses 2020, 12, 1429. [Google Scholar] [CrossRef]
- Caballero-Gómez, J.; García-Bocanegra, I.; Jiménez-Martín, D.; Cano-Terriza, D.; Risalde, M.A.; López-López, P.; Jiménez-Ruiz, S.; Rivero, A.; Rivero-Juarez, A. Epidemiological survey and risk factors associated with hepatitis E virus in small ruminants in southern Spain. Zoonoses Public Health 2022, 69, 387–393. [Google Scholar] [CrossRef]
- Deng, Y. Serological epidemiology of goat hepatitis E in Panxi area of Sichuan province. Zhongguo Yufang Shouyi Xuebao = Chin. J. Prev. Vet. Med. 2014, 36, 805–828. [Google Scholar]
- Usmanov, R.K.; Balaian, M.S.; Dvoĭnikova, O.V.; Alymbaeva, D.B.; Zamiatina, N.A.; Kazachkov, I.; Belov, V.I. An experimental infection in lambs by the hepatitis E virus. Vopr. Virusol. 1994, 39, 165–168. [Google Scholar]
- Wu, J.Y.; Kang, Q.; Bai, W.S.; Bai, Z.H. Seroepidemiological survey of sheep hepatitis E virus infection in Aksu region of Xinjiang Autonomous. Bing Du Xue Bao = Chin. J. Virol. 2010, 26, 234–237. [Google Scholar]
- Wu, J.; Si, F.; Jiang, C.; Li, T.; Jin, M. Molecular detection of hepatitis E virus in sheep from southern Xinjiang, China. Virus Genes 2015, 50, 410–417. [Google Scholar] [CrossRef]
- Shuaibu, A.B.; Alkali, B.R.; Abubakar, M.B.; Daneji, A.I.; Shuaibu, S.A.; Bello, A.I.; Abubaka, F.; Bello, M. Prevalence of Hepatitis E Virus (HEV) Antibodies in Sheep from Sokoto State. J. Adv. Microbiol. 2016, 1, 1–6. [Google Scholar] [CrossRef]
- Sarchese, V.; Di Profio, F.; Melegari, I.; Palombieri, A.; Sanchez, S.B.; Arbuatti, A.; Ciuffetelli, M.; Marsilio, F.; Martella, V.; Di Martino, B. Hepatitis E virus in sheep in Italy. Transbound. Emerg. Dis. 2019, 66, 1120–1125. [Google Scholar] [CrossRef]
- Mesquita, J.R.; Santos-Ferreira, N.; Ferreira, A.S.; Albuquerque, C.; Nóbrega, C.; Esteves, F.; Cruz, R.; Vala, H.; Nascimento, M. Increased risk of hepatitis E virus infection in workers occupationally exposed to sheep. Transbound. Emerg. Dis. 2020; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Ma, X. Detection and sequences analysis of sheep hepatitis E virus RNA in Xinjiang autonomous region. Wei Sheng Wu Xue Bao = Acta Microbiol. Sin. 2010, 50, 937–941. (In Chinese) [Google Scholar]
- Sonoda, H.; Abe, M.; Sugimoto, T.; Sato, Y.; Bando, M.; Fukui, E.; Mizuo, H.; Takahashi, M.; Nishizawa, T.; Okamoto, H. Prevalence of hepatitis E virus (HEV) Infection in wild boars and deer and genetic identification of a genotype 3 HEV from a boar in Japan. J. Clin. Microbiol. 2004, 42, 5371–5374. [Google Scholar] [CrossRef]
- Matsuura, Y.; Suzuki, M.; Yoshimatsu, K.; Arikawa, J.; Takashima, I.; Yokoyama, M.; Igota, H.; Yamauchi, K.; Ishida, S.; Fukui, D.; et al. Prevalence of antibody to hepatitis E virus among wild sika deer, Cervus nippon, in Japan. Arch. Virol. 2007, 152, 1375–1381. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.X.; Qin, S.Y.; Zhang, Y.; Meng, Q.F.; Jiang, J.; Yang, G.L.; Zhao, Q.; Zhu, X.Q. First report of hepatitis E virus infection in sika deer in China. BioMed Res. Int. 2015, 2015, 502846. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, M.; Nishizono, A.; Kawakami, M.; Fukui, E.; Isogai, E.; Matsuoka, H.; Yamamoto, S.; Mizuo, H.; Nagashima, S.; Murata, K.; et al. Identification of hepatitis E virus in wild sika deer in Japan. Virus Res. 2022, 308, 198645. [Google Scholar] [CrossRef]
- Mendoza, M.V.; Yonemitsu, K.; Ishijima, K.; Kuroda, Y.; Tatemoto, K.; Inoue, Y.; Shimoda, H.; Kuwata, R.; Takano, A.; Suzuki, K.; et al. Nationwide survey of hepatitis E virus infection among wildlife in Japan. J. Vet. Med. Sci. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Tomiyama, D.; Inoue, E.; Osawa, Y.; Okazaki, K. Serological evidence of infection with hepatitis E virus among wild Yezo-deer, Cervus nippon yesoensis, in Hokkaido, Japan. J. Viral Hepat. 2009, 16, 524–528. [Google Scholar] [CrossRef]
- Slukinova, O.S.; Kyuregyan, K.K.; Karlsen, A.A.; Potemkin, I.A.; Kichatova, V.S.; Semenov, S.I.; Stepanov, K.M.; Rumyantseva, T.D.; Mikhailov, M.I. Serological Evidence of Hepatitis E Virus Circulation Among Reindeer and Reindeer Herders. Vector-Borne Zoonotic Dis. 2020, 21, 546–551. [Google Scholar] [CrossRef]
- Yu, C.; Zimmerman, C.; Stone, R.; Engle, R.E.; Elkins, W.; Nardone, G.A.; Emerson, S.U.; Purcell, R.H. Using improved technology for filter paper-based blood collection to survey wild Sika deer for antibodies to hepatitis E virus. J. Virol. Methods. 2007, 142, 143–150. [Google Scholar] [CrossRef]
- Medrano, C.; Boadella, M.; Barrios, H.; Cantú, A.; García, Z.; de la Fuente, J.; Gortazar, C. Zoonotic pathogens among white-tailed deer, northern Mexico, 2004–2009. Emerg. Infect. Dis. 2012, 18, 1372–1374. [Google Scholar] [CrossRef] [PubMed]
- Weger, S.; Elkin, B.; Lindsay, R.; Bollinger, T.; Crichton, V.; Andonov, A. Hepatitis E Virus Seroprevalence in Free-Ranging Deer in Canada. Transbound. Emerg. Dis. 2016, 64, 1008–1011. [Google Scholar] [CrossRef] [PubMed]
- Boadella, M.; Casas, M.; Martín, M.; Vicente, J.; Segalés, J.; de la Fuente, J.; Gortázar, C. Increasing contact with hepatitis E virus in red deer, Spain. Emerg. Infect. Dis. 2010, 16, 1994–1996. [Google Scholar] [CrossRef]
- Rutjes, S.A.; Lodder-Verschoor, F.; Lodder, W.J.; van der Giessen, J.; Reesink, H.; Bouwknegt, M.; de Roda Husman, A.M. Seroprevalence and molecular detection of hepatitis E virus in wild boar and red deer in The Netherlands. J. Virol. Methods 2010, 168, 197–206. [Google Scholar] [CrossRef] [PubMed]
- Larska, M.; Krzysiak, M.K.; Jabłoński, A.; Kęsik, J.; Bednarski, M.; Rola, J. Hepatitis E virus antibody prevalence in wildlife in Poland. Zoonoses Public Health 2015, 62, 105–110. [Google Scholar] [CrossRef]
- Kukielka, D.; Rodriguez-Prieto, V.; Vicente, J.; Sánchez-Vizcaíno, J.M. Constant Hepatitis E Virus (HEV) Circulation in Wild Boar and Red Deer in Spain: An Increasing Concern Source of HEV Zoonotic Transmission. Transbound. Emerg. Dis. 2016, 63, e360–e368. [Google Scholar] [CrossRef]
- Lin, J.; Karlsson, M.; Olofson, A.S.; Belák, S.; Malmsten, J.; Dalin, A.M.; Widén, F.; Norder, H. High prevalence of hepatitis e virus in Swedish moose—A phylogenetic characterization and comparison of the virus from different regions. PLoS ONE 2015, 10, e0122102. [Google Scholar] [CrossRef]
- Mazzei, M.; Forzan, M.; Pizzurro, F.; Picciolli, F.; Bandecchi, P.; Poli, A. Detection of Hepatitis E Virus Antibodies in Domestic and Wild Animal Species in Central Italy. Clin. Microbiol. 2015, 4, 227. [Google Scholar] [CrossRef]
- Neumann, S.; Hackl, S.S.; Piepenschneider, M.; Vina-Rodriguez, A.; Dremsek, P.; Ulrich, R.G.; Groschup, M.H.; Eiden, M. Serologic and Molecular Survey of Hepatitis E Virus in German Deer Populations. J. Wildl. Dis. 2016, 52, 106–113. [Google Scholar] [CrossRef]
- Roth, A.; Lin, J.; Magnius, L.; Karlsson, M.; Belák, S.; Widén, F.; Norder, H. Markers for Ongoing or Previous Hepatitis E Virus Infection Are as Common in Wild Ungulates as in Humans in Sweden. Viruses 2016, 8, 259. [Google Scholar] [CrossRef]
- Anheyer-Behmenburg, H.E.; Szabo, K.; Schotte, U.; Binder, A.; Klein, G.; Johne, R. Hepatitis E Virus in Wild Boars and Spillover Infection in Red and Roe Deer, Germany, 2013–2015. Emerg. Infect. Dis. 2017, 23, 130–133. [Google Scholar] [CrossRef]
- Thiry, D.; Mauroy, A.; Saegerman, C.; Licoppe, A.; Fett, T.; Thomas, I.; Brochier, B.; Thiry, E.; Linden, A. Belgian Wildlife as Potential Zoonotic Reservoir of Hepatitis E Virus. Transbound. Emerg. Dis. 2015, 64, 764–773. [Google Scholar] [CrossRef] [PubMed]
- Di Bartolo, I.; Ponterio, E.; Angeloni, G.; Morandi, F.; Ostanello, F.; Nicoloso, S.; Ruggeri, F.M. Presence of Hepatitis E Virus in a RED Deer (Cervus Elaphus) Population in Central Italy. Transbound. Emerg. Dis. 2015, 64, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Trojnar, E.; Kästner, B.; Johne, R. No Evidence of Hepatitis E Virus Infection in Farmed Deer in Germany. Food Environ. Virol. 2019, 12, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Loikkanen, E.; Oristo, S.; Hämäläinen, N.; Jokelainen, P.; Kantala, T.; Sukura, A.; Maunula, L. Antibodies Against Hepatitis E Virus (HEV) in European Moose and White-Tailed Deer in Finland. Food Environ. Virol. 2020, 12, 333–341. [Google Scholar] [CrossRef]
- Trogu, T.; Ferrari, N.; Formenti, N.; Filipello, V.; Pedrotti, L.; Viganò, R.; Lanfranchi, P.; Luzzago, C. Low Serologic Prevalences Suggest Sporadic Infections of Hepatitis E Virus in Chamois (Rupicapra rupicapra) and Red Deer (Cervus elaphus) in the Italian Alps. J. Wildl. Dis. 2020, 56, 443–446. [Google Scholar] [CrossRef]
- Rinaldo, C.H.; Nymo, I.H.; Sánchez Romano, J.; Breines, E.M.; Murguzur, F.; Tryland, M. Serological Evidence of Hepatitis E Virus Infection in Semi-Domesticated Eurasian Tundra Reindeer (Rangifer tarandus tarandus) in Norway. Pathogens 2021, 10, 1542. [Google Scholar] [CrossRef]
- Sacristán, C.; Madslien, K.; Sacristán, I.; Klevar, S.; das Neves, C.G. Seroprevalence of Hepatitis E Virus in Moose (Alces alces), Reindeer (Rangifer tarandus), Red Deer (Cervus elaphus), Roe Deer (Capreolus capreolus), and Muskoxen (Ovibos moschatus) from Norway. Viruses 2021, 13, 224. [Google Scholar] [CrossRef]
- Crotta, M.; Pellicioli, L.; Gaffuri, A.; Trogu, T.; Formenti, N.; Tranquillo, V.; Luzzago, C.; Ferrari, N.; Lanfranchi, P. Analysis of seroprevalence data on Hepatitis E virus and Toxoplasma gondii in wild ungulates for the assessment of human exposure to zoonotic meat-borne pathogens. Food Microbiol. 2021, 101, 103890. [Google Scholar] [CrossRef]
- Zhang, W.; Shen, Q.; Mou, J.; Yang, Z.B.; Yuan, C.L.; Cui, L.; Zhu, J.G.; Hua, X.G.; Xu, C.M.; Hu, J. Cross-species infection of hepatitis E virus in a zoo-like location, including birds. Epidemiol. Infect. 2007, 136, 1020–1026. [Google Scholar] [CrossRef]
- Lin, J.; Norder, H.; Uhlhorn, H.; Belák, S.; Widén, F. Novel hepatitis E like virus found in Swedish moose. J. Gen. Virol. 2014, 95 (Pt 3), 557–570. [Google Scholar] [CrossRef] [PubMed]
- Kubankova, M.; Kralik, P.; Lamka, J.; Zakovcik, V.; Dolanský, M.; Vasickova, P. Prevalence of Hepatitis E Virus in Populations of Wild Animals in Comparison with Animals Bred in Game Enclosures. Food Environ. Virol. 2015, 7, 159–163. [Google Scholar] [CrossRef]
- Lhomme, S.; Top, S.; Bertagnoli, S.; Dubois, M.; Guerin, J.L.; Izopet, J. Wildlife Reservoir for Hepatitis E Virus, Southwestern France. Emerg. Infect. Dis. 2015, 21, 1224–1226. [Google Scholar] [CrossRef] [PubMed]
- Serracca, L.; Battistini, R.; Rossini, I.; Mignone, W.; Peletto, S.; Boin, C.; Pistone, G.; Ercolini, R.; Ercolini, C. Molecular Investigation on the Presence of Hepatitis E Virus (HEV) in Wild Game in North-Western Italy. Food Environ. Virol. 2015, 7, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Spancerniene, U.; Grigas, J.; Buitkuviene, J.; Zymantiene, J.; Juozaitiene, V.; Stankeviciute, M.; Razukevicius, D.; Zienius, D.; Stankevicius, A. Prevalence and phylogenetic analysis of hepatitis E virus in pigs, wild boars, roe deer, red deer and moose in Lithuania. Acta Vet. Scand. 2018, 60, 13. [Google Scholar] [CrossRef] [PubMed]
- Arnaboldi, S.; Righi, F.; Carta, V.; Bonardi, S.; Pavoni, E.; Bianchi, A.; Losio, M.N.; Filipello, V. Hepatitis E Virus (HEV) Spread and Genetic Diversity in Game Animals in Northern Italy. Food Environ. Virol. 2021, 13, 146–153. [Google Scholar] [CrossRef]
- Moraes, D.; Lopez-Lopez, P.; Palmeira, J.D.; Torres, R.T.; Rivero-Juarez, A.; Dutra, V.; Nascimento, M.; Mesquita, J.R. Screening for hepatitis E virus genotype 3 in red deer (Cervus elaphus) and fallow deer (Dama dama), Portugal, 2018–2020. Transbound. Emerg. Dis. 2021; online ahead of print. [Google Scholar] [CrossRef]
- Fonti, N.; Pacini, M.I.; Forzan, M.; Parisi, F.; Periccioli, M.; Mazzei, M.; Poli, A. Molecular and Pathological Detection of Hepatitis E Virus in Roe Deer (Capreolus capreolus) and Fallow Deer (Dama dama) in Central Italy. Vet. Sci. 2022, 9, 100. [Google Scholar] [CrossRef]
- Amiri Dehnoyi, M.; Mokhtari, A. Genomic Investigation of Hepatitis E Virus in Persian Gazelle. Jentashapir J. Cell. Mol. Biol. 2020, 11, e111737. [Google Scholar] [CrossRef]
- Boadella, M. Hepatitis E in wild ungulates: A review. Small Rumin. Res. 2015, 128, 64–71. [Google Scholar] [CrossRef]
- Takahashi, K.; Kitajima, N.; Abe, N.; Mishiro, S. Complete or near-complete nucleotide sequences of hepatitis E virus genome recovered from a wild boar, a deer, and four patients who ate the deer. Virology 2004, 330, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Martelli, F.; Caprioli, A.; Zengarini, M.; Marata, A.; Fiegna, C.; Di Bartolo, I.; Ruggeri, F.M.; Delogu, M.; Ostanello, F. Detection of hepatitis E virus (HEV) in a demographic managed wild boar (Sus scrofa scrofa) population in Italy. Vet. Microbiol. 2008, 126, 74–81. [Google Scholar] [CrossRef]
- Meester, M.; Tobias, T.J.; Bouwknegt, M.; Kusters, N.E.; Stegeman, J.A.; van der Poel, W. Infection dynamics and per-sistence of hepatitis E virus on pig farms—A review. Porc. Health Manag. 2021, 7, 16. [Google Scholar] [CrossRef]
- Matsuda, H.; Okada, K.; Takahashi, K.; Mishiro, S. Severe hepatitis E virus infection after ingestion of uncooked liver from a wild boar. J. Infect. Dis. 2003, 188, 944. [Google Scholar] [CrossRef] [PubMed]
- Colson, P.; Borentain, P.; Queyriaux, B.; Kaba, M.; Moal, V.; Gallian, P.; Heyries, L.; Raoult, D.; Gerolami, R. Pig liver sausage as a source of hepatitis E virus transmission to humans. J. Infect. Dis. 2010, 202, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Lee, J.M.; Jo, Y.W.; Min, H.J.; Kim, H.J.; Jung, W.T.; Lee, O.J.; Yun, H.; Yoon, Y.S. Genotype-4 hepatitis E in a human after ingesting roe deer meat in South Korea. Clin. Mol. Hepatol. 2003, 19, 309–314. [Google Scholar] [CrossRef]
- Renou, C.; Roque-Afonso, A.M.; Pavio, N. Foodborne transmission of hepatitis E virus from raw pork liver sausage, France. Emerg. Infect. Dis. 2014, 20, 1945–1947. [Google Scholar] [CrossRef]
- Riveiro-Barciela, M.; Mínguez, B.; Gironés, R.; Rodriguez-Frías, F.; Quer, J.; Buti, M. Phylogenetic demonstration of hepatitis E infection transmitted by pork meat ingestion. J. Clin. Gastroenterol. 2015, 49, 165–168. [Google Scholar] [CrossRef]
- El-Kafrawy, S.A.; Hassan, A.M.; El-Daly, M.M.; Al-Hajri, M.; Farag, E.; Elnour, F.A.; Khan, A.; Tolah, A.M.; Alandijany, T.A.; Othman, N.A.; et al. Genetic diversity of hepatitis E virus (HEV) in imported and domestic camels in Saudi Arabia. Sci. Rep. 2022, 12, 7005. [Google Scholar] [CrossRef]
- Sayed, I.M.; El-Mokhtar, M.A. Are ruminants and their products potential sources of human hepatitis E virus infection? Future Virol. 2021, 16, 785–789. [Google Scholar] [CrossRef]
- Dremsek, P.; Wenzel, J.J.; Johne, R.; Ziller, M.; Hofmann, J.; Groschup, M.H.; Werdermann, S.; Mohn, U.; Dorn, S.; Motz, M.; et al. Seroprevalence study in forestry workers from eastern Germany using novel genotype 3- and rat hepatitis E virus-specific immunoglobulin G ELISAs. Med. Microbiol. Immunol. 2012, 201, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Carpentier, A.; Chaussade, H.; Rigaud, E.; Rodriguez, J.; Berthault, C.; Boué, F.; Tognon, M.; Touzé, A.; Garcia-Bonnet, N.; Choutet, P.; et al. High hepatitis E virus seroprevalence in forestry workers and in wild boars in France. J. Clin. Microbiol. 2012, 50, 2888–2893. [Google Scholar] [CrossRef] [PubMed]
- Chaussade, H.; Rigaud, E.; Allix, A.; Carpentier, A.; Touzé, A.; Delzescaux, D.; Choutet, P.; Garcia-Bonnet, N.; Coursaget, P. Hepatitis E virus seroprevalence and risk factors for individuals in working contact with animals. J. Clin. Virol. 2013, 58, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Ivanova, A.; Tefanova, V.; Reshetnjak, I.; Kuznetsova, T.; Geller, J.; Lundkvist, Å.; Janson, M.; Neare, K.; Velström, K.; Jokelainen, P.; et al. Hepatitis E Virus in Domestic Pigs, Wild Boars, Pig Farm Workers, and Hunters in Estonia. Food Environ. Virol. 2015, 7, 403–412. [Google Scholar] [CrossRef]
- Hartl, J.; Otto, B.; Madden, R.G.; Webb, G.; Woolson, K.L.; Kriston, L.; Vettorazzi, E.; Lohse, A.W.; Dalton, H.R.; Pischke, S. Hepatitis E Seroprevalence in Europe: A Meta-Analysis. Viruses 2016, 8, 211. [Google Scholar] [CrossRef]
- Kang, Y.H.; Cong, W.; Zhang, X.Y.; Wang, C.F.; Shan, X.F.; Qian, A.D. Hepatitis E virus seroprevalence among farmers, veterinarians and control subjects in Jilin province, Shandong province and Inner Mongolia Autonomous Region, China. J. Med. Virol. 2017, 89, 872–877. [Google Scholar] [CrossRef]
- Monini, M.; Ostanello, F.; Dominicis, A.; Tagliapietra, V.; Vaccari, G.; Rizzoli, A.; Trombetta, C.M.; Montomoli, E.; Di Bartolo, I. Seroprevalence of Hepatitis E Virus in Forestry Workers from Trentino-Alto Adige Region (Northern Italy). Pathogens 2020, 9, 568. [Google Scholar] [CrossRef]
- Krumbholz, A.; Mohn, U.; Lange, J.; Motz, M.; Wenzel, J.J.; Jilg, W.; Walther, M.; Straube, E.; Wutzler, P.; Zell, R. Prevalence of hepatitis E virus-specific antibodies in humans with occupational exposure to pigs. Med. Microbiol. Immunol. 2012, 201, 239–244. [Google Scholar] [CrossRef]
- Teixeira, J.; Mesquita, J.R.; Pereira, S.S.; Oliveira, R.M.; Abreu-Silva, J.; Rodrigues, A.; Myrmel, M.; Stene-Johansen, K.; Øverbø, J.; Gonçalves, G.; et al. Prevalence of hepatitis E virus antibodies in workers occupationally exposed to swine in Portugal. Med. Microbiol. Immunol. 2017, 206, 77–81. [Google Scholar] [CrossRef]
- Mrzljak, A.; Balen, I.; Barbic, L.; Ilic, M.; Vilibic-Cavlek, T. Hepatitis E virus in professionally exposed: A reason for concern? World J. Hepatol. 2021, 13, 723–730. [Google Scholar] [CrossRef]


| Animal Species | Country | Year | Type of Sample | Seroprevalence % (Positive/Total) | Molecular Prevalence % (Positive/Total) | Genotype (gt) | Reference |
|---|---|---|---|---|---|---|---|
| Bos taurus | Ukraine | 1998 | Serum | 12.0% | 1 n.d. | [24] | |
| India | 1994 1999 | Serum | 4.0% (4/91) 6.9% (13/188) | n.d. | [25] | ||
| China | 2002 | Serum | 6.3% (12/190) | n.d. | [26] | ||
| Brazil | 2005 | Serum | 1.4% (1/70) | n.d. | [37] | ||
| China | 2004 | Serum | 6.0% (6/100) | 0% (0/100) | [27] | ||
| China | 2009 | Serum | 18.7% (301/1612) | 3.3% (3/120) | [28] | ||
| China | 2009 | Serum | 29.4% (54/184) | n.d. | [29] | ||
| Spain | 2009 | Serum | 0% (0/1170) | n.d. | [47] | ||
| Hungary | 2005–2006 | Faeces liver | n.d. | 0% (0/30) 0% (0/2) | [48] | ||
| Hungary | 2005–2009 | Faeces | n.d. | 0% (0/125) | [49] | ||
| China | 2007 | Serum | 6.5% (13/200) | 0% (0/200) | [30] | ||
| China | 2008 | Serum | 28.2% (257/912) | 0% (0/912) | [31] | ||
| China | 2010 | Faeces | n.d. | 8.8% (8/91) | gt4 | [50] | |
| China | 2006 | Serum Milk | 25.3% (66/261) 14.9% (40/269) | 0% (0/261) 0% (0269) | [32] | ||
| USA | 2011 | Serum | 15.0% (174/1156) | 0% (0/174) | [38] | ||
| Egypt | 2010 | Serum | 21.6% (11/51) | n.d. | [40] | ||
| Croatia | 2009 | Blood, spleen, liver | n.d. | 0% (0/30) | [51] | ||
| China | 2011 | Serum | 47.0% (120/254) | 3.0% (8/254) | gt4 | [33] | |
| Nigeria | 2014 | Serum | 0% (0/37) | n.d. | [41] | ||
| China | 2015 | Faeces, serum, milk | n.d. | Faeces: 37.1% (52/140) Milk: 100.0% (52/52) * | gt4 | [52] | |
| Germany | 2008 | Bulk milk | n.d. | 0% (0/400) | [53] | ||
| Nigeria | 2018 | Serum | 0% (0/30) | n.d. | [42] | ||
| Vietnam | 2015 | Faeces | 6.8% (11/161) | 0% (0/120) | [34] | ||
| Belgium | 2016 | Milk | 0% (0/275) | 0% (0/1559) | [54] | ||
| USA | 2009 | Faeces | 20.4% (200/983) | 0% | [39] | ||
| Burkina Faso | 2019 | Serum | 26.4% (19/72) | n.d. | [43] | ||
| China | 2017 | Faeces, retail milk | 0% (0/416) | 0% (0/883) | [55] | ||
| Korea | 2017–2018 | Liver | n.d. | 1.0% (1/100) | gt4 | [56] | |
| Turkey | 2016 | Milk | n.d. | 29.2% (14/48) | gt1, gt3, gt4 | [57] | |
| Jordan | 2020 | Serum | 14.5% (18/124) | n.d. | [35] | ||
| Egypt | 2017 | Faeces, milk | 1.7% (8/480) | 0.2% (1/480) | gt3 | [44] | |
| Burkina Faso | 2017 | Serum | 5.1% (24/475) | n.d. | [45] | ||
| Bos grunniens (yak) | China | 2013 | Faeces | n.d. | 1.8% (3/167); Qinghai Province 3.3% (3/92), Gansu Province 0% (0/75) | gt4 | [58] |
| Buffaloes | India | 2007 | Serum | 100.0% (30/30) | n.d | [46] | |
| Bison bison | USA | 2011 | Serum | 4.6% (3/65) | 0% (0/3) | [38] | |
| Syncerus caffer | Egypt | 2010 | Serum | 14.0% (8/57) | n.d. | [40] |
| Country | Year | Type of Sample | Seroprevalence % (Positive/Total) | Molecular Prevalence % (Positive/Total) | Genotype (gt) | Reference |
|---|---|---|---|---|---|---|
| Turkmenistan | 1998 | Serum | 67.0% | 1 n.d. | [24] | |
| India | 1994 1999 | Serum Serum | 0% (0/52) 0% (0/188) | n.d. n.d. | [25] | |
| China | 2002 | Serum | 0% (0/316) | n.d. | [26] | |
| Brazil | 2005 | Serum | 0% (0/5) | n.d. | [37] | |
| India | 2007 | Serum | 100.0% (98/98) | n.d | [46] | |
| China | 2004 | Serum | 24.0% (12/50) | 0% (0/50) | [27] | |
| Spain | 2009 | Serum | 0.6% (7/1143) | n.d. | [47] | |
| China | 2007 | Serum | 7.5% (15/200) | 0% (0/200) | [30] | |
| China | 2008 | Serum | 10.4% (73/700) | 0% (0/700) | [31] | |
| USA | 2002 | Serum, faeces | 16.0% (13/80) | 0% (0/80) | [59] | |
| Egypt | 2010 | Serum | 9.4% (3/32) | n.d. | [40] | |
| Nigeria | 2014 | Serum | 37.2% (16/43) | n.d. | [41] | |
| Italy | 2012 | Faeces | n.d. | 9.2% (11/119) | gt3 | [60] |
| China | 2015 | Faeces, serum, milk | IgM: 3.6% (1/28) IgG: 14.3% (4/28) | 2015 faeces: 74.1% (40/54) 2016 faeces: 60.0% (12/ 20) Serum: 53.6% (15/28) Milk: 100.0% (4/4) * | gt4 | [61] |
| China | 2017 | Serum, liver | 46.7% (50/120) | 4.0% (2/50) | gt4 | [62] |
| Burkina Faso | 2015 | Serum | 28.4% (23/81) | n.d. | [43] | |
| Nigeria | 2018 | Serum | 0% (0/26) | n.d. | [39] | |
| Turkey | 2016 | Milk | n.d. | 18.5% (12/65) | gt1, gt3, gt4 | [57] |
| Egypt | 2017 | Milk | 7.1% (20/280) | 0.7% (2/280) | gt3 | [63] |
| Italy | 2017 | Serum, faeces | 11.4% (19/167) | 0.0% (0/167) | [64] | |
| Czech Republic | 2019 | Milk | n.d. | 1.4% (4/290) | [65] | |
| Spain | 2015 | Serum | 13.8% (33/240) | 0% (0/240) | [66] | |
| China | 2014 | Serum | 26.1% (47/180) | n.d. | [67] |
| Country | Year | Type of Sample | Seroprevalence % (Positive/Total) | Molecular Prevalence % (Positive/Total) | Genotype (gt) | Reference |
|---|---|---|---|---|---|---|
| Turkmenistan | 1998 | Serum | 42.0% | 1 n.d. | [24] | |
| Brazil | 2005 | Serum | 0% (0/12) | n.d. | [37] | |
| India | 2007 | Serum | 100.0% (58/58) 78.0% (47/58) | n.d | [46] | |
| China | 2004–2006 | Serum | 9.8% (20/207) | n.d | [29] | |
| Spain | 2009 | Serum | 1.9% (36/1357) | n.d. | [47] | |
| China | 2009 | Serum | 12.4% (162/1302) | 1.7% (2/115) | [28] | |
| China | 2010 | Serum | 9.9% (33/334) | n.d. | [31] | |
| China | 2010 | Serum | 28.9% (142/490) | n.d. | [69] | |
| China | 2010 | Faeces | n.d. | 11.1% (6/54) | gt4 | [74] |
| China | 2006 | Serum | 9.3% (53/541) | 0% (0/541) | [32] | |
| Egypt | 2010 | Serum | 4.4% (2/45) | n.d. | [40] | |
| Nigeria | 2012 | Serum | 10.5% (2/19) | n.d. | [41] | |
| China | 2014 | Serum, liver | 35.2 % (176/500) | 5.3% (4/75) | gt4 | [70] |
| China | 2011 | Serum | 32.0% (70/222) | 11.4% (8/70) | gt4 | [33] |
| Nigeria | 2017 | Serum | 31.8% (56/176) | n.d. | [71] | |
| Italy | 2018 | Serum, faeces | 21.3% (40/192) | Faeces: 10.4% (20/192) Serum: 1.6% (3/192) | gt3 | [72] |
| Burkina Faso | 2019 | Serum | 12.0% (9/75) | n.d. | [43] | |
| Turkey | 2016 | Milk | n.d. | 12.3% (8/65) | gt1, gt3, gt4 | [57] |
| Italy | 2017 | Serum, faeces | 21.6 % (29/134 ) | 3.0% (4/134) | [64] | |
| Jordan | 2020 | Serum | 12.7% (26/205) | n.d. | [35] | |
| Czech Republic | 2019 | Milk | n.d. | 1.4% (4/290) | [65] | |
| Portugal | 2016 | Serum | 16.6% (15/90) | n.d | [73] | |
| Spain | 2015–2017 | Serum | 2.1% (5/240) | 0% (0/240) | [66] |
| Animal Species | Scientific Name | Country | Type of Sample | Seroprevalence % (Positive/Total) | Molecular Prevalence % (Positive/Total) | Genotype (gt) | Reference |
|---|---|---|---|---|---|---|---|
| Sika deer | Cervus nippon | Japan | Serum, liver | 2.0% (2/117) | 0% (0/117) | [75] | |
| Japan | Serum, faeces, liver | 2.6% (25/976) | 0% (0/501) | [76] | |||
| USA | Serum | 0% (0/174) | n.d. | [82] | |||
| China | faeces | 1 n.d. | 25.0% (2/8) | gt4 | [102] | ||
| Poland | Serum | 0% (0/68) | n.d. | [87] | |||
| China | Serum | 5.4% (46/847) | n.d. | [77] | |||
| Germany | Serum, liver | 0% (0/12) | 0% (0/12) | [96] | |||
| Japan | Serum, liver | 4.3% (17/395) | 0.2% (1/199) | gt3 | [78] | ||
| Japan | Serum | 0.04% (1/2250) | 0.06% (1/1688) | gt4 | [79] | ||
| Yezo deer | Cervus nippon yesoensis | Japan | Serum | 34.8% (181/250) | n.d. | [80] | |
| Roe deer | Capreolus capreolus | Hungary | Faeces, liver | n.d. | 34.1% (11/32) | gt3 | [48] |
| Hungary | Faeces, liver | n.d. | 22.0% (9/41) | gt3 | [49] | ||
| Netherlands | Serum, faeces, Liver, muscle | 0% (0/8) | 0% (0/8) | [86] | |||
| Poland | Serum | 0% (0/38) | n.d. | [87] | |||
| Belgium | Serum, liver | 3% | 0% (0/27) | [94] | |||
| Italy | Liver | n.d. | 0% (0/30) | [106] | |||
| Czech Republic | Faeces | n.d. | 3.3% (1/30) | [104] | |||
| Croatia | Blood, spleen, liver | n.d. | 0% (0/40) | [51] | |||
| Germany | Serum, liver | 2000–2001: 6.8% 2012–2013: 5.4% | 2000–2001: 0% 2012–2013: 0% | [91] | |||
| Sweden | Serum, faeces | 6.9% (2/29) | 0% (0/29) | [92] | |||
| Germany | Serum, liver, muscle, spleen, kidney | 0% (0/59) | 6.4% (5/78) | gt3 | [93] | ||
| Lithuania | Serum, liver | n.d. | 22.6% (21/93) | gt3 | [107] | ||
| Italy | Serum, faeces | 3.1% (1/32) | 0% (0/32) | [64] | |||
| Italy | Liver | n.d. | 0% (0/6) | [108] | |||
| Norway | Serum | 0% (0/86) | n.d. | [100] | |||
| Italy | Serum | 0.4% (1/227) | n.d. | [101] | |||
| Italy | Liver | n.d. | 10.4% (5/48) | gt3 | [110] | ||
| Red deer | Cervus elaphus | Spain | Serum | 10.4% (101/968) | 13.6% (11/81) | gt3 | [85] |
| Hungary | Faeces, liver | n.d. | 10.0% (3/30) | gt3 | [49] | ||
| Netherlands | Serum, faeces, Liver, muscle | 5.0% (2/38) | 15.0% (6/39) | [86] | |||
| Poland | Serum | 0% (0/118) | n.d. | [87] | |||
| Italy | Serum | 5.6% (3/54) | n.d. | [90] | |||
| Belgium | Serum, liver | 1% | 3.4% (1/29) | gt3 | [94] | ||
| Spain | Serum | 12.9% (9/70) | 16.1% (13/81) | gt3 | [88] | ||
| Italy | Serum | 13.9% (35/251) | 10.9% (10/91) | gt3 | [95] | ||
| Czech Republic | Faeces | n.d. | 1.2% (2/169) | [104] | |||
| France | Liver, bile | n.d. | 3.2% (2/62) | [105] | |||
| Croatia | Blood, spleen, liver | n.d. | 0% (0/280) | [51] | |||
| Germany | Serum, liver | 2000–2001: 2% 2012–2013: 3.3% | 2000–2001: 1.9% 2012–2013: 6.6% | [91] | |||
| Sweden | Serum, faeces | 7.1% (1/14) | 0% (0/14) | [92] | |||
| Germany | Serum, liver, muscle, spleen, kidney | 0% (0/78) | 2.4% (2/83) | gt3 | [93] | ||
| Lithuania | Serum, liver | n.d. | 6.7% (1/15) | [107] | |||
| Germany | Serum, liver | 0% (0/23) | 0% (0/22) | [96] | |||
| Italy | Serum | 0.8% (2/255) | 0% (0/255) | [98] | |||
| Italy | Serum, faeces | 2.6% (1/38) | 0% (0/38) | [64] | |||
| Finland | Serum | 0% (0/12) | 0% (0/12) | [97] | |||
| Italy | Liver | n.d. | 0% (0/218) | [108] | |||
| Norway | Serum | 4% (7/177) | n.d. | [100] | |||
| Portugal | Faeces | n.d. | 2.1% (2/95) | gt3 | [109] | ||
| Italy | Serum | 0% (0/96) | n.d. | [101] | |||
| Fallow deer | Dama dama | Poland | Serum | 0% (0/5) | n.d. | [87] | |
| Germany | Serum | 0% (0/46) | 4.3% (2/46) | [91] | |||
| Germany | Serum | 0% (0/22) | 0% (0/22) | [93] | |||
| Germany | Serum, liver | 0% (0/73) | 0% (0/72) | [96] | |||
| Portugal | Faeces | n.d. | 0% (0/35) | [109] | |||
| Italy | Liver | n.d. | 1.7% (1/60) | gt3 | [110] | ||
| Moose | Alces alces | Sweden | Liver, kidney | n.d. | Liver: 1/6 kidney: 0/6 | P. alci | [103] |
| Poland | Serum | 0% (0/1) | n.d. | [87] | |||
| Sweden | Serum, faeces, liver | 18.6% (43/231) | 14.7% (34/231) | P. alci | [89] | ||
| Sweden | Serum, faeces | 14.0% (9/66) | 15.1% (10/66) | P. alci | [92] | ||
| Lithuania | Serum | n.d. | 7.7% (1/13) | [107] | |||
| Finland | Serum | 9.1% (31/342) | 0% (0/342) | [97] | |||
| Norway | Serum | 19.5% (32/164) | n.d. | [100] | |||
| Tufted deer | Elaphodus cephalophus | China | Faeces | n.d. | 50.0% (4/8) | gt4 | [102] |
| White tailed deer | Odocoleicus virginianus | Mexico | Serum | 62.7% (89/142) | n.d. | [83] | |
| Canada | Serum | 8.8% (18/205) | 0% (0/205) | [84] | |||
| Finland | Serum | 1.4% (1/70) | 0% (0/70) | [97] | |||
| Mule deer | Odocoleicus hemionus | Canada | Serum | 4.5% (5/112) | 0% (0/112) | [84] | |
| Barren-ground caribou | Rangifer tarandus groenlandicus | Canada | Serum | 1.7% (2/120) | 0% (0/120) | [84] | |
| Woodland caribou | Rangifer tarandus caribou | Canada | Serum | 5.2% (5/97) | 0% (0/97) | [84] | |
| Eurasian tundra reindeer | Rangifer tarandus tarandus | Russia | Serum | 12.0% (23/191) | 0% (0/191) | [81] | |
| Norway | Serum | 23.1% (43/186) | n.d. | [100] | |||
| Norway | Serum | 15.7% (81/516) | n.d. | [99] | |||
| Reeves’s muntjac | Muntiacus reevesi | China | Faeces | n.d. | 50.0% (1/2) | gt4 | [102] |
| Japan | Serum | 0% (0/1) | n.d. | [79] | |||
| Tatra chamois | Rupicapra rupicapra tatrica | Poland | Serum | 0% (0/4) | n.d. | [87] | |
| Chamois | Rupricapra rupricapra | Italy | Serum | 1.2% (2/172) | 0% (0/172) | [98] | |
| Italy | Serum, faeces | 0% (0/13) | 0% (0/13) | [64] | |||
| Italy | Liver | n.d. | 0% (0/4) | [108] | |||
| Italy | Serum | 5.1% (5/92) | n.d. | [101] | |||
| Alpine ibex | Capra ibex | Italy | Serum, faeces | 6.3% (2/32) | 0% (0/32) | [64] | |
| Muskox | Ovibos moschatus | Norway | Serum | 5.9% (6/102) | n.d. | [100] | |
| European bison | Bison bonasus | Poland | Serum | 0% (0/68) | n.d. | [87] | |
| European muflon | Ovis aries musimon | Czech Republic | Faeces | n.d. | 12.8% (5/39) | [104] | |
| Croatia | Blood, spleen, liver | n.d. | 0% (0/12) | [51] | |||
| Italy | Serum | 2.0% (1/49) | n.d. | [101] | |||
| Persian gazelle | Gazella subgutturosa | Iran | Faeces | n.d. | 6.0% (3/50) | [111] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Profio, F.; Sarchese, V.; Palombieri, A.; Fruci, P.; Lanave, G.; Robetto, S.; Martella, V.; Di Martino, B. Current Knowledge of Hepatitis E Virus (HEV) Epidemiology in Ruminants. Pathogens 2022, 11, 1124. https://doi.org/10.3390/pathogens11101124
Di Profio F, Sarchese V, Palombieri A, Fruci P, Lanave G, Robetto S, Martella V, Di Martino B. Current Knowledge of Hepatitis E Virus (HEV) Epidemiology in Ruminants. Pathogens. 2022; 11(10):1124. https://doi.org/10.3390/pathogens11101124
Chicago/Turabian StyleDi Profio, Federica, Vittorio Sarchese, Andrea Palombieri, Paola Fruci, Gianvito Lanave, Serena Robetto, Vito Martella, and Barbara Di Martino. 2022. "Current Knowledge of Hepatitis E Virus (HEV) Epidemiology in Ruminants" Pathogens 11, no. 10: 1124. https://doi.org/10.3390/pathogens11101124
APA StyleDi Profio, F., Sarchese, V., Palombieri, A., Fruci, P., Lanave, G., Robetto, S., Martella, V., & Di Martino, B. (2022). Current Knowledge of Hepatitis E Virus (HEV) Epidemiology in Ruminants. Pathogens, 11(10), 1124. https://doi.org/10.3390/pathogens11101124








