Reemerging Influenza Virus Infections during the Dominance of the Omicron SARS-CoV-2 Variant in Mexico
Abstract
:1. Introduction
2. Materials and Methods
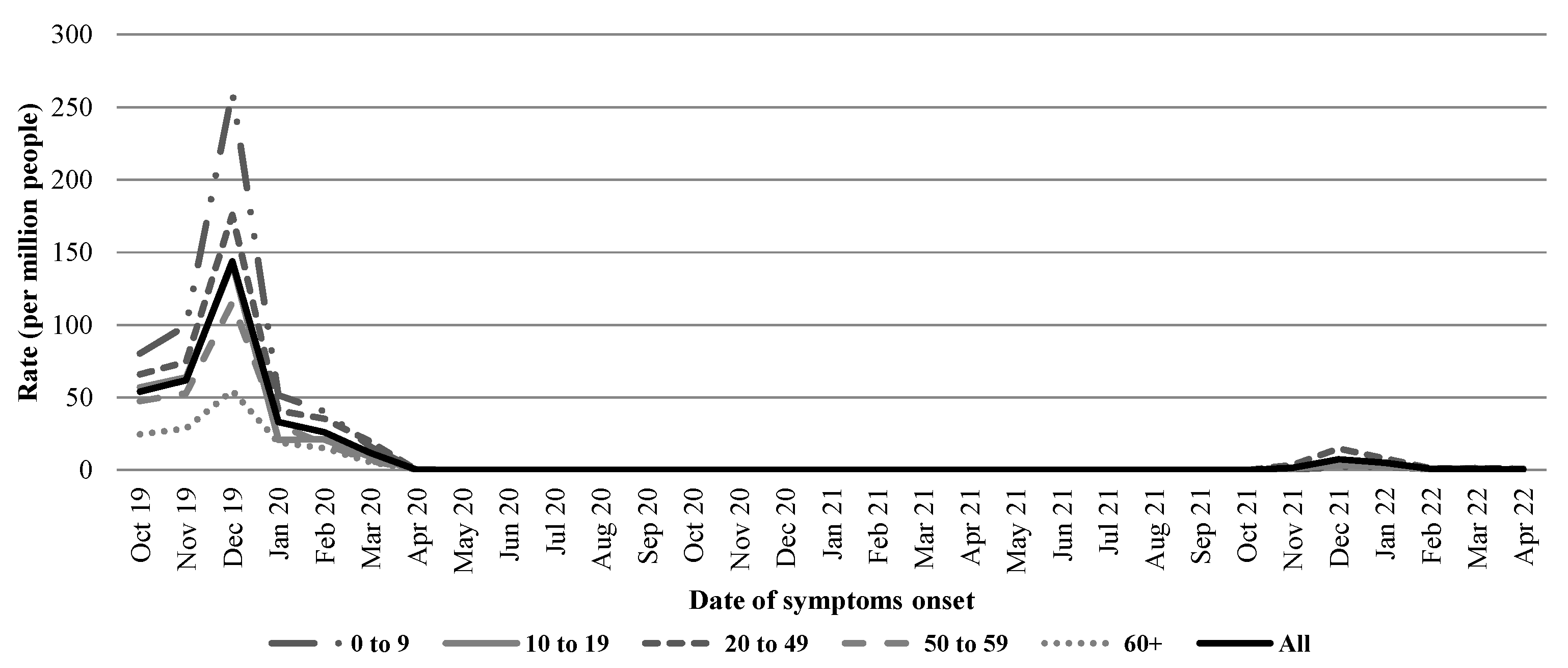
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murillo-Zamora, E.; Trujillo, X.; Huerta, M.; Rios-Silva, M.; Guzman-Esquivel, J.; Benites-Godinez, V.; Mendoza-Cano, O. Survival in Influenza Virus-Related Pneumonia by Viral Subtype: 2016–2020. Int. J. Infect. Dis. 2021, 112, 288–293. [Google Scholar] [CrossRef] [PubMed]
- Liu, P.; Xu, M.; Lu, L.; Ma, A.; Cao, L.; Su, L.; Dong, N.; Jia, R.; Zhu, X.; Xu, J. The Changing Pattern of Common Respiratory and Enteric Viruses among Outpatient Children in Shanghai, China: Two Years of the COVID-19 Pandemic. J. Med. Virol. 2022, 94, 4696–4703. [Google Scholar] [CrossRef]
- Qi, Y.; Shaman, J.; Pei, S. Quantifying the Impact of Covid-19 Nonpharmaceutical Interventions on Influenza Transmission in the United States. J. Infect. Dis. 2021, 224, 1500–1508. [Google Scholar] [CrossRef]
- Government of Mexico. Comprehensive Report on COVID-19 in Mexico (Number 08-2022). Available online: https://epidemiologia.salud.gob.mx/gobmx/salud/documentos/covid19/info-08-22-int_covid-19.pdf (accessed on 3 September 2022).
- Cao, Y.; Wang, J.; Jian, F.; Xiao, T.; Song, W.; Yisimayi, A.; Huang, W.; Li, Q.; Wang, P.; An, R.; et al. Omicron Escapes the Majority of Existing SARS-CoV-2 Neutralizing Antibodies. Nature 2022, 602, 657–663. [Google Scholar] [CrossRef] [PubMed]
- General Directorate of Epidemiology of Mexico. Genomic Surveillance Report of the SARS-CoV-2 Virus in Mexico, National and State Distribution of Variants as of 4 April 2022. Available online: https://coronavirus.gob.mx/wp-content/uploads/2022/04/2022.04.04-varientes-covid-mx.pdf (accessed on 28 August 2022).
- Fernandes-Matano, L.; Monroy-Munoz, I.E.; Bermudez de Leon, M.; Leal-Herrera, Y.A.; Palomec-Nava, Y.D.; Ruiz-Pacheco, J.A.; Escobedo-Guajardo, B.L.; Marin-Budip, C.; Santacruz-Tinoco, C.E.; Gonzalez-Ibarra, J.; et al. Analysis of Influenza Data Generated by Four Epidemiological Surveillance Laboratories in Mexico, 2010–2016. Epidemiol. Infect. 2019, 147, e183. [Google Scholar] [CrossRef] [Green Version]
- Lu, Y.; Wang, Y.; Shen, C.; Luo, J.; Yu, W. Decreased Incidence of Influenza During the COVID-19 Pandemic. Int. J. Gen. Med. 2022, 15, 2957–2962. [Google Scholar] [CrossRef] [PubMed]
- Murillo-Zamora, E.; Guzman-Esquivel, J.; Sanchez-Pina, R.A.; Cedeno-Laurent, G.; Delgado-Enciso, I.; Mendoza-Cano, O. Physical Distancing Reduced the Incidence of Influenza and Supports a Favorable Impact on SARS-CoV-2 Spread in Mexico. J. Infect. Dev. Ctries. 2020, 14, 953–956. [Google Scholar] [CrossRef]
- Yeoh, D.K.; Foley, D.A.; Minney-Smith, C.A.; Martin, A.C.; Mace, A.O.; Sikazwe, C.T.; Le, H.; Levy, A.; Blyth, C.C.; Moore, H.C. Impact of Coronavirus Disease 2019 Public Health Measures on Detections of Influenza and Respiratory Syncytial Virus in Children during the 2020 Australian Winter. Clin. Infect. Dis. 2021, 72, 2199–2202. [Google Scholar] [CrossRef]
- Suarez, V.; Suarez Quezada, M.; Oros Ruiz, S.; Ronquillo de Jesus, E. Epidemiology of COVID-19 in Mexico: From the 27th of February to the 30th of April 2020. Rev. Clin. Esp. 2020, 220, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Moncion, K.; Young, K.; Tunis, M.; Rempel, S.; Stirling, R.; Zhao, L. Effectiveness of Hand Hygiene Practices in Preventing Influenza Virus Infection in the Community Setting: A Systematic Review. Can. Commun. Dis. Rep. 2019, 45, 12–23. [Google Scholar] [CrossRef]
- Wagatsuma, K.; Koolhof, I.S.; Saito, R. Was the Reduction in Seasonal Influenza Transmission during 2020 Attributable to Non-Pharmaceutical Interventions to Contain Coronavirus Disease 2019 (COVID-19) in Japan? Viruses 2022, 14, 1417. [Google Scholar] [CrossRef] [PubMed]
- Kuehn, B.M. Influenza Vaccination Increased during the COVID-19 Pandemic. JAMA 2021, 326, 2465. [Google Scholar] [CrossRef]
- Menni, C.; Valdes, A.M.; Polidori, L.; Antonelli, M.; Penamakuri, S.; Nogal, A.; Louca, P.; May, A.; Figueiredo, J.C.; Hu, C.; et al. Symptom Prevalence, Duration, and Risk of Hospital Admission in Individuals Infected with Sars-Cov-2 during Periods of Omicron and Delta Variant Dominance: A Prospective Observational Study from the Zoe Covid Study. Lancet 2022, 399, 1618–1624. [Google Scholar] [CrossRef]
- Lai, S.; Ruktanonchai, N.W.; Zhou, L.; Prosper, O.; Luo, W.; Floyd, J.R.; Wesolowski, A.; Santillana, M.; Zhang, C.; Du, X.; et al. Effect of Non-Pharmaceutical Interventions to Contain COVID-19 in China. Nature 2020, 585, 410–413. [Google Scholar] [CrossRef]
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W.; et al. Estimating the Effects of Non-Pharmaceutical Interventions on Covid-19 in Europe. Nature 2020, 584, 257–261. [Google Scholar] [CrossRef]
- Merced-Morales, A.; Daly, P.; Abd Elal, A.I.; Ajayi, N.; Annan, E.; Budd, A.; Barnes, J.; Colon, A.; Cummings, C.N.; Iuliano, A.D.; et al. Influenza Activity and Composition of the 2022–2023 Influenza Vaccine—United States, 2021–2022 Season. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 913–919. [Google Scholar] [CrossRef]
- Ruiz-Matus, C.; Kuri-Morales, P.; Narro-Robles, J. Behavior of Influenza Seasons in Mexico from 2010 to 2016: Analysis and Prospective. Gac. Med. Mex. 2017, 153, 205–213. [Google Scholar] [PubMed]
- Pan American Health Organization. Regional Update, Influenza. Epidemiological Week 37 (28 September 2022). Available online: https://iris.paho.org/handle/10665.2/56485 (accessed on 8 October 2022).
- Centers for Disease Control and Prevention. 2020–2021 Flu Season Summary. Available online: https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm#anchor_1627000307956 (accessed on 3 September 2022).

| Characteristic | Overall, n (%) | Flu Season, n (%) | p | ||||
|---|---|---|---|---|---|---|---|
| 2019–2020 | 2021–2022 | ||||||
| Gender | |||||||
| Female | 3099 | (54.8) | 2633 | (54.5) | 466 | (57.1) | 0.158 |
| Male | 2553 | (45.2) | 2203 | (45.5) | 350 | (42.9) | |
| Age group (years) | |||||||
| 0 to 9 | 997 | (17.6) | 955 | 19.8 | 42 | 5.2 | <0.001 |
| 10 to 19 | 504 | (8.9) | 452 | 9.4 | 52 | 6.4 | |
| 20 to 39 | 2371 | (42.0) | 1927 | 39.9 | 444 | 54.4 | |
| 40 to 59 | 1122 | (19.9) | 972 | 20.1 | 150 | 18.4 | |
| 60 or above | 658 | (11.6) | 530 | 11.0 | 128 | 15.7 | |
| Flu-vaccinated a | |||||||
| No | 4710 | (83.3) | 3979 | 82.3 | 731 | 89.6 | <0.001 |
| Yes | 942 | (16.7) | 857 | 17.7 | 85 | 10.4 | |
| Pneumonia b | |||||||
| No | 5051 | (89.4) | 4292 | 88.75 | 759 | 93.01 | <0.001 |
| Yes | 601 | (10.6) | 544 | 11.25 | 57 | 6.99 | |
| Hospital admission | |||||||
| No | 3197 | (56.6) | 2610 | 54.0 | 587 | 71.9 | <0.001 |
| Yes | 2455 | (43.4) | 2226 | 46.0 | 229 | 28.1 | |
| Disease outcome | |||||||
| Recovery | 5362 | (94.9) | 4591 | 94.9 | 771 | 94.5 | 0.591 |
| Death | 290 | (5.1) | 245 | 5.1 | 45 | 5.5 | |
| Characteristic | RR (95% CI), p | |||
|---|---|---|---|---|
| Bivariate Analysis | Multiple Analysis | |||
| Gender | ||||
| Female | 1.00 | 1.00 | ||
| Male | 1.02 (1.01–1.03) | 0.004 | 1.02 (1.01–1.03) | 0.004 |
| Age group (years) | ||||
| 0 to 9 | 1.00 | 1.00 | ||
| 10 to 19 | 0.99 (0.98–1.02) | 0.974 | 1.01 (0.98–1.03) | 0.765 |
| 20 to 39 | 0.99 (0.98–1.01) | 0.846 | 1.01 (0.99–1.02) | 0.693 |
| 40 to 59 | 1.08 (1.06–1.10) | <0.001 | 1.07 (1.05–1.09) | <0.001 |
| 60 or above | 1.23 (1.21–1.26) | <0.001 | 1.23 (1.20–1.27) | <0.001 |
| Influenza season of symptom onset a | ||||
| 2019–2020 | 1.00 | 1.00 | ||
| 2021–2022 | 1.01 (0.99–1.02) | 0.588 | 1.01 (0.99–1.03) | 0.211 |
| Flu-vaccinated b | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.96 (0.95–0.98) | <0.001 | 0.97 (0.96–0.99) | <0.001 |
| Identified virus subtype | ||||
| AH1N1 | 1.00 | 1.00 | ||
| AH3N2 | 0.96 (0.94–0.97) | <0.001 | 0.96 (0.95–0.98) | <0.001 |
| A non-typified | 0.98 (0.93–1.02) | 0.272 | 0.98 (0.94–1.01) | 0.161 |
| B Victoria lineage | 0.93 (0.92–0.94) | <0.001 | 0.96 (0.95–0.98) | <0.001 |
| B Yamagata lineage | 0.96 (0.91–1.01) | 0.128 | 0.95 (0.91–0.99) | 0.046 |
| B non-typified | 0.97 (0.92–1.02) | 0.262 | 0.97 (0.92–1.03) | 0.335 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ríos-Silva, M.; Trujillo, X.; Huerta, M.; Benites-Godínez, V.; Guzmán-Esquivel, J.; Bricio-Barrios, J.A.; Mendoza-Cano, O.; Lugo-Radillo, A.; Murillo-Zamora, E. Reemerging Influenza Virus Infections during the Dominance of the Omicron SARS-CoV-2 Variant in Mexico. Pathogens 2022, 11, 1181. https://doi.org/10.3390/pathogens11101181
Ríos-Silva M, Trujillo X, Huerta M, Benites-Godínez V, Guzmán-Esquivel J, Bricio-Barrios JA, Mendoza-Cano O, Lugo-Radillo A, Murillo-Zamora E. Reemerging Influenza Virus Infections during the Dominance of the Omicron SARS-CoV-2 Variant in Mexico. Pathogens. 2022; 11(10):1181. https://doi.org/10.3390/pathogens11101181
Chicago/Turabian StyleRíos-Silva, Mónica, Xóchitl Trujillo, Miguel Huerta, Verónica Benites-Godínez, José Guzmán-Esquivel, Jaime Alberto Bricio-Barrios, Oliver Mendoza-Cano, Agustín Lugo-Radillo, and Efrén Murillo-Zamora. 2022. "Reemerging Influenza Virus Infections during the Dominance of the Omicron SARS-CoV-2 Variant in Mexico" Pathogens 11, no. 10: 1181. https://doi.org/10.3390/pathogens11101181
APA StyleRíos-Silva, M., Trujillo, X., Huerta, M., Benites-Godínez, V., Guzmán-Esquivel, J., Bricio-Barrios, J. A., Mendoza-Cano, O., Lugo-Radillo, A., & Murillo-Zamora, E. (2022). Reemerging Influenza Virus Infections during the Dominance of the Omicron SARS-CoV-2 Variant in Mexico. Pathogens, 11(10), 1181. https://doi.org/10.3390/pathogens11101181








