A Population-Based Evaluation of Polymicrobial Staphylococcus aureus Bacteremia
Abstract
:1. Introduction
2. Material and Methods
3. Statistical Analysis
4. Results
4.1. Incidence of p-SAB
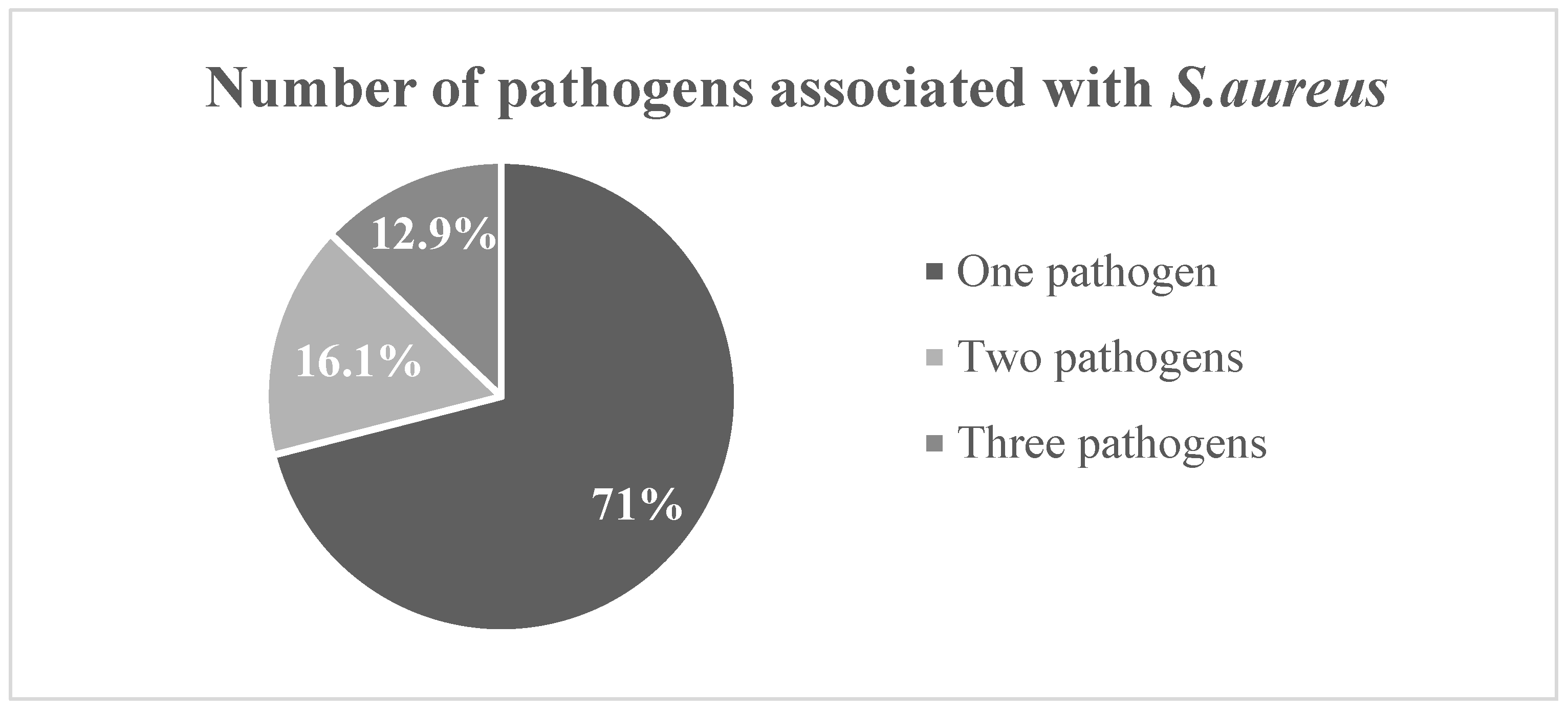
4.2. Microbiology of p-SAB
4.3. Baseline Characteristics of p-SAB and m-SAB
4.4. Outcomes in p-SAB and m-SAB Patients
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rello, J.; Quintana, E.; Mirelis, B.; Gurguí, M.; Net, A.; Prats, G. Polymicrobial Bacteremia in Critically Ill Patients. Intensive Care Med. 1993, 19, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.-N.; Lai, C.-H.; Chen, Y.-H.; Chang, L.-L.; Lu, P.-L.; Tsai, S.-S.; Lin, H.-L.; Lin, H.-H. Characteristics and Outcomes of Polymicrobial Bloodstream Infections in the Emergency Department: A Matched Case–Control Study. Acad. Emerg. Med. 2010, 17, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Pavlaki, M.; Poulakou, G.; Drimousis, P.; Adamis, G.; Apostolidou, E.; Gatselis, N.K.; Kritselis, I.; Mega, A.; Mylona, V.; Papatsoris, A.; et al. Polymicrobial Bloodstream Infections: Epidemiology and Impact on Mortality. J. Glob. Antimicrob. Resist. 2013, 1, 207–212. [Google Scholar] [CrossRef]
- Uslan, D.Z.; Crane, S.J.; Steckelberg, J.M.; Cockerill, F.R.; St Sauver, J.L.; Wilson, W.R.; Baddour, L.M. Age- and Sex-Associated Trends in Bloodstream Infection: A Population-Based Study in Olmsted County, Minnesota. Arch. Intern. Med. 2007, 167, 834–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wisplinghoff, H.; Bischoff, T.; Tallent, S.M.; Seifert, H.; Wenzel, R.P.; Edmond, M.B. Nosocomial Bloodstream Infections in US Hospitals: Analysis of 24,179 Cases from a Prospective Nationwide Surveillance Study. Clin. Infect. Dis. 2004, 39, 309–317. [Google Scholar] [CrossRef] [Green Version]
- Verway, M.; Brown, K.A.; Marchand-Austin, A.; Diong, C.; Lee, S.; Langford, B.; Schwartz, K.L.; MacFadden, D.R.; Patel, S.N.; Sander, B.; et al. Prevalence and Mortality Associated with Bloodstream Organisms: A Population-Wide Retrospective Cohort Study. J. Clin. Microbiol. 2022, 60, e0242921. [Google Scholar] [CrossRef]
- Kaasch, A.J.; Barlow, G.; Edgeworth, J.D.; Fowler, V.G.; Hellmich, M.; Hopkins, S.; Kern, W.V.; Llewelyn, M.J.; Rieg, S.; Rodriguez-Baño, J.; et al. Staphylococcus aureus Bloodstream Infection: A Pooled Analysis of Five Prospective, Observational Studies. J. Infect. 2014, 68, 242–251. [Google Scholar] [CrossRef] [Green Version]
- Khatib, R.; Sharma, M.; Johnson, L.B.; Riederer, K.; Briski, L. Polymicrobial Staphylococcus aureus Bacteremia: Frequency, Distinguishing Characteristics and Outcome. Diagn. Microbiol. Infect. Dis. 2016, 86, 311–315. [Google Scholar] [CrossRef]
- Park, S.Y.; Park, K.-H.; Bang, K.M.; Chong, Y.P.; Kim, S.-H.; Lee, S.-O.; Choi, S.-H.; Jeong, J.-Y.; Woo, J.H.; Kim, Y.S. Clinical Significance and Outcome of Polymicrobial Staphylococcus aureus Bacteremia. J. Infect. 2012, 65, 119–127. [Google Scholar] [CrossRef]
- Zheng, C.; Zhang, S.; Chen, Q.; Zhong, L.; Huang, T.; Zhang, X.; Zhang, K.; Zhou, H.; Cai, J.; Du, L.; et al. Clinical Characteristics and Risk Factors of Polymicrobial Staphylococcus aureus Bloodstream Infections. Antimicrob. Resist. Infect. Control 2020, 9, 76. [Google Scholar] [CrossRef]
- Laupland, K.B.; Kibsey, P.C.; Gregson, D.B.; Galbraith, J.C. Population-Based Laboratory Assessment of the Burden of Community-Onset Bloodstream Infection in Victoria, Canada. Epidemiol. Infect. 2013, 141, 174–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asgeirsson, H.; Gudlaugsson, O.; Kristinsson, K.G.; Heiddal, S.; Kristjansson, M. Staphylococcus aureus Bacteraemia in Iceland, 1995–2008: Changing Incidence and Mortality. Clin. Microbiol. Infect. 2011, 17, 513–518. [Google Scholar] [CrossRef] [Green Version]
- Hindy, J.-R.; Quintero-Martinez, J.A.; Lahr, B.D.; Palraj, R.; Go, J.R.; Fida, M.; Abu Saleh, O.M.; Arshad, V.; Talha, K.M.; DeSimone, D.C.; et al. Incidence of Monomicrobial Staphylococcus aureus Bacteremia: A Population-Based Study in Olmsted County, Minnesota—2006 to 2020. Open Forum Infect. Dis. 2022, 9, ofac190. [Google Scholar] [CrossRef] [PubMed]
- Melton, L.J. History of the Rochester Epidemiology Project. Mayo Clin. Proc. 1996, 71, 266–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Fowler, V.G., Jr.; Olsen, M.K.; Corey, G.R.; Woods, C.W.; Cabell, C.H.; Reller, L.B.; Cheng, A.C.; Dudley, T.; Oddone, E.Z. Clinical Identifiers of Complicated Staphylococcus aureus Bacteremia. Arch. Intern. Med. 2003, 163, 2066–2072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedman, N.D.; Kaye, K.S.; Stout, J.E.; McGarry, S.A.; Trivette, S.L.; Briggs, J.P.; Lamm, W.; Clark, C.; MacFarquhar, J.; Walton, A.L.; et al. Health Care--Associated Bloodstream Infections in Adults: A Reason to Change the Accepted Definition of Community-Acquired Infections. Ann. Intern. Med. 2002, 137, 791–797. [Google Scholar] [CrossRef]
- Chong, Y.P.; Moon, S.M.; Bang, K.-M.; Park, H.J.; Park, S.-Y.; Kim, M.-N.; Park, K.-H.; Kim, S.-H.; Lee, S.-O.; Choi, S.-H.; et al. Treatment Duration for Uncomplicated Staphylococcus aureus Bacteremia To Prevent Relapse: Analysis of a Prospective Observational Cohort Study. Antimicrob. Agents Chemother. 2013, 57, 1150–1156. [Google Scholar] [CrossRef] [Green Version]
- Hall, K.K.; Lyman, J.A. Updated Review of Blood Culture Contamination. Clin. Microbiol. Rev. 2006, 19, 788–802. [Google Scholar] [CrossRef] [Green Version]
- Hindy, J.-R.; Quintero-Martinez, J.A.; Lee, A.T.; Scott, C.G.; Gerberi, D.J.; Mahmood, M.; DeSimone, D.C.; Baddour, L.M. Incidence Trends and Epidemiology of Staphylococcus aureus Bacteremia: A Systematic Review of Population-Based Studies. Cureus 2022, 14, e25460. [Google Scholar] [CrossRef]
- Austin, T.W.; Austin, M.A.; Coleman, B. Methicillin-Resistant/Methicillin-Sensitive Staphylococcus aureus Bacteremia. Saudi Med. J. 2003, 24, 256–260. [Google Scholar] [PubMed]
- Shabbir, S.; Jamil, S.; Hafiz, S. Pattern of Polymicrobial Isolates and Antimicrobial Susceptibility from Blood. J. Coll. Physicians Surg. Pak. 2016, 26, 585–588. [Google Scholar] [PubMed]
- Laupland, K.B.; Steele, L.; Pasquill, K.; Parfitt, E.C. Staphylococcus aureus Bloodstream Infection: Secular Changes Associated with the Implementation of a de Novo Clinical Infectious Diseases Service in a Canadian Population. Int. J. Infect. Dis. 2021, 104, 45–49. [Google Scholar] [CrossRef]
- Vogel, M.; Schmitz, R.P.H.; Hagel, S.; Pletz, M.W.; Gagelmann, N.; Scherag, A.; Schlattmann, P.; Brunkhorst, F.M. Infectious Disease Consultation for Staphylococcus aureus Bacteremia—A Systematic Review and Meta-Analysis. J. Infect. 2016, 72, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, J.; Solligård, E.; Damås, J.K.; DeWan, A.; Åsvold, B.O.; Bracken, M.B. The Impact of Infectious Disease Specialist Consultation for Staphylococcus aureus Bloodstream Infections: A Systematic Review. Open Forum Infect. Dis. 2016, 3, ofw048. [Google Scholar] [CrossRef] [Green Version]
- Lam, J.C.; Gregson, D.B.; Robinson, S.; Somayaji, R.; Welikovitch, L.; Conly, J.M.; Parkins, M.D. Infectious Diseases Consultation Improves Key Performance Metrics in the Management of Staphylococcus aureus Bacteremia: A Multicentre Cohort Study. Off. J. Assoc. Med. Microbiol. Infect. Dis. Can. 2019, 4, 24–32. [Google Scholar] [CrossRef]


| Female | Male | Total | ||||
|---|---|---|---|---|---|---|
| No. | IR | No. | IR | No. | IR | |
| Age Category | ||||||
| 18–49 | 2 | 0.4 | 2 | 0.4 | 4 | 0.4 |
| 50–64 | 5 | 2.3 | 6 | 3.0 | 11 | 2.6 |
| 65–79 | 4 | 3.3 | 7 | 6.9 | 11 | 5.0 |
| 80–100 | 2 | 3.8 | 3 | 9.1 | 5 | 5.9 |
| All ages | 13 | 1.4 | 18 | 2.2 | 31 | 1.8 |
| Calendar Year | ||||||
| 2006–2010 | 6 | 2.1 | 4 | 1.6 | 10 | 1.8 |
| 2011–2015 | 3 | 1.0 | 2 | 0.7 | 5 | 0.9 |
| 2016–2020 | 4 | 1.2 | 12 | 4.2 | 16 | 2.6 |
| Overall | 13 | 1.5 (0.7–2.3) 1 | 18 | 2.6 (1.4–3.8) 1 | 31 | 1.9 (1.3–2.6) 2 |
| Cases of Polymicrobial SAB | n = 31 |
|---|---|
| Gram positive | 15 (48.4%) |
| Bacillus cereus/thuringiensis | 1 (3.2%) |
| Enterococcus species | 3 (9.7%) |
| Enterococcus faecalis | 3 (9.7%) |
| Enterococcus faecalis + Staphylococcus warneri + Staphylococcus epidermidis | 1 (3.2%) |
| Enterococcus faecium | 1 (3.2%) |
| Staphylococcus epidermidis | 1 (3.2%) |
| Streptococcus agalactiae | 2 (6.5%) |
| Viridans group streptococci | 3 (9.7%) |
| Gram negative | 9 (29%) |
| Acinetobacter species | 1 (3.2%) |
| Escherichia coli | 2 (6.5%) |
| Klebsiella oxytoca | 1 (3.2%) |
| Proteus mirabilis | 1 (3.2%) |
| Pseudomonas aeruginosa | 2 (6.5%) |
| Pseudomonas aeruginosa + Enterobacter cloacae | 1 (3.2%) |
| Unidentified Gram-negative bacillus anaerobic | 1 (3.2%) |
| Gram positive plus Gram negative | 4 (12.9%) |
| Enterococcus faecalis + Enterobacter cloacae | 1 (3.2%) |
| Escherichia coli + Streptococcus mitis group + Gemella haemolysans | 1 (3.2%) |
| Klebsiella pneumoniae + Enterococcus faecalis + Veillonella species | 1 (3.2%) |
| Pseudomonas aeruginosa + Enterococcus faecalis | 1 (3.2%) |
| Bacteria plus Fungus | 3 (9.7%) |
| Proteus mirabilis + Escherichia coli + Candida glabrata | 1 (3.2%) |
| Rothia + Candida albicans | 1 (3.2%) |
| Staphylococcus devriesei/haemolyticus + Candida parapsilosis | 1 (3.2%) |
| Characteristic | n | Monomicrobial SAB (n = 541) | Polymicrobial SAB (n = 31) | p-Value |
|---|---|---|---|---|
| Age, years | 572 | 66.8 (54.4–78.5) | 65.5 (54.9–77.7) | 0.877 1 |
| Sex: Female | 572 | 214 (39.6%) | 13 (41.9%) | 0.792 2 |
| Diabetes Mellitus | 572 | 249 (46.0%) | 9 (29.0%) | 0.064 2 |
| Liver Disease | 572 | 156 (28.8%) | 14 (45.2%) | 0.053 2 |
| Chronic Kidney Disease | 572 | 0.789 2 | ||
| No | 322 (59.5%) | 18 (58.1%) | ||
| Yes, without HD | 168 (31.1%) | 11 (35.5%) | ||
| Yes, with HD | 51 (9.4%) | 2 (6.5%) | ||
| Charlson Comorbidity Index | 572 | 6.0 (3.0–9.0) | 8.0 (2.5–10.5) | 0.265 1 |
| Source of SAB | 572 | |||
| SSTI | 203 (37.5%) | 9 (29.0%) | 0.341 2 | |
| CRBSI | 67 (12.4%) | 9 (29.0%) | 0.008 2 | |
| CAUTI | 43 (7.9%) | 7 (22.6%) | 0.005 2 | |
| Unknown | 108 (20.0%) | 7 (22.6%) | 0.724 2 | |
| Pneumonia | 70 (12.9%) | 1 (3.2%) | 0.111 2 | |
| Septic Arthritis | 52 (9.6%) | 1 (3.2%) | 0.233 2 | |
| Other | 86 (15.9%) | 0 (0.0%) | 0.016 2 | |
| Site of Infection Onset | 570 | 0.027 2 | ||
| Nosocomial | 57 (10.6%) | 5 (16.1%) | ||
| Healthcare Associated | 265 (49.2%) | 21 (67.7%) | ||
| Community Acquired | 217 (40.3%) | 5 (16.1%) | ||
| Type of SAB: MRSA | 560 | 232 (43.8%) | 10 (33.3%) | 0.261 2 |
| ICU Admission | 571 | 144 (26.7%) | 9 (29.0%) | 0.772 2 |
| ID Consult | 571 | 424 (78.5%) | 28 (90.3%) | 0.116 2 |
| Hospitalization | 572 | 532 (98.3%) | 31 (100.0%) | 1.000 3 |
| TTE Obtained | 569 | 178 (33.1%) | 16 (51.6%) | 0.034 2 |
| TEE Obtained | 567 | 257 (47.9%) | 7 (22.6%) | 0.006 2 |
| n | Monomicrobial SAB (n = 541) | Polymicrobial SAB (n = 31) | p Value | |
|---|---|---|---|---|
| Complication | ||||
| Complicated Bacteremia | 571 | 207 (38.3%) | 9 (29.0%) | 0.299 1 |
| Infective Endocarditis | 569 | 39 (7.2%) | 2 (6.5%) | 0.867 1 |
| Vertebral Osteomyelitis | 571 | 30 (5.6%) | 1 (3.2%) | 0.578 1 |
| Non-vertebral Osteomyelitis | 571 | 40 (7.4%) | 4 (12.9%) | 0.264 1 |
| Septic Arthritis | 570 | 47 (8.7%) | 1 (3.2%) | 0.284 1 |
| Psoas Abscess | 571 | 4 (0.7%) | 0 (0.0%) | 1.000 2 |
| Splenic Abscess | 571 | 3 (0.6%) | 0 (0.0%) | 1.000 2 |
| Renal Abscess | 571 | 2 (0.4%) | 0 (0.0%) | 1.000 2 |
| Deep Seated Abscess | 571 | 49 (9.1%) | 0 (0.0%) | 0.079 1 |
| Pneumonitis | 571 | 30 (5.6%) | 0 (0.0%) | 0.178 1 |
| Cerebral Abscess | 571 | 5 (0.9%) | 0 (0.0%) | 1.000 2 |
| Meningitis | 571 | 2 (0.4%) | 0 (0.0%) | 1.000 2 |
| Stroke | 571 | 4 (0.7%) | 1 (3.2%) | 0.244 2 |
| Septic Emboli | 571 | 16 (3.0%) | 2 (6.5%) | 0.255 2 |
| Epidural Abscess | 571 | 9 (1.7%) | 0 (0.0%) | 1.000 2 |
| Altered Mental Status | 571 | 11 (2.0%) | 0 (0.0%) | 1.000 2 |
| Outcome | ||||
| In-hospital Mortality | 559 | 59 (11.2%) | 6 (19.4%) | 0.167 1 |
| Hospital Length of Stay, days | 559 | 10 (6–19) | 12 (7–37) | 0.254 3 |
| 6-month Mortality | 572 | 144 (26.7%) | 14 (45.2%) | 0.018 4 |
| 6-month Reinfection | 572 | 7 (1.3%) | 0 (0.0%) | 0.524 3 |
| Predictor | Comparison | HR (95% CI) | p |
|---|---|---|---|
| SAB group | Polymicrobial vs. Monomicrobial | 1.93 (0.96–3.87) | 0.064 |
| Age | 78.5 years vs. 54.4 years | 3.15 (2.33–4.27) | <0.001 |
| Sex | Female vs. Male | 1.39 (1.01–1.91) | 0.044 |
| Diabetes mellitus | Yes vs. No | 0.75 (0.52–1.07) | 0.115 |
| Liver disease | Yes vs. No | 1.06 (0.71–1.58) | 0.778 |
| Chronic kidney disease | 0.231 | ||
| Yes, without HD vs. No | 1.37 (0.92–2.03) | ||
| Yes, with HD vs. No | 1.59 (0.78–3.26) | ||
| Charlson Comorbidity Index | 10 vs. 3 | 1.27 (0.89–1.80) | 0.301 |
| Source of SAB | Unknown vs. Known | 1.75 (1.22–2.51) | 0.002 |
| Site of infection onset | 0.492 | ||
| HA vs. Nosocomial | 0.77 (0.47–1.26) | ||
| CA vs. Nosocomial | 0.73 (0.43–1.24) | ||
| Type of SAB | MRSA vs. MSSA | 0.86 (0.62–1.21) | 0.392 |
| ICU admission | Yes vs. No | 2.23 (1.59–3.13) | <0.001 |
| ID consult | Yes vs. No; phase = early 1 | 0.31 (0.19–0.50) | <0.001 |
| Yes vs. No; phase = late 1 | 0.94 (0.52–1.70) | 0.827 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hindy, J.-R.; Quintero-Martinez, J.A.; Lahr, B.D.; DeSimone, D.C.; Baddour, L.M. A Population-Based Evaluation of Polymicrobial Staphylococcus aureus Bacteremia. Pathogens 2022, 11, 1499. https://doi.org/10.3390/pathogens11121499
Hindy J-R, Quintero-Martinez JA, Lahr BD, DeSimone DC, Baddour LM. A Population-Based Evaluation of Polymicrobial Staphylococcus aureus Bacteremia. Pathogens. 2022; 11(12):1499. https://doi.org/10.3390/pathogens11121499
Chicago/Turabian StyleHindy, Joya-Rita, Juan A. Quintero-Martinez, Brian D. Lahr, Daniel C. DeSimone, and Larry M. Baddour. 2022. "A Population-Based Evaluation of Polymicrobial Staphylococcus aureus Bacteremia" Pathogens 11, no. 12: 1499. https://doi.org/10.3390/pathogens11121499
APA StyleHindy, J.-R., Quintero-Martinez, J. A., Lahr, B. D., DeSimone, D. C., & Baddour, L. M. (2022). A Population-Based Evaluation of Polymicrobial Staphylococcus aureus Bacteremia. Pathogens, 11(12), 1499. https://doi.org/10.3390/pathogens11121499






