Basophil Activation Test in the Diagnosis of Anisakis Allergy: An Observational Study from an Area of High Seafood Consumption in Italy
Abstract
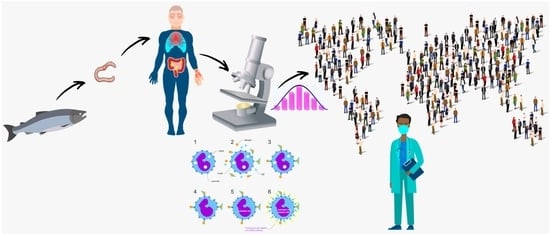
1. Introduction
2. Materials and Methods
2.1. Subjects in Study
2.2. Anisakis Protein Extraction and Species Identification
2.3. Current Diagnostic Approach
2.4. Basophil Activation Test
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Lehel, J.; Yaucat-Guendi, R.; Darnay, L.; Palotás, P.; Laczay, P. Possible food safety hazards of ready-to-eat raw fish containing product (sushi, sashimi). Crit. Rev. Food Sci. Nutr. 2021, 61, 867–888. [Google Scholar] [CrossRef] [PubMed]
- Parasites Anisakiasis. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/parasites/anisakiasis/faqs.html (accessed on 20 March 2023).
- Golden, O.; Caldeira, A.J.R.; Rangel, L.F.; Santos, M.J. Seafood safety and food-borne zoonoses from fish: Examining the risk of Anisakis in the Portuguese Population and Consumer Risk Perceptions of Fish Consumption. EFSA J. 2022, 20, e200409. [Google Scholar] [CrossRef] [PubMed]
- European Food Safety Authority (EFSA). Scientific Opinion on risk assessment of parasites in fishery products, EFSA Panel on Biological Hazards (BIOHAZ). EFSA J. 2010, 8, 1543–1634. [Google Scholar] [CrossRef]
- Mattiucci, S.; Cipriani, P.; Levsen, A.; Paoletti, M.; Nascetti, G. Molecular Epidemiology of Anisakis and Anisakiasis: An Ecological and Evolutionary Road Map. Adv. Parasitol. 2018, 99, 93–263. [Google Scholar] [CrossRef]
- Costa, A.; Cammilleri, G.; Graci, S.; Buscemi, M.D.; Vazzana, M.; Principato, D.; Giangrosso, G.; Ferrantelli, V. Survey on the presence of A. simplex s.s. and A. pegreffii hybrid forms in Central-Western Mediterranean Sea. Parasitol. Int. 2016, 65, 696–701. [Google Scholar] [CrossRef]
- Pravettoni, V.; Primavesi, L.; Piantanida, M. Anisakis simplex: Current knowledge. Eur. Ann. Allergy Clin. Immunol. 2012, 44, 150–156. [Google Scholar]
- AAITO-IFIACI Anisakis Consortium. Anisakis hypersensitivity in Italy: Prevalence and clinical features: A multicenter study. Allergy 2011, 66, 1563–1569. [Google Scholar] [CrossRef]
- Sakanari, J.A.; Mckerrow, J.H. Anisakiasis. Clin. Microbiol. Rev. 1989, 2, 278–284. [Google Scholar] [CrossRef]
- Mattiucci, S.; Paoletti, M.; Colantoni, A.; Carbone, A.; Gaeta, R.; Proietti, A.; Frattaroli, S.; Fazii, P.; Bruschi, F.; Nascetti, G. Invasive anisakiasis by the parasite Anisakis pegreffii (Nematoda: Anisakidae): Diagnosis by Real-Time PCR hydrolysis probe system and Immunoblotting assay. BMC Infect. Dis. 2017, 17, 530. [Google Scholar] [CrossRef]
- Mattiucci, S.; Colantoni, A.; Crisafi, B.; Mori-Ubaldini, F.; Caponi, L.; Fazii, P.; Nascetti, G.; Bruschi, F. IgE sensitization to Anisakis pegreffii in Italy: Comparison of two methods for the diagnosis of allergic anisakiasis. Parasite Immunol. 2017, 39, 1–10. [Google Scholar] [CrossRef]
- Baird, F.J.; Gasser, R.B.; Jabbar, A.; Lopata, A.L. Foodborne anisakiasis and allergy. Mol. Cell. Probes 2014, 28, 167–174. [Google Scholar] [CrossRef]
- Johansson, E.; Aponno, M.; Lundberg, M.; Van Hage-Hamsten, M. Allergenic cross-reactivity between the nematode Anisakis simplex and the dust mites Acarus siro, Lepidoglyphus destructor, Tyrophagus putrescentiae, and Dermatophagoides pteronyssinus. Allergy 2001, 56, 660–666. [Google Scholar] [CrossRef]
- Lorenzo, S.; Iglesias, R.; Paniagua, E.; Ansotegui, I.; Alonso, J.M.; Ubeira, F.M. Natural antibodies to nematode biotinyl-enzymes in human sera. Med. Microbiol. Immunol. 2001, 189, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Petithory, J.C. New data on Anisakiasis. Bull. Acad. Natl. Med. 2007, 191, 53–65. [Google Scholar] [PubMed]
- Pasolini, B.; Alessi, E.; De Medici, D. Rapporto ISTISAN 05/24. In Proceedings of the Workshop di Aggiornamento su Problematiche Emergenti nel Settore dei Prodotti Ittici, Rome, Italy, 24–25 May 2004. [Google Scholar]
- Asturias, J.A.; Gómez-Bayón, N.; Arilla, M.C.; Martínez, A.; Palacios, R.; Sánchez-Gascón, F.; Martínez, J. Molecular characterization of American cockroach tropomyosin (Periplaneta americana allergen 7), a cross-reactive allergen. J. Immunol. 1999, 162, 4342–4348. [Google Scholar] [CrossRef] [PubMed]
- Caballero, M.L.; Asero, R.; Antonicelli, L.; Kamberi, E.; Colangelo, C.; Fazii, P.; de Burgos, C.; Rodriguez-Perez, R. Anisakis allergy component-resolved diagnosis: Clinical and immunologic differences between patients from Italy and Spain. Int. Arch. Allergy Immunol. 2013, 162, 39–44. [Google Scholar] [CrossRef]
- Reese, G.; Ayuso, R.; Lehrer, S.B. Tropomyosin: An invertebrate panallergen. Int. Arch. Allergy Immunol. 1999, 119, 247–258. [Google Scholar] [CrossRef]
- Del Pozo, M.D.; Audícana, M.; Diez, J.M.; Munoz, D.; Ansotegui, I.J.; Fernández, E.; García, M.; Etxenagusia, M.; Moneo, I.; Fernández de Corres, L. Anisakis simplex, a relevant etiologic factor in acute urticarial. Allergy 1997, 52, 576–579. [Google Scholar] [CrossRef]
- Ventura, M.T.; Napolitano, S.; Menga, R.; Cecere, R.; Asero, R. Anisakis simplex hypersensitivity is associated with chronic urticaria in endemic areas. Int. Arch. Allergy Immunol. 2013, 160, 297–300. [Google Scholar] [CrossRef]
- Frezzolini, A.; Cadoni, S.; De Pita, O. Usefulness of the CD63 basophil activation test in detecting Anisakis hypersensitivity in patients with chronic urticaria: Diagnosis and follow-up. Clin. Exp. Dermatol. 2010, 35, 765–770. [Google Scholar] [CrossRef]
- Del Rey Moreno, A.; Valero, A.; Mayorga, C.; Gómez, B.; Torres, M.J.; Hernández, J.; Ortiz, M.; Lozano Maldonado, J. Sensitization to Anisakis simplex s.l. in a healthy population. Acta Trop. 2006, 97, 265–269. [Google Scholar] [CrossRef]
- del Pozo, M.D.; Moneo, I.; de Corres, L.F.; Audicana, M.T.; Muñoz, D.; Fernandez, E.; Navarro, J.A.; García, M. Laboratory determination in Anisakis simplex allergy. J. Allergy Clin. Immunol. 1996, 97, 977–984. [Google Scholar] [CrossRef]
- García, M.; Moneo, I.; Audicana, M.T.; del Pozo, M.D.; Muñoz, D.; Fernández, E.; Díez, J.; Etxenagusia, M.A.; Ansotegui, I.J.; Fernández de Corres, L. The use of IgE immunoblotting as a diagnostic tool in Anisakis simplex allergy. J. Allergy Clin. Immunol. 1997, 99, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo, S.; Iglesias, R.; Leiro, J.; Ubeira, F.M.; Ansotegui, I.; García, M.; Fernández de Corres, L. Usefulness currently available methods for the diagnosis of Anisakis simplex allergy. Allergy 2000, 55, 627–633. [Google Scholar] [CrossRef]
- Sastre, J.; Lluch-Bernal, M.; Quirce, S.; Arrieta, I.; Lahoz, C.; Del Amo, A.; Fernández-Caldas, E.; Marañón, F. A double blind, placebo-controlled oral challenge study with lyophilized larvae and antigen of the fish parasite, Anisakis simplex. Allergy 2000, 55, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Lluch-Bernal, M.; Sastre, J.; Fernández-Caldas, E.; Marañon, F.; Cuesta-Herranz, J.; De las Heras, M.; Quirce, S.; Novalbos, A. Conjunctival provocation tests in the diagnosis of Anisakis simplex hypersensitivity. J. Investig. Allergol. Clin. Immunol. 2002, 12, 21–24. [Google Scholar] [PubMed]
- Brusca, I.; Graci, S.; Barrale, M.; Cammilleri, G.; Zarcone, M.; Onida, R.; Costa, A.; Ferrantelli, V.; Buscemi, M.D.; Uasuf, C.G.; et al. Use of a comprehensive diagnostic algorithm for Anisakis allergy in a high seroprevalence Mediterranean setting. Eur. Ann. Allergy Clin. Immunol. 2020, 52, 131–141. [Google Scholar] [CrossRef]
- D’Amelio, S.; Mathiopoulos, K.D.; Santos, C.P.; Pugachev, O.N.; Webb, S.C.; Picanço, M.; Paggi, L. Genetic markers in ribosomal DNA for the identification of members of the genus Anisakis (Nematoda: Ascaridoidea) defined by polymerase-chain-reactionbased restriction fragment length polymorphism. Int. J. Parasitol. 2000, 30, 223–226. [Google Scholar] [CrossRef]
- Blaker, H. Confidence curves and improved exact confidence intervals for discrete distributions. Can. J. Stat. 2000, 28, 783–798. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef] [PubMed]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Audicana, M.T.; Ansotegui, I.J.; de Corres, L.F.; Kennedy, M.W. Anisakis simplex: Dangerous-dead and alive? Trends Parasitol. 2002, 18, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Bao, M.; Pierce, G.J.; Pascual, S.; González-Muñoz, M.; Mattiucci, S.; Mladineo, I.; Cipriani, P.; Bušelić, I.; Strachan, N.J. Assessing the risk of an emerging zoonosis of worldwide concern: Anisakiasis. Sci. Rep. 2017, 7, 43699. [Google Scholar] [CrossRef]
- Morishima, R.; Motojima, S.; Tsuneishi, D.; Kimura, T.; Nakashita, T.; Fudouji, J.; Ichikawa, S.; Ito, H.; Nishino, H. Anisakis is a major cause of anaphylaxis in seaside areas: An epidemiological study in Japan. Allergy 2020, 75, 441–444. [Google Scholar] [CrossRef]
- Abattouy, N.; Valero, A.; Martín-Sánchez, J.; Peñalver, M.C.; Lozano, J. Sensitization to Anisakis simplex species in the population of northern Morocco. J. Investig. Allergol. Clin. Immunol. 2012, 22, 514–519. [Google Scholar]
- Mladineo, I.; Poljak, V.; Martínez-Sernández, V.; Ubeira, F.M. Anti-Anisakis IgE seroprevalence in the healthy Croatian coastal population and associated risk factors. PLoS Negl. Trop. Dis. 2014, 8, e2673. [Google Scholar] [CrossRef]
- Mazzucco, W.; Lacca, G.; Cusimano, R.; Provenzani, A.; Costa, A.; Di Noto, A.M.; Massenti, M.F.; Leto-Barone, M.S.; Lorenzo, G.D.; Vitale, F. Prevalence of Sensitization to Anisakis simplex Among Professionally Exposed Populations in Sicily. Arch. Environ. Occup. Health 2012, 67, 91–97. [Google Scholar] [CrossRef]
- Baird, F.J.; Su, X.; Aibinu, I.; Nolan, M.J.; Sugiyama, H.; Otranto, D.; Lopata, A.L.; Cantacessi, C. The Anisakis transcriptome provides a resource for fundamental and applied studies on allergy-causing parasites. PLoS Negl. Trop. Dis. 2016, 10, e0004845. [Google Scholar] [CrossRef]
- Cavallero, S.; Lombardo, F.; Xiaopei, S.; Salvemini, M.; Cantacess, C.; D’Amelio, S. Tissue-specific transcriptomes of Anisakis simplex (sensu stricto) and Anisakis pegreffii reveal potential molecular mechanisms involved in pathogenicity. Parasit. Vectors 2018, 11, 31. [Google Scholar] [CrossRef]
- Kochanowski, M.; Dąbrowska, J.; Różycki, M.; Sroka, J.; Karamon, J.; Bełcik, A.; Korpysa-Dzirba, W.; Cencek, T. Proteomic profiling and in silico characterization of the secretome of Anisakis simplex sensu stricto L3 Larvae. Pathogens 2022, 11, 246. [Google Scholar] [CrossRef] [PubMed]
- Boysen, A.T.; Whitehead, B.; Stensballe, A.; Carnerup, A.; Nylander, T.; Nejsum, P. Fluorescent labelling of helminth extracellular vesicles using an in vivo whole organism approach. Biomedicines 2020, 8, 213. [Google Scholar] [CrossRef] [PubMed]
- Fæste, C.K.; Jonscher, K.R.; Dooper, M.M.; Egge-Jacobsen, W.; Moen, A.; Daschner, A.; Egaas, E.; Christians, U. Characterisation of potential novel allergens in the fish parasite Anisakis simplex. EuPA Open Proteom. 2014, 4, 140–155. [Google Scholar] [CrossRef]
- Aibinu, I.; Smooker, P.M.; Lopata, A.L. Anisakis nematodes in fish and shellfish–from infection toallergies. Int. J. Parasitol. Parasites Wildl. 2019, 9, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Palomba, M.; Libro, P.; Di Martino, J.; Rughetti, A.; Santoro, M.; Mattiucci, S.; Castrignanò, T. De novo transcriptome assembly and annotation of the third stage larvae of the zoonotic parasite Anisakis pegreffii. BMC Res. Notes 2022, 15, 223. [Google Scholar] [CrossRef]
- Moneo, I.; Carballeda-Sangiao, N.; González-Muñoz, M. New Perspectives on the Diagnosis of Allergy to Anisakis spp. Curr. Allergy Asthma Rep. 2017, 17, 27. [Google Scholar] [CrossRef]
- Zuberbier, T.; Aberer, W.; Asero, R.; Abdul Latiff, A.H.; Baker, D.; Ballmer-Weber, B.; Bernstein, J.A.; Bindslev-Jensen, C.; Brzoza, Z.; Buense Bedrikow, R.; et al. The EAACI/GA²LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy 2018, 73, 1393–1414. [Google Scholar] [CrossRef]
- Gonzalez-Muñoz, M.; Luque, R.; Nauwelaers, F.; Moneo, I. Detection of Anisakis simplex-induced basophil activation by flow cytometry. Cytom. B Clin. Cytom. 2005, 68, 31–36. [Google Scholar] [CrossRef]
- Gamboa, P.M.; Asturias, J.; Martínez, R.; Antépara, I.; Jáuregui, I.; Urrutia, I.; Fernández, J.; Sanz, M.L. Diagnostic utility of components in allergy to Anisakis simplex. J. Investig. Allergol. Clin. Immunol. 2012, 22, 13–19. [Google Scholar]
- Daschner, A.; De Frutos, C.; Valls, A.; Vega, F. Anisakis simplex sensitization-associated urticaria: Short-lived immediate type or prolonged acute urticarial. Arch. Dermatol. Res. 2010, 302, 625–694. [Google Scholar] [CrossRef]
- Daschner, A.; Rodero, M.; DEFrutos, C.; Valls, A.; Vega, F.; Blanco, C.; Cuéllar, C. Different serum cytokine levels in chronic vs. acute Anisakis simplex sensitization-associated urticarial. Parasite Immunol. 2011, 33, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Daschner, A.; Fernández-Fígares, V.; Valls, A.; de Frutos, C.; Rodero, M.; Ubeira, F.M.; Cuéllar, C. Different fish-eating habits and cytokine production in chronic urticaria with and without sensitization against the fish-parasite Anisakis simplex. Allergol. Int. 2013, 62, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; An, S.; Kim, J.E.; Choi, G.S.; Ye, Y.M.; Park, H.S. Beef-induced anaphylaxis confirmed by the basophil activation test. Allergy Asthma Immunol. Res. 2010, 2, 206–208. [Google Scholar] [CrossRef] [PubMed]
- Daschner, F.; de la Osada, V.; Pascual, C.Y. Allergy and parasites reevaluated: Wide-scale induction of chronic urticaria by the ubiquitous fish-nematode Anisakis simplex in an endemic region. Allergol. Immunopathol. 2005, 33, 31–37. [Google Scholar] [CrossRef]
- Tramuto, F.; Mazzucco, W.; Maida, C.M.; Affronti, A.; Affronti, M.; Montalto, G.; Vitale, F. Serological pattern of Hepatitis B, C, and HIV infections among immigrants in Sicily: Epidemiological aspects and implication on public health. J. Community Health. 2012, 37, 547–553. [Google Scholar] [CrossRef]
- Mazzucco, W.; Raia, D.D.; Marotta, C.; Costa, A.; Ferrantelli, V.; Vitale, F.; Casuccio, A. Anisakis sensitization in different population groups and public health impact: A systematic review. PLoS ONE 2018, 13, e0203671. [Google Scholar] [CrossRef]


| Gender | Total (%) n = 53 | ||
|---|---|---|---|
| Male (%) n = 22 | Female (%) n = 31 | ||
| Age | |||
| 0–30 | 6 (27.3%) | 5 (16.1%) | 11 (20.8%) |
| 31–60 | 5 (22.7%) | 15 (48.4%) | 20 (37.7%) |
| >60 | 11 (50.0%) | 11 (35.5%) | 22 (41.5%) |
| Simptoms | |||
| Idiopatic anaphilaxis | 0 (0%) | 1 (3.2%) | 1 (1.9%) |
| Anaphilaxis after fish ingestion | 1 (4.5%) | 1 (3.2%) | 2 (3.8%) |
| Fainting after fish ingestion | 0 (0%) | 1 (3.2%) | 1 (1.9%) |
| Urticaria/angioedema after fish ingestion | 6 (27.3%) | 7 (22.6%) | 13 (24.5%) |
| Urticaria/angioedema after fish and shellfish ingestion | 5 (22.7%) | 3 (9.7%) | 8 (15.1%) |
| Urticaria/angioedema after shellfish ingestion | 0 (0%) | 2 (6.5%) | 2 (3.8%) |
| Urticaria | 2 (9.1%) | 0 (0%) | 2 (3.8%) |
| Urticaria enhanced by shellfish ingestion | 8 (36.4%) | 16 (51.6%) | 24 (45.3%) |
| IgE (kIU/L) | [ALL] (%) n = 53 | Chronic Urticarial (%) n = 27 | Anisakis Allergy (%) n = 26 | OR [95% CI] | p-Value |
|---|---|---|---|---|---|
| Anisakis (p4): | |||||
| <0.35 | 12 (22.6%) | 10 (37.0%) | 2 (7.69%) | Ref. | Ref. |
| ≥0.35 | 41 (77.4%) | 17 (63.0%) | 24 (92.3%) | 6.81 [1.37;48.41] | 0.019 |
| Ascaris (p1): | |||||
| <0.35 | 28 (52.8%) | 17 (63.0%) | 11 (42.3%) | Ref. | Ref. |
| ≥0.35 | 25 (47.2%) | 10 (37.0%) | 15 (57.7%) | 2.28 [0.68;7.73] | 0.173 |
| Tropomyosin (pena1): | |||||
| <0.35 | 46 (86.8%) | 25 (92.6%) | 21 (80.8%) | Ref. | Ref. |
| ≥0.35 | 7 (13.2%) | 2 (7.41%) | 5 (19.2%) | 2.92 [0.51;22.62] | 0.239 |
| [ALL] Mean ± SD (n = 53) | Chronic Urticaria Mean ± SD (n = 27) | Anisakis Allergy Mean ± SD (n = 26) | p-Value | |
|---|---|---|---|---|
| Anisakis (p4) s-IgE ^ | 7.62 ± 19.2 | 2.28 ± 4.50 | 13.2 ± 26.1 | 0.046 |
| Ascaris (p1) s-IgE ^ | 1.16 ± 1.89 | 0.42 ± 0.54 | 1.92 ± 2.43 | 0.005 |
| Tropomiosin s-IgE ^ (Pena1) | 3.41 ± 14.9 | 0.16 ± 0.68 | 6.79 ± 20.9 | 0.118 |
| BAT (%) * | 23.7 ± 29.0 | 2.95 ± 3.45 | 45.2 ± 28.0 | <0.001 |
| Concentrations | Diagnosis | A. pegreffi (A.P.e.) Mean ± SD | A. simplex (A.S.e.) Mean ± SD | Delta (95%CI) | p-Value |
|---|---|---|---|---|---|
| 4.5 ng/mL | Chronic urticaria | 1.46 ± 2.35 | 1.73 ± 2.37 | −0.27 (−1.015; +0.478) | 0.4907 |
| Anisakis allergy | 31.13 ±27.80 | 17.39 ± 22.04 | +12.79 (+3.099; +22.489) | 0.0110 | |
| 22.5 ng/mL | Chronic urticaria | 1.66 ± 2.26 | 1.72 ± 2.85 | −0.06 (−0.652; +0.520) | 0.8406 |
| Anisakis allergy | 45.06 ± 32.48 | 28.88 ± 26.98 | +16.18 (+7.454; +24.890) | 0.0008 | |
| 112.5 ng/mL | Chronic urticaria | 1.94 ± 2.58 | 2.01 ± 2.97 | −0.065 (−0.954; +0.823) | 0.8883 |
| Anisakis allergy | 45.14 ± 31.20 | 38.19 ± 30.44 | +6.95 (−0.485; +14.394) | 0.0656 |
| Test | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | Accuracy | Positive Likehood Ratio | Negative Likehood Ratio |
|---|---|---|---|---|---|---|---|
| BAT > 15% Activated Basophils | 84.62% | 100.00% | 100.00% | 87.10% | 92.45% | Infinite | 0.1538 |
| Anisakis (p4) | 92.31% | 37.04% | 58.54% | 83.33% | 64.15% | 1.4662 | 0.2076 |
| Ascaris (p1) | 57.69% | 62.96% | 60.00% | 60.71% | 60.37% | 1.5575 | 0.672 |
| ratio p4/p1 > 4.2 | 53.85% | 44.00% | 50.00% | 47.83% | 49.02% | 0.9616 | 1.0489 |
| Tropomiosina (pena1) | 19.23% | 92.59% | 71.43% | 54.35% | 56.60% | 2.5951 | 0.8723 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brusca, I.; Barrale, M.; Zarcone, M.; Fruscione, S.; Onida, R.; De Bella, D.D.; Alba, D.; Belluzzo, M.; Uasuf, C.G.; Cammilleri, G.; et al. Basophil Activation Test in the Diagnosis of Anisakis Allergy: An Observational Study from an Area of High Seafood Consumption in Italy. Pathogens 2023, 12, 777. https://doi.org/10.3390/pathogens12060777
Brusca I, Barrale M, Zarcone M, Fruscione S, Onida R, De Bella DD, Alba D, Belluzzo M, Uasuf CG, Cammilleri G, et al. Basophil Activation Test in the Diagnosis of Anisakis Allergy: An Observational Study from an Area of High Seafood Consumption in Italy. Pathogens. 2023; 12(6):777. https://doi.org/10.3390/pathogens12060777
Chicago/Turabian StyleBrusca, Ignazio, Maria Barrale, Maurizio Zarcone, Santo Fruscione, Rosa Onida, Daniele Domenico De Bella, Davide Alba, Miriam Belluzzo, Carina Gabriela Uasuf, Gaetano Cammilleri, and et al. 2023. "Basophil Activation Test in the Diagnosis of Anisakis Allergy: An Observational Study from an Area of High Seafood Consumption in Italy" Pathogens 12, no. 6: 777. https://doi.org/10.3390/pathogens12060777
APA StyleBrusca, I., Barrale, M., Zarcone, M., Fruscione, S., Onida, R., De Bella, D. D., Alba, D., Belluzzo, M., Uasuf, C. G., Cammilleri, G., Costa, A., Ferrantelli, V., Savatteri, A., Cannizzaro, E., Calamusa, G., Lacca, G., Maida, C. M., Pipitone, S., D’Atria, A., ... Mazzucco, W. (2023). Basophil Activation Test in the Diagnosis of Anisakis Allergy: An Observational Study from an Area of High Seafood Consumption in Italy. Pathogens, 12(6), 777. https://doi.org/10.3390/pathogens12060777