Missed Opportunities for HIV Diagnosis and Their Clinical Repercussions in the Portuguese Population—A Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Setting, Participants, and Definitions
2.2. Outcomes and Variables
2.3. Statistical Analysis
3. Results
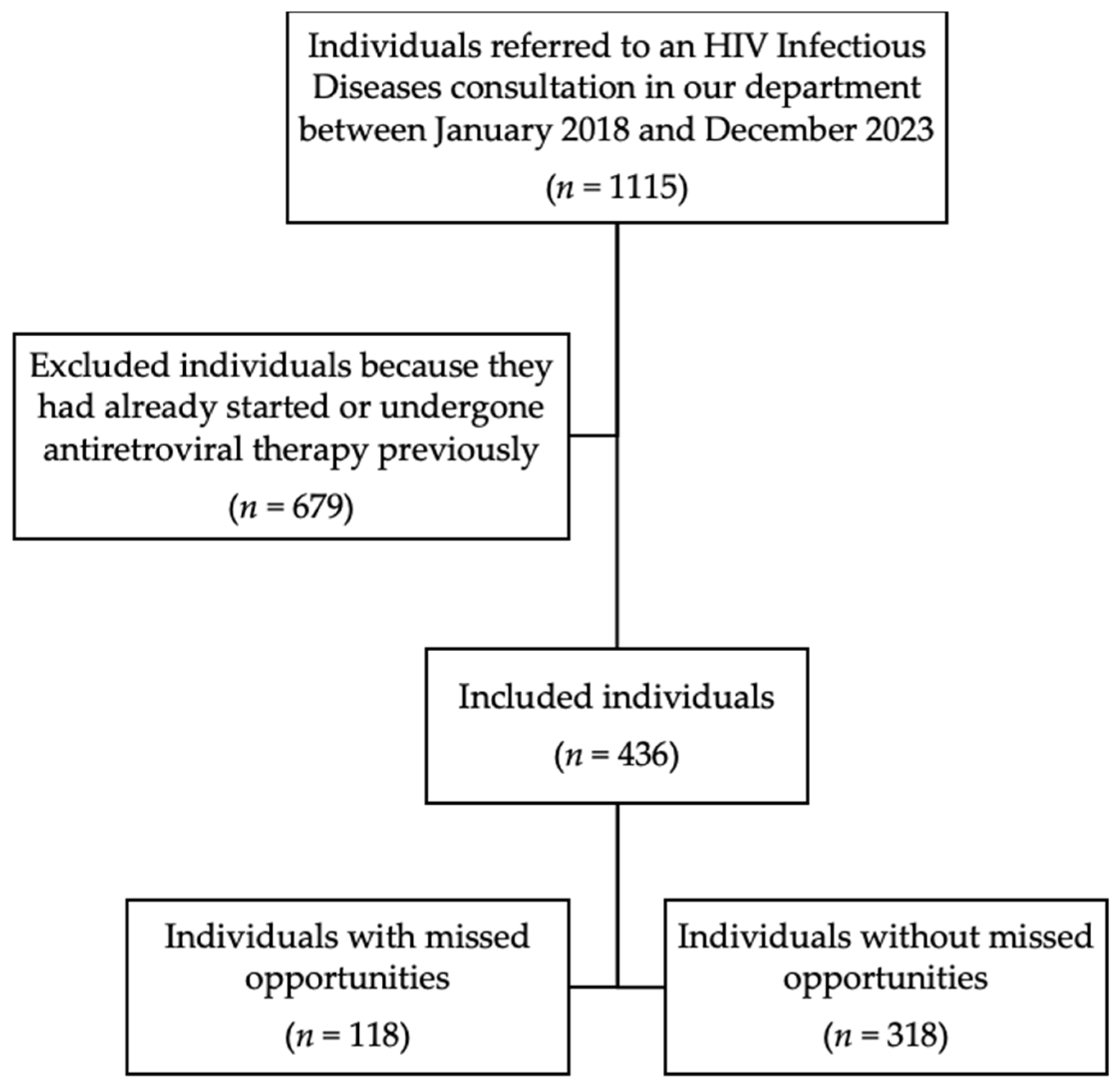
3.1. Study Population
3.2. Missed Opportunities
3.3. AIDS-Defining Conditions
3.4. Primary and Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Centre for Disease Prevention and Control. HIV/AIDS Surveillance in Europe 2023–2022 Data; European Centre for Disease Prevention and Control: Solna, Sweden, 2023; ISBN 9789294986702. [Google Scholar]
- van Sighem, A.; Pharris, A.; Quinten, C.; Noori, T.; Amato-Gauci, A.J. Reduction in Undiagnosed HIV Infection in the European Union/European Economic Area, 2012 to 2016. Eurosurveillance 2017, 22, 17–00771. [Google Scholar] [CrossRef] [PubMed]
- Late Presentation Working Groups in EuroSIDA and COHERE Estimating the Burden of HIV Late Presentation and Its Attributable Morbidity and Mortality across Europe 2010–2016. BMC Infect. Dis. 2020, 20, 728. [CrossRef]
- Mocroft, A.; Lundgren, J.D.; Sabin, M.L.; Monforte, A.D.A.; Brockmeyer, N.; Casabona, J.; Castagna, A.; Costagliola, D.; Dabis, F.; De Wit, S.; et al. Risk Factors and Outcomes for Late Presentation for HIV-Positive Persons in Europe: Results from the Collaboration of Observational HIV Epidemiological Research Europe Study (COHERE). PLoS Med. 2013, 10, e1001510. [Google Scholar] [CrossRef] [PubMed]
- Horsley Downie, J.; Pegler, M.; Widdrington, J.; Price, D.; Premchand, N.; Chadwick, D. Late HIV Diagnosis and Missed Opportunities for Testing: Piloting a Standardised, Multi-Source Review Process. Int. J. STD AIDS 2020, 31, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Nanditha, N.G.A.; St-Jean, M.; Tafessu, H.; Guillemi, S.A.; Hull, M.W.; Lu, M.; Henry, B.; Barrios, R.; Montaner, J.S.G.; Lima, V.D. Missed Opportunities for Earlier Diagnosis of HIV in British Columbia, Canada: A Retrospective Cohort Study. PLoS ONE 2019, 14, e0214012. [Google Scholar] [CrossRef] [PubMed]
- Downing, A.; Garcia-Diaz, J.B. Missed Opportunities for HIV Diagnosis. J. Int. Assoc. Provid. AIDS Care 2017, 16, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Brawley, D.; MacConnachie, A.; Nandwani, R.; Bell, D.; Fargie, F.; Fox, R.; Peters, E.; Seaton, R.; Winter, A. Missed Opportunities for HIV Diagnosis: A Three-Year Audit in the West of Scotland. Scott. Med. J. 2013, 58, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Tominski, D.; Katchanov, J.; Driesch, D.; Daley, M.; Liedtke, A.; Schneider, A.; Slevogt, H.; Arastéh, K.; Stocker, H. The Late-Presenting HIV-Infected Patient 30 Years after the Introduction of HIV Testing: Spectrum of Opportunistic Diseases and Missed Opportunities for Early Diagnosis. HIV Med. 2017, 18, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, M.; Ballouz, T.; Lahoud, C.; Adnan, J.; Habib, P.A.; Saab, R.; Farhat, H.; Hussein, M.E.; Rizk, N. Late Presentations and Missed Opportunities among Newly Diagnosed HIV Patients Presenting to a Specialty Clinic in Lebanon. Sci. Rep. 2024, 14, 8296. [Google Scholar] [CrossRef] [PubMed]
- Rüütel, K.; Lemsalu, L.; Lätt, S.; Epštein, J. Missed Opportunities for HIV Testing in People Diagnosed with HIV, Estonia, 2014 to 2015. Eurosurveillance 2019, 24, 1800382. [Google Scholar] [CrossRef] [PubMed]
- Levy, I.; Maor, Y.; Mahroum, N.; Olmer, L.; Wieder, A.; Litchevski, V.; Mor, O.; Rahav, G. Missed Opportunities for Earlier Diagnosis of HIV in Patients Who Presented with Advanced HIV Disease: A Retrospective Cohort Study. BMJ Open 2016, 6, e012721. [Google Scholar] [CrossRef] [PubMed]
- Gallego-Márquez, N.; Iniesta, C. Identificando Objetivos Fast-Track: Oportunidades Perdidas En El Diagnóstico de VIH En La Comunidad de Madrid. Enferm. Infecc. Microbiol. Clin. 2022, 40, 138–141. [Google Scholar] [CrossRef] [PubMed]
- Direção-Geral da Saúde. Norma No 058/2011—Diagnóstico e Rastreio Laboratorial Da Infeção Pelo Vírus Da Imunodeficiência Humana (VIH); Direção-Geral da Saúde: Lisbon, Portugal, 2014; ISBN 9789726752127. [Google Scholar]
- Direção-Geral da Saúde; Instituto Nacional de Saúde Doutor Ricardo Jorge. Infeção Por VIH Em Portugal; Direção-Geral da Saúde: Lisbon, Portugal, 2023; ISBN 9789898794970. [Google Scholar]
- Joint United Nations Programme on HIV and AIDS. Data Book UNAIDS 2023; Joint United Nations Programme on HIV and AIDS: Geneva, Switzerland, 2023. [Google Scholar]
- Gill, M.; Powell, M.; Vu, Q.; Krentz, H. Economic Impact on Direct Healthcare Costs of Missing Opportunities for Diagnosing HIV within Healthcare Settings. HIV Med. 2021, 22, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Croxford, S.; Kitching, A.; Desai, S.; Kall, M.; Edelstein, M.; Skingsley, A.; Burns, F.; Copas, A.; Brown, A.E.; Sullivan, A.K.; et al. Mortality and Causes of Death in People Diagnosed with HIV in the Era of Highly Active Antiretroviral Therapy Compared with the General Population: An Analysis of a National Observational Cohort. Lancet Public Health 2017, 2, e35–e46. [Google Scholar] [CrossRef] [PubMed]
- Marih, L.; Sawras, V.; Pavie, J.; Sodqi, M.; Malmoussi, M.; Tassi, N.; Bensghir, R.; Nani, S.; Lahsen, A.O.; Laureillard, D.; et al. Missed Opportunities for HIV Testing in Patients Newly Diagnosed with HIV in Morocco. BMC Infect. Dis. 2021, 21, 48. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, A.K.; Raben, D.; Reekie, J.; Rayment, M.; Mocroft, A.; Esser, S.; Leon, A.; Begovac, J.; Brinkman, K.; Zangerle, R.; et al. Feasibility and Effectiveness of Indicator Condition-Guided Testing for HIV: Results from HIDES I (HIV Indicator Diseases across Europe Study). PLoS ONE 2013, 8, e52845. [Google Scholar] [CrossRef] [PubMed]
- Raben, D.; Sullivan, A.K.; Mocroft, A.; Kutsyna, G.; Hadžiosmanović, V.; Vassilenko, A.; Chkhartisvili, N.; Mitsura, V.; Pedersen, C.; Anderson, J.; et al. Improving the Evidence for Indicator Condition Guided HIV Testing in Europe: Results from the HIDES II Study—2012–2015. PLoS ONE 2019, 14, e0220108. [Google Scholar] [CrossRef] [PubMed]
- Marks, G.; Crepaz, N.; Janssen, R.S. Estimating Sexual Transmission of HIV from Persons Aware and Unaware That They Are Infected with the Virus in the USA. AIDS 2006, 20, 1447–1450. [Google Scholar] [CrossRef] [PubMed]
| Epidemiological criteria | All adults up to 64 years old in opportunistic manner | |
| Sexual partners of individuals diagnosed with HIV infection | ||
| Men who have sex with men | ||
| Sexual partners of men who have sex with men | ||
| Individuals with history of drug use | ||
| Individuals originating from countries with high prevalence of HIV infection (> 1%) | ||
| Sexual partners of individuals originating from countries with high prevalence of HIV infection | ||
| Inmates | ||
| Nomad population | ||
| Homeless individuals | ||
| Sex workers | ||
| Individuals subjected to sexual violence | ||
| Clinical criteria | Any AIDS-defining condition | |
| Pneumological | Bacterial pneumonia | |
| Aspergillosis | ||
| Neurological | Aseptic meningitis/encephalitis | |
| Cerebral abscess | ||
| Space-occupying lesion of unknown cause | ||
| Guillain–Barré syndrome | ||
| Transverse myelitis | ||
| Peripheral neuropathy | ||
| Dementia | ||
| Leukoencephalopathy | ||
| Dermatological | Severe seborrheic dermatitis | |
| Severe psoriasis | ||
| Recurrent or multidermatomal herpes zoster | ||
| Gastroenterological | Oral candidiasis | |
| Chronic diarrhoea of unknown cause | ||
| Weight loss of unknown cause | ||
| Infection with Salmonella spp., Shigella spp. or Campylobacter spp. | ||
| Hepatitis B or C virus infection | ||
| Oncological | Anal intraepithelial neoplasia or dysplasia | |
| Lung neoplasm | ||
| Seminoma | ||
| Head and neck neoplasm | ||
| Hodgkin’s lymphoma | ||
| Castleman’s disease | ||
| Gynaecological | Vaginal intraepithelial neoplasia | |
| Grade 2 or higher cervical intraepithelial neoplasia | ||
| Haematological | Thrombocytopenia, leukopenia, lymphopenia | |
| Ophthalmological | Retinal diseases, including herpes viruses or Toxoplasma | |
| Any unexplained retinopathy | ||
| Ears, nose and throat | Lymphadenopathy of unknown cause | |
| Chronic parotitis | ||
| Lymphoepithelial parotid cysts | ||
| Others | Mononucleosis-like syndromes | |
| Fever of unknown cause | ||
| Any lymphadenopathy of unknown cause | ||
| Any sexually transmitted infection | ||
| Characteristic | Total (n = 436) | Without Missed Opportunities (n = 318) | With Missed Opportunities (n = 118) | p Value |
|---|---|---|---|---|
| Female—n (%) | 155 (35.6) | 101 (31.8) | 54 (45.8) | 0.007 |
| Age, years—median (IQR) | 38 (29–47) | 36 (29–45.3) | 42 (33–55) | <0.001 |
| Birthplace, by continent—n (%) | <0.001 | |||
| Europe | 199 (45.6) | 145 (45.6) | 54 (45.8) | |
| Africa | 139 (31.9) | 87 (27.4) | 52 (44.1) | |
| America | 97 (22.2) | 85 (26.7) | 12 (10.2) | |
| Asia | 1 (0.2) | 1 (0.3) | 0 (0.0) | |
| High-prevalence countries—n (%) | 91 (20.9) | 48 (15.1) | 43 (36.4) | <0.001 |
| Heterosexual transmission—n (%) | 220 (55.8) | 148 (50.9) | 72 (69.9) | <0.001 |
| Assigned general practitioner—n (%) | 207 (51.0) | 134 (46.2) | 73 (62.9) | 0.002 |
| Visits to the emergency department—median (IQR) | 0 (0–1) | 0 (0–1) | 1 (0–3) | <0.001 |
| HIV type 1—n (%) | 419 (96.1) | 308 (96.9) | 111 (94.1) | 0.182 |
| HIV viral load at diagnosis, log—median (IQR) | 4.8 (4.0–5.5) | 4.8 (4.0–5.4) | 5.0 (4.0–5.6) | 0.255 |
| HBV coinfection—n (%) | 19 (4.4) | 13 (4.1) | 6 (5.1) | 0.652 |
| HCV coinfection—n (%) | 11 (2.6) | 10 (3.2) | 1 (0.9) | 0.302 |
| Missed Opportunities for HIV Diagnosis | n (%) | ||
|---|---|---|---|
| Epidemiological criteria | Individuals originating from countries with high prevalence of HIV infection (>1%) | 40 (20.8) | |
| Individuals with history of drug use | 4 (2.1) | ||
| Men who have sex with men | 1 (0.5) | ||
| Individuals subjected to sexual violence | 1 (0.5) | ||
| Sexual partners of individuals diagnosed with HIV infection | 1 (0.5) | ||
| Clinical criteria | Pneumological | Bacterial pneumonia | 14 (7.3) |
| Neurological | Aseptic meningitis/encephalitis | 1 (0.5) | |
| Dermatological | Recurrent or multidermatomal herpes zoster | 6 (3.1) | |
| Severe psoriasis | 1 (0.5) | ||
| Gastroenterological | Weight loss of unknown cause | 17 (8.9) | |
| Oral candidiasis | 3 (1.6) | ||
| Chronic diarrhoea of unknown cause | 3 (1.6) | ||
| Gynaecological | Grade 2 or higher cervical intraepithelial neoplasia | 1 (0.5) | |
| Haematological | Thrombocytopenia, leukopenia, lymphopenia | 27 (14.1) | |
| Others | Mononucleosis-like syndromes | 33 (17.2) | |
| Fever of unknown cause | 1 (0.5) | ||
| Any lymphadenopathy of unknown cause | 8 (4.2) | ||
| Any sexually transmitted infection | 30 (15.6) | ||
| AIDS-Defining Conditions | n (%) |
|---|---|
| Candidiasis of the oesophagus | 13 (12.5) |
| Cryptococcosis, extrapulmonary | 2 (1.9) |
| Cryptosporidiosis, chronic intestinal (greater than one month’s duration) | 1 (1.0) |
| Cytomegalovirus disease (other than liver, spleen, or nodes) | 7 (6.7) |
| Encephalopathy, HIV-related | 6 (5.8) |
| Kaposi sarcoma | 5 (4.8) |
| Lymphoma, immunoblastic (or equivalent term) | 1 (1.0) |
| Mycobacterium tuberculosis, any site (pulmonary or extrapulmonary) | 19 (18.3) |
| Mycobacterium, other species or unidentified species, disseminated or extrapulmonary | 2 (1.9) |
| Pneumocystis jirovecii pneumonia | 22 (21.2) |
| Progressive multifocal leukoencephalopathy | 1 (1.0) |
| Toxoplasmosis of brain | 10 (9.6) |
| Wasting syndrome due to HIV | 15 (14.4) |
| Outcome | Total (n = 436) | Without Missed Opportunities (n = 318) | With Missed Opportunities (n = 118) | p Value |
|---|---|---|---|---|
| AIDS-defining conditions at diagnosis—n (%) | 76 (17.4) | 41 (12.9) | 35 (29.7) | <0.001 |
| CD4 count ≤ 200 cells/mm3 at diagnosis—n (%) | 145 (33.3) | 96 (30.3) | 49 (41.5) | 0.027 |
| CD4 count ≤ 350 cells/mm3 at diagnosis—n (%) | 244 (56.0) | 177 (55.8) | 67 (56.8) | 0.860 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lourinho, J.; Miguel, M.J.; Gonçalves, F.; Vale, F.; Franco, C.S.; Marques, N. Missed Opportunities for HIV Diagnosis and Their Clinical Repercussions in the Portuguese Population—A Cohort Study. Pathogens 2024, 13, 683. https://doi.org/10.3390/pathogens13080683
Lourinho J, Miguel MJ, Gonçalves F, Vale F, Franco CS, Marques N. Missed Opportunities for HIV Diagnosis and Their Clinical Repercussions in the Portuguese Population—A Cohort Study. Pathogens. 2024; 13(8):683. https://doi.org/10.3390/pathogens13080683
Chicago/Turabian StyleLourinho, João, Maria João Miguel, Frederico Gonçalves, Francisco Vale, Cláudia Silva Franco, and Nuno Marques. 2024. "Missed Opportunities for HIV Diagnosis and Their Clinical Repercussions in the Portuguese Population—A Cohort Study" Pathogens 13, no. 8: 683. https://doi.org/10.3390/pathogens13080683
APA StyleLourinho, J., Miguel, M. J., Gonçalves, F., Vale, F., Franco, C. S., & Marques, N. (2024). Missed Opportunities for HIV Diagnosis and Their Clinical Repercussions in the Portuguese Population—A Cohort Study. Pathogens, 13(8), 683. https://doi.org/10.3390/pathogens13080683





